Possible Adrenal Involvement in Long COVID Syndrome
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021. [Google Scholar] [CrossRef]
- Ladds, E.; Rushforth, A.; Wieringa, S.; Taylor, S.; Rayner, C.; Husain, L.; Greenhalgh, T. Persistent symptoms after Covid-19: Qualitative study of 114 “long Covid” patients and draft quality principles for services. BMC Health Serv. Res. 2020, 20, 1144. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, M.; Nel, J.; Blumberg, L.; Madhi, S.A.; Dryden, M.; Stevens, W. Long-COVID: An evolving problem with an extensive impact. S. Afr. Med. J. 2020, 111, 10–12. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelma, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef] [PubMed]
- Martimbianco, A.L.C.; Pacheco, R.L.; Bagattini, A.M.; Riera, R. Frequency, signs and symptoms, and criteria adopted for long COVID-19: A systematic review. Int. J. Clin. Pract. 2021, e14357. [Google Scholar] [CrossRef]
- Khoo, B.; Tan, T.; Clarke, S.A.; Mills, E.G.; Patel, B.; Modi, M.; Phylactou, M.; Eng, P.C.; Thurston, L.; Alexander, E.C. Thyroid Function Before, During, and After COVID-19. J. Clin. Endocrinol. Metab. 2021, 106, e803–e811. [Google Scholar] [CrossRef] [PubMed]
- Pal, R.; Banerjee, M. COVID-19 and the endocrine system: Exploring the unexplored. J. Endocrinol. Investig. 2020, 43, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Lisco, G.; De Tullio, A.; Stragapede, A.; Solimando, A.G.; Albanese, F.; Capobianco, M.; Giagulli, V.A.; Guastamacchia, E.; de Pergola, G.; Vacca, A. COVID-19 and the Endocrine System: A Comprehensive Review on the Theme. J. Clin. Med. 2021, 10, 2920. [Google Scholar] [CrossRef] [PubMed]
- Piticchio, T.; Le Moli, R.; Tumino, D.; Frasca, F. Relationship between betacoronaviruses and the endocrine system: A new key to understand the COVID-19 pandemic—A comprehensive review. J. Endocrinol. Investig. 2021, 44, 1553–1570. [Google Scholar] [CrossRef] [PubMed]
- Brender, E.; Lynm, C.; Glass, R.M. JAMA patient page. Adrenal insufficiency. JAMA 2005, 294, 2528. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Naeije, R.; Caravita, S. Phenotyping long COVID. Eur. Respir. J. 2021, 58, 2101763. [Google Scholar] [CrossRef] [PubMed]
- Kamin, H.S.; Kertes, D.A. Cortisol and DHEA in development and psychopathology. Horm. Behav. 2017, 89, 69–85. [Google Scholar] [CrossRef] [PubMed]
