PD-L1 Expression in Different Segments and Histological Types of Ovarian Cancer According to Lymphocytic Infiltrate
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Tissue Microarray (TMA)
2.3. Immunohistochemical Analysis
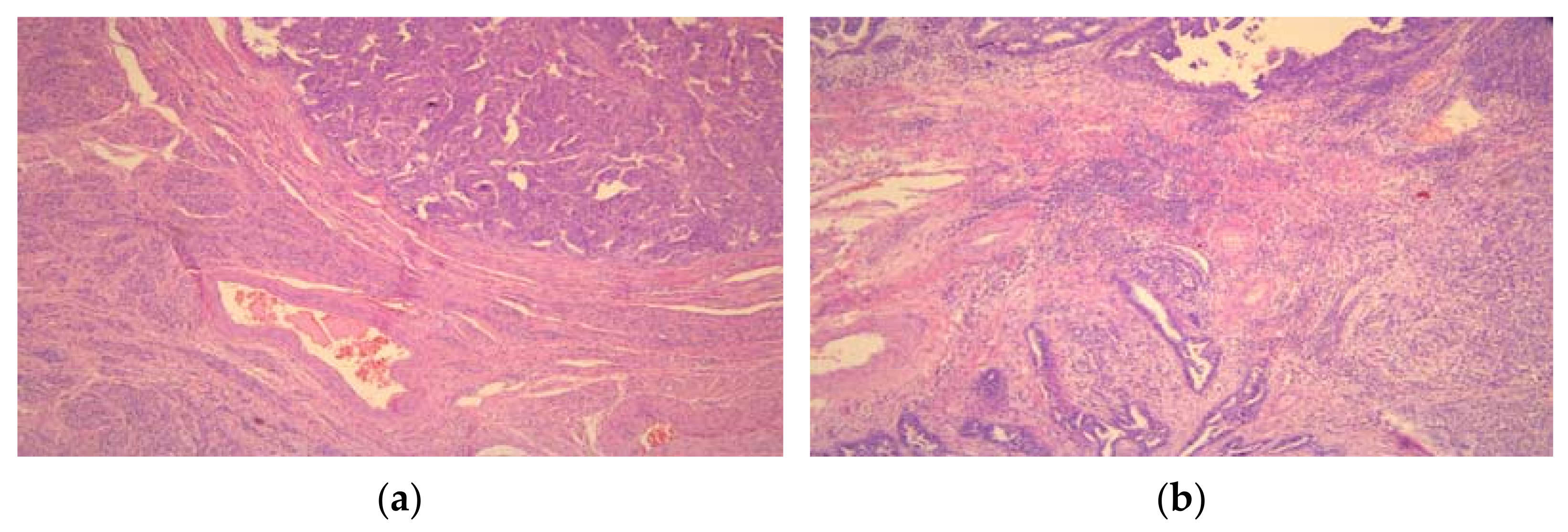
2.4. Tumor-Infiltrating Lymphocytes (TILs)
2.5. Statistical Analysis
3. Results
3.1. Clinical and Histopathological Characteristics
3.2. Immunohistochemical Analysis of PD-L1 Expression
3.3. PD-L1 Expression in Different Tumor Parts in Relation to the Localization of Lymphocytic Infiltrate
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Battaglia, A.; Piermattei, A.; Buzzonetti, A.; Pasciuto, T.; Zampetti, N.; Fossati, M.; Angelico, G.; Iacobelli, V.; Nero, C.; Iannucci, V.; et al. PD-L1 Expression on Circulating Tumour-Derived Microvesicles as a Complementary Tool for Stratification of High-Grade Serous Ovarian Cancer Patients. Cancers 2021, 13, 5200. [Google Scholar] [CrossRef] [PubMed]
- Motalleb Nezhad, M.; Jadidi-Niaragh, F.; Ghamsari, E.S.; Bagheri, S.; Gharibi, T.; Yousefi, M. The immunobiology of myeloid-derived suppressor cells in cancer. Tumor Biol. 2016, 37, 1387–1406. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.S.; Mellman, I. Elements of cancer immunity and the cancer-immune set point. Nature 2017, 541, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Farrag, M.S.; Abdelwahab, K.; Farrag, N.S.; Elrefaie, W.E.; Emarah, Z. Programmed death ligand-1 and CD8 tumor-infiltrating lymphocytes (TILs) as prognostic predictors in ovarian high-grade serous carcinoma (HGSC). J. Egypt. Natl. Cancer Inst. 2021, 33, 16. [Google Scholar] [CrossRef]
- Pietzner, K.; Nasser, S.; Alavi, S.; Darb-Esfahani, S.; Passler, M.; Muallem, M.Z.; Sehouli, J. Checkpoint-inhibition in ovarian cancer: Rising star or just a dream? J. Gynecol. Oncol. 2018, 29, e93. [Google Scholar] [CrossRef]
- Zhu, X.; Lang, J. Programmed death-1 pathway blockade produces a synergistic antitumor effect: Combined application in ovarian cancer. J. Gynecol. Oncol. 2017, 28, e64. [Google Scholar] [CrossRef] [Green Version]
- Darb-Esfahani, S.; Kunze, C.A.; Kulbe, H.; Sehouli, J.; Wienert, S.; Lindner, J.; Budczies, J.; Bockmayr, M.; Dietel, M.; Denkert, C.; et al. Prognostic impact of programmed cell death-1 (PD-1) and PD-ligand 1 (PD-L1) expression in cancer cells and tumor-infiltrating lymphocytes in ovarian high grade serous carcinoma. Oncotarget 2016, 7, 1486–1499. [Google Scholar] [CrossRef] [Green Version]
