Maternal–Fetal Outcomes in Women with Endometriosis and Shared Pathogenic Mechanisms
Abstract
1. Introduction
2. Materials and Methods
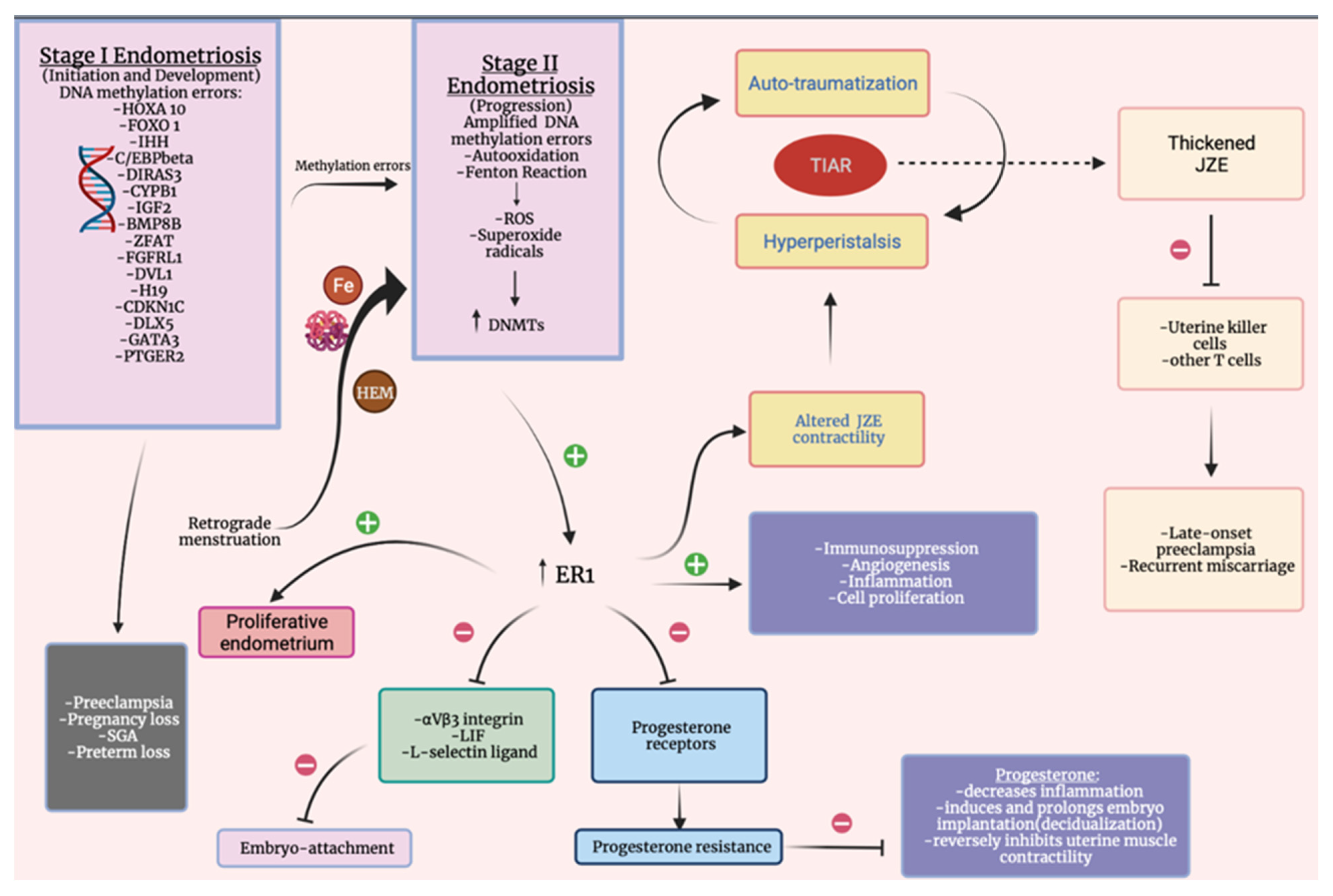
3. Pathogenic Mechanisms Involved in Adverse Pregnancy Outcomes in Women with Endometriosis
4. Placenta Praevia
5. Premature Rupture of Membranes, Spontaneous Preterm Birth
6. Gestational Hypertension, Preeclampsia
7. Obstetric Hemorrhages (Ante- and Postpartum Bleeding, Abruptio Placentae)
8. Miscarriage, Stillbirth, and Neonatal Death
9. Gestational Diabetes Mellitus, Gestational Cholestasis
10. Small for Gestational Age
11. Limitations and Further Perspectives
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Counsellor, V.S. Endometriosis: A clinical and surgical review. Am. J. Obstet. Gynecol. 1938, 36, 877. [Google Scholar] [CrossRef]
- Giudice, L.C.; Kao, L.C. Endometriosis. Lancet 2004, 364, 789–799. [Google Scholar] [CrossRef]
- Haas, D.; Wurm, P.; Schimetta, W.; Schabetsberger, K.; Shamiyeh, A.; Oppelt, P.; Binder, H. Endometriosis patients in the postmenopausal period: Pre- and postmenopausal factors influencing postmenopausal health. BioMed Res. Int. 2014, 2014, 746705. [Google Scholar] [CrossRef] [PubMed]
- Rock, J.A.; Markham, S.M. Pathogenesis of endometriosis. Lancet 1992, 340, 1264–1267. [Google Scholar] [CrossRef]
- Kennedy, S.; Bergqvist, A.; Chapron, C.; D’Hooghe, T.; Dunselman, G.; Greb, R.; Hummelshoj, L.; Prentice, A.; Saridogan, E. ESHRE guideline on the diagnosis and management of endometriosis. Hum. Reprod. 2005, 20, 2698–2704. [Google Scholar] [CrossRef]
- Soliman, A.M.; Yang, H.; Du, E.X.; Kelley, C.; Winkel, C. The direct and indirect costs associated with endometriosis: A systematic literature review. Hum. Reprod. 2016, 31, 712–722. [Google Scholar] [CrossRef] [PubMed]
- Stilley, J.A.W.; Birt, J.A.; Sharpe-Timms, K.L. Cellular and molecular basis for endometriosis-associated infertility. Cell Tissue Res. 2012, 349, 849–862. [Google Scholar] [CrossRef] [PubMed]
- Bulletti, C.; Coccia, M.E.; Battistoni, S.; Borini, A. Endometriosis and infertility. J. Assist. Reprod. Genet. 2010, 27, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Chapron, C.; Bourret, A.; Chopin, N.; Dousset, B.; Leconte, M.; Amsellem-Ouazana, D.; de Ziegler, D.; Borghese, B. Surgery for bladder endometriosis: Long-term results and concomitant management of associated posterior deep lesions. Hum. Reprod. 2010, 25, 884–889. [Google Scholar] [CrossRef]
- Andres, M.P.; Arcoverde, F.V.L.; Souza, C.C.C.; Fernandes, L.F.C.; Abrão, M.S.; Kho, R.M. Extrapelvic Endometriosis: A Systematic Review. J. Minim. Invasive Gynecol. 2020, 27, 373–389. [Google Scholar] [CrossRef]
- Redwine, D.B. Ovarian endometriosis: A marker for more extensive pelvic and intestinal disease. Fertil. Steril. 1999, 72, 310–315. [Google Scholar] [CrossRef]
- Chapron, C.; Pietin-Vialle, C.; Borghese, B.; Davy, C.; Foulot, H.; Chopin, N. Associated ovarian endometrioma is a marker for greater severity of deeply infiltrating endometriosis. Fertil. Steril. 2009, 92, 453–457. [Google Scholar] [CrossRef] [PubMed]
