Effects of Prolonged Sitting with Slumped Posture on Trunk Muscular Fatigue in Adolescents with and without Chronic Lower Back Pain
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Protocol
2.3. Outcome Measurements
2.4. Data Analysis
3. Results
3.1. General Characteristics of Participants
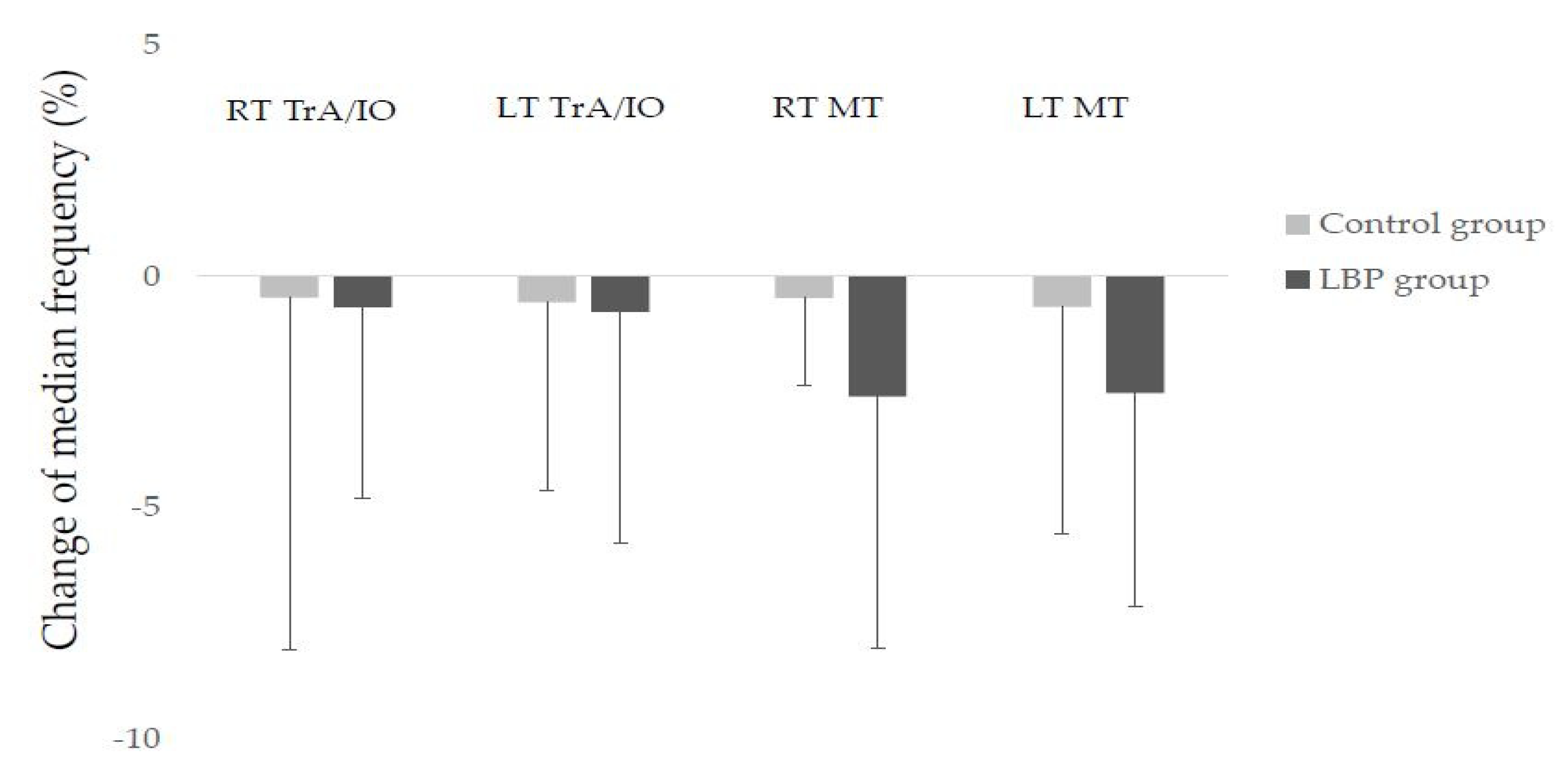
3.2. Comparison of Median Frequency
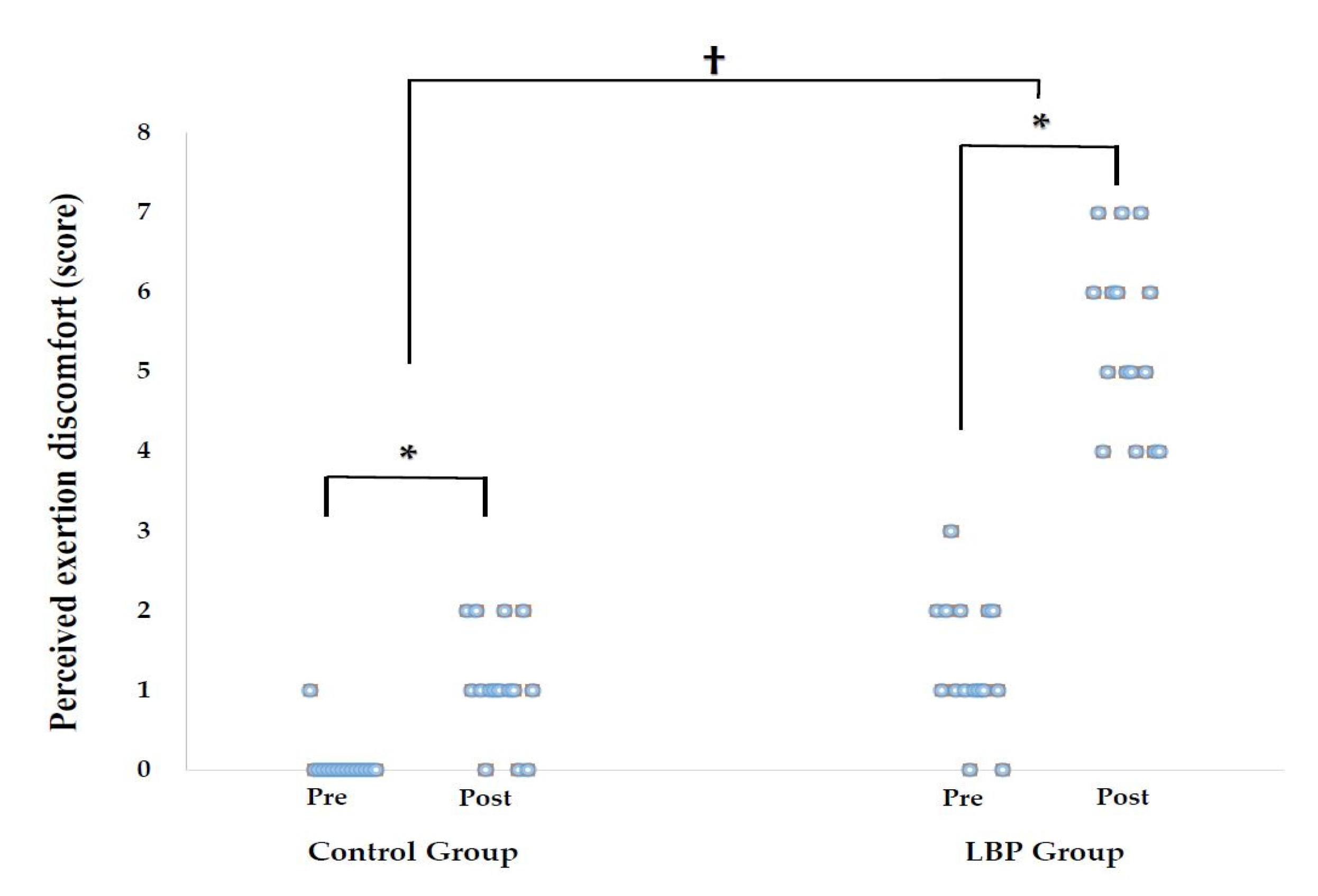
3.3. Comparison of Body Perceived Discomfort
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Waongenngarm, P.; Rajaratnam, B.S.; Janwantanakul, P. Perceived body discomfort and trunk muscle activity in three prolonged sitting postures. J. Phys. Ther. Sci. 2015, 27, 2183–2187. [Google Scholar] [CrossRef]
- Lis, A.; Black, K.; Korn, H.; Nordin, M. Association between sitting and occupational LBP. Eur. Spine. J. 2007, 16, 283–298. [Google Scholar] [CrossRef]
- Hamberg-van Reenen, H.H.; Ariëns, G.A.; Blatter, B.M.; Twisk, J.W.; van Mechelen, W.; Bongers, P.M. Physical capacity in relation to low back, neck, or shoulder pain in a working population. Occup. Environ. Med. 2006, 63, 371–377. [Google Scholar] [CrossRef]
- Heneweer, H.; Picavet, H.S.; Staes, F.; Kiers, H.; Vanhees, L. Physical fitness, rather than self-reported physical activities, is more strongly associated with low back pain: Evidence from a working population. Eur. Spine. J. 2012, 21, 1265–1272. [Google Scholar] [CrossRef]
- Ringheim, I.; Indahl, A.; Roeleveld, K. Reduced muscle activity variability in lumbar extensor muscles during sustained sitting in individuals with chronic low back pain. PLoS ONE 2019, 14, e0213778. [Google Scholar] [CrossRef]
- Abboud, J.; Nougarou, F.; Page, I.; Cantin, V.; Massicotte, D.; Descarreaux, M. Trunk motor variability in patients with non-specific chronic low back pain. Eur. J. Appl. Physiol. 2014, 114, 2645–2654. [Google Scholar] [CrossRef]
- Falla, D.; Gizzi, L.; Tschapek, M.; Erlenwein, J.; Petzke, F. Reduced task-induced variations in the distribution of activity across back muscle regions in individuals with low back pain. Pain 2014, 155, 944–953. [Google Scholar] [CrossRef]
- Biering-Sørensen, F. Physical measurements as risk indicators for low back trouble over a one year period. Spine 1984, 9, 106–119. [Google Scholar] [CrossRef]
- Jia, B.; Nussbaum, M.A. Influences of continuous sitting and psychosocial stress on low back kinematics, kinetics, discomfort, and localized muscle fatigue during unsupported sitting activities. Ergonomics 2018, 61, 1671–1684. [Google Scholar] [CrossRef]