- Hwang, W.T.; Adams, S.F.; Tahirovic, E.; Hagemann, I.S.; Coukos, G. Prognostic significance of tumor-infiltrating T cells in ovarian cancer: A meta-analysis. Gynecol. Oncol. 2012, 124, 192–198. [Google Scholar] [CrossRef] [Green Version]
- Landskron, J.; Helland, O.; Torgersen, K.M.; Aandahl, E.M.; Gjertsen, B.T.; Bjorge, L.; Taskén, K. Activated regulatory and memory T-cells accumulate in malignant ascites from ovarian carcinoma patients. Cancer Immunol. Immunother. 2015, 64, 337–347. [Google Scholar] [CrossRef]
- Bansal, A.; Srinivasan, R.; Rohilla, M.; Rai, B.; Rajwanshi, A.; Suri, V.; Saha, S.C. Immunotyping in tubo-ovarian high-grade serous carcinoma by PD-L1 and CD8+ T-lymphocytes predicts disease-free survival. APMIS 2021, 129, 254–264. [Google Scholar] [CrossRef]
- D’Incecco, A.; Andreozzi, M.; Ludovini, V.; Rossi, E.; Capodanno, A.; Landi, L.; Tibaldi, C.; Minuti, G.; Salvini, J.; Coppi, E.; et al. PD-1 and PD-L1 expression in molecularly selected non-small-cell lung cancer patients. Br. J. Cancer 2015, 112, 95–102. [Google Scholar] [CrossRef] [Green Version]
- Heymann, J.J.; Bulman, W.A.; Swinarski, D.; Pagan, C.A.; Crapanzano, J.P.; Haghighi, M.; Fazlollahi, L.; Stoopler, M.B.; Sonett, J.R.; Sacher, A.G.; et al. PD-L1 expression in non-small cell lung carcinoma: Comparison among cytology, small biopsy, and surgical resection specimens. Cancer Cytopathol. 2017, 125, 896–907. [Google Scholar] [CrossRef] [Green Version]
- Scognamiglio, G.; De Chiara, A.; Di Bonito, M.; Tatangelo, F.; Losito, N.S.; Anniciello, A.; De Cecio, R.; D’Alterio, C.; Scala, S.; Cantile, M.; et al. Variability in Immunohistochemical Detection of Programmed Death Ligand 1 (PD-L1) in Cancer Tissue Types. Int. J. Mol. Sci. 2016, 17, 790. [Google Scholar] [CrossRef] [Green Version]
- Gaillard, S.L.; Secord, A.A.; Monk, B. The role of immune checkpoint inhibition in the treatment of ovarian cancer. Gynaecol. Oncol. Res. Pract. 2016, 3, 11. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.; Lou, W.; Di, W.; Wu, X. Prognostic value of tumor PD-L1 expression combined with CD8+ tumor infiltrating lymphocytes in high grade serous ovarian cancer. Int. Immunopharmacol. 2017, 52, 7–14. [Google Scholar] [CrossRef]
- Choi, C.H.; Kim, K.H.; Song, J.Y.; Choi, S.J.; Kim, L.; Park, I.S.; Han, J.Y.; Kim, J.M.; Chu, Y.C. Construction of high-density tissue microarrays at low cost by using self-made manual microarray kits and recipient paraffin blocks. Korean J. Pathol. 2012, 46, 562–568. [Google Scholar] [CrossRef]
- Dako. PD-L1 IHC 22C3 PharmDx Interpretation Manual—Gastric or Gastroesophageal Junction Adenocarcinoma. PD-L1 IHC 22C3 pharmDx Is FDA-Approved for In Vitro Diagnostic Use. 2019. Available online: https://www.agilent.com/cs/library/usermanuals/public/29219_pd-l1-ihc-22C3-pharmdx-gastric-interpretation-manual_us.pdf (accessed on 28 November 2021).