- Chapron, C.; Tosti, C.; Marcellin, L.; Bourdon, M.; Lafay-Pillet, M.C.; Millischer, A.E.; Streuli, I.; Borghese, B.; Petraglia, F.; Santulli, P. Relationship between the magnetic resonance imaging appearance of adenomyosis and endometriosis phenotypes. Hum. Reprod. 2017, 32, 1393–1401. [Google Scholar] [CrossRef] [PubMed]
- Leyendecker, G.; Bilgicyildirim, A.; Inacker, M.; Stalf, T.; Huppert, P.; Mall, G.; Böttcher, B.; Wildt, L. Adenomyosis and endometriosis. Re-visiting their association and further insights into the mechanisms of auto-traumatisation. An MRI study. Arch. Gynecol. Obstet. 2015, 291, 917–932. [Google Scholar] [CrossRef]
- Pinzauti, S.; Lazzeri, L.; Tosti, C.; Centini, G.; Orlandini, C.; Luisi, S.; Zupi, E.; Exacoustos, C.; Petraglia, F. Transvaginal sonographic features of diffuse adenomyosis in 18–30-year-old nulligravid women without endometriosis: Association with symptoms. Ultrasound Obstet. Gynecol. 2015, 46, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Harada, T.; Khine, Y.M.; Kaponis, A.; Nikellis, T.; Decavalas, G.; Taniguchi, F. The Impact of Adenomyosis on Women’s Fertility. Obstet. Gynecol. Surv. 2016, 71, 557–568. [Google Scholar] [CrossRef] [PubMed]
- Soave, I.; Wenger, J.M.; Pluchino, N.; Marci, R. Treatment options and reproductive outcome for adenomyosis-associated infertility. Curr. Med. Res. Opin. 2018, 34, 839–849. [Google Scholar] [CrossRef]
- Abbott, J.A. Adenomyosis and Abnormal Uterine Bleeding (AUB-A)-Pathogenesis, diagnosis, and management. Best Pract Res. Clin. Obstet. Gynaecol. 2017, 40, 68–81. [Google Scholar] [CrossRef]
- Pontis, A.; D’Alterio, M.N.; Pirarba, S.; de Angelis, C.; Tinelli, R.; Angioni, S. Adenomyosis: A systematic review of medical treatment. Gynecol. Endocrinol. 2016, 32, 696–700. [Google Scholar] [CrossRef] [PubMed]
- Lacheta, J. Uterine adenomyosis: Pathogenesis, diagnostics, symptomatology and treatment. Ceska Gynekol. 2019, 84, 240–246. [Google Scholar] [PubMed]
- Cron, R.S.; Gey, G. The viability of cast-off menstrual endometrium. Am. J. Obstet. Gynecol. 1927, 13, 645–647. [Google Scholar] [CrossRef]
- Gruenwald, P. Origin of endometriosis from the mesenchyme of the celomic walls. Am. J. Obstet. Gynecol. 1942, 44, 470–474. [Google Scholar] [CrossRef]
- Scutiero, G.; Iannone, P.; Bernardi, G.; Spadaro, S.; Volta, C.A.; Greco, P.; Nappi, L. Oxidative stress and endometriosis: A systematic review of the literature. Oxidative Med. Cell. Longev. 2017, 2017, 7265238. [Google Scholar] [CrossRef]
- Patel, B.G.; Rudnicki, M.; Yu, J.; Shu, Y.; Taylor, R.N. Progesterone resistance in endometriosis: Origins, consequences and interventions. Acta Obstet. Gynecol. Scand. 2017, 96, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, B.D.; Bulun, S.E. Endometriosis and nuclear receptors. Hum. Reprod. Update 2019, 25, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Nicholes, K.; Shih, I.M. The Origin and Pathogenesis of Endometriosis. Annu. Rev. Pathol. 2020, 15, 71–95. [Google Scholar] [CrossRef] [PubMed]
- Greene, A.D.; Lang, S.A.; Kendziorski, J.A.; Sroga-Rios, J.M.; Herzog, T.J.; Burns, K.A. Endometriosis: Where are we and where are we going? Reproduction 2016, 152, R63–R78. [Google Scholar] [CrossRef]