- Kim, M.-S. Influence of neck pain on cervical movement in the sagittal plane during smartphone use. J. Phys. Ther. Sci. 2015, 27, 15–17. [Google Scholar] [CrossRef]
- Yassierli, Y.; Juraida, A. Effects of Netbook and Tablet Usage Postures on the Development of Fatigue, Discomfort and Pain. J. Eng. Technol. Sci. 2016, 48, 243–253. [Google Scholar] [CrossRef][Green Version]
- Roffey, D.M.; Wai, E.K.; Bishop, P.; Kwon, B.K.; Dagenais, S. Causal assessment of occupational standing or walking and low back pain: Results of a systematic review. Spine J. 2010, 10, 262–272. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Leboeuf, C.; Corder, E.H. Is sitting-while-at-work associated with low back pain? A systematic, critical literature review. Scand. J. Public Health 2000, 28, 230–239. [Google Scholar] [CrossRef]
- Waongenngarm, P.; Areerak, K.; Janwantanakul, P. The effects of breaks on low back pain, discomfort, and work productivity in office workers: A systematic review of randomized and non-randomized controlled trials. Appl. Ergon. 2018, 68, 230–239. [Google Scholar] [CrossRef]
- Dankaerts, W.; O′sullivan, P.; Burnett, A.; Straker, L. Differences in Sitting Postures are Associated with Nonspecific Chronic Low Back Pain Disorders When Patients Are Subclassified. Spine 2006, 31, 698–704. [Google Scholar] [CrossRef]
- Gupta, N.; Christiansen, C.S.; Hallman, D.M.; Korshøj, M.; Carneiro, I.G.; Holtermann, A. Is Objectively Measured Sitting Time Associated with Low Back Pain? A Cross-Sectional Investigation in the NOMAD study. PLoS ONE 2015, 10, e0121159. [Google Scholar] [CrossRef]
- Wong, A.Y.L.; Chan, T.P.M.; Chau, A.W.M.; Tung Cheung, H.; Kwan, K.C.K.; Lam, A.K.H.; Wong, P.Y.C.; De Carvalho, D. Do different sitting postures affect spinal biomechanics of asymptomatic individuals? Gait. Posture 2019, 67, 230–235. [Google Scholar] [CrossRef]
- O’Sullivan, P.B.; Dankaerts, W.; Burnett, A.F.; Farrell, G.T.; Jefford, E.; Naylor, C.S.; O’Sullivan, K.J. Effect of different upright sitting postures on spinalepelvic curvature and trunk muscle activation in a pain-free population. Spine 2006, 31, 707–712. [Google Scholar] [CrossRef]
- Reeve, A.; Dilley, A. Effects of posture on the thickness of transversus abdominis in pain-free subjects. Man. Ther. 2009, 14, 679–684. [Google Scholar] [CrossRef]
- Waongenngarm, P.; Rajaratnam, B.S.; Janwantanakul, P. Internal Oblique and Transversus Abdominis Muscle Fatigue Induced by Slumped Sitting Posture after 1 Hour of Sitting in Office Workers. Saf. Health Work 2016, 7, 49–54. [Google Scholar] [CrossRef]