- Dako. PD-L1 IHC 22C3 PharmDX Interpretation Manual—NSCLC—For In Vitro Diagnostic Use. 2018. Available online: https://usermanual.wiki/m/36cf5deff6015d44ebe696b439deba5ec850657a9b00689e6c52d5bc11706076.pdf (accessed on 28 November 2021).
- Teng, M.W.; Ngiow, S.F.; Ribas, A.; Smyth, M.J. Classifying cancers based on T-cell infiltration and PD-L1. Cancer Res. 2015, 75, 2139–2145. [Google Scholar] [CrossRef] [Green Version]
- Zhang, C.; Yang, Q. Predictive Values of Programmed Cell Death-Ligand 1 Expression for Prognosis, Clinicopathological Factors, and Response to Programmed Cell Death-1/Programmed Cell Death-Ligand 1 Inhibitors in Patients with Gynecological Cancers: A Meta-Analysis. Front. Oncol. 2021, 10, 572203. [Google Scholar] [CrossRef]
- Santoiemma, P.P.; Powell, D.J., Jr. Tumor infiltrating lymphocytes in ovarian cancer. Cancer Biol. Ther. 2015, 16, 807–820. [Google Scholar] [CrossRef]
- Nhokaew, W.; Kleebkaow, P.; Chaisuriya, N.; Kietpeerakool, C. Programmed Death Ligand 1 (PD-L1) Expression in Epithelial Ovarian Cancer: A Comparison of Type I and Type II Tumors. Asian Pac. J. Cancer Prev. 2019, 20, 1161–1169. [Google Scholar] [CrossRef] [Green Version]
- Webb, J.R.; Milne, K.; Kroeger, D.R.; Nelson, B.H. PD-L1 expression is associated with tumor-infiltrating T cells and favorable prognosis in high-grade serous ovarian cancer. Gynecol. Oncol. 2016, 141, 293–302. [Google Scholar] [CrossRef] [Green Version]
- Strickland, K.; Howitt, B.E.; Rodig, S.J.; Ritterhouse, L.; D’Andrea, D.A.; Matulonis, U.; Konstantinopoulos, P. Tumor infiltrating and peritumoral T cells and expression of PD-L1 in BRCA1/2-mutated high grade serous ovarian cancers. J. Clin. Oncol. 2015, 33, 5512. [Google Scholar] [CrossRef]
- Chen, H.; Molberg, K.; Strickland, A.L.; Castrillon, D.H.; Carrick, K.; Jiang, Q.; Niu, S.; Rivera-Colon, G.; Gwin, K.; Hinson, S.; et al. PD-L1 Expression and CD8+ Tumor-infiltrating Lymphocytes in Different Types of Tubo-ovarian Carcinoma and Their Prognostic Value in High-grade Serous Carcinoma. Am. J. Surg. Pathol. 2020, 44, 1050–1060. [Google Scholar] [CrossRef]
- Hamanishi, J.; Mandai, M.; Iwasaki, M.; Okazaki, T.; Tanaka, Y.; Yamaguchi, K.; Higuchi, T.; Yagi, H.; Takakura, K.; Minato, N.; et al. Programmed cell death 1 ligand 1 and tumor-infiltrating CD8+ T lymphocytes are prognostic factors of human ovarian cancer. Proc. Natl. Acad. Sci. USA 2007, 104, 3360–3365. [Google Scholar] [CrossRef] [Green Version]
