Effectiveness of Percutaneous Nephrolithotomy, Retrograde Intrarenal Surgery, and Extracorporeal Shock Wave Lithotripsy for Treatment of Renal Stones: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Search Strategy
2.3. Study Selection and Data Extraction
2.4. Quality Assessment
2.5. Heterogeneity Tests
2.6. Statistical Analysis
3. Results
3.1. Characteristics of Included Studies
3.2. Quality Assessment and Publication Bias
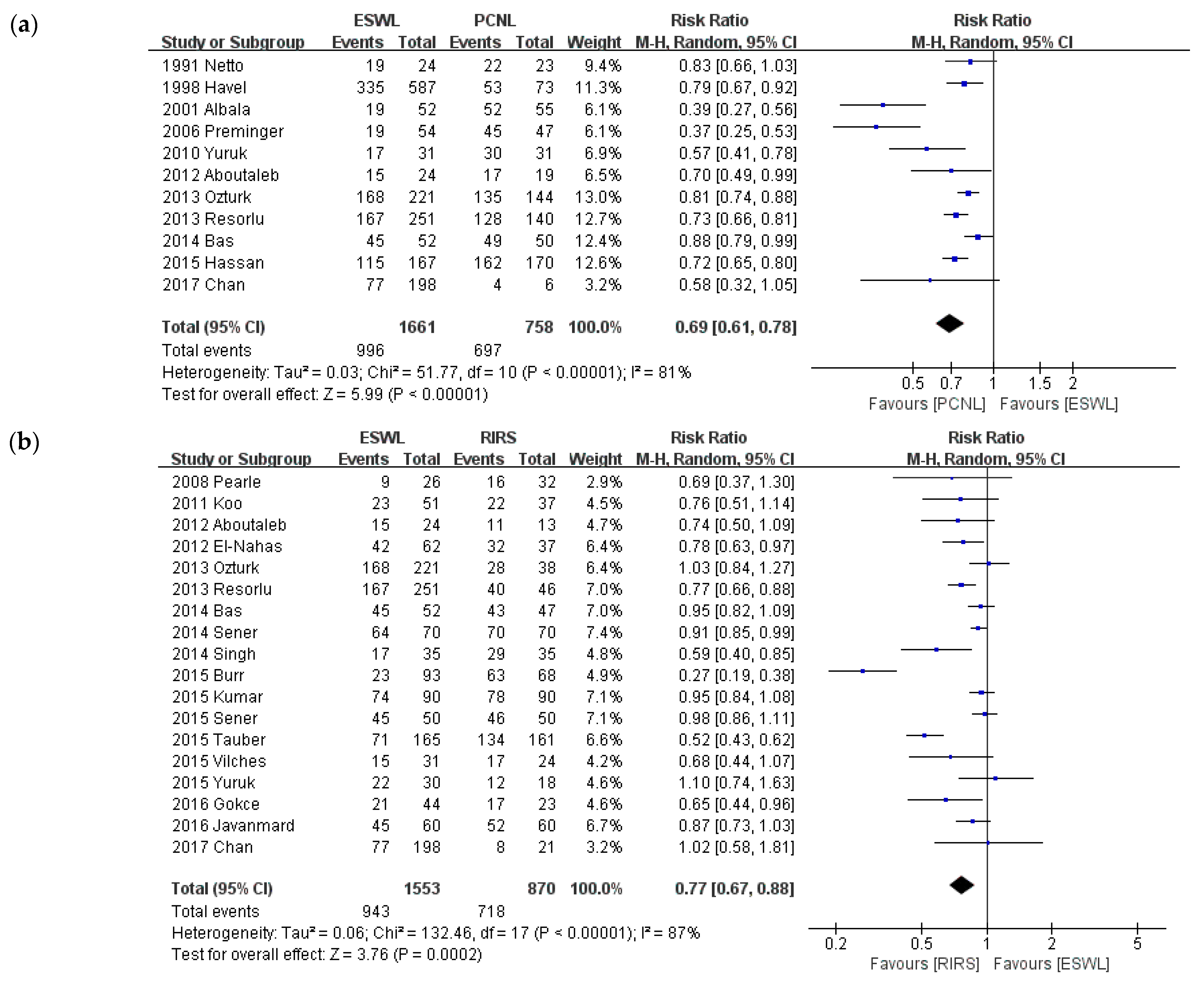
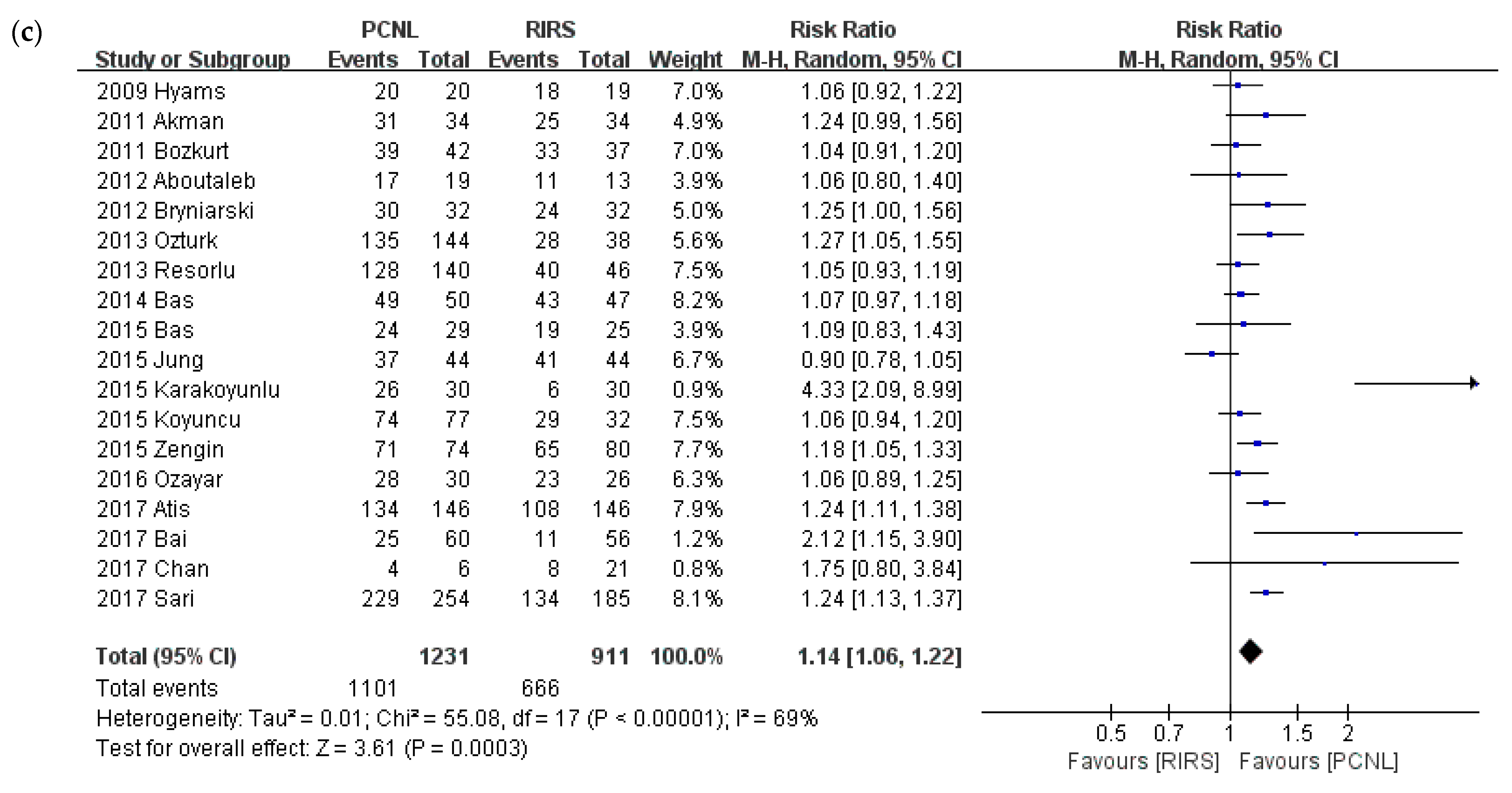
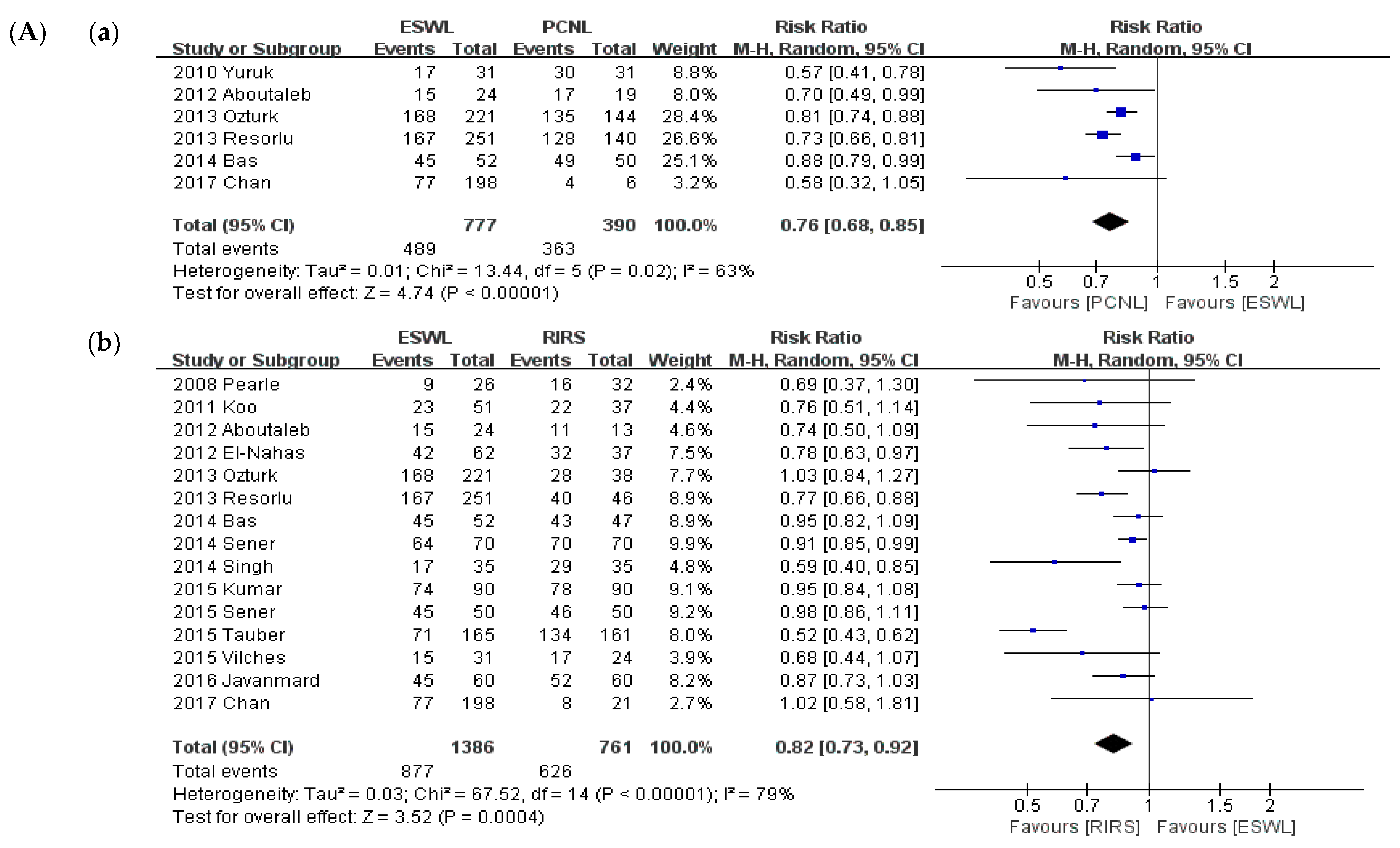
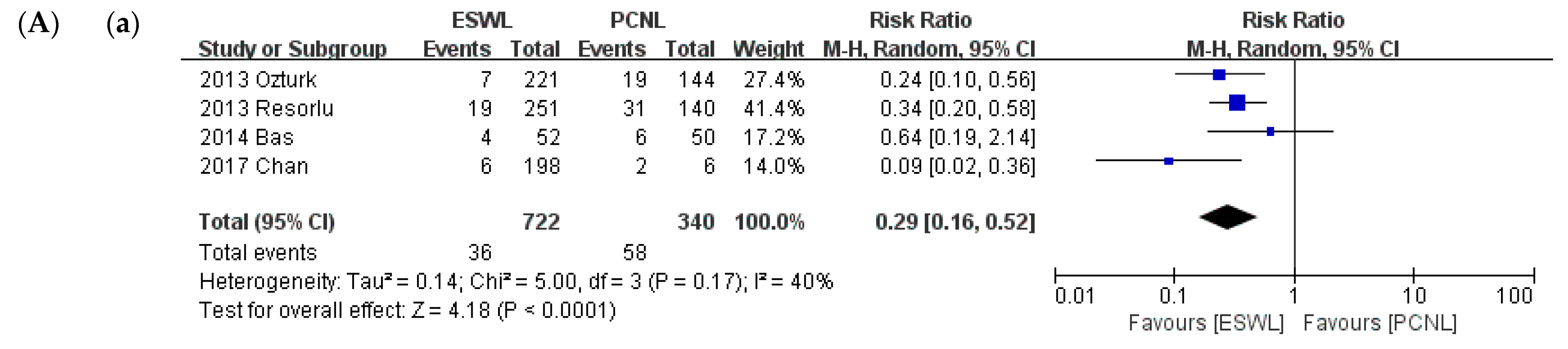
3.3. Stone-Free Rate
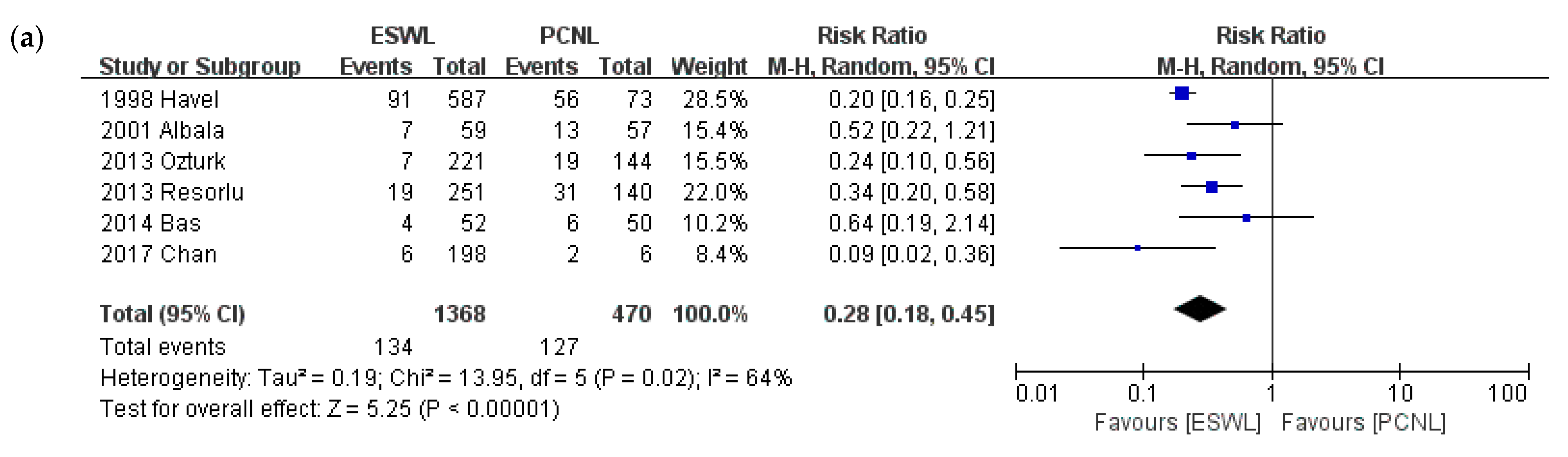
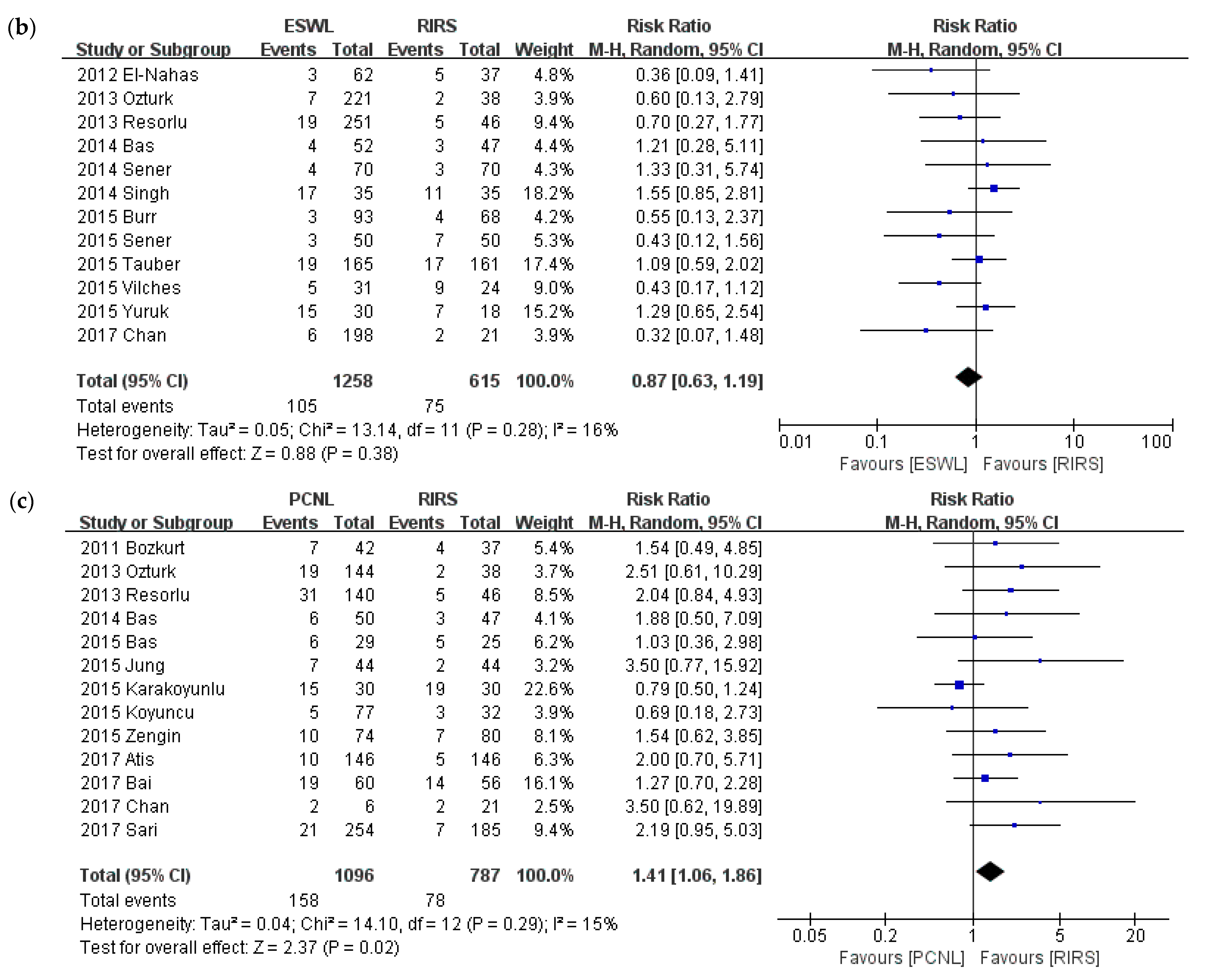
3.4. Total Complications
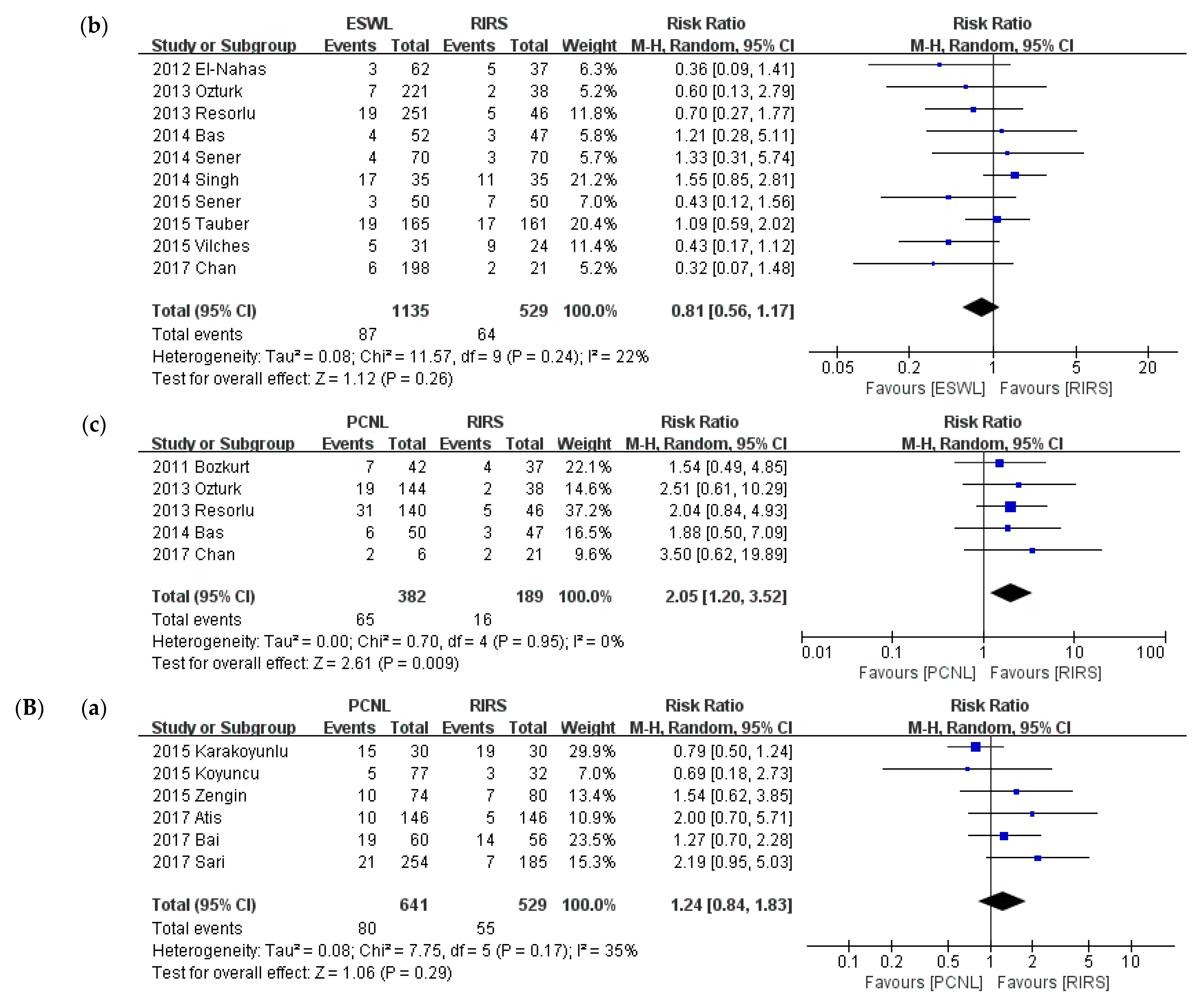
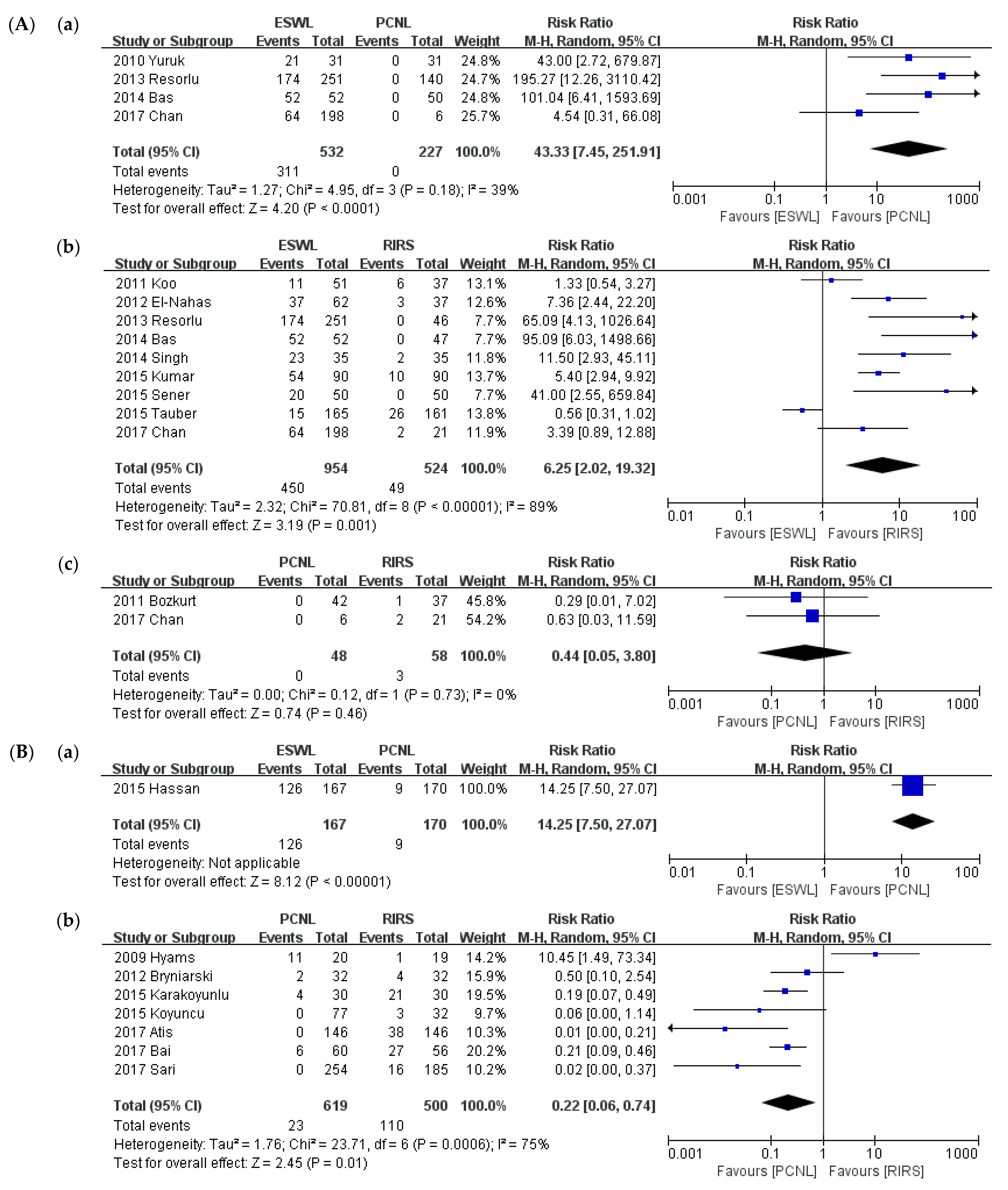
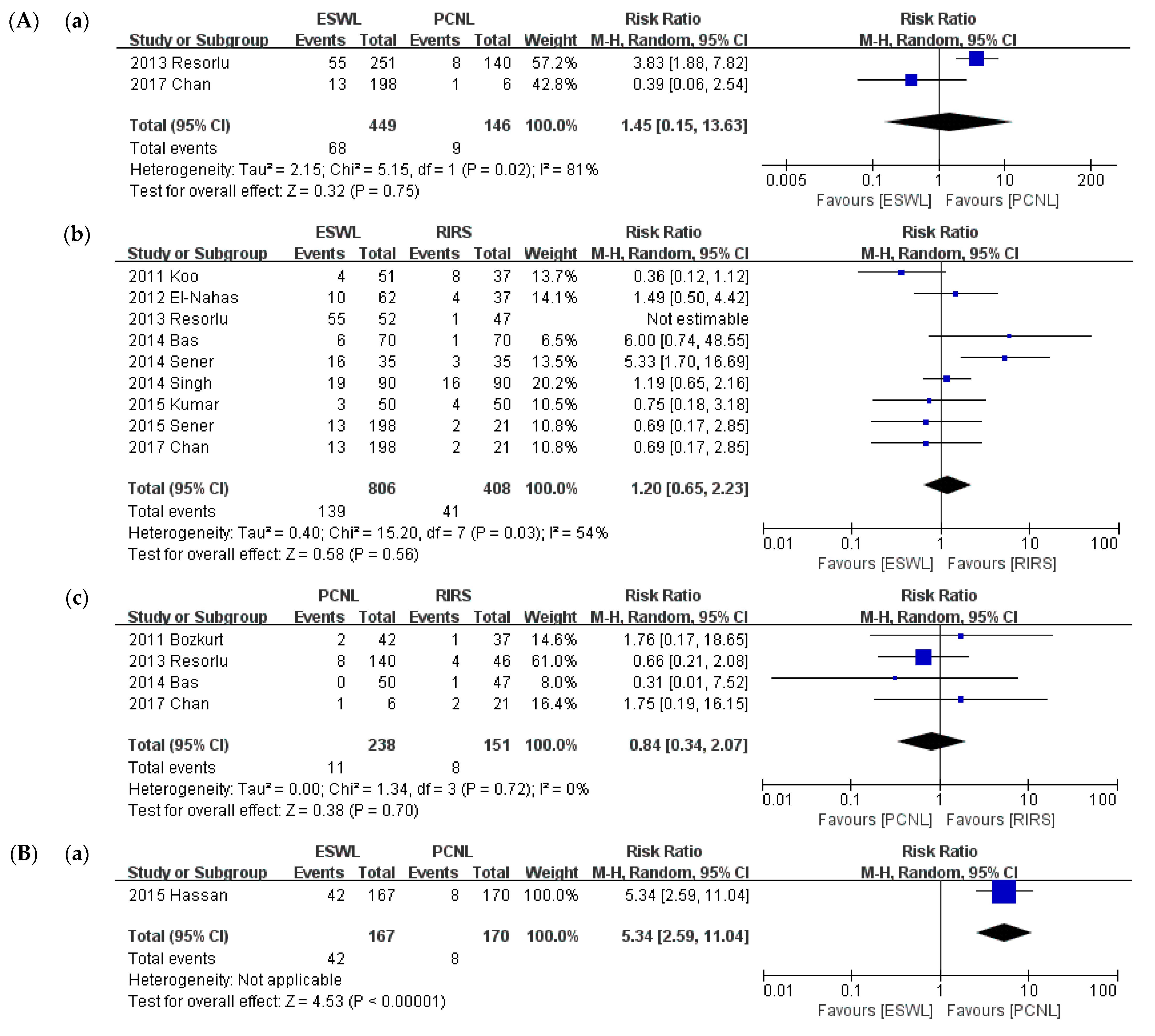
3.5. Retreatment Procedure
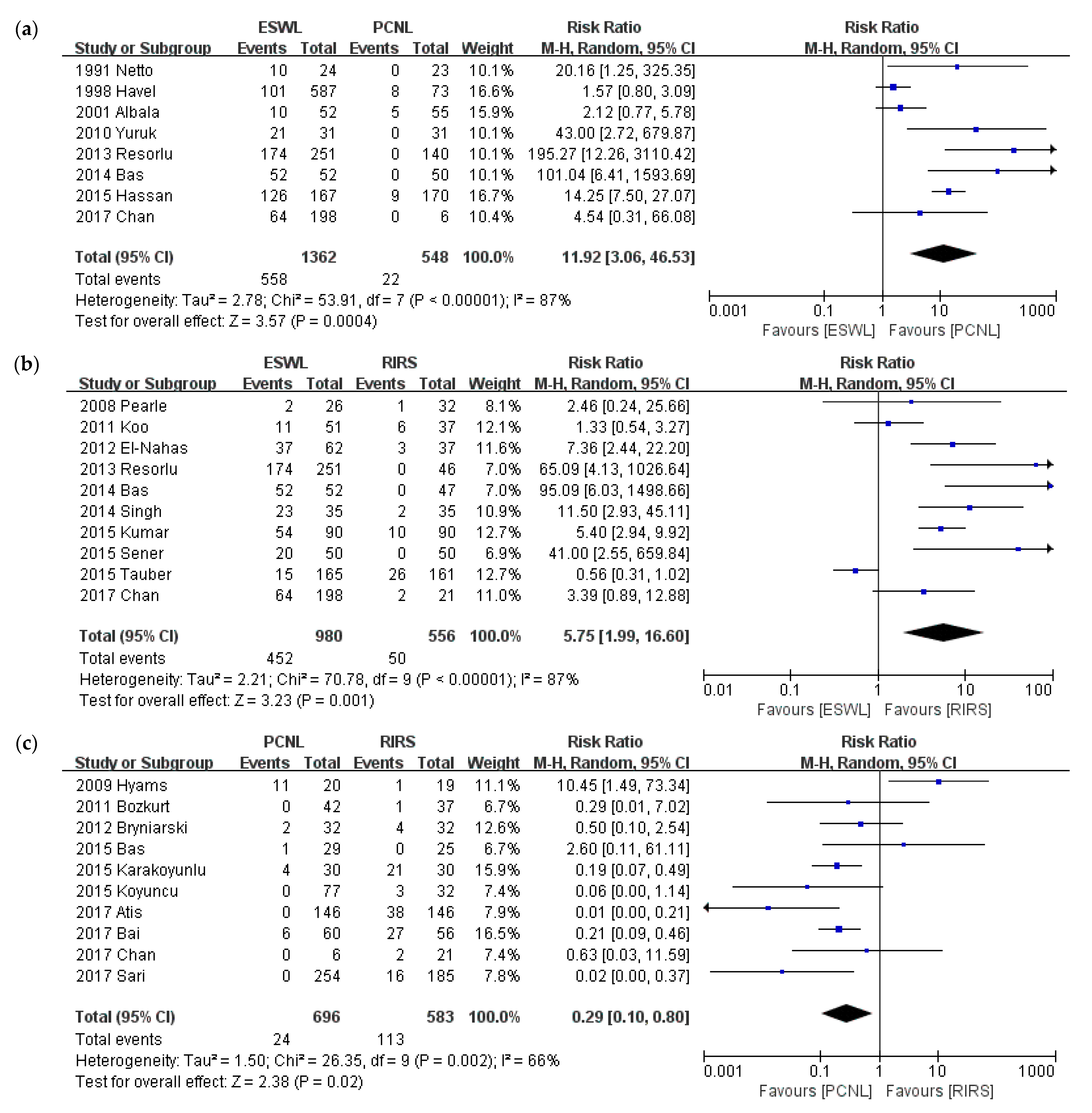
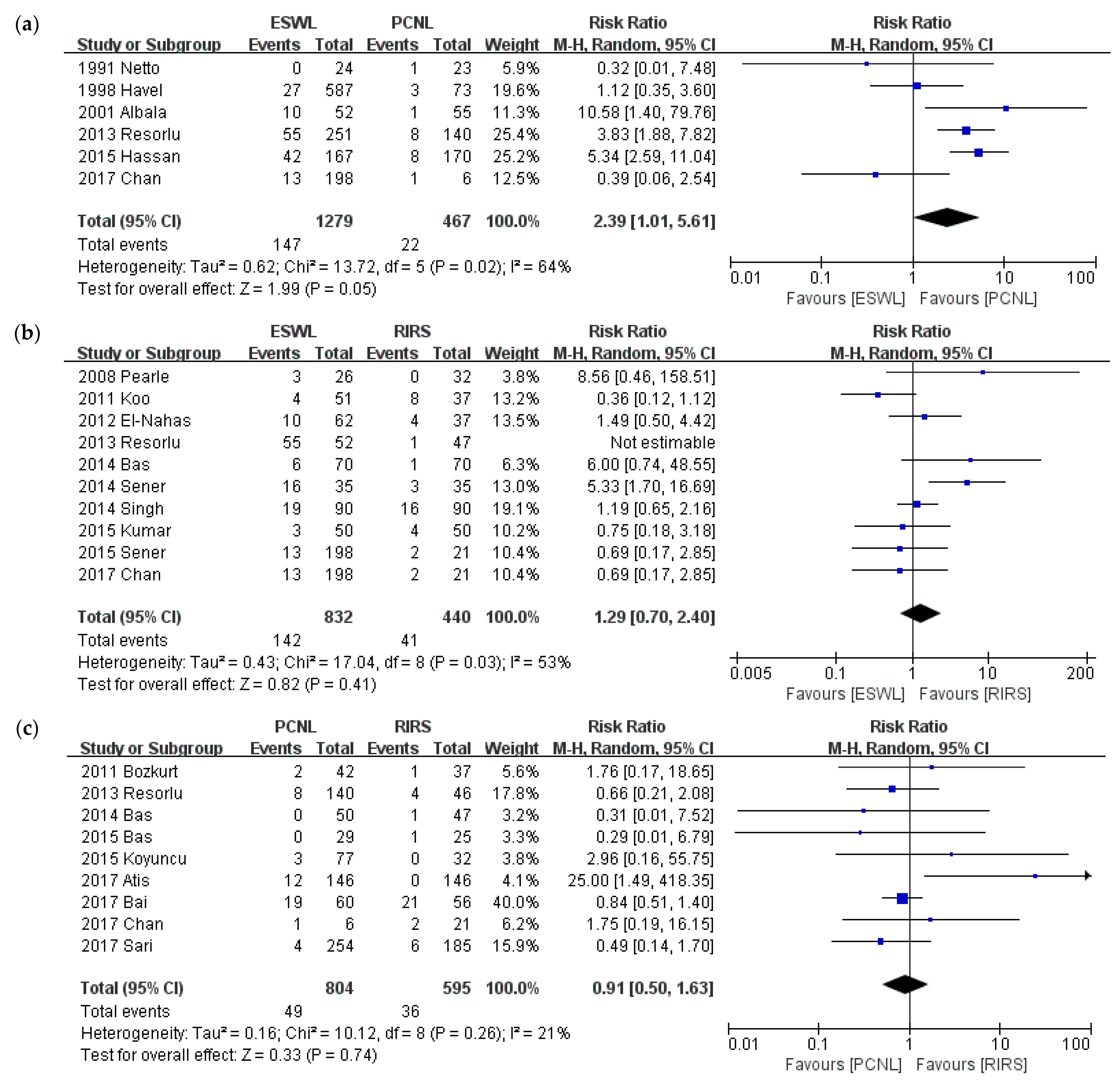
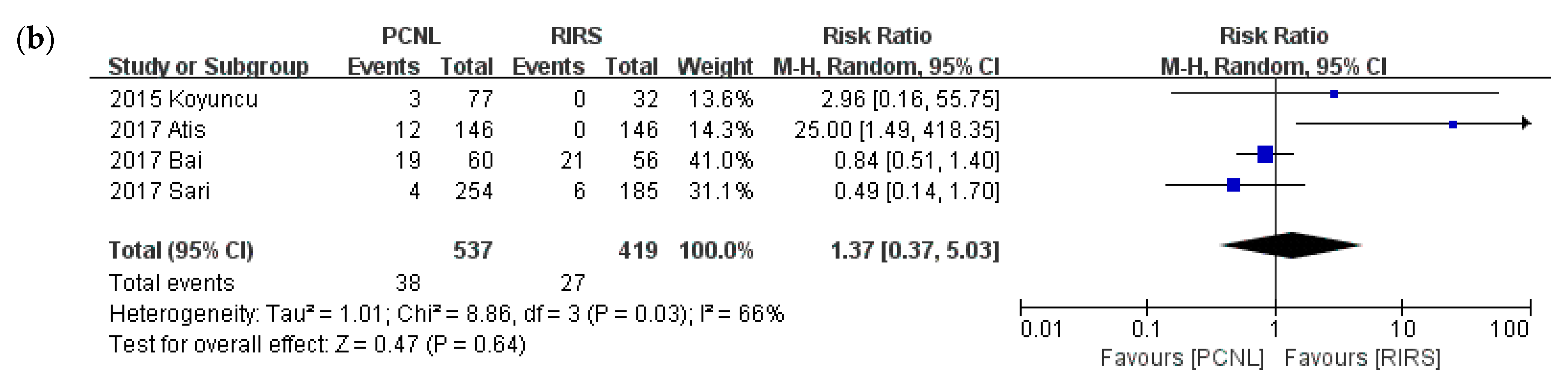
3.6. Auxiliary Procedure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Romero, V.; Akpinar, H.; Assimos, D.G. Kidney stones: A global picture of prevalence, incidence, and associated risk factors. Rev. Urol. 2010, 12, e86–e96. [Google Scholar]
- Hesse, A.; Brandle, E.; Wilbert, D.; Kohrmann, K.U.; Alken, P. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur. Urol. 2003, 44, 709–713. [Google Scholar] [CrossRef]
- Bas, O.; Bakirtas, H.; Sener, N.C.; Ozturk, U.; Tuygun, C.; Goktug, H.N.; Imamoglu, M.A. Comparison of shock wave lithotripsy, flexible ureterorenoscopy and percutaneous nephrolithotripsy on moderate size renal pelvis stones. Urolithiasis 2014, 42, 115–120. [Google Scholar] [CrossRef]
- Zhang, W.; Zhou, T.; Wu, T.; Gao, X.; Peng, Y.; Xu, C.; Chen, Q.; Song, R.; Sun, Y. Retrograde Intrarenal Surgery Versus Percutaneous Nephrolithotomy Versus Extracorporeal Shockwave Lithotripsy for Treatment of Lower Pole Renal Stones: A Meta-Analysis and Systematic Review. J. Endourol. 2015, 29, 745–759. [Google Scholar] [CrossRef]
- Jung, H.D.; Kim, J.C.; Ahn, H.K.; Kwon, J.H.; Han, K.; Han, W.K.; Kim, M.D.; Lee, J.Y. Real-time simultaneous endoscopic combined intrarenal surgery with intermediate-supine position: Washout mechanism and transport technique. Investig. Clin. Urol. 2018, 59, 348–354. [Google Scholar] [CrossRef]
- Turk, C.; Petrik, A.; Sarica, K.; Seitz, C.; Skolarikos, A.; Straub, M.; Knoll, T. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur. Urol. 2016, 69, 475–482. [Google Scholar] [CrossRef]
- Chang, K.D.; Lee, J.Y.; Park, S.Y.; Kang, D.H.; Lee, H.H.; Cho, K.S. Impact of Pretreatment Hydronephrosis on the Success Rate of Shock Wave Lithotripsy in Patients with Ureteral Stone. Yonsei Med. J. 2017, 58, 1000–1005. [Google Scholar] [CrossRef]
- Kang, D.H.; Cho, K.S.; Ham, W.S.; Chung, D.Y.; Kwon, J.K.; Choi, Y.D.; Lee, J.Y. Ureteral stenting can be a negative predictor for successful outcome following shock wave lithotripsy in patients with ureteral stones. Investig. Clin. Urol. 2016, 57, 408–416. [Google Scholar] [CrossRef]
- Zhu, W.; Liu, Y.; Liu, L.; Lei, M.; Yuan, J.; Wan, S.P.; Zeng, G. Minimally invasive versus standard percutaneous nephrolithotomy: A meta-analysis. Urolithiasis 2015, 43, 563–570. [Google Scholar] [CrossRef]
- Zheng, C.; Yang, H.; Luo, J.; Xiong, B.; Wang, H.; Jiang, Q. Extracorporeal shock wave lithotripsy versus retrograde intrarenal surgery for treatment for renal stones 1–2 cm: A meta-analysis. Urolithiasis 2015, 43, 549–556. [Google Scholar] [CrossRef]
