Effectiveness of Smartwatch Guidance for High-Quality Infant Cardiopulmonary Resuscitation: A Simulation Study
Abstract
1. Introduction
2. Materials and Methods
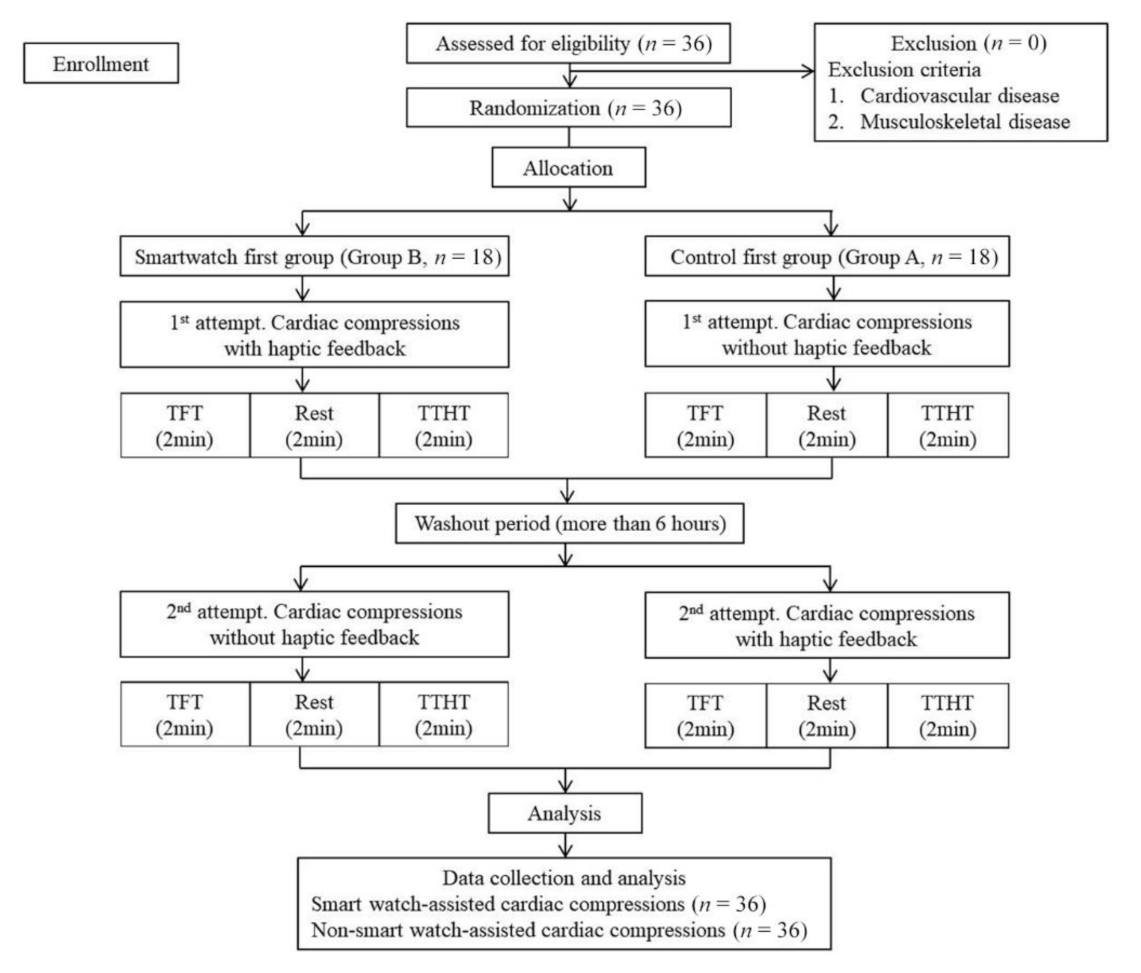
2.1. Study Design
2.2. Study Participants
2.3. Study Protocol
2.4. Description of the Devices
2.5. Measures
2.6. Outcomes
2.7. Data Analysis
3. Results
3.1. Result for CC Performance
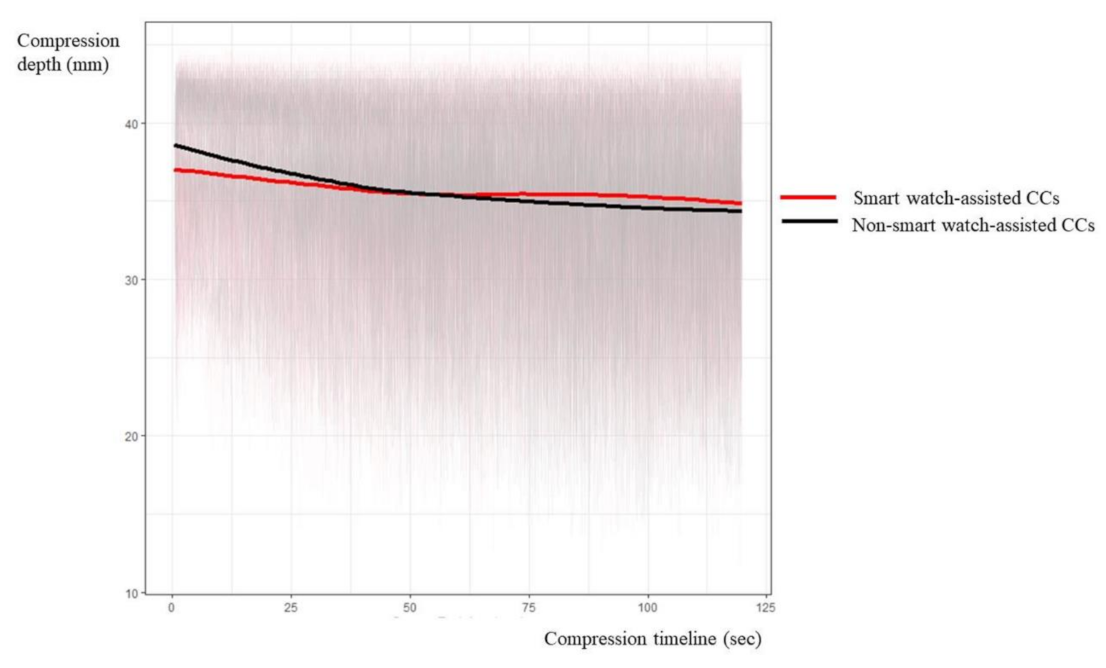
3.2. Results for Compression Depth
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Atkins, D.L.; Everson-Stewart, S.; Sears, G.K.; Daya, M.; Osmond, M.H.; Warden, C.R.; Berg, R.A.; ROC Investigators. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: The ROC Epistry-Cardiac Arrest. Circulation 2009, 119, 1484–1491. [Google Scholar]
- Fink, E.L.; Prince, D.K.; Kaltman, J.R.; Atkins, D.L.; Austin, M.; Warden, C.; Hutchison, J.; Daya, M.; Goldberg, S.; Herren, H.; et al. Unchanged pediatric out-of-hospital cardiac arrest incidence and survival rates with regional variation in North America. Resuscitation 2016, 107, 121–128. [Google Scholar] [CrossRef]
- Feneley, M.P.; Maier, G.W.; Kern, K.B.; Gaynor, J.W.; Gall, S.A.; Sanders, A.B.; Raessler, K.; Muhlbaier, L.H.; Rankin, J.S.; Ewy, G.A. Influence of compression rate on initial success of resuscitation and 24 hour survival after prolonged manual cardiopulmonary resuscitation in dogs. Circulation 1988, 77, 240–250. [Google Scholar] [CrossRef]
- Meaney, P.A.; Bobrow, B.J.; Mancini, M.E.; Christenson, J.; de Caen, A.R.; Bhanji, F.; Abella, B.S.; Kleinman, M.E.; Edelson, D.P.; Berg, R.A.; et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the American Heart Association. Circulation 2013, 128, 417–435. [Google Scholar] [CrossRef]
- Maconochie, I.K.; Bingham, R.; Eich, C.; Lopez-Herce, J.; Rodriguez-Nunez, A.; Rajka, T.; Van de Voorde, P.; Zideman, D.A.; Biarent, D.; Paediatric Life Support Section, Collaborators. European Resuscitation Council Guidelines for Resuscitation 2015: Section 6. Paediatric life support. Resuscitation 2015, 95, 223–248. [Google Scholar] [PubMed]