- Martin de la Fuente, L.; Westbom-Fremer, S.; Arildsen, N.S.; Hartman, L.; Malander, S.; Kannisto, P.; Måsbäck, A.; Hedenfalk, I. PD-1/PD-L1 expression and tumor-infiltrating lymphocytes are prognostically favorable in advanced high-grade serous ovarian carcinoma. Virchows Arch. 2020, 477, 83–91. [Google Scholar] [CrossRef] [Green Version]
- Bekos, C.; Pils, D.; Dekan, S.; Hofstetter, G.; Horak, P.; Reinthaller, A.; Polterauer, S.; Schwameis, R.; Aust, S. PD-1 and PD-L1 expression on TILs in peritoneal metastases compared to ovarian tumor tissues and its associations with clinical outcome. Sci. Rep. 2021, 11, 6400. [Google Scholar] [CrossRef]
- Diskin, B.; Adam, S.; Cassini, M.F.; Sanchez, G.; Liria, M.; Aykut, B.; Buttar, C.; Li, E.; Sundberg, B.; Salas, R.D.; et al. PD-L1 engagement on T cells promotes self-tolerance and suppression of neighboring macrophages and effector T cells in cancer. Nat. Immunol. 2020, 21, 442–454. [Google Scholar] [CrossRef]
- Pawłowska, A.; Kwiatkowska, A.; Suszczyk, D.; Chudzik, A.; Tarkowski, R.; Barczyński, B.; Kotarski, J.; Wertel, I. Clinical and Prognostic Value of Antigen-Presenting Cells with PD-L1/PD-L2 Expression in Ovarian Cancer Patients. Int. J. Mol. Sci. 2021, 22, 11563. [Google Scholar] [CrossRef]
- Maiorano, B.A.; Maiorano, M.F.P.; Lorusso, D.; Maiello, E. Ovarian Cancer in the Era of Immune Checkpoint Inhibitors: State of the Art and Future Perspectives. Cancers 2021, 13, 4438. [Google Scholar] [CrossRef]
- Parvathareddy, S.K.; Siraj, A.K.; Al-Badawi, I.A.; Tulbah, A.; Al-Dayel, F.; Al-Kuraya, K.S. Differential expression of PD-L1 between primary and metastatic epithelial ovarian cancer and its clinico-pathological correlation. Sci. Rep. 2021, 11, 3750. [Google Scholar] [CrossRef] [PubMed]
- Wan, C.; Keany, M.P.; Dong, H.; Al-Alem, L.F.; Pandya, U.M.; Lazo, S.; Boehnke, K.; Lynch, K.N.; Xu, R.; Zarrella, D.T.; et al. Enhanced Efficacy of Simultaneous PD-1 and PD-L1 Immune Checkpoint Blockade in High-Grade Serous Ovarian Cancer. Cancer Res. 2021, 81, 158–173. [Google Scholar] [CrossRef] [PubMed]

| Total n = 328 | EOT | p | EOC vs. ATP | EOC vs. BOT | ATP vs. BOT | |||
|---|---|---|---|---|---|---|---|---|
| EOC n = 122 | ATP n = 42 | BOT n = 164 | ||||||
| Age, mean ± sd (years) | 52.4 ± 15.8 | 61.8 ± 10.1 | 45.8 ± 12.2 | 47.2 ± 15.6 | <0.001 | <0.001 | <0.001 | 0.834 |
| Menopause, n (%) | ||||||||
| Yes | 199 (60.7) | 106 (86.9) | 20 (47.6) | 73 (44.5) | <0.001 | <0.001 | <0.001 | 0.718 |
| No | 129 (39.3) | 16 (13.1) | 22 (52.4) | 91 (55.5) | ||||
| Histological type, n (%) | ||||||||
