Designers Drugs—A New Challenge to Emergency Departments—An Observational Study in Poland
Abstract
1. Introduction
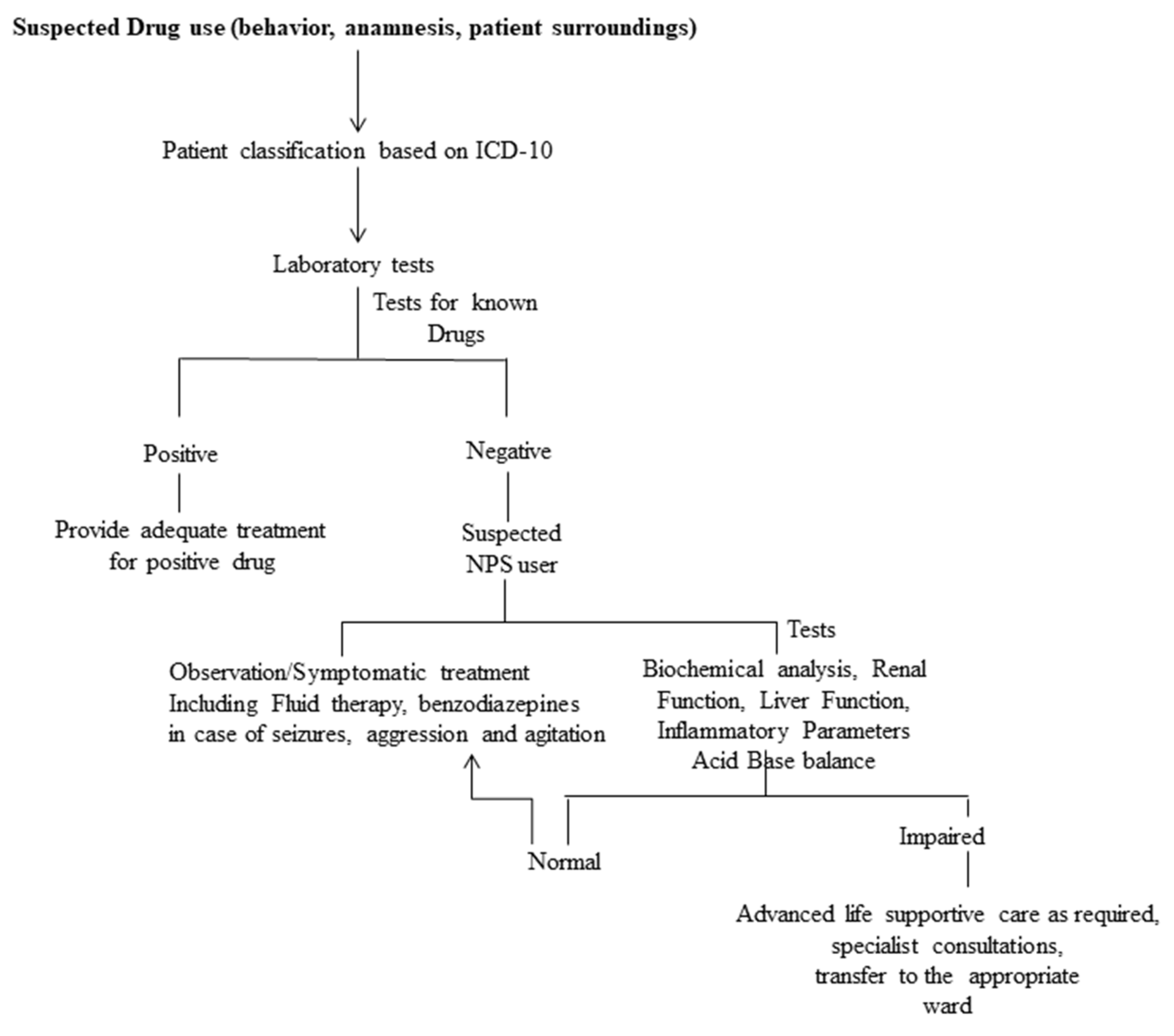
2. Materials and Methods
- GCS [15]: evaluation of eye, speech, and motor functions;
- NEWS [16]: seven routinely collected vital signs, including respiratory rate, oxygen saturation, temperature, blood pressure, pulse and AVPU response;
- PEWS [17]; three routinely collected vital signs including capillary refill, behavior and respiration rate.