- Zheng, C.; Xiong, B.; Wang, H.; Luo, J.; Zhang, C.; Wei, W.; Wang, Y. Retrograde intrarenal surgery versus percutaneous nephrolithotomy for treatment of renal stones >2 cm: A meta-analysis. Urol. Int. 2014, 93, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, J.F.; Lardas, M.; Scrimgeour, D.; Stewart, F.; MacLennan, S.; Lam, T.B.; McClinton, S. Systematic review and meta-analysis of the clinical effectiveness of shock wave lithotripsy, retrograde intrarenal surgery, and percutaneous nephrolithotomy for lower-pole renal stones. Eur. Urol. 2015, 67, 612–616. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Kim, J.H.; Lim, K.-C.; Lee, K.-S.; Jeong, J.-S.; Choe, M.; Chae, Y.R. Quality assessment tools and reporting standards in nursing research. J. Korean Biol. Nurs. Sci. 2012, 14, 221–230. [Google Scholar] [CrossRef][Green Version]
- Lim, S.M.; Shin, E.S.; Lee, S.H.; Seo, K.H.; Jung, Y.M.; Jang, J.E. Tools for assessing quality and risk of bias by levels of evidence. J. Korean Med. Assoc. Taehan Uisa Hyophoe Chi 2011, 54, 419–429. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kang, D.H.; Chung, D.Y.; Kwon, J.K.; Lee, H.; Cho, N.H.; Choi, Y.D.; Hong, S.J.; Cho, K.S. Meta-Analysis of the Relationship between CXCR4 Expression and Metastasis in Prostate Cancer. World J. Men’s Health 2014, 32, 167–175. [Google Scholar] [CrossRef]
- Fleiss, J.L. Analysis of data from multiclinic trials. Control Clin. Trials 1986, 7, 267–275. [Google Scholar] [CrossRef]
- L’Abbe, K.A.; Detsky, A.S.; O’Rourke, K. Meta-analysis in clinical research. Ann. Intern. Med. 1987, 107, 224–233. [Google Scholar] [CrossRef]
- Galbraith, R.F. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat. Med. 1988, 7, 889–894. [Google Scholar] [CrossRef]
- Javanmard, B.; Kashi, A.H.; Mazloomfard, M.M.; Ansari Jafari, A.; Arefanian, S. Retrograde Intrarenal Surgery Versus Shock Wave Lithotripsy for Renal Stones Smaller Than 2 cm: A Randomized Clinical Trial. Urol. J. 2016, 13, 2823–2828. [Google Scholar] [PubMed]
- Karakoyunlu, N.; Goktug, G.; Sener, N.C.; Zengin, K.; Nalbant, I.; Ozturk, U.; Ozok, U.; Imamoglu, A. A comparison of standard PCNL and staged retrograde FURS in pelvis stones over 2 cm in diameter: A prospective randomized study. Urolithiasis 2015, 43, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Sener, N.C.; Bas, O.; Sener, E.; Zengin, K.; Ozturk, U.; Altunkol, A.; Evliyaoglu, Y. Asymptomatic lower pole small renal stones: Shock wave lithotripsy, flexible ureteroscopy, or observation? A prospective randomized trial. Urology 2015, 85, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Sener, N.C.; Imamoglu, M.A.; Bas, O.; Ozturk, U.; Goktug, H.N.; Tuygun, C.; Bakirtas, H. Prospective randomized trial comparing shock wave lithotripsy and flexible ureterorenoscopy for lower pole stones smaller than 1 cm. Urolithiasis 2014, 42, 127–131. [Google Scholar] [CrossRef]
- Yuruk, E.; Binbay, M.; Sari, E.; Akman, T.; Altinyay, E.; Baykal, M.; Muslumanoglu, A.Y.; Tefekli, A. A prospective, randomized trial of management for asymptomatic lower pole calculi. J. Urol. 2010, 183, 1424–1428. [Google Scholar] [CrossRef]
- Ozayar, E.; Gulec, H.; Bayraktaroglu, M.; Tutal, Z.B.; Kurtay, A.; Babayigit, M.; Ozayar, A.; Horasanli, E. Comparison of Retrograde Intrarenal Surgery and Percutaneous Nephrolithotomy: From the View of an Anesthesiologist. J. Endourol. 2016, 30, 184–188. [Google Scholar] [CrossRef]
- Atis, G.; Culpan, M.; Pelit, E.S.; Canakci, C.; Ulus, I.; Gunaydin, B.; Yildirim, A.; Caskurlu, T. Comparison of Percutaneous Nephrolithotomy and Retrograde Intrarenal Surgery in Treating 20-40 mm Renal Stones. Urol. J. 2017, 14, 2995–2999. [Google Scholar]
- Gokce, M.I.; Tokatli, Z.; Suer, E.; Hajiyev, P.; Akinci, A.; Esen, B. Comparison of shock wave lithotripsy (SWL) and retrograde intrarenal surgery (RIRS) for treatment of stone disease in horseshoe kidney patients. Int. Braz. J. Urol. Off. J. Braz. Soc. Urol. 2016, 42, 96–100. [Google Scholar] [CrossRef]