- Asundi, K.; Odell, D.; Luce, A.; Dennerlein, J.T. Notebook computer use on a desk, lap and lap support: Effects on posture, performance and comfort. Ergonomics 2010, 53, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Gold, J.E.; Driban, J.B.; Yingling, V.R.; Komaroff, E. Characterization of posture and comfort in laptop users in non-desk settings. Appl. Ergon. 2012, 43, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Moffet, H.; Hagberg, M.; Hansson-Risberg, E.; Karlqvist, L. Influence of laptop computer design and working position on physical exposure variables. Clin. Biomech. 2002, 17, 368–375. [Google Scholar] [CrossRef]
- Borg, G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand. J. Work Environ. Health 1990, 16, 55–58. [Google Scholar] [CrossRef]
- Le, P.; Marras, W.S. Evaluating the low back biomechanics of three different office workstations: Seated, standing, and perching. Appl. Ergon. 2016, 56, 170–178. [Google Scholar] [CrossRef]
- Morl, F.; Bradl, I. Lumbar posture and muscular activity while sitting during office work. J. Electromyogr. Kinesiol. 2013, 23, 362–368. [Google Scholar] [CrossRef]
- Baker, R.; Coenen, P.; Howie, E.; Williamson, A.; Straker, L. The Short Term Musculoskeletal and Cognitive Effects of Prolonged Sitting During Office Computer Work. Int. J. Environ. Res. Public. Health 2018, 15, 1678. [Google Scholar] [CrossRef]
- Kavcic, N.; Grenier, S.; McGill, S.M. Determining the stabilizing role of individual torso muscles during rehabilitation exercises. Spine 2004, 29, 1254–1265. [Google Scholar] [CrossRef]
- Moretti, A.; Menna, F.; Aulicino, M.; Paoletta, M.; Liguori, S.; Iolascon, G. Characterization of Home Working Population during COVID-19 Emergency: A Cross-Sectional Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6284. [Google Scholar] [CrossRef]
- O’Sullivan, P.P.; Twomey, L.; Allison, G.T.; Sinclair, J.; Miller, K.; Knox, J. Altered patterns of abdominal muscle activation in patients with chronic low back pain. Aust. J. Physiother. 1997, 43, 91–98. [Google Scholar] [CrossRef]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Different ways to balance the spine in sitting: Muscle activity in specific postures differs between individuals with and without a history of back pain in sitting. Clin. Biomech. 2018, 52, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Floyd, W.F.; Silver, P.H.S. The function of the erector spinae muscle in certain movements and postures in man. J. Physiol. 1995, 129, 184–203. [Google Scholar] [CrossRef] [PubMed]