Statistical Analysis
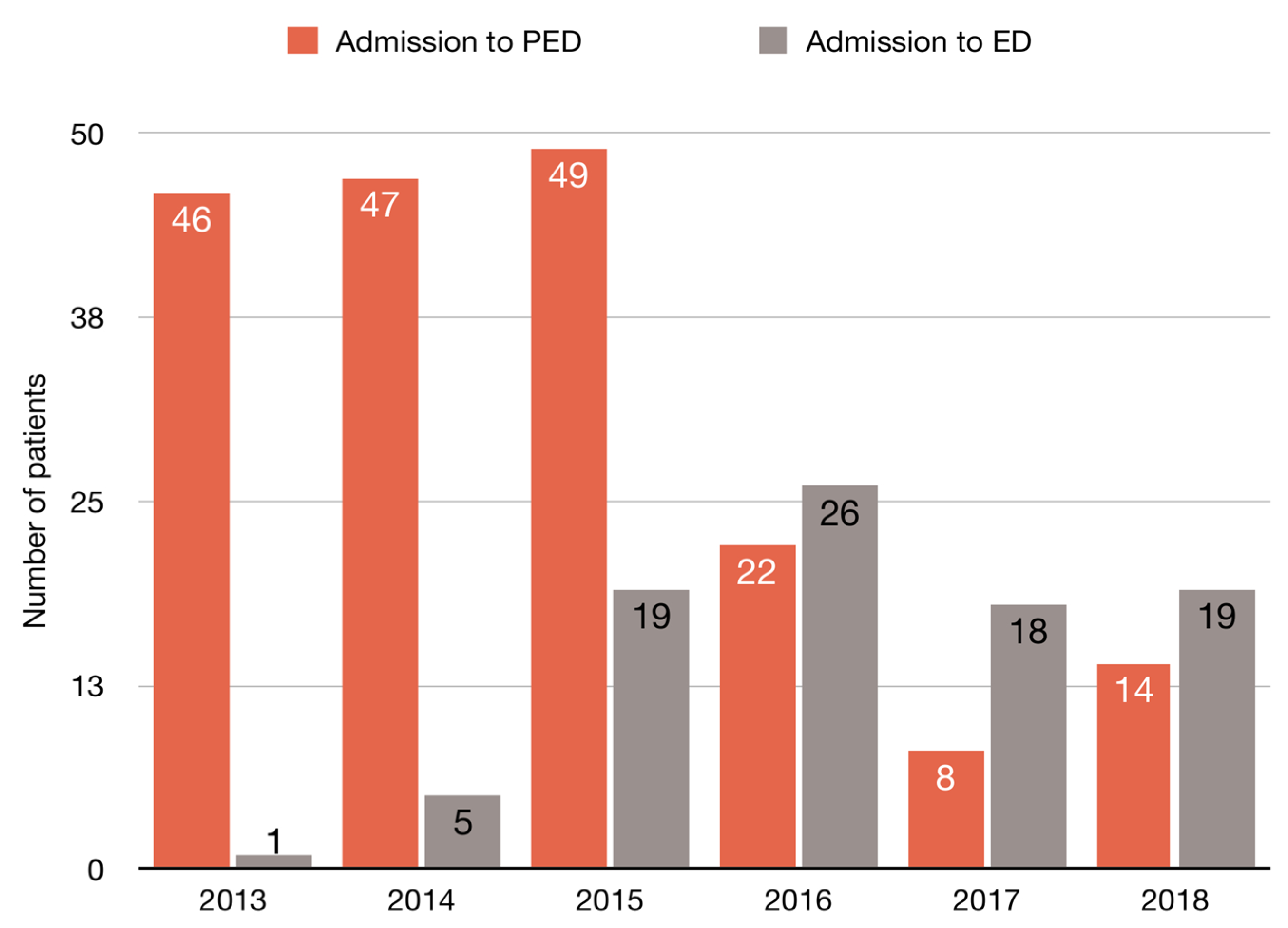
3. Results
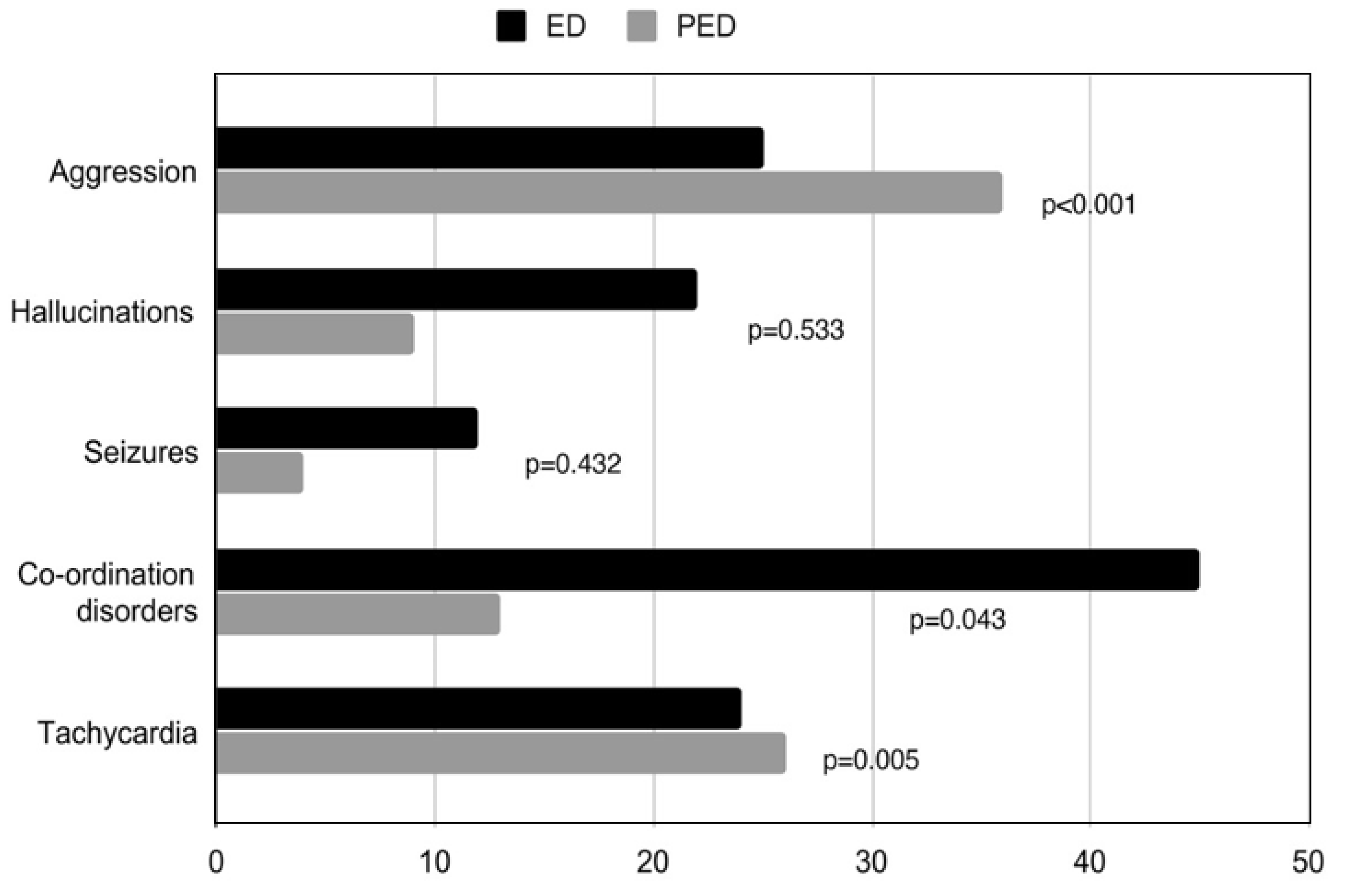
3.1. General Condition and Symptoms
3.2. NPS and Other Drugs
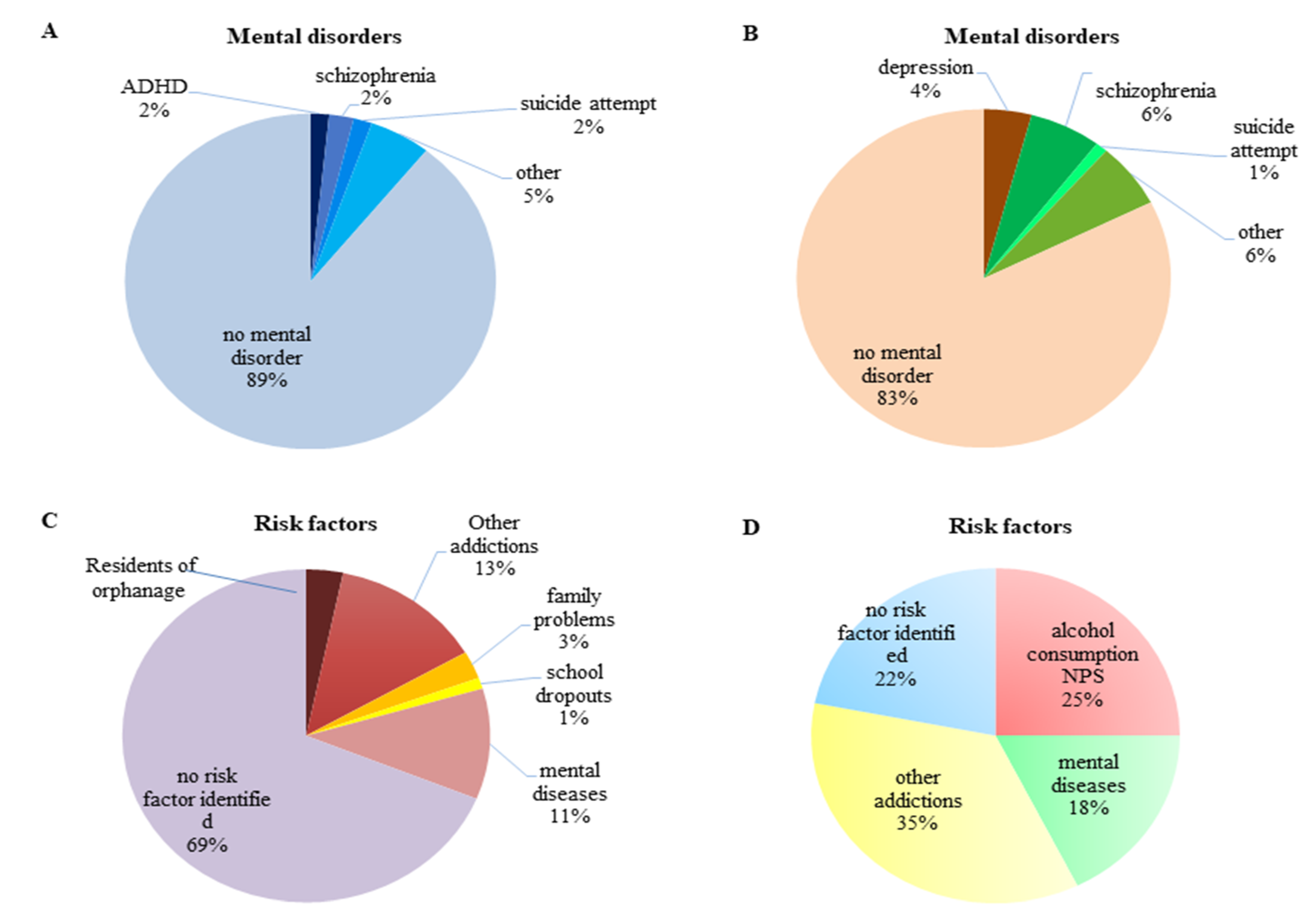
3.3. NPS and Mental Disorders
3.4. Risk Factors
3.5. Additional Medical Tests
3.6. Other Health Threats
4. Discussion
5. Limitations
6. Summary
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Andrabi, S.; Greene, S.; Moukaddam, N.; Li, B. New drugs of abuse and withdrawal syndromes. Emerg. Med. Clin. 2015, 33, 779–795. [Google Scholar] [CrossRef] [PubMed]
- Scherbaum, N.; Schifano, F.; Bonnet, U. New psychoactive substances (NPS)—A challenge for the addiction treatment services. Pharmacopsychiatry 2017, 50, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Rinaldi, R.; Bersani, G.; Marinelli, E.; Zaami, S. The rise of new psychoactive substances and psychiatric implications: A wide-ranging, multifaceted challenge that needs far-reaching common legislative strategies. Hum. Psychopharmacol. Clin. Exp. 2020, 35, e2727. [Google Scholar] [CrossRef] [PubMed]
- Journal of Laws of the Republic of Poland. Available online: http://prawo.sejm.gov.pl/isap.nsf/download.xsp/WDU20180001490/O/D20181490.pdf (accessed on 6 August 2018).