- Sari, S.; Ozok, H.U.; Cakici, M.C.; Ozdemir, H.; Bas, O.; Karakoyunlu, N.; Sagnak, L.; Senturk, A.B.; Ersoy, H. A Comparison of Retrograde Intrarenal Surgery and Percutaneous Nephrolithotomy for Management of Renal Stones? 2 CM. Urol. J. 2017, 14, 2949–2954. [Google Scholar]
- Bas, O.; Ozyuvali, E.; Aydogmus, Y.; Sener, N.C.; Dede, O.; Ozgun, S.; Hizli, F.; Senocak, C.; Bozkurt, O.F.; Basar, H.; et al. Management of calyceal diverticular calculi: A comparison of percutaneous nephrolithotomy and flexible ureterorenoscopy. Urolithiasis 2015, 43, 155–161. [Google Scholar] [CrossRef]
- Koyuncu, H.; Yencilek, F.; Kalkan, M.; Bastug, Y.; Yencilek, E.; Ozdemir, A.T. Intrarenal Surgery vs. Percutaneous Nephrolithotomy in the Management of Lower Pole Stones Greater than 2 cm. Int. Braz. J. Urol. Off. J. Braz. Soc. Urol. 2015, 41, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Yuruk, E.; Binbay, M.; Ozgor, F.; Sekerel, L.; Berberoglu, Y.; Muslumanoglu, A.Y. Comparison of shockwave lithotripsy and flexible ureteroscopy for the treatment of kidney stones in patients with a solitary kidney. J. Endourol. 2015, 29, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Zengin, K.; Tanik, S.; Karakoyunlu, N.; Sener, N.C.; Albayrak, S.; Tuygun, C.; Bakirtas, H.; Imamoglu, M.A.; Gurdal, M. Retrograde intrarenal surgery versus percutaneous lithotripsy to treat renal stones 2–3 cm in diameter. BioMed Res. Int. 2015, 2015, 914231. [Google Scholar] [CrossRef] [PubMed]
- Resorlu, B.; Unsal, A.; Ziypak, T.; Diri, A.; Atis, G.; Guven, S.; Sancaktutar, A.A.; Tepeler, A.; Bozkurt, O.F.; Oztuna, D. Comparison of retrograde intrarenal surgery, shockwave lithotripsy, and percutaneous nephrolithotomy for treatment of medium-sized radiolucent renal stones. World J. Urol. 2013, 31, 1581–1586. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, U.; Sener, N.C.; Goktug, H.N.; Nalbant, I.; Gucuk, A.; Imamoglu, M.A. Comparison of percutaneous nephrolithotomy, shock wave lithotripsy, and retrograde intrarenal surgery for lower pole renal calculi 10–20 mm. Urol. Int. 2013, 91, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Aboutaleb, H.; El-Shazly, M.; Badr Eldin, M. Lower pole midsize (1–2 cm) calyceal stones: Outcome analysis of 56 cases. Urol. Int. 2012, 89, 348–354. [Google Scholar] [CrossRef]
- Akman, T.; Binbay, M.; Ozgor, F.; Ugurlu, M.; Tekinarslan, E.; Kezer, C.; Aslan, R.; Muslumanoglu, A.Y. Comparison of percutaneous nephrolithotomy and retrograde flexible nephrolithotripsy for the management of 2–4 cm stones: A matched-pair analysis. BJU Int. 2012, 109, 1384–1389. [Google Scholar] [CrossRef]
- Bozkurt, O.F.; Resorlu, B.; Yildiz, Y.; Can, C.E.; Unsal, A. Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J. Endourol. 2011, 25, 1131–1135. [Google Scholar] [CrossRef]
- Bryniarski, P.; Paradysz, A.; Zyczkowski, M.; Kupilas, A.; Nowakowski, K.; Bogacki, R. A randomized controlled study to analyze the safety and efficacy of percutaneous nephrolithotripsy and retrograde intrarenal surgery in the management of renal stones more than 2 cm in diameter. J. Endourol. 2012, 26, 52–57. [Google Scholar] [CrossRef]
- Chan, L.H.; Good, D.W.; Laing, K.; Phipps, S.; Thomas, B.G.; Keanie, J.Y.; Tolley, D.A.; Cutress, M.L. Primary SWL Is an Efficient and Cost-Effective Treatment for Lower Pole Renal Stones Between 10 and 20 mm in Size: A Large Single Center Study. J. Endourol. 2017, 31, 510–516. [Google Scholar] [CrossRef]
- Burr, J.; Ishii, H.; Simmonds, N.; Somani, B.K. Is flexible ureterorenoscopy and laser lithotripsy the new gold standard for lower pole renal stones when compared to shock wave lithotripsy: Comparative outcomes from a University hospital over similar time period. Cent. Eur. J. Urol. 2015, 68, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Tauber, V.; Wohlmuth, M.; Hochmuth, A.; Schimetta, W.; Krause, F.S. Efficacy Management of Urolithiasis: Flexible Ureteroscopy versus Extracorporeal Shockwave Lithotripsy. Urol. Int. 2015, 95, 324–328. [Google Scholar] [CrossRef]