- Kolanska, K.; Alijotas-Reig, J.; Cohen, J.; Cheloufi, M.; Selleret, L.; d’Argent, E.; Kayem, G.; Valverde, E.E.; Fain, O.; Bornes, M.; et al. Endometriosis with infertility: A comprehensive review on the role of immune deregulation and immunomodulation therapy. Am. J. Reprod. Immunol. 2021, 85, e13384. [Google Scholar] [CrossRef]
- García-Gómez, E.; Vázquez-Martínez, E.R.; Reyes-Mayoral, C.; Cruz-Orozco, O.P.; Camacho-Arroyo, I.; Cerbón, M. Regulation of Inflammation Pathways and Inflammasome by Sex Steroid Hormones in Endometriosis. Front. Endocrinol. 2020, 10, 935. [Google Scholar] [CrossRef]
- Zubrzycka, A.; Zubrzycki, M.; Perdas, E.; Zubrzycka, M. Genetic, Epigenetic, and Steroidogenic Modulation Mechanisms in Endometriosis. J. Clin. Med. 2020, 9, 1309. [Google Scholar] [CrossRef]
- Laganà, A.S.; Garzon, S.; Götte, M.; Viganò, P.; Franchi, M.; Ghezzi, F.; Martin, D.C. The Pathogenesis of Endometriosis: Molecular and Cell Biology Insights. Int. J. Mol. Sci. 2019, 20, 5615. [Google Scholar] [CrossRef]
- Teng, S.W.; Horng, H.C.; Ho, C.H.; Yen, M.S.; Chao, H.T.; Wang, P.H. Taiwan Association of Gynecology Systematic Review Group. Women with endometriosis have higher comorbidities: Analysis of domestic data in Taiwan. J. Chin. Med. Assoc. 2016, 79, 577–582. [Google Scholar] [CrossRef] [PubMed]
- Shigesi, N.; Kvaskoff, M.; Kirtley, S.; Feng, Q.; Fang, H.; Knight, J.C.; Missmer, S.A.; Rahmioglu, N.; Zondervan, K.T.; Becker, C.M. The association between endometriosis and autoimmune diseases: A systematic review and meta-analysis. Hum. Reprod. Update 2019, 25, 486–503. [Google Scholar] [CrossRef] [PubMed]
- Parazzini, F.; Esposito, G.; Tozzi, L.; Noli, S.; Bianchi, S. Epidemiology of endometriosis and its comorbidities. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 209, 3–7. [Google Scholar] [CrossRef]
- Kok, V.C.; Tsai, H.J.; Su, C.F.; Lee, C.K. The Risks for Ovarian, Endometrial, Breast, Colorectal, and Other Cancers in Women With Newly Diagnosed Endometriosis or Adenomyosis: A Population-Based Study. Int. J. Gynecol. Cancer 2015, 25, 968–976. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.C.; Su, F.H.; Tzeng, C.R.; Muo, C.H.; Wang, W.C. Women with adenomyosis are at higher risks of endometrial and thyroid cancers: A population-based historical cohort study. PLoS ONE 2018, 13, e0194011. [Google Scholar] [CrossRef]
- Breintoft, K.; Pinnerup, R.; Henriksen, T.B.; Rytter, D.; Uldbjerg, N.; Forman, A.; Arendt, L.H. Endometriosis and Risk of Adverse Pregnancy Outcome: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 667. [Google Scholar] [CrossRef]
- Warzecha, D.; Pietrzak, B.; Szymusik, I.; Smiech, Z.; Wielgos, M. Should the patients with endometriosis be treated as a risk group of pregnancy complications? Single center experience and literature review and literature review. Ginekol. Pol. 2020, 91, 383–388. [Google Scholar] [CrossRef]
- Ahn, S.H.; Khalaj, K.; Young, S.L.; Lessey, B.A.; Koti, M.; Tayade, C. Immune-inflammation gene signatures in endometriosis patients. Fertil. Steril. 2016, 106, 1420–1431.e7. [Google Scholar] [CrossRef]
- Kitawaki, J.; Noguchi, T.; Amatsu, T.; Maeda, K.; Tsukamoto, K.; Yamamoto, T.; Fushiki, S.; Osawa, Y.; Honjo, H. Expression of aromatase cytochrome P450 protein and messenger ribonucleic acid in human endometriotic and adenomyotic tissues but not in normal endometrium. Biol. Reprod. 1997, 57, 514–519. [Google Scholar] [CrossRef]