| Serous | 206 (62.8) | 103 (84.4) | 25 (59.5) | 78 (47.6) | <0.001 | <0.001 | <0.001 | 0.044 |
| Mucinous | 112 (34.1) | 10 (8.2) | 16 (38.1) | 86 (52.4) | ||||
| Endometrioid | 10 (3.0) | 9 (7.4) | 1 (2.4) | 0 (0.0) | ||||
| FIGO stage, n (%) | ||||||||
| I + II | 81 (49.4) | 39 (32.0) | 42 (100.0) | / | <0.001 | <0.001 | NA | NA |
| III + IV | 83 (50.6) | 83 (68.0) | 0 (0.0) | / | ||||
| Characteristic | EOCs n = 122 | p a | p b | p c | ||
|---|---|---|---|---|---|---|
| Serous n = 103 | Mucinous n = 10 | Endometrioid n = 9 | ||||
| Differentiation (Grade), n (%) | ||||||
| Well and moderately differentiated (Grade 1 + Grade 2) | 12 (11.7) | 9 (90.0) | 6 (66.7) | <0.001 | <0.001 | 0.213 |
| Poorly differentiated (Grade 3) | 91 (88.3) | 1 (10.0) | 3 (33.3) | |||
| Lymphovascular invasion, n (%) | 95 (92.2) | 4 (40.0) | 4 (44.4) | <0.001 | <0.001 | 1.000 |
| Necrosis, n (%) | 88 (85.4) | 5 (50.0) | 4 (44.4) | 0.005 | 0.001 | 1.000 |
| Intratumoral lymphocyte infiltration, n (%) | 89 (86.4) | 3 (30.0) | 7 (77.8) | <0.001 | <0.001 | 0.070 |
| Peritumoral lymphocyte infiltration, n (%) | 96 (93.2) | 6 (60.0) | 8 (88.9) | 0.008 | 0.003 | 0.303 |
| PD-L1 Expression Level | Group | p | EOC vs. ATP | EOC vs. BOT | ATP vs. BOT | ||
|---|---|---|---|---|---|---|---|
| EOC | ATP | BOT | |||||
| 0 | 0 (0.0) | 7 (16.7) | 159 (97.0) | <0.001 | <0.001 | <0.001 | <0.001 |
| 1+ | 34 (27.9) | 30 (71.4) | 5 (3.0) | ||||
| 2+ | 86 (70.5) | 5 (11.9) | 0 (0.0) | ||||
| 3+ | 2 (1.6) | 0 (0.0) | 0 (0.0) | ||||
| Characteristic | Categories | PD-L1 Expression | p | ||||
|---|---|---|---|---|---|---|---|
| Absent/Low * | High * | ||||||
| Age | <65 | 21 (31.8) | 45 (68.2) | 0.291 | |||
| 65+ | 13 (23.2) | 43 (76.8) | |||||
| Menopausal status | Yes | 28 (26.4) | 78 (73.6) | 0.357 | |||
| No | 6 (37.5) | 10 (62.5) | |||||
| Localization | Unilateral | 20 (50.0) | 20 (50.0) | <0.001 | |||
| Bilateral | 14 (17.1) | 68 (82.9) | |||||
| EOC size (mm) | <80 | 14 (24.6) | 43 (75.4) | 0.445 | |||
| ≥80 | 20 (30.8) | 45 (69.2) | |||||
| Histological type | Serous | HGSC | 21 (20.4) | 15 (16.5) | 82 (79.6) | 76 (83.5) | <0.001 |
| LGSC | 6 (50.0) | 6 (50.0) | |||||
| Mucinous | 7 (70.0) | 3 (30.0) | <0.001 | ||||
| Endometrioid | 6 (66.7) | 3 (33.3) | |||||
| FIGO stage | I + II | 30 (76.9) | 9 (23.1) | <0.001 | |||
| III + IV | 4 (4.8) | 79 (95.2) | |||||
| Differentiation (Grade) | 1 | 15 (100.0) | 0 | <0.001 | |||
| 2 | 4 (33.3) | 8 (66.7) | |||||
| 3 | 15 (15.8) | 80 (84.2) | |||||
| Necrosis | Yes | 19 (19.6) | 78 (80.4) | <0.001 | |||
| No | 15 (60.0) | 10 (40.0) | |||||