- Koo, V.; Young, M.; Thompson, T.; Duggan, B. Cost-effectiveness and efficiency of shockwave lithotripsy vs. flexible ureteroscopic holmium:yttrium-aluminium-garnet laser lithotripsy in the treatment of lower pole renal calculi. BJU Int. 2011, 108, 1913–1916. [Google Scholar] [CrossRef] [PubMed]
- Havel, D.; Saussine, C.; Fath, C.; Lang, H.; Faure, F.; Jacqmin, D. Single stones of the lower pole of the kidney. Comparative results of extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy. Eur. Urol. 1998, 33, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Vasudeva, P.; Nanda, B.; Kumar, N.; Das, M.K.; Jha, S.K. A Prospective Randomized Comparison between Shock Wave Lithotripsy and Flexible Ureterorenoscopy for Lower Caliceal Stones </=2 cm: A Single-Center Experience. J. Endourol. 2015, 29, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.P.; Prakash, J.; Sankhwar, S.N.; Dhakad, U.; Sankhwar, P.L.; Goel, A.; Kumar, M. Retrograde intrarenal surgery vs. extracorporeal shock wave lithotripsy for intermediate size inferior pole calculi: A prospective assessment of objective and subjective outcomes. Urology 2014, 83, 1016–1022. [Google Scholar] [CrossRef]
- Bai, Y.; Wang, X.; Yang, Y.; Han, P.; Wang, J. Percutaneous nephrolithotomy versus retrograde intrarenal surgery for the treatment of kidney stones up to 2 cm in patients with solitary kidney: A single centre experience. BMC Urol. 2017, 17, 9. [Google Scholar] [CrossRef]
- Jung, G.H.; Jung, J.H.; Ahn, T.S.; Lee, J.S.; Cho, S.Y.; Jeong, C.W.; Lee, S.B.; Kim, H.H.; Oh, S.J. Comparison of retrograde intrarenal surgery versus a single-session percutaneous nephrolithotomy for lower-pole stones with a diameter of 15 to 30 mm: A propensity score-matching study. Korean J. Urol. 2015, 56, 525–532. [Google Scholar] [CrossRef]
- Preminger, G.M. Management of lower pole renal calculi: Shock wave lithotripsy versus percutaneous nephrolithotomy versus flexible ureteroscopy. Urol. Res. 2006, 34, 108–111. [Google Scholar] [CrossRef]
- Pearle, M.S.; Lingeman, J.E.; Leveillee, R.; Kuo, R.; Preminger, G.M.; Nadler, R.B.; Macaluso, J.; Monga, M.; Kumar, U.; Dushinski, J.; et al. Prospective, randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole caliceal calculi 1 cm or less. J. Urol. 2005, 173, 2005–2009. [Google Scholar] [CrossRef]
- Albala, D.M.; Assimos, D.G.; Clayman, R.V.; Denstedt, J.D.; Grasso, M.; Gutierrez-Aceves, J.; Kahn, R.I.; Leveillee, R.J.; Lingeman, J.E.; Macaluso, J.N., Jr.; et al. Lower pole I: A prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J. Urol. 2001, 166, 2072–2080. [Google Scholar] [CrossRef]
- Hyams, E.S.; Shah, O. Percutaneous nephrostolithotomy versus flexible ureteroscopy/holmium laser lithotripsy: Cost and outcome analysis. J. Urol. 2009, 182, 1012–1017. [Google Scholar] [CrossRef] [PubMed]
- Vilches, R.M.; Aliaga, A.; Reyes, D.; Sepulveda, F.; Mercado, A.; Moya, F.; Ledezma, R.; Hidalgo, J.P.; Olmedo, T.; Marchant, F. Comparison between retrograde intrarenal surgery and extracorporeal shock wave lithotripsy in the treatment of lower pole kidney stones up to 15 mm. Prospect. Randomized Study Actas Urol. Esp. 2015, 39, 236–242. [Google Scholar] [CrossRef]
- Netto, N.R., Jr.; Claro, J.F.; Lemos, G.C.; Cortado, P.L. Renal calculi in lower pole calices: What is the best method of treatment? J. Urol. 1991, 146, 721–723. [Google Scholar] [CrossRef]
- Hassan, M.; El-Nahas, A.R.; Sheir, K.Z.; El-Tabey, N.A.; El-Assmy, A.M.; Elshal, A.M.; Shokeir, A.A. Percutaneous nephrolithotomy vs. extracorporeal shockwave lithotripsy for treating a 20–30 mm single renal pelvic stone. Arab J. Urol. 2015, 13, 212–216. [Google Scholar] [CrossRef] [PubMed]