- Bukulmez, O.; Hardy, D.B.; Carr, B.R.; Word, R.A.; Mendelson, C.R. Inflammatory status influences aromatase and steroid receptor expression in endometriosis. Endocrinology 2008, 149, 1190–1204. [Google Scholar] [CrossRef] [PubMed]
- Somkuti, S.G.; Yuan, L.; Fritz, M.A.; Lessey, B.A. Epidermal growth factor and sex steroids dynamically regulate a marker of endometrial receptivity in Ishikawa cells. J. Clin. Endocrinol. Metab. 1997, 82, 2192–2197. [Google Scholar] [CrossRef] [PubMed]
- Miller, P.B.; Parnell, B.A.; Bushnell, G.; Tallman, N.; Forstein, D.A.; Higdon, H.L., III; Kitawaki, J.; Lessey, B.A. Endometrial receptivity defects during IVF cycles with and without letrozole. Hum. Reprod. 2012, 27, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Franasiak, J.M.; Holoch, K.J.; Yuan, L.; Schammel, D.P.; Young, S.L.; Lessey, B.A. Prospective assessment of midsecretory endometrial leukemia inhibitor factor expression versus ανβ3 testing in women with unexplained infertility. Fertil. Steril. 2014, 101, 1724–1731. [Google Scholar] [CrossRef]
- Margarit, L.; Gonzalez, D.; Lewis, P.D.; Hopkins, L.; Davies, C.; Conlan, R.S.; Joels, L.; White, J.O. L-selectin ligands in human endometrium: Comparison of fertile and infertile subjects. Hum. Reprod. 2009, 24, 2767–2777. [Google Scholar] [CrossRef]
- Ahmed, A.; Ramma, W. Unravelling the theories of preeclampsia: Are the protective pathways the new paradigm? Br. J. Pharmacol. 2015, 172, 1574–1586. [Google Scholar] [CrossRef]
- Hirata, T.; Osuga, Y.; Takamura, M.; Saito, A.; Hasegawa, A.; Koga, K.; Yoshino, O.; Hirota, Y.; Harada, M.; Taketani, Y. Interleukin-17F increases the secretion of interleukin-8 and the expression of cyclooxygenase 2 in endometriosis. Fertil. Steril. 2011, 96, 113–117. [Google Scholar] [CrossRef]
- Yoo, J.Y.; Shin, H.; Kim, T.H.; Choi, W.S.; Ferguson, S.D.; Fazleabas, A.T.; Young, S.L.; Lessey, B.A.; Ha, U.-H.; Jeong, J.-W. CRISPLD2 is a target of progesterone receptor and its expression is decreased in women with endometriosis. PLoS ONE 2014, 9, e100481. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Lee, J.H.; Kim, M.; Chang, H.J.; Hwang, K.J.; Chang, K.H. Endometrium from women with endometriosis shows increased proliferation activity. Fertil. Steril. 2009, 92, 1246–1249. [Google Scholar] [CrossRef]
- Large, M.J.; DeMayo, F.J. The regulation of embryo implantation and endometrial decidualization by progesterone receptor signaling. Mol. Cell. Endocrinol. 2012, 358, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.; Elguero, S.; Thakore, S.; Dahoud, W.; Bedaiwy, M.; Mesiano, S. Role of nuclear progesterone receptor isoforms in uterine pathophysiology. Hum. Reprod. Update 2015, 21, 155–173. [Google Scholar] [CrossRef]
- Suda, K.; Nakaoka, H.; Yoshihara, K.; Ishiguro, T.; Tamura, R.; Mori, Y.; Yamawaki, K.; Adachi, S.; Takahashi, T.; Kase, H.; et al. Clonal expansion and diversification of cancer-associated mutations in endometriosis and Normal endometrium. Cell Rep. 2018, 24, 1777–1789. [Google Scholar] [CrossRef]