- Monsieurs, K.G.; Nolan, J.P.; Bossaert, L.L.; Greif, R.; Maconochie, I.K.; Nikolaou, N.I.; Perkins, G.D.; Soar, J.; Truhlar, A.; Wyllie, J.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 1. Executive summary. Resuscitation 2015, 95, 1–80. [Google Scholar] [CrossRef]
- Atkins, D.L.; Berger, S.; Duff, J.P.; Gonzales, J.C.; Hunt, E.A.; Joyner, B.L.; Meaney, P.A.; Niles, D.E.; Samson, R.A.; Schexnayder, S.M. Part 11: Pediatric Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care (reprint). Pediatrics 2015, 136, S167–S175. [Google Scholar] [CrossRef] [PubMed]
- De Caen, A.R.; Berg, M.D.; Chameides, L.; Gooden, C.K.; Hickey, R.W.; Scott, H.F.; Sutton, R.M.; Tijssen, J.A.; Topjian, A.; Van Der Jagt, É.W.; et al. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care (reprint). Pediatrics 2015, 136, S176–S195. [Google Scholar] [CrossRef]
- Kleinman, M.E.; Brennan, E.E.; Goldberger, Z.D.; Swor, R.A.; Terry, M.; Bobrow, B.J.; Gazmuri, R.J.; Travers, A.H.; Rea, T. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 132, S414–S435. [Google Scholar] [CrossRef]
- Link, M.S.; Berkow, L.C.; Kudenchuk, P.J.; Halperin, H.R.; Hess, E.P.; Moitra, V.K.; Neumar, R.W.; O’Neil, B.J.; Paxton, J.H.; Silvers, S.M.; et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 132, S444–S464. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.D.; Olasveengen, T.M.; Maconochie, I.; Soar, J.; Wyllie, J.; Greif, R.; Lockey, A.; Semeraro, F.; Van De Voorde, P.; Lott, C.; et al. European Resuscitation Council guidelines for resuscitation: 2017 update. Resuscitation 2018, 123, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.W.; Oh, J.H. Effect of metronome guidance on infant cardiopulmonary resuscitation. Eur. J. Pediatr. 2019, 178, 795–801. [Google Scholar] [CrossRef]
- Yu, B.G.; Oh, J.H.; Kim, Y.; Kim, T.W. Accurate measurement of chest compression depth using impulse-radio ultra-wideband sensor on a mattress. PLoS ONE 2017, 12, e0183971. [Google Scholar] [CrossRef]
- Kirkbright, S.; Finn, J.; Tohira, H.; Bremner, A.; Jacobs, I.; Celenza, A. Audiovisual feedback device use by health care professionals during CPR: A systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation 2014, 85, 460–471. [Google Scholar] [CrossRef]