- Dankaerts, W.; O’Sullivan, P.; Burnett, A.; Straker, L. Altered Patterns of Superficial Trunk Muscle Activation During Sitting in Nonspecific Chronic Low Back Pain Patients. Spine 2006, 31, 2017–2023. [Google Scholar] [CrossRef] [PubMed]
- Falla, D.; Farina, D. Neuromuscular adaptation in experimental and clinical neck pain. J. Electromyogr. Kinesiol. 2008, 18, 255–261. [Google Scholar] [CrossRef]
- Coorevits, P.; Danneels, L.; Cambier, D.; Ramon, H.; Vanderstraeten, G. Assessment of the validity of the Biering-Sørensen test for measuring back muscle fatigue based on EMG median frequency characteristics of back and hip muscles. J. Electromyogr. Kinesiol. 2008, 18, 997–1005. [Google Scholar] [CrossRef]
- Søgaard, K.; Blangsted, A.K.; Jørgensen, L.V.; Madeleine, P.; Sjøgaard, G. Evidence of long term muscle fatigue following prolonged intermittent contractions based on mechano- and electromyograms. J. Electromyogr. Kinesiol. 2003, 13, 441–450. [Google Scholar] [CrossRef]
- van Dieën, J.H.; Westebring-van der Putten, E.P.; Kingma, I.; de Looze, M.P. Low-level activity of the trunk extensor muscles causes electromyographic manifestations of fatigue in absence of decreased oxygenation. J. Electromyogr. Kinesiol. 2009, 19, 98–406. [Google Scholar]
- Öberg, T.; Sandsjo, L.; Kadefors, R.; Larsson, S.E. Electromyographic changes in work-related myalgia of the trapezius muscle. Eur. J. Appl. Physiol. Occup. Physiol. 1992, 65, 251–257. [Google Scholar] [CrossRef]
- Öberg, T.; Sandsjo, L.; Kadefors, R. Subjective and objective evaluation of shoulder muscle fatigue. Ergonomics 1994, 37, 1323–1333. [Google Scholar] [CrossRef]
- Mork, P.J.; Westgaard, R.H. Long-term electromyographic activity in upper trapezius and low back muscles of women with moderate physical activity. J. Appl. Physiol. 2005, 99, 570–578. [Google Scholar] [CrossRef]
- van Dieen, J.H.; De Looze, M.P.; Hermans, V. Effects of dynamic office chairs on trunk kinematics, trunk extensor EMG and spinal shrinkage. Ergonomics 2001, 44, 739–750. [Google Scholar] [CrossRef] [PubMed]
- Astfalck, R.G.; O’Sullivan, P.B.; Straker, L.M.; Smith, A.J.; Burnett, A.; Caneiro, J.P.; Dankaerts, W. Sitting postures and trunk muscle activity in adolescents with and without nonspecific chronic low back pain: An analysis based on subclassification. Spine 2010, 35, 1387–1395. [Google Scholar] [CrossRef] [PubMed]
