Transvaginal Sonographic Evaluation of Cesarean Section Scar Niche in Pregnancy: A Prospective Longitudinal Study
Abstract
:1. Introduction
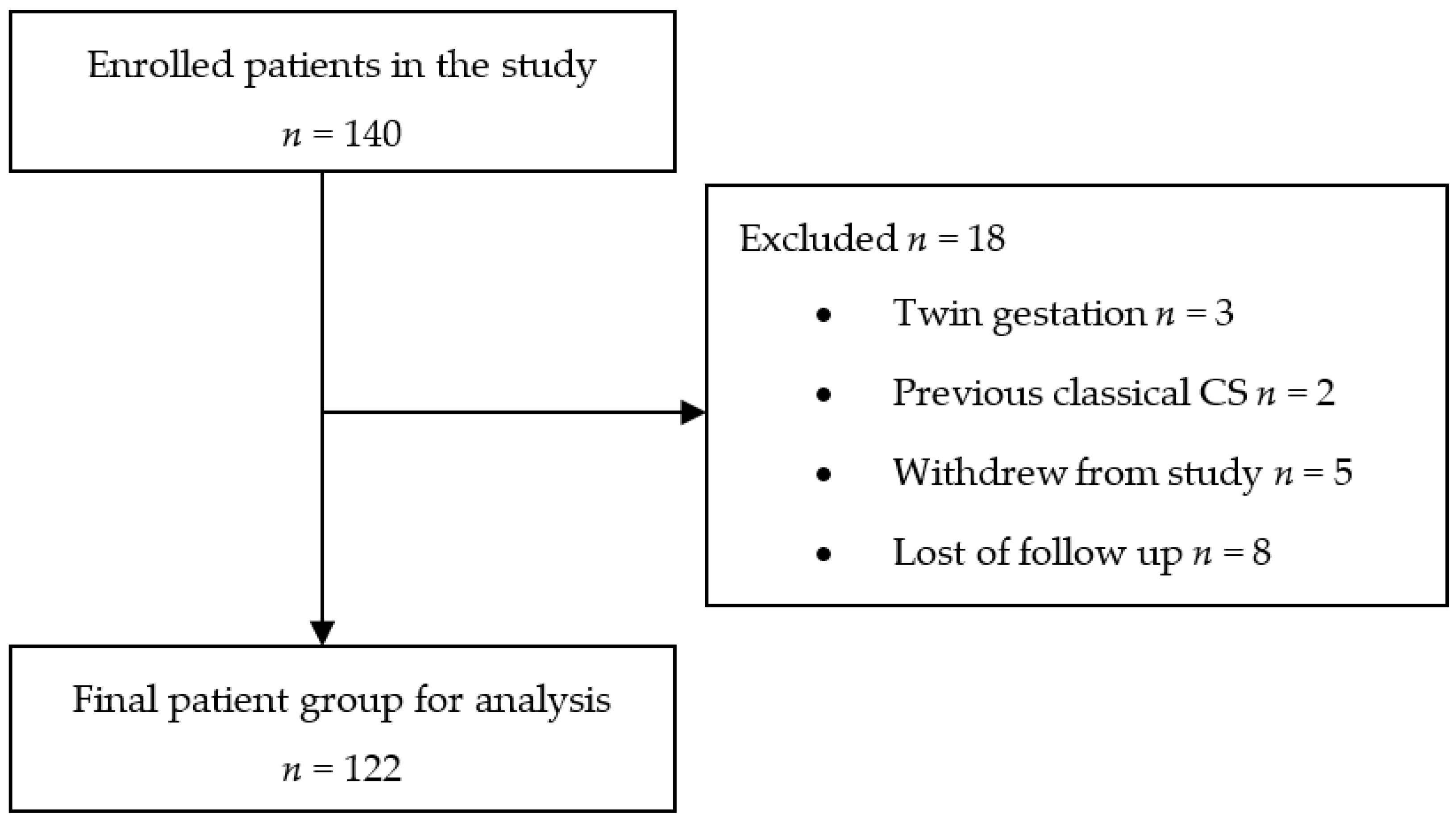
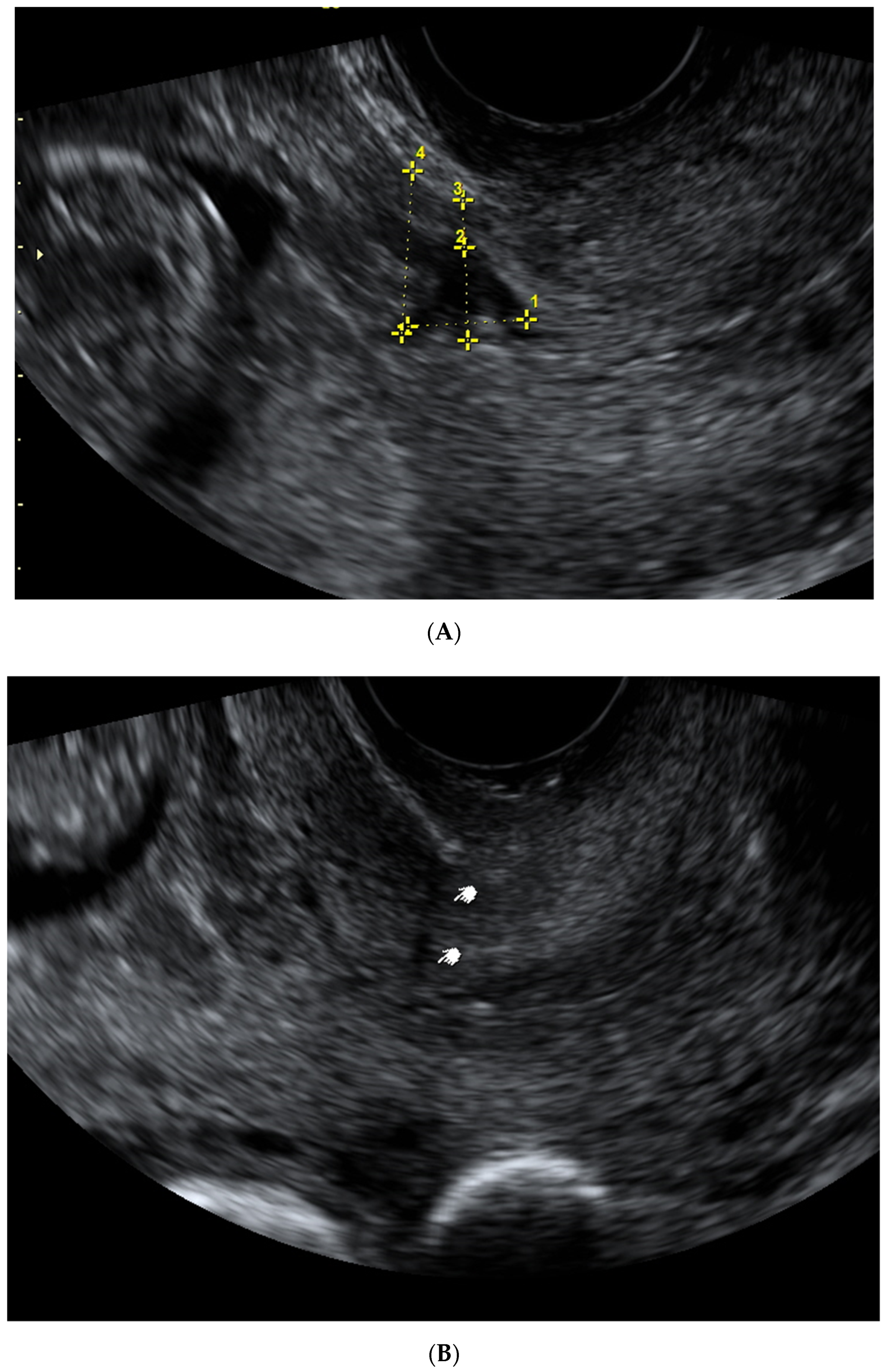
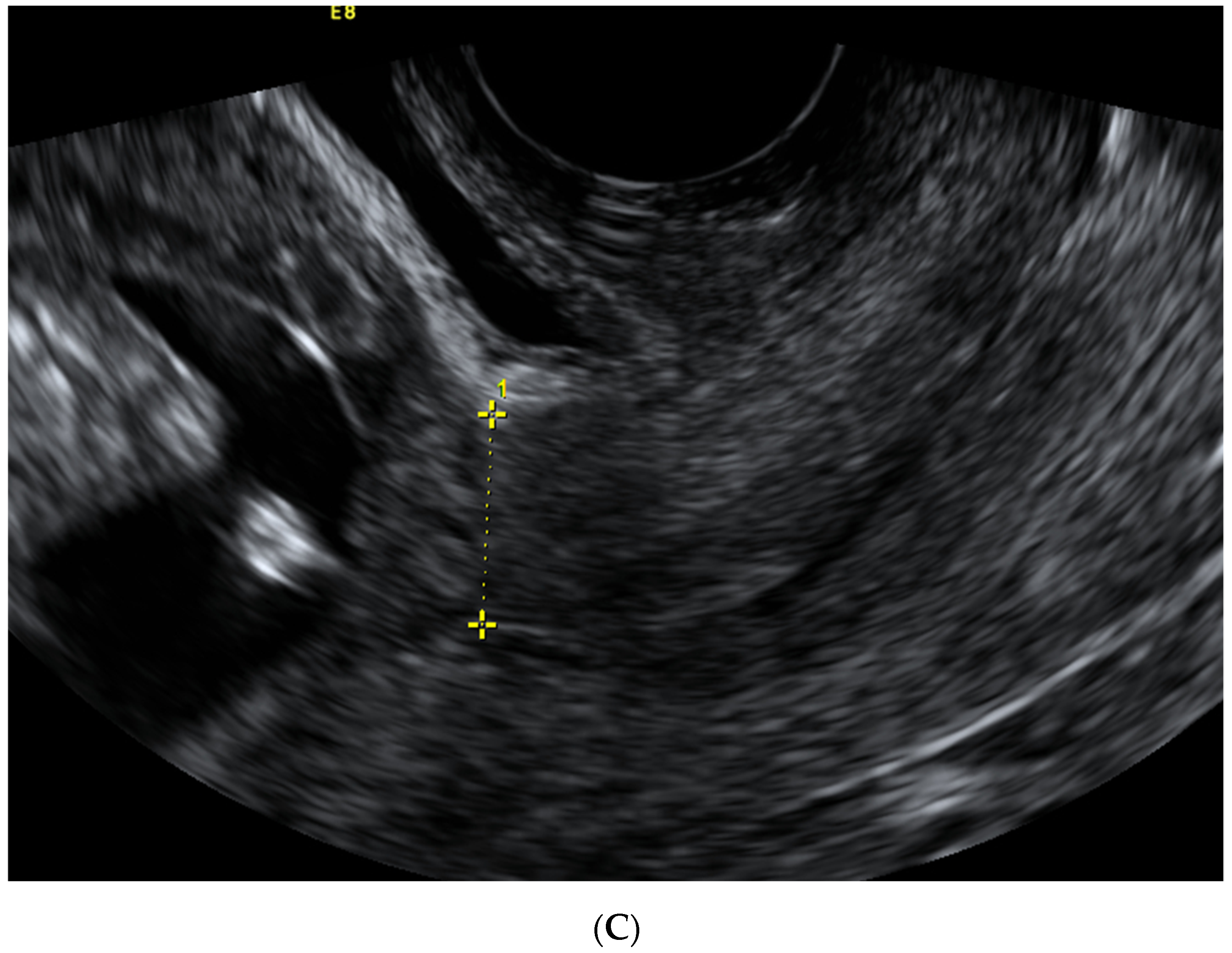
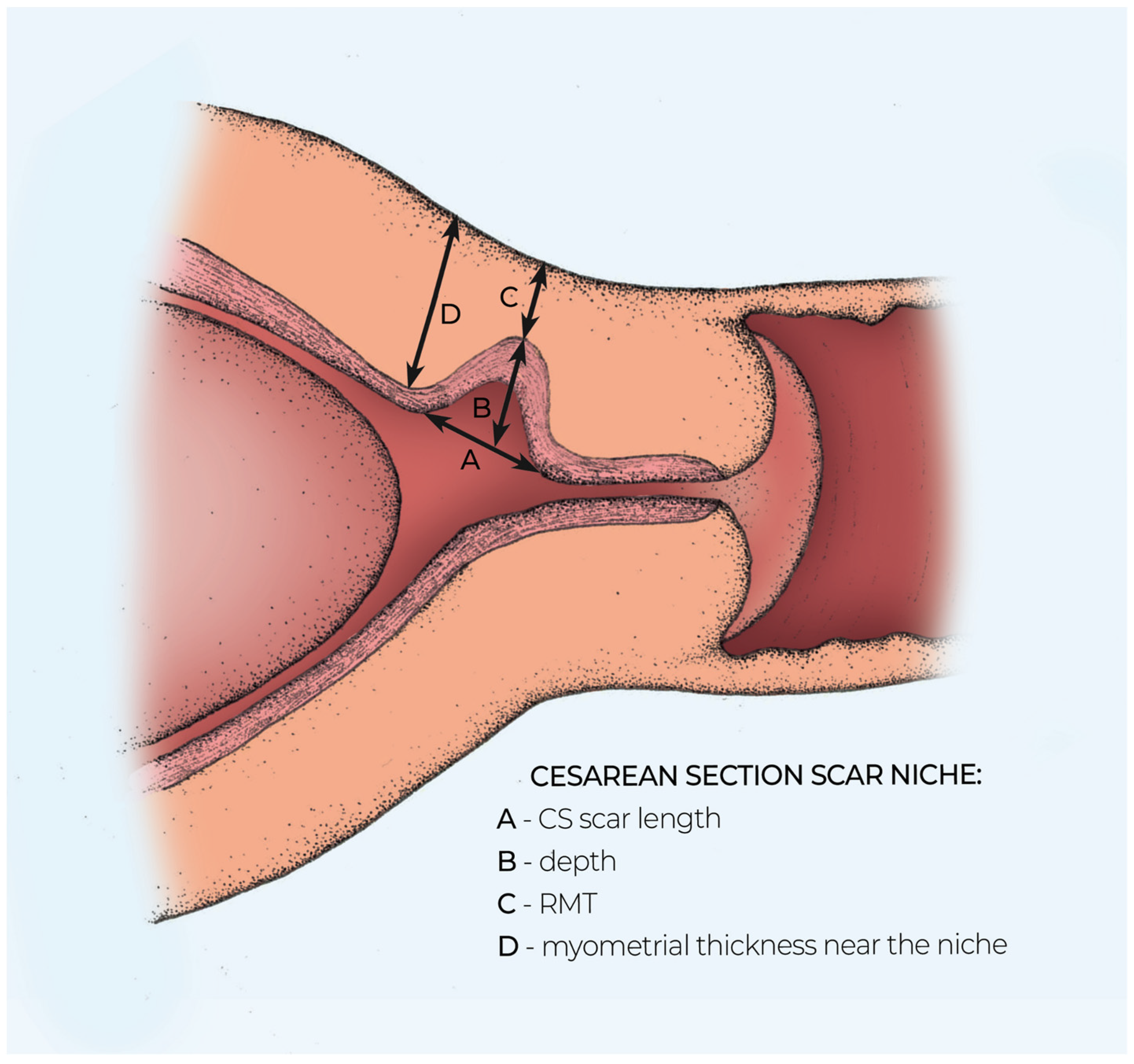
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- de Bij Vaate, A.J.; Brolmann, H.A.; van der Voet, L.F.; van der Slikke, J.W.; Veersema, S.; Huirne, J.A. Ultrasound evaluation of the Cesarean scar: Relation between a niche and postmenstrual spotting. Ultrasound Obstet. Gynecol. 2011, 37, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Ofili-Yebovi, D.; Ben-Nagi, J.; Sawyer, E.; Yazbek, J.; Lee, C.; Gonzalez, J.; Jurkovic, D. Deficient lower-segment Cesarean section scars: Prevalence and risk factors. Ultrasound Obstet. Gynecol. 2008, 31, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Vikhareva Osser, O.; Jokubkiene, L.; Valentin, L. Cesarean section scar defect: Agreement between transvaginal sonographic findings with and without saline contrast enhancement. Ultrasound Obstet. Gynecol. 2010, 35, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Stirnemann, J.J.; Chalouhi, G.E.; Forner, S.; Saidji, Y.; Salomon, L.J.; Bernard, J.P.; Ville, Y. First-trimester uterine scar assessment by transvaginal ultrasound. Am. J. Obstet. Gynecol. 2011, 205, 551.e1–551.e6. [Google Scholar] [CrossRef] [PubMed]