- Nicolaides, N.C.; Pavlaki, A.N.; Maria Alexandra, M.A.; Chrousos, G.P. Glucocorticoid Therapy and Adrenal Suppression. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Boyce, A., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK279156/ (accessed on 19 October 2018).
- Broersen, L.H.; Pereira, A.M.; Jørgensen, J.O.; Dekkers, O.M. Adrenal Insufficiency in Corticosteroids Use: Systematic Review and Meta-Analysis. J. Clin. Endocrinol. Metab. 2015, 100, 2171–2180. [Google Scholar] [CrossRef] [PubMed]
- Inder, W.J.; Dimeski, G.; Russell, A. Measurement of salivary cortisol in 2012–laboratory techniques and clinical indications. Clin. Endocrinol. 2012, 77, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Langelaan, M.L.P.; Kisters, J.M.H.; Oosterwerff, M.M.; Boer, A.K. Salivary cortisol in the diagnosis of adrenal insufficiency: Cost efficient and patient friendly. Endocr. Connect. 2018, 7, 560–566. [Google Scholar] [CrossRef] [PubMed]
- Wheatland, R. Molecular mimicry of ACTH in SARS–implications for corticosteroid treatment and prophylaxis. Med. Hypotheses 2004, 63, 855–862. [Google Scholar] [CrossRef]
- Mao, Y.; Xu, B.; Guan, W.; Xu, D.; Li, F.; Ren, R.; Zhu, X.; Gao, Y.; Jiang, L. The Adrenal Cortex, an Underestimated Site of SARS-CoV-2 Infection. Front. Endocrinol. (Lausanne) 2021, 11, 593179. [Google Scholar] [CrossRef]
| Complete Blood Count | |||
|---|---|---|---|
| Analyte | Value | Units | Reference Range |
| Red blood cells (RBC) | 5.07 | 1012 cells/L | 4.0–5.4 |
| Hemoglobin (Hb) | 136 | g/L | 120–160 |
| Hematocrit (Hct) | 42.2 | % | 35–48 |
| MCV | 83.2 | fL | 78–95 |
| MCH | 26.9 | pg | 26–33 |
| MCHC | 323 | g/L | 320–360 |
| RDW | 14.4 | % | 11.0–15.5 |
| Reticulocytes | 1 | % | 0.5–2.5 |
| Platelets (PLT) | 339 | 109 cells/L | 130–400 |
| MPV | 7.6 | fL | 7.2–11.1 |
| PCT | 0.26 | % | 0.12–0.36 |
| PDW | 50.3 | % | 25.0–65.0 |
| White blood cells (WBC) | 9.28 | 109 cells/L | 4.8–10.8 |
| Neutrophils | 5.94 | 109 cells/L | 1.90–8.10 |
| Lymphocytes | 2.63 | 109 cells/L | 0.90–5.20 |
| Monocytes | 0.41 | 109 cells/L | 0.16–1.20 |
| Eosinophils | 0.19 | 109 cells/L | 0.00–0.80 |
| Basophils | 0.03 | 109 cells/L | 0.00–0.20 |
| LUC | 0.08 | 109 cells/L | 0.00–0.40 |
| Monocytes to Lymphocytes Ratio (MLR) | 0.156 | 0.105–0.403 | |
| Neutrophils to Lymphocytes Ratio (NLR) | 2.3 | 0.7–3.5 | |
| Platelets to Lymphocytes Ratio (PLR) | 128.9 | 76.5–251.4 | |
| Systemic Inflammation Index (SII) | 765.7 | 109 cells/L | 158–1028 |
| Iron metabolism | |||