- Martin, P.; Theobald, P.; Kemp, A.; Maguire, S.; Maconochie, I.; Jones, M. Real-time feedback can improve infant manikin cardiopulmonary resuscitation by up to 79%—A randomised controlled trial. Resuscitation 2013, 84, 1125–1130. [Google Scholar] [CrossRef] [PubMed]
- Abella, B.S.; Edelson, D.P.; Kim, S.; Retzer, E.; Myklebust, H.; Barry, A.M.; O’Hearn, N.; Hoek, T.L.V.; Becker, L.B. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resusciation 2007, 73, 54–61. [Google Scholar] [CrossRef]
- Lee, J.; Song, Y.; Oh, J.; Chee, Y.; Ahn, C.; Shin, H.; Kang, H.; Lim, T.H. Smartwatch feedback device for high-quality chest compressions by a single rescuer during infant cardiac arrest: A randomized, controlled simulation study. Eur. J. Emerg. Med. 2019, 26, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Chee, Y.; Oh, J.; Ahn, C.; Lim, T.H. Smartwatches as chest compression feedback devices: A feasibility study. Resuscitation 2016, 103, 20–23. [Google Scholar] [CrossRef] [PubMed]
- Reeder, B.; David, A. Health at hand: A systematic review of smart watch uses for health and wellness. J. Biomed. Inform. 2016, 63, 269–276. [Google Scholar] [CrossRef]
- Lu, T.-C.; Chang, Y.-T.; Ho, T.-W.; Chen, Y.; Lee, Y.-T.; Wang, Y.-S.; Chen, Y.-P.; Tsai, C.-L.; Ma, M.H.-M.; Fang, C.-C.; et al. Using a smartwatch with real-time feedback improves the delivery of high-quality cardiopulmonary resuscitation by healthcare professionals. Resuscitation 2019, 140, 16–22. [Google Scholar] [CrossRef]
- Ahn, C.; Lee, J.; Oh, J.; Song, Y.; Chee, Y.; Lim, T.H.; Kang, H.; Shin, H. Effectiveness of feedback with a smartwatch for high-quality chest compressions during adult cardiac arrest: A randomized controlled simulation study. PLoS ONE 2017, 12, e0169046. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Hsia, S.-H.; Lee, E.-P.; Chan, O.-W.; Lin, J.-J.; Wu, H.-P. Effect of audiovisual cardiopulmonary resuscitation feedback device on improving chest compression quality. Sci. Rep. 2020, 10, 398. [Google Scholar] [CrossRef] [PubMed]
