Prognostic Value of the PROFUND Index for 30-Day Mortality in Acute Heart Failure
Abstract
:1. Introduction
2. Methodology
2.1. Design, Study Population, Variables, Data Collection and Analysis, and Ethical Aspects of the Study
2.1.1. Design and Study Population
2.1.2. Data Collection
2.1.3. Statistical Analysis
2.1.4. Ethical Aspects
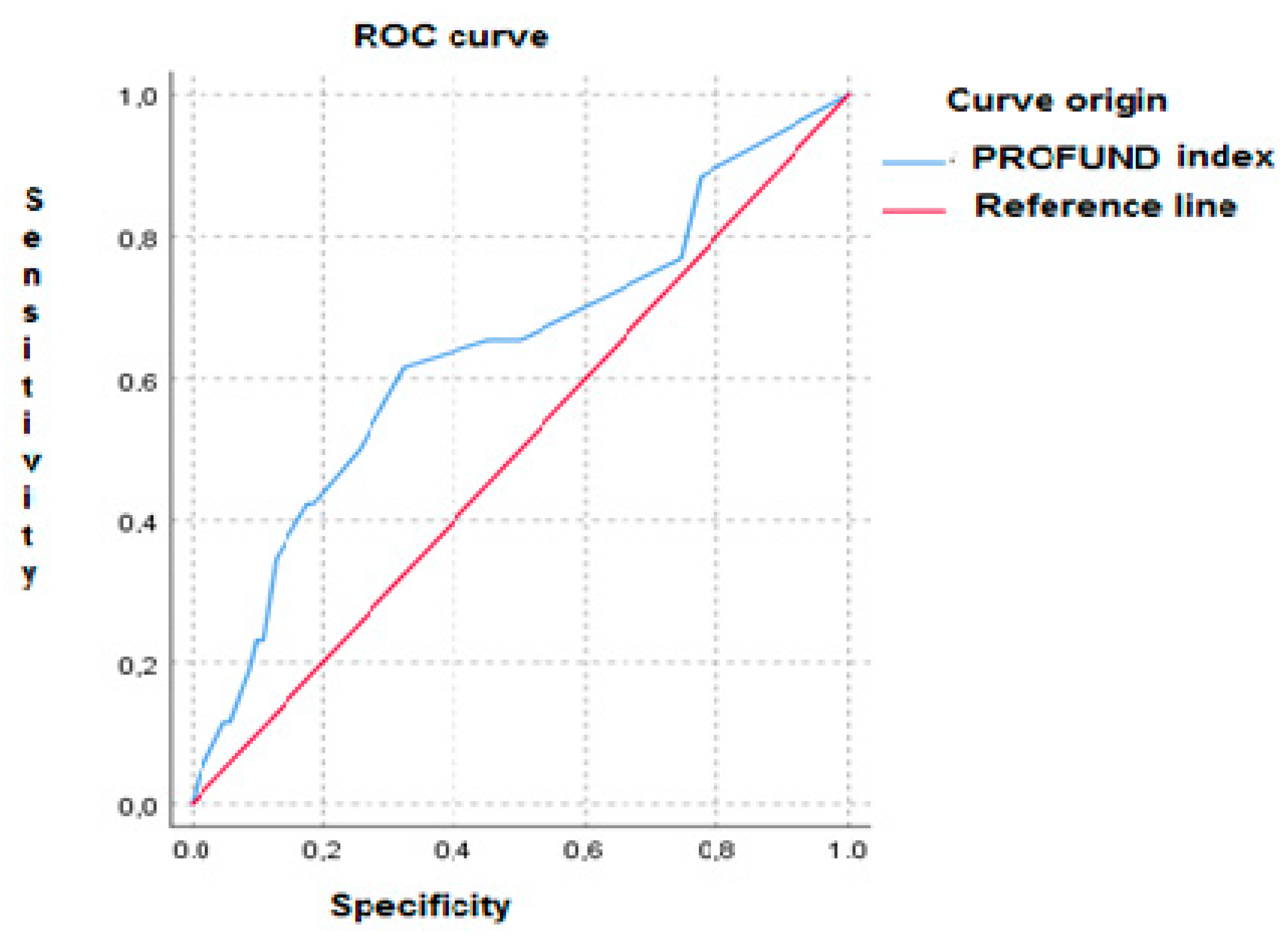
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Cortina, A.; Reguero, J.; Segovia, E.; Lambert, J.L.; Cortina, R.; Arias, J.C.; Vara, J.; Torre, F. Prevalence of heart failure in Asturias (a region in the North of Spain). Am. J. Cardiol. 2001, 87, 1417–1419. [Google Scholar] [CrossRef]
- Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillón, P. Situación epidemiológica de la insuficiencia cardiaca en España. Rev. Esp. Cardiol. Supl. 2006, 6, 4C–9C. [Google Scholar] [CrossRef]
- Fernández Gassó, M.L.; Hernando-Arizaleta, L.; Palomar-Rodríguez, J.A.; Soria-Arcos, F.; Pascual-Figal, D.A. Trends and characteristics of hospitalization for heart failure in a population setting from 2003 to 2013. Rev. Esp. Cardiol. 2017, 70, 720–726. [Google Scholar] [CrossRef] [PubMed]
- Dharmarajan, K. Comprehensive strategies to reduce readmissions in older patients with cardiovascular disease. Can. J. Cardiol. 2016, 32, 1306–1314. [Google Scholar] [CrossRef] [PubMed]
- Conde-Martel, A.; Hernández-Meneses, M. Prevalencia y significado pronóstico de la comorbilidad en la insuficiencia cardiaca. Rev. Clin. Esp. 2016, 216, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Formiga, F.; Chivite, D.; Conde, A.; Ruiz-Laiglesia, F.; Franco, Á.G.; Bocanegra, C.P.; Manzano, L.; Pérez-Barquero, M.M.; RICA Investigators. Basal functional status predicts three-month mortality after a heart failure hospitalization in elderly patients—The prospective RICA study. Int. J. Cardiol. 2014, 172, 127–131. [Google Scholar] [CrossRef] [PubMed]
- García-Morillo, J.S.; Bernabeu-Wittel, M.; Ollero-Baturone, M.; Aguilar-Guisad, M.; Ramírez-Duque, N.; de la Puente, M.A.; Limpo, P.; Romero-Carmona, S.; Cuello-Contreras, J.A. Incidencia y características clínicas de los pacientes con pluripatología ingresados en una unidad de medicina interna. Med. Clin. 2005, 125, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Bernabeu-Wittel, M.; Ollero-Baturone, M.; Moreno-Gaviño, L.; Barón-Franco, B.; Fuertes, A.; Murcia-Zaragoza, J.; Ramos-Cantos, C.; Alemán, A.; Fernández-Moyano, A. Development of a new predictive model for polypathological patients. The PROFUND index. Eur. J. Intern. Med. 2011, 22, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Bernabeu-Wittel, M.; Barón-Franco, B.; Nieto-Martín, D.; Moreno-Gaviño, L.; Ramírez-Duque, N.; Ollero-Baturone, M. Estratificación pronóstica y abordaje asistencial de los pacientes pluripatológicos. Rev. Clin. Esp. 2017, 217, 410–419. [Google Scholar] [CrossRef] [PubMed]
- Moretti, D.; Buncuga, M.G.; Laudanno, C.D.; Quiñones, N.D.; Scolari Pasinato, C.M.; Rossi, F.E. Índice PROFUND y mortalidad intrahospitalaria en pacientes pluripatológicos. Análisis post-hoc [PROFUND index and intrahospital mortality in plurypathological patients. A post-hoc analysis]. Medicina 2021, 81, 329–336. [Google Scholar] [PubMed]
- Bernabeu-Wittel, M.; Moreno-Gaviño, L.; Ollero-Baturone, M.; Barón-Franco, B.; Díez-Manglano, J.; Rivas-Cobas, C.; Murcia-Zaragoza, J.; Ramos-Cantos, C.; Fernández-Moyano, A. Validation of PROFUND prognostic index over a four-year follow-up period. Eur. J. Intern. Med. 2016, 36, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Moretti, D.; Buncuga, M.G.; Laudanno, C.D.; Quiñones, N.D.; Scolari Pasinato, C.M.; Rossi, F.E. Índice PROFUND y valoración global subjetiva. Valor pronóstico en pacientes pluripatológicos internados. Medicina 2020, 80, 622–632. [Google Scholar] [PubMed]
- López-Garrido, M.A.; Martín-Portugués, I.A.; Becerra-Muñoz, V.M.; Orellana-Figueroa, H.N.; Sánchez-Lora, F.J.; Morcillo-Hidalgo, L.; Jiménez-Navarro, M.F.; Gómez-Doblas, J.J.; de Teresa-Galván, E.; García-Pinilla, J.M. Prevalencia de pluripatología y valor pronóstico del índice PROFUND en una unidad de hospitalización de Cardiología. Rev. Clin. Esp. 2017, 217, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Colombo, P.B.; Nieto Martín, M.D.; Pascual de la Pisa, B.; José García Lozano, M.; Ángeles Ortiz Camúñez, M.; Wittel, M.B. Validación de un modelo pronóstico para pacientes pluripatológicos en atención primaria: Estudio PROFUND en atención primaria. Aten Primaria. 2014, 46, 41–48. [Google Scholar] [CrossRef] [Green Version]