- Naji, O.; Abdallah, Y.; Bij de Vaate, A.; Smith, A.; Pexters, A.; Stalder, C.; McIndoe, A.; Ghaem-Maghami, S.; Lees, C.; Brolmann, H.A.; et al. Standardized approach for imaging and measuring Cesarean section scars using ultrasonography. Ultrasound Obstet. Gynecol. 2012, 39, 252–259. [Google Scholar] [CrossRef]
- Vervoort, A.J.; Uittenbogaard, L.B.; Hehenkamp, W.J.; Brölmann, H.A.; Mol, B.W.; Huirne, J.A. Why do niches develop in Caesarean uterine scars? Hypotheses on the aetiology of niche development. Hum. Reprod. 2015, 30, 2695–2702. [Google Scholar] [CrossRef]
- van der Voet, L.F.; Bij de Vaate, A.M.; Veersema, S.; Brolmann, H.A.M.; Huirne, J.A.F. Long term complications of cesarean section. The niche in the scar: A prospective cohort study on niche prevalence and its relation to abnormal uterine bleeding. BJOG Int. J. Obstet. Gynaecol. 2014, 121, 236–244. [Google Scholar] [CrossRef]
- Antila-Långsjö, R.M.; Mäenpää, J.U.; Huhtala, H.S.; Tomás, E.I.; Staff, S.M. Cesarean scar defect: A prospective study on risk factors. Am. J. Obstet. Gynecol. 2018, 219, 458.e1–458.e8. [Google Scholar] [CrossRef] [Green Version]
- Asakura, H.; Nakai, A.; Ishikawa, G.; Suzuki, S.; Araki, T. Prediction of uterine dehiscence by measuring lower uterine segment thickness prior to the onset of labor: Evaluation by transvaginal ultrasonography. J. Nippon Med. Sch. 2000, 67, 352–356. [Google Scholar] [CrossRef] [Green Version]
- Gotoh, H.; Masuzaki, H.; Yoshida, A.; Yoshimura, T.; Miyamura, T.; Ishimaru, T. Predicting incomplete uterine rupture with vaginal sonography during the late second trimester in women with prior cesarean. Obstet. Gynecol. 2000, 95, 596–600. [Google Scholar]