- Thakali, K.M.; Faske, J.B.; Ishwar, A.; Alfaro, M.P.; Cleves, M.A.; Badger, T.M.; Andres, A.; Shankar, K. Maternal obesity and gestational weight gain are modestly associated with umbilical cord DNA methylation. Placenta 2017, 57, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Anglesio, M.S.; Papadopoulos, N.; Ayhan, A.; Nazeran, T.M.; Noë, M.; Horlings, H.M.; Lum, A.; Jones, S.; Senz, J.; Seckin, T.; et al. Cancer-associated mutations in endometriosis without cancer. N. Engl. J. Med. 2017, 376, 1835–1848. [Google Scholar] [CrossRef]
- Li, Y.; Adur, M.K.; Kannan, A.; Davila, J.; Zhao, Y.; Nowak, R.A.; Bagchi, M.K.; Bagchi, I.C.; Li, Q. Progesterone alleviates endometriosis via inhibition of uterine cell proliferation, Inflammation and Angiogenesis in an Immunocompetent Mouse Model. PLoS ONE 2016, 11, e0165347. [Google Scholar] [CrossRef] [PubMed]
- Saare, M.; Modhukur, V.; Suhorutshenko, M.; Rajashekar, B.; Rekker, K.; Sõritsa, D.; Karro, H.; Soplepmann, P.; Sõritsa, A.; Lindgren, C.M.; et al. The influence of menstrual cycle and endometriosis on endometrial methylome. Clin. Epigenetics 2016, 8, 2. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.; Iwai, K.; Niiro, E.; Morioka, S.; Yamada, Y. Fetal programming theory: Implication for the understanding of endometriosis. Hum. Immunol. 2014, 75, 208–217. [Google Scholar] [CrossRef]
- Koike, N.; Higashiura, Y.; Akasaka, J.; Uekuri, C.; Ito, F.; Kobayashi, H. Epigenetic dysregulation of endometriosis susceptibility genes. Mol. Med. Rep. 2015, 12, 1611–1616. [Google Scholar] [CrossRef][Green Version]
- Kobayashi, H. Imprinting genes associated with endometriosis. EXCLI J. 2014, 13, 252–264. [Google Scholar]
- Kobayashi, H. Potential scenarios leading to ovarian cancer arising from endometriosis. Redox Rep. 2016, 21, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Ito, F.; Yamada, Y.; Shigemitsu, A.; Akinishi, M.; Kaniwa, H.; Miyake, R.; Yamanaka, S.; Kobayashi, H. Role of oxidative stress in epigenetic modification in endometriosis. Reprod. Sci. 2017, 24, 1493–1502. [Google Scholar] [CrossRef]
- Zadora, J.; Singh, M.; Herse, F.; Przybyl, L.; Haase, N.; Golic, M.; Yung, H.W.; Huppertz, B.; Cartwright, J.E.; Whitley, G.; et al. Disturbed placental imprinting in preeclampsia leads to altered expression of DLX5, a human-specific early Trophoblast marker. Circulation 2017, 136, 1824–1839. [Google Scholar] [CrossRef]
- Bellessort, B.; Le Cardinal, M.; Bachelot, A.; Narboux-Nême, N.; Garagnani, P.; Pirazzini, C.; Barbieri, O.; Mastracci, L.; Jonchere, V.; Duvernois-Berthet, E.; et al. Dlx5 and Dlx6 control uterine adenogenesis during postnatal maturation: Possible consequences for endometriosis. Hum. Mol. Genet. 2016, 25, 97–108. [Google Scholar] [CrossRef]
- Chen, P.; Wang, D.B.; Liang, Y.M. Evaluation of estrogen in endometriosis patients: Regulation of GATA-3 in endometrial cells and effects on Th2 cytokines. J. Obstet. Gynaecol. Res. 2016, 42, 669–677. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, A.; Neto, A.P.; Carvalho, F.; Ramalho, C.; Dória, S. Relevance of genomic imprinting in intrauterine human growth expression of CDKN1C, H19, IGF2, KCNQ1 and PHLDA2 imprinted genes. J. Assist. Reprod. Genet. 2014, 31, 1361–1368. [Google Scholar] [CrossRef]