- Monsieurs, K.G.; De Regge, M.; Vansteelandt, K.; De Smet, J.; Annaert, E.; LeMoyne, S.; Kalmar, A.F.; Calle, P.A. Excessive chest compression rate is associated with insufficient compression depth in prehospital cardiac arrest. Resuscitation 2012, 83, 1319–1323. [Google Scholar] [CrossRef]
- Lu, L.; Zhang, J.; Xie, Y.; Gao, F.; Xu, S.; Wu, X.; Ye, Z. Wearable health devices in health care: Narrative systematic review. JMIR mHealth uHealth 2020, 8, e18907. [Google Scholar] [CrossRef] [PubMed]
- Wee, J.C.P.; Nandakumar, M.; Chan, Y.H.; Yeo, R.S.L.; Kaur, K.; Anantharaman, V.; Yap, S.; Ong, M.E.H. Effect of using an audiovisual CPR feedback device on chest compression rate and depth. Ann. Acad. Med. Singap. 2014, 43, 33–38. [Google Scholar]
- Choi, B.; Kim, T.; Yoon, S.Y.; Yoo, J.S.; Won, H.-J.; Kim, K.; Kang, E.J.; Yoon, H.; Hwang, S.Y.; Shin, T.G.; et al. Effect of watch-type haptic metronome on the quality of cardiopulmonary resuscitation: A simulation study. Health Inform. Res. 2019, 25, 274–282. [Google Scholar] [CrossRef]
- Berden, H.J.; Willems, F.F.; Hendrick, J.M.; Pijls, N.H.; Knape, J.T. How frequently should basic cardiopulmonary resuscitation training be repeated to maintain adequate skills? BMJ 1993, 306, 1576–1577. [Google Scholar] [CrossRef]
- Haque, I.U.; Udassi, J.P.; Udassi, S.; Theriaque, U.W.; Shuster, J.J.; Zaritsky, A.L. Chest compression quality and rescuer fatigue with increased compression to ventilation ratio during single rescuer pediatric CPR. Resuscitation 2008, 79, 82–89. [Google Scholar] [CrossRef]
- Pece, F.; Zarate, J.J.; Vechev, V.; Besse, N.; Gudozhnik, O.; Shea, H.; Hilliges, O. MagTics: Flexible and Thin Form Factor Magnetic Actuators for Dynamic and Wearable Haptic Feedback. In Proceedings of the 30th Annual ACM Symposium on User Interface Software and Technology, Quebec, QC, Canada, 22–25 October; 2017; pp. 143–154. [Google Scholar]

| Smartwatch First Group (n = 18) | Control First Group (n = 18) | p-Value | |
|---|---|---|---|
| Age, median (IQR) | 28.5 (25.0–30.0) | 27.5 (25.0–31.0) | 0.622 |
| Sex, n (%) | 1 | ||
| Male | 6 (33.3%) | 7 (38.9%) | |
| Female | 12 (66.7%) | 11 (61.1%) | |
| Job, n (%) | 0.298 | ||
| Doctor | 12 (66.6%) | 16 (88.8%) | |