- Sen, S.; Malik, S.; Salhan, S. Ultrasonographic evaluation of lower uterine segment thickness in patients of previous cesarean section. Int. J. Gynaecol. Obstet. 2004, 87, 215–219. [Google Scholar] [CrossRef]
- Jastrow, N.; Chaillet, N.; Roberge, S.; Morency, A.M.; Lacasse, Y.; Bujold, E. Sonographic lower uterine segment thickness and risk of uterine scar defect: A systematic review. J. Obstet. Gynaecol. Can. 2010, 32, 321–327. [Google Scholar] [CrossRef]
- Naji, O.; Daemen, A.; Smith, A.; Abdallah, Y.; Saso, S.; Stalder, C.; Sayasneh, A.; McIndoe, A.; Ghaem-Maghami, S.; Timmerman, D.; et al. Visibility and measurement of Cesarean section scars in pregnancy: A reproducibility study. Ultrasound Obstet. Gynecol. 2012, 40, 549–556. [Google Scholar] [CrossRef] [Green Version]
- Jastrow, N.; Antonelli, E.; Robyr, R.; Irion, O.; Boulvan, M. Inter- and intraobserver variability in sonographic measurement of the lower uterine segment after a previous Cesarean section. Ultrasound Obstet. Gynecol. 2006, 27, 420–424. [Google Scholar] [CrossRef]
- Jastrow, N.; Vikhareva, O.; Gauthier, R.J.; Irion, O.; Boulvain, M.; Bujold, E. Can third-trimester assessment of uterine scar in women with prior Cesarean section predict uterine rupture? Ultrasound Obstet. Gynecol. 2016, 47, 410–414. [Google Scholar] [CrossRef] [Green Version]
- Baranov, A.; Salvesen, K.A.; Vikhreva Osser, O. Validation of prediction model for successful vaginal birth after Cesarean delivery based on sonographic assessment of hysterotomy scar. Ultrasound Obstet. Gynecol. 