- Ruiz-Laiglesia, F.J.; Sánchez-Marteles, M.; Pérez-Calvo, J.I.; Formiga, F.; Bartolomé-Satué, J.A.; Armengou-Arxé, A.; Lopez-Quiros, R.; Perez-Silvestre, J.; Serrado-Iglesias, A.; Montero-Pérez-Barquero, M. Comorbidity in heart failure. Results of the Spanish RICA Registry. QJM 2014, 107, 989–994. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| PROFUND Index | |
|---|---|
| VARIABLE | Points |
| Age ≥ 85 years | 3 |
Clinical features
| 6 3 3 3 |
| Hb < 10 g/dL | 3 |
Socio-familial features
| 4 2 |
| Variable | |
|---|---|
| Age | 80.5 +/− 9.98 years |
| Sex (female) | 66 (52%) |
| Comorbid Conditions | |
| Hypertension | 114 (90%) |
| Dyslipidemia | 97 (76%) |
| Atrial fibrillation | 82 (65%) |
| Chronic renal failure | 60 (47%) |
| Diabetes | 59 (46%) |
| Ischemic heart disease | 45 (43%) |
| Anemia (Hb < 10 g/dL) | 45 (35%) |
| COPD | 26 (20%) |
| Sleep apnea | 18 (14%) |
| Solid tumors | 9 (7%) |
| Cognitive impairment | 14 (11%) |
| Heart Failure Etiology | |
| Hypertensive | 53 (41%) |
| Ischemic | 40 (31%) |
| Valvular | 16 (12%) |
| Amyloidosis | 6 (5%) |
| Other | 13 (10%) |
| NYHA Functional Class | |
| Class I | 5 (4%) |
| Class II | 80 (62%) |
| Class III | 42 (33%) |
| Class IV | 1 (0.8%) |
| Left ventricular ejection fraction | |
| 40–49% | 23 (18%) |
| ≥50% | 78 (61%) |
| <40% | 27 (11%) |
| Functional status (Barthel) | 71.4+/− 27.83 |
| Laboratory Results upon Admission | |
| Hemoglobin | 11.8 +/− 1.9 g/dL |
| Serum creatinine | 1.4 +/− 0.7 mg/dL |
| Sodium | 139.6 +/− 4.7 mmol/L |
| Potassium | 4.3 +/− 0.6 mmol/L |
| NT-proBNP | 5815.5 pg/mL * |
| Treatment upon Admission | |
| Furosemide | 104 (85%) |
| Beta blockers | 74 (61%) |
| Angiotensin converting enzyme inhibitors | 35 (29%) |
| Mineralocorticoids | 34 (28%) |
| Angiotensin II receptor antagonist | 21 (17%) |
| Sacubutril-Valsartan | 8(6.6%) |
| SGTL-2 inhibitors | 8 (6.6%) |
| Cardiovascular cause of death | 8 (2%) |
| Variable | Expired (N = 26) | Survived (N = 102) | p |
|---|---|---|---|
| Age | 83.2 +/− 9.8 years | 79.8 +/− 9.9 years | 0.0119 |
| Sex (Males) | 21% | 79% | 0.516 |
| Left ventricular ejection fraction | 46.6 +/− 13.1% | 48.2 +/− 11.3% | 0.561 |