- Dunk, N.M.; Kedgley, A.E.; Jenkyn, T.R.; Callaghan, J.P. Evidence of a pelvis-driven flexion pattern: Are the joints of the lower lumbar spine fully flexed in seated postures? Clin. Biomech. 2009, 24, 164–168. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, P.B.; Dankaerts, W.; Burnett, A.; Chen, D.; Booth, R.; Carlsen, C.; Schultz, A. Evaluation of the Flexion Relaxation Phenomenon of the Trunk Muscles in Sitting. Spine 2006, 31, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
| Variables | LBP Group (n = 15) | Control Group (n = 15) | p |
|---|---|---|---|
| Sex (Male/Female) | 11/4 | 10/5 | 0.690 a |
| Age (years) | 17.40 ± 2.85 | 17.53 ± 2.47 | 0.381 b |
| Height (cm) | 171.87 ± 5.96 | 168.53 ± 8.94 | 0.239 b |
| Weight (kg) | 68.87 ± 10.58 | 66.20 ± 13.02 | 0.543 b |
| Postures that make symptoms worse (lumbar flexion/extension) | (13/2) |
| Control Group | Difference | LBP Group | Difference | p | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||
| RT IO | 100 ± 0.00 | 99.54 ± 7.60 | −0.46 ± 7.60 | 100 ± 0.00 | 99.33 ± 4.13 | −0.67 ± 4.13 | 0.927 |
| LT IO | 100 ± 0.00 | 99.44 ± 4.07 | −0.56 ± 4.07 | 100 ± 0.00 | 99.23 ± 5.01 | −0.77 ± 5.01 | 0.898 |
| RT MT | 100 ± 0.00 | 99.53 ± 1.88 | −0.47 ± 1.88 | 100 ± 0.00 | 97.40 ± 5.42 | −2.60 ± 5.42 | 0.161 |
| LT MT | 100 ± 0.00 | 99.34 ± 4.91 | −0.66 ± 4.91 | 100 ± 0.00 | 97.48 ± 4.61 | −2.52 ± 4.61 | 0.293 |
| Control Group | Difference | LBP Group | Difference | p | |||
|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||
| Disability | 0.07 ± 0.26 | 1.07 ± 0.70 | 1.00 ± 0.65 * | 1.33 ± 0.82 | 5.40 ± 1.12 | 4.07 ± 1.33 * | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, K.-S.; Jung, J.-H.; In, T.-S.; Cho, H.-Y. Effects of Prolonged Sitting with Slumped Posture on Trunk Muscular Fatigue in Adolescents with and without Chronic Lower Back Pain. Medicina 2021, 57, 3. https://doi.org/10.3390/medicina57010003
Jung K-S, Jung J-H, In T-S, Cho H-Y. Effects of Prolonged Sitting with Slumped Posture on Trunk Muscular Fatigue in Adolescents with and without Chronic Lower Back Pain. Medicina. 2021; 57(1):3. https://doi.org/10.3390/medicina57010003
Chicago/Turabian StyleJung, Kyoung-Sim, Jin-Hwa Jung, Tae-Sung In, and Hwi-Young Cho. 2021. "Effects of Prolonged Sitting with Slumped Posture on Trunk Muscular Fatigue in Adolescents with and without Chronic Lower Back Pain" Medicina 57, no. 1: 3. https://doi.org/10.3390/medicina57010003
APA StyleJung, K.-S., Jung, J.-H., In, T.-S., & Cho, H.-Y. (2021). Effects of Prolonged Sitting with Slumped Posture on Trunk Muscular Fatigue in Adolescents with and without Chronic Lower Back Pain. Medicina, 57(1), 3. https://doi.org/10.3390/medicina57010003