| EMT | 5 (27.8%) | 1 (5.6%) | |
| Nurse | 1 (5.6%) | 1 (5.6%) | |
| Work experience, n (%) | 1 | ||
| Up to 3 years | 9 (50.0%) | 8 (44.4%) | |
| More than 3 years | 9 (50.0%) | 10 (55.6%) | |
| Experience of cardiac compression within 5 years (IQR) | 30.0 (10.0–50.0) | 30.0 (20.0–50.0) | 0.662 |
| Experience of cardiac compression within 1 month (IQR) | 2.0 (0.0–5.0) | 4.0 (3.0–5.0] | 0.032 |
| Smartwatch -Assisted CCs | Non-Smartwatch -Assisted CCs | p-Value | |
|---|---|---|---|
| Total number of chest compression | 15,585 | 16,212 | |
| Proportion of optimal chest compression (%) | 11,081 (71.1%) | 9630 (59.4%) | <0.001 |
| Chest compression duration (msec) | 550.8 ± 54.8 | 529.9 ± 68.4 | <0.001 |
| Parameter | Level (vs. Ref.) | Estimate | Standard Error | 95% Confidence Limits | Z | p-Value | ||
|---|---|---|---|---|---|---|---|---|
| Group | Smartwatch-assisted CCs vs. Non-smartwatch-assisted CCs | 18.15 | 4.79 | 8.75 | 27.54 | 3.78 | <0.001 | |
| Quartile | 2Q vs. 1Q | 9.39 | 2.40 | 4.69 | 14.09 | 3.92 | <0.001 | |
| 3Q vs. 1Q | 12.95 | 3.15 | 6.78 | 19.13 | 4.11 | |||
| 4Q vs. 1Q | 13.69 | 3.19 | 7.44 | 19.93 | 4.3 | |||
| Method | TTHT vs. TFT | −0.32 | 4.53 | −9.19 | 8.55 | −0.07 | 0.943 | |
| Group* quartile | Smartwatch-assisted CCs vs. Non-smartwatch-assisted CCs | 2Q vs. 1Q | 0.86 | 2.40 | −3.85 | 5.57 | 0.36 | 0.266 |
| 3Q vs. 1Q | 3.99 | 3.50 | −2.86 | 10.84 | 1.14 | |||
| 4Q vs. 1Q | 6.16 | 3.44 | −0.58 | 12.89 | 1.79 | |||
| Parameter | Level (vs. Ref.) | Estimate | Standard Error | 95% Confidence Limits | Z | p-Value | |
|---|---|---|---|---|---|---|---|
| Group | Smartwatch-assisted CCs vs. Non-smartwatch-assisted CCs | −8.56 | 3.63 | −15.68 | −1.45 | −2.36 | 0.018 |
| Method | TTHT vs. TFT | 4.03 | 2.11 | −0.11 | 8.16 | 1.91 | 0.057 |
| Average Compressions | Smartwatch -Assisted CCs | Non-Smartwatch -Assisted CCs | Overall |
|---|---|---|---|
| TFT | 216.01 | 224.57 | 220.29 |
| TTHT | 220.04 | 228.60 | 224.32 |
| Overall | 218.02 | 226.59 | 222.31 |
| Absolute difference from 220 | 1.98 | 6.59 |