- El-Nahas, A.R.; Ibrahim, H.M.; Youssef, R.F.; Sheir, K.Z. Flexible ureterorenoscopy versus extracorporeal shock wave lithotripsy for treatment of lower pole stones of 10–20 mm. BJU Int. 2012, 110, 898–902. [Google Scholar] [CrossRef]
- Osman, Y.; Harraz, A.M.; El-Nahas, A.R.; Awad, B.; El-Tabey, N.; Shebel, H.; Shoma, A.M.; Eraky, I.; El-Kenawy, M. Clinically insignificant residual fragments: An acceptable term in the computed tomography era? Urology 2013, 81, 723–726. [Google Scholar] [CrossRef]
- Seitz, C.; Tanovic, E.; Kikic, Z.; Memarsadeghi, M.; Fajkovic, H. Rapid extracorporeal shock wave lithotripsy for proximal ureteral calculi in colic versus noncolic patients. Eur. Urol. 2007, 52, 1223–1227. [Google Scholar] [CrossRef]
- Kim, B.S. Recent advancement or less invasive treatment of percutaneous nephrolithotomy. Korean J. Urol. 2015, 56, 614–623. [Google Scholar] [CrossRef]
- Fernstrom, I.; Johansson, B. Percutaneous pyelolithotomy. A new extraction technique. Scand. J. Urol. Nephrol. 1976, 10, 257–259. [Google Scholar] [CrossRef]
- Wickham, J.E.; Miller, R.A.; Kellett, M.J.; Payne, S.R. Percutaneous nephrolithotomy: One stage or two? Br. J. Urol. 1984, 56, 582–585. [Google Scholar] [CrossRef] [PubMed]
- Helal, M.; Black, T.; Lockhart, J.; Figueroa, T.E. The hickman peel-away sheath: Alternative for pediatric percutaneous nephrolithotomy. J. Endourol. 1997, 11, 171–172. [Google Scholar] [CrossRef] [PubMed]
- Rana, A.M.; Bhojwani, J.P.; Junejo, N.N.; Das Bhagia, S. Tubeless PCNL with patient in supine position: Procedure for all seasons?—with comprehensive technique. Urology 2008, 71, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Zanetti, S.P.; Boeri, L.; Gallioli, A.; Talso, M.; Montanari, E. Minimally invasive PCNL-MIP. Arch Esp. Urol. 2017, 70, 226–234. [Google Scholar] [PubMed]
- Chaussy, C.; Schuller, J.; Schmiedt, E.; Brandl, H.; Jocham, D.; Liedl, B. Extracorporeal shock-wave lithotripsy (ESWL) for treatment of urolithiasis. Urology 1984, 23, 59–66. [Google Scholar] [CrossRef]
- Brandt, B.; Ostri, P.; Lange, P.; Kvist Kristensen, J. Painful caliceal calculi. The treatment of small nonobstructing caliceal calculi in patients with symptoms. Scand. J. Urol. Nephrol. 1993, 27, 75–76. [Google Scholar] [CrossRef]
- De, S.; Autorino, R.; Kim, F.J.; Zargar, H.; Laydner, H.; Balsamo, R.; Torricelli, F.C.; Di Palma, C.; Molina, W.R.; Monga, M.; et al. Percutaneous nephrolithotomy versus retrograde intrarenal surgery: A systematic review and meta-analysis. Eur. Urol. 2015, 67, 125–137. [Google Scholar] [CrossRef]
- Mancini, V.; Cormio, L.; d’Altilia, N.; Benedetto, G.; Ferrarese, P.; Balzarro, M.; Defidio, L.; Carrieri, G. Retrograde Intrarenal Surgery for Symptomatic Renal Sinus Cysts: Long-Term Results and Literature Review. Urol. Int. 2018, 101, 150–155. [Google Scholar] [CrossRef]
- Ferakis, N.; Stavropoulos, M. Mini percutaneous nephrolithotomy in the treatment of renal and upper ureteral stones: Lessons learned from a review of the literature. Urol. Ann. 2015, 7, 141–148. [Google Scholar] [CrossRef]
- Haghighi, R.; Zeraati, H.; Ghorban Zade, M. Ultra-mini-percutaneous nephrolithotomy (PCNL) versus standard PCNL: A randomised clinical trial. Arab J. Urol. 2017, 15, 294–298. [Google Scholar] [CrossRef]



| Author Year | Institution (Country) | Study Design | Study Quality | Inclusion Criteria | Definition of Stone-Free Rate | Sample Size | Age * | Male:Female | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PCNL | RIRS | ESWL | PCNL | RIRS | ESWL | PCNL | RIRS | ESWL | ||||||
| Javanmard [21] 2016 | Multiple institutions (Iran) | RCT | ++ | 0.6–2 cm | Residual stone fragments ≤3 mm | - | 60 | 60 | 32.4 ± 7.8 | 31.3 ± 6.5 | 37:23 | 39:21 | ||