- Burris, H.H.; Baccarelli, A.A.; Motta, V.; Byun, H.M.; Just, A.C.; Mercado-Garcia, A.; Schwartz, J.; Svensson, K.; Téllez-Rojo, M.M.; Wright, R.O. Association between length of gestation and cervical DNA methylation of PTGER2 and LINE 1-HS. Epigenetics 2014, 9, 1083–1091. [Google Scholar] [CrossRef] [PubMed]
- Kunz, G.; Beil, D.; Huppert, P.; Leyendecker, G. Structural abnormalities of the uterine wall in women with endometriosis and infertility visualized by vaginal sonography and magnetic resonance imaging. Hum. Reprod. 2000, 15, 76–82. [Google Scholar] [CrossRef]
- Brosens, I.; Derwig, I.; Brosens, J.; Fusi, L.; Benagiano, G.; Pijnenborg, R. The enigmatic uterine junctional zone:the missing link between reproductive disorders and major obstetrical disorders? Hum. Reprod. 2010, 25, 569–574. [Google Scholar] [CrossRef]
- Juang, C.M.; Chou, P.; Yen, M.S.; Twu, N.F.; Horng, H.C.; Hsu, W.L. Adenomyosis and risk of preterm delivery. Br. J. Obstet. Gynaecol. 2007, 114, 165–169. [Google Scholar] [CrossRef]
- Tanos, V.; Balami, S.; Lingwood, L. Junctional zone endometrium alterations in gynecological and obstetrical disorders and impact on diagnosis, prognosis and treatment. Curr. Opin. Obstet. Gynecol. 2019, 31, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Lazzarin, N.; Exacoustos, C.; Vaquero, E.; De Felice, G.; Manfellotto, D.; Zupi, E. Uterine junctional zone at threedimensional transvaginal ultrasonography in patients with recurrent miscarriage: A new diagnostic tool? Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 174, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Brosens, I.; Pijnenborg, R.; Benagiano, G. Defective myometrial spiral artery remodelling as a cause of major obstetrical syndromes in endometriosis and adenomyosis. Placenta 2013, 34, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, H.N.; Mitchell, B.F. Physiological pathways and molecular mechanisms regulating uterine contractility. Hum. Reprod. Update 2010, 16, 725–744. [Google Scholar] [CrossRef] [PubMed]
- Leone Roberti Maggiore, U.; Ferrero, S.; Mangili, G.; Bergamini, A.; Inversetti, A.; Giorgione, V.; Viganò, P.; Candiani, M. A systematic review on endometriosis during pregnancy: Diagnosis, misdiagnosis, complications and outcomes. Hum. Reprod. Update 2016, 22, 70–103. [Google Scholar] [CrossRef] [PubMed]
- Vercellini, P.; Parazzini, F.; Pietropaolo, G.; Cipriani, S.; Frattaruolo, M.P.; Fedele, L. Pregnancy outcome in women with peritoneal, ovarian and rectovaginal endometriosis: A retrospective cohort study. BJOG 2012, 119, 1538–1543. [Google Scholar] [CrossRef]
- Gasparri, M.L.; Nirgianakis, K.; Taghavi, K.; Papadia, A.; Mueller, M.D. Placenta previa and placental abruption after assisted reproductive technology in patients with endometriosis: A systematic review and meta-analysis. Arch. Gynecol. Obstet. 2018, 298, 27–34. [Google Scholar] [CrossRef]
- Fujii, T.; Wada-Hiraike, O.; Nagamatsu, T.; Harada, M.; Hirata, T.; Koga, K.; Fujii, T.; Osuga, Y. Assisted reproductive technology pregnancy complications are significantly associated with endometriosis severity before conception: A retrospective cohort study. Reprod. Biol. Endocrinol. 2016, 14, 73. [Google Scholar] [CrossRef]