2018, 51, 189–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vikhareva Osser, O.; Jokubkiene, L.; Valentin, L. High prevalence of defects in Cesarean section scars at transvaginal ultrasound examination. Ultrasound Obstet. Gynecol. 2009, 34, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Vikhareva Osser, O.; Valentin, L. Risk factors for incomplete healing of the uterine incision after caesarean section. BJOG Int. J. Obstet. Gynaecol. 2010, 117, 1119–1126. [Google Scholar] [CrossRef] [PubMed]
- Naji, O.; Daemen, A.; Smith, A.; Abdallah, Y.; Saso, S.; Stalder, C.; Sayasneh, A.; McIndoe, A.; Ghaem-Maghami, S.; Timmerman, D.; et al. Changes in Cesarean section scar dimensions during pregnancy: A prospective longitudinal study. Ultrasound Obstet. Gynecol. 2013, 41, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Jordans, I.P.M.; de Leeuw, R.A.; Stegwee, S.I.; Amso, N.N.; Bari-Soldevila, P.N.; van den Bosch, T. Sonographic examination of uterine niche in non-pregnant women: A modified Delphi procedure. Ultrasound Obstet. Gynecol. 2019, 53, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Pomorski, M.; Fuchs, T.; Rosner-Tenerowicz, A.; Zimmer, M. Standardized ultrasonographic approach for the assessment of risk factors of incomplete healing of the cesarean scar in the uterus. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 205, 141–145. [Google Scholar] [CrossRef]
- Chen, Y.; Han, P.; Wang, Y.J.; Li, X.Y. Risk factors for incomplete healing of the uterine incision after cesarean section. Arch. Gynecol. Obstet. 2017, 296, 355–361. [Google Scholar] [CrossRef]