| Karakoyunlu [22] 2015 | Diskapi Yildirim Beyazit Training & Research Hospital (Turkey) | RCT | + | >2 cm | Radiological absence of stone, or residual stone fragments <4 mm | 30 | 30 | - | 45.8 ± 14.1 | 48.4 ± 15.5 | - | 18:12 | 16:14 | - |
| Kumar [45] 2015 | Safdarjang Hospital (India) | RCT | ++ | ≤2 cm | Radiological absence of stone, asymptomatic patients with residual stone fragments <3 mm | - | 90 | 90 | - | 35.6 ± 2.1 | 37.7 ± 2.4 | - | 46:44 | 44:46 |
| Sener [23] 2015 | Numune Education and Research Hospital (Turkey) | RCT | + | <1 cm, lower pole, asymptomatic | Residual stone fragments <3 mm | - | 50 | 50 | 36.84 ± 11.70 | 34.5 ± 11.04 | 35:15 | 37:13 | ||
| Vilches [53] 2015 | Clinical Hospital University of Chile (Chile) | RCT | + | <1.5 cm, lower pole | Radiological absence of stone | - | 24 | 31 | 43.7 ± 9.2 | 45.6 ± 13.7 | 15:9 | 18:13 | ||
| Singh [46] 2014 | King George Medical University (India) | RCT | + | 1–2 cm, inferior calyx | Radiological absence of stone | - | 35 | 35 | 37.65 ± 11.8 | 34.5 ± 13.07 | 22:13 | 20:15 | ||
| Sener [24] 2014 | Numune Education and Research Hospital (Turkey) | RCT | + | <1 cm, lower pole | Residual stone fragments <3 mm | - | 70 | 70 | - | 45.4 ± 6.4 | 42.9 ± 5.6 | - | 41:29 | 31:29 |
| Bryniarski [39] 2012 | Silesian Medical University (Poland) | RCT | + | ≥2 cm | Radiological absence of stone | 32 | 32 | - | 51.8 ± 11.8 | 53.4 ± 12.4 | - | 16:16 | 15:17 | - |
| Yuruk [25] 2010 | Haseki Teaching & Research Hospital (Turkey) | RCT | + | ≤2 cm, lower pole, asymptomatic | Radiological absence of stone | 31 | - | 31 | 44.1 ± 12.3 | - | 44.5 ± 9.4 | 15:16 | - | 16:15 |
| Preminger [49] 2006 | Duke University Medical Center (US) | RCT | + | ≤3 cm, lower pole | Radiological absence of stone | 47 | - | 54 | ||||||
| Pearle [50] 2005 | Multiple institutions (US) | RCT | + | <1 cm, lower pole | Radiological absence of stone | - | 32 | 26 | - | 49.3 ± 14.2 | 52.5 ± 12.3 | - | 17:18 | 19:13 |
| Albala [51] 2001 | Methodist Hospital (US) | RCT | - | ≤3 cm, lower pole, symptomatic | Residual stone fragments <3 mm | 55 | - | 52 | ||||||
| Chan [40] 2017 | Western General Hospital (Scotland) | Prospective | - | 1–2 cm, lower pole | Residual stone fragments ≤ 3 mm | 6 | 21 | 198 | 55.2 ± 20.3 | 62.2 ± 15 | 54.1 ± 13.3 | 50:50 | 52:48 | 73:27 |
| Ozayar [26] 2016 | Multiple institutions (Turkey) | Prospective | + | <2 cm, lower pole | Not specific | 30 | 26 | - | 47.8 ± 11.4 | 42.5 ± 10.9 | 20:10 | 14:12 | ||
| Atis [27] 2017 | Multiple institutions (Turkey) | Retrospective | ++ | 2–4 cm | Radiological absence of stone | 146 | 146 | - | 46.33 ± 12.34 | 47.23 ± 15.16 | 104:42 | 98:48 | ||
| Bai [47] 2017 | Sichuan University (China) | Retrospective | + | >2 cm, solitary kidney | Radiological absence of stone | 60 | 56 | - | 52.22 ± 10.56 | 48.84 ± 11.27 | - | 44:16 | 37:19 | - |
| Sari [29] 2017 | Sarikamis State Hospital (Turkey) | Retrospective | + | ≥2 cm | Asymptomatic patients with residual stone fragments <3 mm | 254 | 185 | - | 46.88 ± 14.35 | 48.04 ± 14.09 | 155:99 | 111:74 | ||
| Gokce [28] 2016 | Ankara University (Turkey) | Retrospective | + | any size, horseshoe kidney | Residual stone fragments <3 mm | - | 23 | 44 | - | 44.2 ± 9.9 | 42.8 ± 8.4 | - | 18:5 | 32:12 |
| Hassan [55] 2015 | Multiple institutions (Egypt) | Retrospective | + | 2–3 cm | Residual stone fragments ≤ 4 mm | 170- | - | 167 | 50.9 ± 12.4 | - | 47.7 ± 11.7 | 80:90 | - | 107:60 |
| Bas [30] 2015 | Abdurrahman Yurtaslan hospital (Turkey) | Retrospective | + | any size, symptomatic | Radiological absence of stone | 29 | 25 | - | 45.10 ± 10.53 | 36.28 ± 10.43 | - | 14:15 | 12:13 | - |
| Burr [41] 2015 | Southampton University Hospital (UK) | Retrospective | + | any size, lower pole | Residual stone fragments ≤ 3 mm | - | 68 | 93 | 54 ± 16.6 | 54 ± 14.6 | 39:29 | 60:33 | ||