| Iron | 21.3 | μmol/L | 5.0–30.4 |
| Ferritin | 64.0 | μmol/L | 33.7–337.1 |
| Transferrin | 31.3 | μmol/L | 25.1–50.3 |
| Total Iron Binding Capacity (TIBC) | 62.5 | μmol/L | 50.2–100.6 |
| Unsaturated Iron Binding Capacity (UIBC) | 41.2 | μmol/L | 21.0–84.0 |
| Transferrin saturation | 34.1 | % | 15–50 |
| Thyroid Function | |||
| TSH | 2.035 | mU/L | 0.45–4.5 |
| fT4 | 11.58 | pmol/L | 10–22 |
| fT3 | 5.01 | pmol/L | 2.8–6.5 |
| Liver Function | |||
| Fibrinogen | 3.9 | g/L | 1.5–4.5 |
| D-dimer | 349 | μg/L | 140–500 |
| Aspartate Aminotransferase (AST) | 22 | U/L | 6–34 |
| Alanine Aminotransferase (ALT) | 13 | U/L | 7–35 |
| γ-Glutamyl transferase (GGT) | 11 | U/L | 7–38 |
| AST/ALT | 1.7 | ≤1 | |
| GGT/ALT | 0.8 | ≤1 | |
| AST to Platelets Ratio Index (APRI) | 0.2 | ≤0.5 | |
| Inflammatory Markers | |||
| α2-Macroglobulin | 2.1 | g/L | 1.3–3.0 |
| C-reactive protein (CRP) | 5.5 | mg/L | ≤10 |
| Aptoglobin | 2.68 | g/L | 0.30–2.00 |
| Erythrocyte sedimentation rate (ESR) | 38 | mm | ≤20 |
| Uric acid | 2.97 | mmol/L | ≤1.78 |
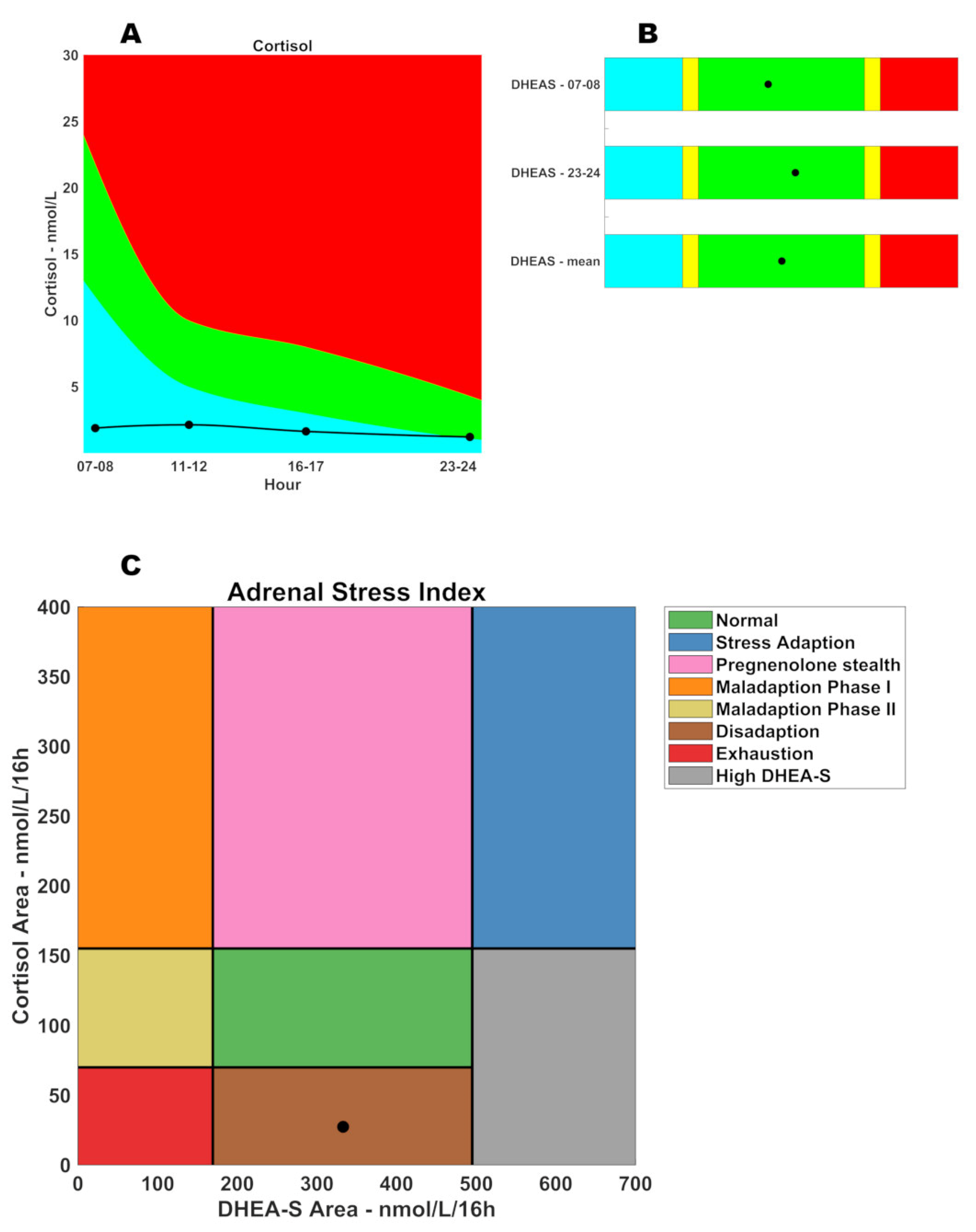
| SALIVARY CORTISOL | |||
|---|---|---|---|
| Hours | ng/mL | nmol/L | Range |
| 07:00–08:00 | 0.68 | 1.88 | 13–24 nmol/L |
| 11:00–12:00 | 0.77 | 2.12 | 5–10 nmol/L |
| 16:00–17:00 | 0.59 | 1.63 | 3–8 nmol/L |
| 23:00–24:00 | 0.44 | 1.21 | 1–4 nmol/L |
| Cortisol area | 27.3 | 70–155 nmol/L/16 h | |
| SALIVARY DHEA-S | |||
| Hours | ng/mL | nmol/L | Range |
| 07:00–08:00 | 7.15 | 19.40 | Sex: Female-Age: 38 |
| 23:00–24:00 | 8.18 | 22.20 | |
| Mean | 20.80 | 10.6–30.9 nmol/L | |
| DHEA-S area | 332.8 | 169–495 nmol/L/16 h | |
| DHEA-S–CORTISOL AREAS RATIO | |||
| Ratio | Range | ||
| 12.2 | 1.1–7.1 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salzano, C.; Saracino, G.; Cardillo, G. Possible Adrenal Involvement in Long COVID Syndrome. Medicina 2021, 57, 1087. https://doi.org/10.3390/medicina57101087
Salzano C, Saracino G, Cardillo G. Possible Adrenal Involvement in Long COVID Syndrome. Medicina. 2021; 57(10):1087. https://doi.org/10.3390/medicina57101087
Chicago/Turabian StyleSalzano, Ciro, Giovanna Saracino, and Giuseppe Cardillo. 2021. "Possible Adrenal Involvement in Long COVID Syndrome" Medicina 57, no. 10: 1087. https://doi.org/10.3390/medicina57101087
APA StyleSalzano, C., Saracino, G., & Cardillo, G. (2021). Possible Adrenal Involvement in Long COVID Syndrome. Medicina, 57(10), 1087. https://doi.org/10.3390/medicina57101087