- Zhou, X.Y.; Li, H.; Fu, X.D. Identifying possible risk factors for cesarean scar pregnancy based on a retrospective study of 291 cases. J. Obstet. Gynecol. Res. 2020, 2, 272–278. [Google Scholar] [CrossRef]
- Armstrong, V.; Hansen, W.F.; Van Voothis, B.J.; Syrop, C.H. Detection of cesarean scars by transvaginal ultrasound. Obstet. Gynecol. 2003, 101, 61–65. [Google Scholar] [PubMed]
- Wang, C.B.; Chiu, W.W.C.; Lee, C.Y.; Sun, Y.L.; Lin, Y.H.; Tseng, C.J. Cesarean section number, defect size, clinical symptoms and uterine position. Ultrasound Obstet. Gynecol. 2009, 34, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Vikhareva Osser, O.; Valentin, L. Clinical importance of appearance of cesarean hysterotomy scar at transvaginal ultrasonography in nonpregnant women. Obstet. Gynecol. 2011, 117, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Stirnemann, J.J.; Mousty, E.; Chalouhi, G.; Salomon, L.J.; Bernard, J.P.; Ville, Y. Screening for placenta accreta at 11-14 weeks of gestation. Am. J. Obstet. Gynecol. 2011, 205, 547.e1–547.e6. [Google Scholar] [CrossRef] [PubMed]
- Paquette, K.; Markey, S.; Roberge, S.; Girard, M.; Bujold, E.; Demers, S. First and Third trimester uterine scar thickness in women with previous caesarean: A prospective comparative study. J. Obstet. Gynaecol. Can. (JOGC) 2019, 41, 59–63. [Google Scholar] [CrossRef]
| Characteristic | Median (IQR) or n (%) |
|---|---|
| Maternal age (years) | 34 (29–34) |
| BMI (kg/m2) | 25 (21–28) |
| Gestational diabetes | 15 (12.3) |
| Hypertension | 12 (9.8) |
| Smoking during pregnancy | 16 (13.1) |
| Previous uterine curettage | 32 (26.2) |