| Koyuncu [31] 2015 | Multiple institutions (Turkey) | Retrospective | + | ≥2 cm, lower pole | Radiological absence of stone | 77 | 32 | - | 38.7 ± 13.6 | 40.7 ± 15.8 | 45:32 | 20:12 | ||
| Jung [48] 2015 | Multiple institutions (Korea) | Retrospective | + | 1.5–3 cm, lower pole | Asymptomatic patients with residual stone fragments <3 mm | 44 | 44 | - | 56.1 ± 13.2 | 53.8 ± 13.4 | 52:35 | 29:15 | ||
| Tauber [42] 2015 | Multiple institutions (Austria) | Retrospective | + | ≤1.5 cm | Radiological absence of stone | - | 161 | 165 | 53.9 | 52.0 | 37.3:62.7 | 36.4:63.6 | ||
| Yuruk [32] 2015 | Haseki Training and Research Hospital (Turkey) | Retrospective | ++ | any size, solitary kidney | Not specific | - | 18 | 30 | 47.1 ± 13.8 | 51.7 ± 17.8 | 9:9 | 22:8 | ||
| Zengin [33] 2015 | Bozok University (Turkey) | Retrospective | + | 2–3 cm | Residual stone fragments < 2 mm | 74 | 80 | - | 45.6 | 48.3 | 34:40 | 38:42 | ||
| Bas [3] 2014 | Abdurrahman Yurtaslan hospital (Turkey) | Retrospective | + | 1–2 cm | Radiological absence of stone | 50 | 47 | 42 | 45.54 ± 13.1 | 47.2 ± 14.2 | 46.4 ± 15.1 | 58:42 | 63.82:36.17 | 53.84:46.15 |
| Resorlu [34] 2013 | Multiple institutions (Turkey) | Retrospective | + | 1–2 cm | Radiological absence of stone, or asymptomatic patients with residual stone < 3 mm | 140 | 46 | 251 | 36.4 ± 19.7 | 29.6 ± 20.3 | 30.8 ± 15.9 | 72:68 | 24:22 | 175:76 |
| Ozturk [35] 2013 | Yıldırım Beyazit Education and Research Hospital (Turkey) | Retrospective | + | 1–2 cm, lower pole | Radiological absence of stone, or residual stone fragments < 3 mm | 144 | 38 | 221 | 41.1 | 52 | 44.2 | 88:56 | 22:16 | 123:98 |
| Aboutaleb [36] 2012 | Farwaniya Hospital (Kuwait) | Retrospective | + | 1–2 cm, lower pole | Residual stone fragments <3 mm | 19 | 13 | 24 | 45.3 ± 14.3 | 47.2 ± 15.2 | 53.2 ± 19 | 14:5 | 7:6 | 19:5 |
| El-nahas [56] 2012 | Mansoura University (Egypt) | Retrospective | + | 1–2 cm, lower pole | Residual stone fragments <4 mm | - | 37 | 62 | 47.8 ± 10.7 | 45.4 ± 11.3 | 26:11 | 41:21 | ||
| Akman [37] 2011 | Haseki Training & Research Hospital (Turkey) | Retrospective | + | 2–4 cm | Radiological absence of stone | 34 | 34 | - | 44.8 ± 17.1 | 44.5 ± 16.5 | 47.1:52.9 | 52.9:47.1 | ||
| Bozkurt [38] 2011 | Kecioren Research & Training Hospital (Turkey) | Retrospective | + | 1.5–2 cm | Residual stone fragments <3 mm | 42 | 37 | - | 47.4 ± 15.5 | 41.2 ± 13.6 | 25:17 | 21:16 | ||
| Koo [43] 2011 | Craigavon Area Hospital (UK) | Retrospective | + | ≤2 cm, lower pole | Radiological absence of stone, or residual stone fragments < 3 mm | - | 37 | 51 | 56.6 ± 15.9 | 51.2 ± 14.9 | 22:15 | 35:16 | ||
| Hyams [52] 2009 | New York University (US) | Retrospective | + | 2–3 cm | Residual stone fragments <4 mm | 20 | 19 | - | 48 | 56 | 11:9 | 5:14 | ||
| Havel [44] 1998 | Strasbourg University (France) | Retrospective | - | any size, lower pole | Radiological absence of stone | 73 | - | 587 | 50 | - | 48 | |||
| Netto [54] 1991 | Israelita Albert Einstiein Hospital (Brazil) | Retrospective | + | ≤3 cm | Radiological absence of stone | 23 | - | 24 | 44 | 48 | 13:10 | 14:10 | ||
| Outcome | No. of Studies | RR (95% CI) | p Value | I2 (%) | |
| ESWL vs. PCNL | Stone-free rate | 11 | 0.69 (0.61–0.78) | <0.00001 | 81 |
| stone size ≤ 2 cm | 6 | 0.76 (0.68–0.85) | <0.00001 | 63 | |
| stone size > 2 cm | 1 | 0.72 (0.65–0.80) | <0.00001 | - | |
| Lower pole stone | 6 | 0.58 (0.44–0.76) | 0.001 | 88 | |
| Total complication | 6 | 0.28 (0.18–0.45) | <0.00001 | 64 | |
| stone size ≤ 2 cm | 4 | 0.29 (0.16–0.52) | <0.0001 | 40 | |
| stone size > 2 cm | 0 | - | - | - | |
| Lower pole stone | 4 | 0.24 (0.14–0.41) | <0.00001 | 57 | |
| Retreatment procedure | 8 | 11.92 (3.06–46.53) | 0.0004 | 87 | |