| Parameter | Level (vs. Ref.) | Estimate | Standard Error | 95% Confidence Limits | Z | p−Value | Odds Ratio | 95% CI of OR | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | Smartwatch-assisted CCs vs. Non-smartwatch assisted CCs | −0.44 | 0.27 | −0.96 | 0.08 | −1.67 | 0.096 | 0.64 | 0.38 | 1.08 | |
| Quartile | 2Q vs. 1Q | −0.54 | 0.16 | −0.85 | −0.24 | −3.48 | <0.001 | 0.58 | 0.43 | 0.79 | |
| 3Q vs. 1Q | −0.71 | 0.19 | −1.09 | −0.34 | −3.71 | 0.49 | 0.34 | 0.72 | |||
| 4Q vs. 1Q | −0.91 | 0.20 | −1.30 | −0.52 | −4.56 | 0.40 | 0.27 | 0.59 | |||
| Method | TTHT vs. TFT | 2.14 | 0.33 | 1.49 | 2.78 | 6.49 | <0.001 | 8.49 | 4.45 | 16.19 | |
| Group* Quartile | Smartwatch-assisted CCs vs. Non-smartwatch-assisted CCs | 2Q vs. 1Q | 0.39 | 0.19 | 0.03 | 0.76 | 2.13 | 0.015 | 1.49 | 1.03 | 2.14 |
| 3Q vs. 1Q | 0.59 | 0.24 | 0.12 | 1.05 | 2.47 | 1.80 | 1.13 | 2.87 | |||
| 4Q vs. 1Q | 0.77 | 0.25 | 0.28 | 1.26 | 3.11 | 2.16 | 1.33 | 3.52 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeon, S.A.; Chang, H.; Yoon, S.Y.; Hwang, N.; Kim, K.; Yoon, H.; Hwang, S.Y.; Shin, T.G.; Cha, W.C.; Kim, T. Effectiveness of Smartwatch Guidance for High-Quality Infant Cardiopulmonary Resuscitation: A Simulation Study. Medicina 2021, 57, 193. https://doi.org/10.3390/medicina57030193
Jeon SA, Chang H, Yoon SY, Hwang N, Kim K, Yoon H, Hwang SY, Shin TG, Cha WC, Kim T. Effectiveness of Smartwatch Guidance for High-Quality Infant Cardiopulmonary Resuscitation: A Simulation Study. Medicina. 2021; 57(3):193. https://doi.org/10.3390/medicina57030193
Chicago/Turabian StyleJeon, Seong A, Hansol Chang, Sun Young Yoon, Nayeong Hwang, Kyunga Kim, Hee Yoon, Sung Yeon Hwang, Tae Gun Shin, Won Chul Cha, and Taerim Kim. 2021. "Effectiveness of Smartwatch Guidance for High-Quality Infant Cardiopulmonary Resuscitation: A Simulation Study" Medicina 57, no. 3: 193. https://doi.org/10.3390/medicina57030193
APA StyleJeon, S. A., Chang, H., Yoon, S. Y., Hwang, N., Kim, K., Yoon, H., Hwang, S. Y., Shin, T. G., Cha, W. C., & Kim, T. (2021). Effectiveness of Smartwatch Guidance for High-Quality Infant Cardiopulmonary Resuscitation: A Simulation Study. Medicina, 57(3), 193. https://doi.org/10.3390/medicina57030193