| Previous VBAC | 8 (6.6) |
| Previous postpartum infection | 5 (4.1) |
| Scar Characteristic (mm) | First Trimester Median (IQR) | Second Trimester Median (IQR) | Third Trimester Median (IQR) |
|---|---|---|---|
| CS scar niche length | 5.0 (3.9–7.0) | - | - |
| CS scar niche depth | 6.9 (4.8–9.7) | - | - |
| RMT | 4.7 (3.3–5,9) | - | - |
| Myometrial thickness in the isthmus uteri | 12.7 (10.8–14.5) | - | - |
| LUS thickness | - | 6.85 (5.2–9.1) | 4.0 (0.9–5.5) |
| Myometrial thickness | - | 3.85 (2.5–5.3) | 2.1 (1.7–2.7) |
| Scar Characteristic (mm) | First Trimester Mean ± SEM of Difference (95% LoA) | Second Trimester Mean ± SEM of Difference (95% LoA) | Third Trimester Mean ± SEM of Difference (95% LoA) |
|---|---|---|---|
| CS scar niche length | −0.300 ± 0.467 (+3.723 to 3.123) | - | - |
| CS scar depth | −0014 ± 0.211 (−1.565 to 1.536) | - | - |
| RMT | −0.114 ± 0.140 (−1.142 to 0.914) | - | - |
| Myometrial thickness in the isthmus uteri | −0.133 ± 0.169 (−1.761 to 1.494) | - | - |
| LUS thickness | - | −0.104 ± 0.169 (−1.725 to 1.517) | 0.021 ± 0.077 (−0.717 to 0.759) |
| Myometrial thickness | - | −0.083 ± 0.216 (−2.158 to 1.999) | 0.004 ± 0.036 (−0.340 to 0.348) |
| Percentage of Difference ≤ 1 mm | Intraclass Correlation Coefficient (95% CI) | |
|---|---|---|
| Intraobserver Agreement | ||
| CS scar niche length | 92.9 | 0.984 (0.95–0.995) |
| CS scar niche depth | 92.9 | 0.989 (0.968–0.997) |
| RMT | 100 | 0.991 (0.971–0.991) |
| Myometrial thickness at internal os | 83.3 | 0.96 (0.91–0.983) |
| LUS second trimester | 95.8 | 0.992 (0.982–0.997) |