| Hemoglobin | 11.9 +/− 2.0 g/dL | 11.8 +/− 1.9 g/dL | 0.782 |
| Creatinine | 1.8 +/− 1.1 mg/dL | 1.3 +/− 0.6 mg/dL | 0.001 |
| NT-proBNP | 184500 +/− 3790 pg/mL | 7953 +/− 965 pg/mL | <0.001 |
| Sodium | 136.4 +/− 4.8 mmol/L | 140.4 +/− 4.3 mmol/L | <0.001 |
| PROFUND index | 7.2 +/− 5.1 | 4.7 +/− 4.2 | 0.001 |
| Variable | OR | CI95% | p |
|---|---|---|---|
| PROFUND index ≥ 9 points | 2.39 | 0.87–6.51 | 0.088 |
| NT-proBNP ≥ 14,000 pg/mL | 4.31 | 1.59–11.67 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Méndez-Bailón, M.; Iguarán-Bermúdez, R.; López-García, L.; Sánchez-Sauce, B.; Pérez-Mateos, P.; Barrado-Cuchillo, J.; Villar-Martínez, M.; Fernández-Castelao, S.; García-Klepzig, J.L.; Fuentes-Ferrer, M.E.; et al. Prognostic Value of the PROFUND Index for 30-Day Mortality in Acute Heart Failure. Medicina 2021, 57, 1150. https://doi.org/10.3390/medicina57111150
Méndez-Bailón M, Iguarán-Bermúdez R, López-García L, Sánchez-Sauce B, Pérez-Mateos P, Barrado-Cuchillo J, Villar-Martínez M, Fernández-Castelao S, García-Klepzig JL, Fuentes-Ferrer ME, et al. Prognostic Value of the PROFUND Index for 30-Day Mortality in Acute Heart Failure. Medicina. 2021; 57(11):1150. https://doi.org/10.3390/medicina57111150
Chicago/Turabian StyleMéndez-Bailón, Manuel, Rosario Iguarán-Bermúdez, Lidia López-García, Beatriz Sánchez-Sauce, Pablo Pérez-Mateos, Julia Barrado-Cuchillo, Miguel Villar-Martínez, Santiago Fernández-Castelao, Jose Luis García-Klepzig, Manuel Enrique Fuentes-Ferrer, and et al. 2021. "Prognostic Value of the PROFUND Index for 30-Day Mortality in Acute Heart Failure" Medicina 57, no. 11: 1150. https://doi.org/10.3390/medicina57111150
APA StyleMéndez-Bailón, M., Iguarán-Bermúdez, R., López-García, L., Sánchez-Sauce, B., Pérez-Mateos, P., Barrado-Cuchillo, J., Villar-Martínez, M., Fernández-Castelao, S., García-Klepzig, J. L., Fuentes-Ferrer, M. E., García-García, A., Vilacosta, I., de Miguel-Yanes, J. M., Casas-Rojo, J. M., Calvo-Manuel, E., Andres, E., Lorenzo-Villalba, N., & on behalf of the Heart Failure and Pluripathology Groups from the Spanish National Society of Internal Medicine. (2021). Prognostic Value of the PROFUND Index for 30-Day Mortality in Acute Heart Failure. Medicina, 57(11), 1150. https://doi.org/10.3390/medicina57111150