- Lin, H.; Leng, J.H.; Liu, J.T.; Lang, J.H. Obstetric outcomes in Chinese women with endometriosis: A retrospective cohort study. Chin. Med. J. 2015, 128, 455–458. [Google Scholar] [CrossRef]
- Kmietowicz, Z. Endometriosis is linked to greater risk of complications in pregnancy and birth, study finds. BMJ 2015, 350, h3252. [Google Scholar] [CrossRef]
- Lalani, S.; Choudhry, A.J.; Firth, B.; Bacal, V.; Walker, M.; Wen, S.W.; Singh, S.; Amath, A.; Hodge, M.; Chen, I. Endometriosis and adverse maternal, fetal and neonatal outcomes, a systematic review and meta-analysis. Hum. Reprod. 2018, 33, 1854–1865. [Google Scholar] [CrossRef]
- Takemura, Y.; Osuga, Y.; Fujimoto, A.; Oi, N.; Tsutsumi, R.; Koizumi, M.; Yano, T.; Taketani, Y. Increased risk of placenta previa is associated with endometriosis and tubal factor infertility in assisted reproductive technology pregnancy. Gynecol. Endocrinol. 2013, 29, 113–115. [Google Scholar] [CrossRef]
- Vadillo-Ortega, F.; Estrada-Gutiérrez, G. Role of matrix metalloproteinases in preterm labour. BJOG 2005, 112, 19–22. [Google Scholar] [CrossRef] [PubMed]
- Rakhila, H.; Carli, C.; Daris, M.; Lemyre, M.; Leboeuf, M.; Akoum, A. Identification of multiple and distinct defects in prostaglandin biosynthetic pathways in eutopic and ectopic endometrium of women with endometriosis. Fertil. Steril 2013, 100, 1650–1659. [Google Scholar] [CrossRef] [PubMed]
- Conti, N.; Cevenini, G.; Vannuccini, S.; Orlandini, C.; Valensise, H.; Gervasi, M.T.; Ghezzi, F.; Di Tommaso, M.; Severi, F.M.; Petraglia, F. Women with endometriosis at first pregnancy have an increased risk of adverse obstetric outcome. J. Matern. Fetal Neonatal Med. 2015, 28, 1795–1798. [Google Scholar] [CrossRef]
- Berlac, J.F.; Hartwell, D.; Skovlund, C.W.; Langhoff-Roos, J.; Lidegaard, Ø. Endometriosis increases the risk of obstetrical and neonatal complications. Acta Obstet. Gynecol. Scand. 2017, 96, 751–760. [Google Scholar] [CrossRef] [PubMed]
- Stephansson, O.; Kieler, H.; Granath, F.; Falconer, H. Endometriosis, assisted reproduction technology, and risk of adverse pregnancy outcome. Hum. Reprod. 2009, 24, 2341–2347. [Google Scholar] [CrossRef]
- Kintiraki, E.; Papakatsika, S.; Kotronis, G.; Goulis, D.G.; Kotsis, V. Pregnancy-Induced hypertension. Hormones 2015, 14, 211–223. [Google Scholar] [CrossRef]
- Kortelahti, M.; Anttila, M.A.; Hippeläinen, M.I.; Heinonen, S.T. Obstetric outcome in women with endometriosis—A matched case control study. Gynecol. Obstet. Investig. 2003, 56, 207–212. [Google Scholar] [CrossRef]
- Hadfield, R.M.; Lain, S.J.; Raynes-Greenow, C.H.; Morris, J.M.; Roberts, C.L. Is there an association between endometriosis and the risk of preeclampsia? A population based study. Hum. Reprod. 2009, 24, 2348–2352. [Google Scholar] [CrossRef]
- Schmidt, P.; Skelly, C.L.; Raines, D.A. Placental Abruption. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Healy, D.L.; Breheny, S.; Halliday, J.; Jaques, A.; Rushford, D.; Garrett, C.; Talbot, J.M.; Baker, H.W. Prevalence and risk factors for obstetric haemorrhage in 6730 singleton births after assisted reproductive technology in Victoria Australia. Hum. Reprod. 2010, 25, 265–274. [Google Scholar] [CrossRef]