| Myometrial thickness second trimester | 95.8 | 0.979 (0.953–0.991) |
| LUS third trimester | 91.7 | 0.914 (0.811–0.962) |
| Myometrial thickness third trimester | 91.6 | 0.906 (0.796–0.958) |
| Percentage of difference ≤ 1 mm | Intraclass correlation coefficient (95% CI) | |
| Interobserver Agreement | ||
| CS scar niche length | 85.7 | 0.758 (0.399–0.915) |
| CS scar niche depth | 85.7 | 0.972 (0.916–0.991) |
| RMT | 85.7 | 0.969 (0.906–0.995) |
| Myometrial thickness at internal os | 87.5 | 0.966 (0.924–0.985) |
| LUS second trimester | 87.5 | 0.967 (0.925–0.986) |
| Myometrial thickness second trimester | 91.7 | 0.854 (0.692–0.934) |
| LUS third trimester | 100 | 0.969 (0.929–0.986) |
| Myometrial thickness third trimester | 100 | 0.918 (0.824–0.964) |
| Finding | One CS Median (IQR) or n (%) | Two and More CS Median (IQR) or n (%) | p Value |
|---|---|---|---|
| Visible CS scar | 77 (81.1) | 18 (18.9) | 0.049 |
| Non-visible CS scar | 17 (63) | 10 (37) | 0.049 |
| CS scar niche | 41 (43.6) | 8 (28.5) | 0.228 |
| RMT | 4.8 (3.6–6.6) | 3.4 (1.9–5.3) | 0.09 |
| RMT ≤ 2 mm | 3 (60.0) | 2 (40.0) | 0.323 |
| Ratio (%) | 35.2 (25.7–51.34) | 31.2 (24.9–47.7) | 0.532 |
| ≤50 | 30 (73.2) | 6 (75) | 0.645 |
| LUS thickness in second trimester | 7.4 (5.4–9.5) | 6.0 (4.6–7.9) | 0.012 |
| Myometrial thickness in second trimester | 4.0 (2.77–5.4) | 2.5 (2.0–5.3) | 0.022 |
| LUS thickness in third trimester | 4.0 (2.7–5.4) | 4.1 (2.8–5.1) | 0.503 |
| Myometrial thickness in third trimester | 2.1 (1.6–2.8) | 2.3 (1.7–2.6) | 0.97 |