| stone size ≤ 2 cm | 4 | 43.33 (7.45–251.91) | <0.0001 | 39 | |
| stone size > 2 cm | 1 | 14.25 (7.50–27.07) | <0.00001 | - | |
| Lower pole stone | 4 | 2.91 (0.99–8.56) | 0.05 | 58 | |
| Auxiliary procedure | 6 | 2.39 (1.01–5.61) | 0.05 | 64 | |
| stone size ≤ 2 cm | 2 | 1.45 (0.15–13.63) | 0.75 | 81 | |
| stone size > 2 cm | 1 | 5.34 (2.59–11.04) | <0.00001 | - | |
| Lower pole stone | 3 | 1.56 (0.27–8.93) | 0.62 | 70 | |
| Outcome | No. of Studies | RR (95% CI) | p Value | I2 (%) | |
| ESWL vs. RIRS | Stone-free rate | 18 | 0.77 (0.67–0.88) | 0.0002 | 87 |
| stone size ≤ 2 cm | 15 | 0.82 (0.73–0.92) | 0.0004 | 79 | |
| stone size > 2 cm | - | - | - | - | |
| Lower pole stone | 10 | 0.76 (0.60–0.97) | 0.03 | 92 | |
| Total complication | 12 | 0.87 (0.63–1.19) | 0.38 | 16 | |
| stone size ≤ 2 cm | 10 | 0.81 (0.56–1.17) | 0.26 | 22 | |
| stone size > 2 cm | - | - | - | - | |
| Lower pole stone | 6 | 0.49 (0.29–0.83) | 0.008 | 0 | |
| Retreatment procedure | 10 | 5.75 (1.99–16.60) | 0.001 | 87 | |
| stone size ≤ 2 cm | 9 | 6.25 (2.02–19.32) | 0.001 | 89 | |
| stone size > 2 cm | - | - | - | - | |
| Lower pole stone | 3.96 (1.35–11.60) | 0.01 | 63 | ||
| Auxiliary procedure | 10 | 1.29 (0.70–2.40) | 0.41 | 53 | |
| stone size ≤ 2 cm | 9 | 1.2 (0.65–2.23) | 0.56 | 54 | |
| stone size > 2 cm | - | - | - | ||
| Lower pole stone | 5 | 1.46 (0.48–4.48) | 0.50 | 70 | |
| Outcome | No. of studies | RR (95% CI) | pvalue | I2 (%) | |
| PCNL vs. RIRS | Stone-free rate | 18 | 1.14 (1.06–1.22) | 0.0003 | 69 |
| stone size ≤ 2 cm | 7 | 1.08 (1.02–1.14) | 0.01 | 0 | |
| stone size > 2 cm | 9 | 1.23 (1.10–1.37) | 0.0003 | 74 | |
| Lower pole stone | 5 | 1.34 (0.95–1.88) | 0.10 | 89 | |
| Total complication | 13 | 1.41 (1.06–1.86) | 0.02 | 15 | |
| stone size ≤ 2 cm | 5 | 2.05 (1.20–3.52) | 0.009 | 0 | |
| stone size > 2 cm | 6 | 1.24 (0.84–1.83) | 0.29 | 35 | |
| Lower pole stone | 4 | 1.99 (0.91–4.37) | 0.09 | 10 | |
| Retreatment procedure | 10 | 0.29 (0.10–0.80) | 0.02 | 66 | |
| stone size ≤ 2 cm | 2 | 0.44 (0.05–3.80) | 0.46 | 0 | |
| stone size > 2 cm | 7 | 0.22 (0.06–0.74) | 0.01 | 75 | |
| Lower pole stone | 2 | 0.20 (0.02–1.97) | 0.17 | 20 | |
| Auxiliary procedure | 9 | 0.91 (0.50–1.63) | 0.74 | 21 | |
| stone size ≤ 2 cm | 4 | 0.84 (0.34–2.07) | 0.70 | 0 | |
| stone size > 2 cm | 4 | 1.37 (0.37–5.03) | 0.64 | 66 | |
| Lower pole stone | 2 | 2.12 (0.36–12.47) | 0.41 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, C.H.; Chung, D.Y.; Rha, K.H.; Lee, J.Y.; Lee, S.H. Effectiveness of Percutaneous Nephrolithotomy, Retrograde Intrarenal Surgery, and Extracorporeal Shock Wave Lithotripsy for Treatment of Renal Stones: A Systematic Review and Meta-Analysis. Medicina 2021, 57, 26. https://doi.org/10.3390/medicina57010026
Kim CH, Chung DY, Rha KH, Lee JY, Lee SH. Effectiveness of Percutaneous Nephrolithotomy, Retrograde Intrarenal Surgery, and Extracorporeal Shock Wave Lithotripsy for Treatment of Renal Stones: A Systematic Review and Meta-Analysis. Medicina. 2021; 57(1):26. https://doi.org/10.3390/medicina57010026
Chicago/Turabian StyleKim, Chan Hee, Doo Yong Chung, Koon Ho Rha, Joo Yong Lee, and Seon Heui Lee. 2021. "Effectiveness of Percutaneous Nephrolithotomy, Retrograde Intrarenal Surgery, and Extracorporeal Shock Wave Lithotripsy for Treatment of Renal Stones: A Systematic Review and Meta-Analysis" Medicina 57, no. 1: 26. https://doi.org/10.3390/medicina57010026
APA StyleKim, C. H., Chung, D. Y., Rha, K. H., Lee, J. Y., & Lee, S. H. (2021). Effectiveness of Percutaneous Nephrolithotomy, Retrograde Intrarenal Surgery, and Extracorporeal Shock Wave Lithotripsy for Treatment of Renal Stones: A Systematic Review and Meta-Analysis. Medicina, 57(1), 26. https://doi.org/10.3390/medicina57010026