- Horton, J.; Sterrenburg, M.; Lane, S.; Maheshwari, A.; Li, T.C.; Cheong, Y. Reproductive, obstetric, and perinatal outcomes of women with adenomyosis and endometriosis: A systematic review and meta-analysis. Hum. Reprod. Update 2019, 25, 592–632. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, X.; Chen, Y.; Wang, J.; Zheng, W.; Cao, L. Miscarriage on Endometriosis and Adenomyosis in Women by Assisted Reproductive Technology or with Spontaneous Conception: A Systematic Review and Meta-Analysis. Biomed. Res. Int. 2020, 2020, 4381346. [Google Scholar] [CrossRef] [PubMed]
- Zullo, F.; Spagnolo, E.; Saccone, G.; Acunzo, M.; Xodo, S.; Ceccaroni, M.; Berghella, V. Endometriosis and obstetrics complications: A systematic review and meta-analysis. Fertil. Steril. 2017, 108, 667–672.e5. [Google Scholar] [CrossRef] [PubMed]
- Hjordt Hansen, M.V.; Dalsgaard, T.; Hartwell, D.; Skovlund, C.W.; Lidegaard, O. Reproductive prognosis in endometriosis. A national cohort study. Acta Obstet. Gynecol. Scand. 2014, 93, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Aris, A. A 12-year cohort study on adverse pregnancy outcomes in Eastern Townships of Canada: Impact of endometriosis. Gynecol. Endocrinol. 2014, 30, 34–37. [Google Scholar] [CrossRef] [PubMed]
- Alfadhli, E.M. Gestational diabetes mellitus. Saudi Med. J. 2015, 36, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Piechota, J.; Jelski, W. Intrahepatic Cholestasis in Pregnancy: Review of the Literature. J. Clin. Med. 2020, 9, 1361. [Google Scholar] [CrossRef]
- Pérez-López, F.R.; Martínez-Domínguez, S.J.; Viñas, A.; Pérez-Tambo, R.; Lafita, A.; Lajusticia, H.; Chedraui, P. Health Outcomes and Systematic Analyses (HOUSSAY) Project. Endometriosis and gestational diabetes mellitus risk: A systematic review and meta-analysis. Gynecol. Endocrinol. 2018, 34, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Osuchukwu, O.O.; Reed, D.J. Small for Gestational Age. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Vigano, P.; Corti, L.; Berlanda, N. Beyond infertility: Obstetrical and postpartum complications associated with endometriosis and adenomyosis. Fertil. Steril. 2015, 104, 802–812. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frincu, F.; Carp-Veliscu, A.; Petca, A.; Badiu, D.-C.; Bratila, E.; Cirstoiu, M.; Mehedintu, C. Maternal–Fetal Outcomes in Women with Endometriosis and Shared Pathogenic Mechanisms. Medicina 2021, 57, 1258. https://doi.org/10.3390/medicina57111258
Frincu F, Carp-Veliscu A, Petca A, Badiu D-C, Bratila E, Cirstoiu M, Mehedintu C. Maternal–Fetal Outcomes in Women with Endometriosis and Shared Pathogenic Mechanisms. Medicina. 2021; 57(11):1258. https://doi.org/10.3390/medicina57111258
Chicago/Turabian StyleFrincu, Francesca, Andreea Carp-Veliscu, Aida Petca, Dumitru-Cristinel Badiu, Elvira Bratila, Monica Cirstoiu, and Claudia Mehedintu. 2021. "Maternal–Fetal Outcomes in Women with Endometriosis and Shared Pathogenic Mechanisms" Medicina 57, no. 11: 1258. https://doi.org/10.3390/medicina57111258
APA StyleFrincu, F., Carp-Veliscu, A., Petca, A., Badiu, D.-C., Bratila, E., Cirstoiu, M., & Mehedintu, C. (2021). Maternal–Fetal Outcomes in Women with Endometriosis and Shared Pathogenic Mechanisms. Medicina, 57(11), 1258. https://doi.org/10.3390/medicina57111258