| Parameter | CS Scar Niche Median (IQR) or n (%) | Without CS Scar Niche Median (IQR) or n (%) | p Value |
|---|---|---|---|
| Age (years) | 34 (27.9–36.0) | 35 (26.0–37.0) | 0.486 |
| BMI (kg/m2) | 24.9 (21.6–28.5) | 25.5 (21.9–28.5) | 0.529 |
| Gestational diabetes | 6 (12.2) | 9 (12.3) | 1 |
| Smoker | 5 (10.4) | 11 (14.9) | 0.662 |
| Previous VBAC | 3 (6.25) | 5 (6.8) | 1 |
| Uterine curettage | 18 (56.3) | 31 (34.4) | 0.049 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savukyne, E.; Machtejeviene, E.; Paskauskas, S.; Ramoniene, G.; Nadisauskiene, R.J. Transvaginal Sonographic Evaluation of Cesarean Section Scar Niche in Pregnancy: A Prospective Longitudinal Study. Medicina 2021, 57, 1091. https://doi.org/10.3390/medicina57101091
Savukyne E, Machtejeviene E, Paskauskas S, Ramoniene G, Nadisauskiene RJ. Transvaginal Sonographic Evaluation of Cesarean Section Scar Niche in Pregnancy: A Prospective Longitudinal Study. Medicina. 2021; 57(10):1091. https://doi.org/10.3390/medicina57101091
Chicago/Turabian StyleSavukyne, Egle, Egle Machtejeviene, Saulius Paskauskas, Gitana Ramoniene, and Ruta Jolanta Nadisauskiene. 2021. "Transvaginal Sonographic Evaluation of Cesarean Section Scar Niche in Pregnancy: A Prospective Longitudinal Study" Medicina 57, no. 10: 1091. https://doi.org/10.3390/medicina57101091
APA StyleSavukyne, E., Machtejeviene, E., Paskauskas, S., Ramoniene, G., & Nadisauskiene, R. J. (2021). Transvaginal Sonographic Evaluation of Cesarean Section Scar Niche in Pregnancy: A Prospective Longitudinal Study. Medicina, 57(10), 1091. https://doi.org/10.3390/medicina57101091