| Lymphovascular invasion | Yes | 18 (17.5) | 85 (82.5) | <0.001 | |||
| No | 16 (84.2) | 3 (15.8) | |||||
| Intratumoral lymphocyte infiltration | Yes | 20 (20.2) | 79 (79.8) | <0.001 | |||
| No | 14 (60.9) | 9 (39.1) | |||||
| Peritumoral lymphocyte infiltration | Yes | 27 (24.5) | 83 (75.5) | 0.013 | |||
| No | 7 (58.3) | 5 (41.7) | |||||
| Categories of PD-L1 Expression | Tumor Localization | p | |
|---|---|---|---|
| Center | Invasive Front | ||
| HGSC | |||
| 1+ | 15 (16.5) | 3 (3.3) | <0.001 |
| 2+ | 74 (81.3) | 60 (65.9) | |
| 3+ | 2 (2.2) | 28 (30.8) | |
| LGSC | |||
| 1+ | 6 (50.0) | 1 (8.3) | 0.069 |
| High expression (2+ and 3+) | 6 (50.0) | 11 (91.7) | |
| Mucinous EOC | |||
| 1+ | 7 (70.0) | 5 (50.0) | 0.650 |
| 2+ | 3 (30.0) | 5 (50.0) | |
| Endometrioid EOC | |||
| 1+ | 6 (66.7) | 3 (33.3) | 0.347 |
| 2+ | 3 (33.3) | 6 (66.7) | |
| Tumor Part | Categories of PD-L1 Expression | Intratumoral Lymphocytic Infiltrate | p | Peritumoral Lymphocytic Infiltrate | p | ||
|---|---|---|---|---|---|---|---|
| with | without | with | without | ||||
| Center | absent/low * | 14 (15.7) | 7 (50.0) | 0.003 | 18 (18.8) | 3 (42.9) | 0.126 |
| High ** | 75 (84.3) | 7 (50.0) | 78 (81.3) | 4 (57.1) | |||
| Invasive front | absent/low * | 2 (2.2) | 2 (14.3) | 0.088 | 3 (3.1) | 1 (14.3) | 0.249 |
| high * | 87 (97.8) | 12 (85.7) | 93 (96.9) | 6 (85.7) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jovanović, L.; Janković, R.; Ćirković, A.; Jović, M.; Janjić, T.; Djuričić, S.; Milenković, S. PD-L1 Expression in Different Segments and Histological Types of Ovarian Cancer According to Lymphocytic Infiltrate. Medicina 2021, 57, 1309. https://doi.org/10.3390/medicina57121309
Jovanović L, Janković R, Ćirković A, Jović M, Janjić T, Djuričić S, Milenković S. PD-L1 Expression in Different Segments and Histological Types of Ovarian Cancer According to Lymphocytic Infiltrate. Medicina. 2021; 57(12):1309. https://doi.org/10.3390/medicina57121309
Chicago/Turabian StyleJovanović, Ljubiša, Radmila Janković, Andja Ćirković, Milena Jović, Tijana Janjić, Slaviša Djuričić, and Svetlana Milenković. 2021. "PD-L1 Expression in Different Segments and Histological Types of Ovarian Cancer According to Lymphocytic Infiltrate" Medicina 57, no. 12: 1309. https://doi.org/10.3390/medicina57121309
APA StyleJovanović, L., Janković, R., Ćirković, A., Jović, M., Janjić, T., Djuričić, S., & Milenković, S. (2021). PD-L1 Expression in Different Segments and Histological Types of Ovarian Cancer According to Lymphocytic Infiltrate. Medicina, 57(12), 1309. https://doi.org/10.3390/medicina57121309