- Whissell, P.D.; Tohyama, S.; Martin, L.J. The use of DREADDs to deconstruct behavior. Front. Genet. 2016, 7, 70. [Google Scholar] [CrossRef]
- Kemp, A.M.; Clark, M.S.; Dobbs, T.; Galli, R.; Sherman, J.; Cox, R. Top 10 facts you need to know about synthetic cannabinoids: Not so nice spice. Am. J. Med. Sci. 2016, 129, 240–244. [Google Scholar] [CrossRef]
- Baumeister, D.; Tojo, L.M.; Tracy, D.K. Legal highs: Staying on top of the flood of novel psychoactive substances. Ther. Adv. Psychopharmacol. 2015, 5, 97–132. [Google Scholar] [CrossRef]
- Cohen, K.; Weinstein, A.M. Synthetic and non-synthetic cannabinoid drugs and their adverse effects—A review from public health prospective. Front. Public Health 2018, 6, 162. [Google Scholar] [CrossRef]
- Schneir, A.; Ly, B.T.; Casagrande, K.; Darracq, M.; Offerman, S.R.; Thornton, S.; Smollin, C.; Vorah, R.; Rangun, C.; Tomaszewski, C.; et al. Comprehensive analysis of “bath salts” purchased from California stores and the internet. Clin. Toxicol. 2014, 52, 651–658. [Google Scholar] [CrossRef]
- The Supreme Audit Office in Poland. Available online: https://www.nik.gov.pl/aktualnosci/nik-o-przeciwdzialaniu-sprzedazy-dopalaczy.html (accessed on 3 November 2017).
- Musselman, M.E.; Hampton, J.P. “Not for human consumption”: A review of emerging designer drugs. Pharmacotherapy 2014, 34, 745–757. [Google Scholar] [CrossRef]
- Saleh, A.; Tittley, J.; Anand, S. Limb-threatening ischemia in a young man with cathinone “bath salt” intoxication: A case report. Ann. Vasc. Surg. 2016, 36, 294.e1–294.e5. [Google Scholar] [CrossRef]
- Kamijo, Y.; Takai, M.; Fujita, Y.; Sakamoto, T. A multicenter retrospective survey of poisoning after consumption of products containing novel psychoactive substances from 2013 to 2014 in Japan. Am. J. Drug Alcohol Abus. 2016, 42, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Miliano, C.; Serpelloni, G.; Rimondo, C.; Mereu, M.; Marti, M.; de Luca, M.A. Neuropharmacology of new psychoactive substances (NPS): Focus on the rewarding and reinforcing properties of cannabimimetics and amphetamine-like stimulants. Front. Neurosci. 2016, 10, 153–174. [Google Scholar] [CrossRef] [PubMed]
- Ghelichkhani, P.; Esmaeili, M.; Hosseini, M.; Seylani, K. Glasgow coma scale and four score in predicting the mortality of trauma patients; a diagnostic accuracy study. Emergency 2018, 6, e42. [Google Scholar] [PubMed]
- Shamout, F.G.; Zhu, T.; Clifton, L.; Briggs, J.; Prytherch, D.; Meridith, P.; Tarassenko, L.; Watkinson, P.J.; Clifton, D.A. Early warning score adjusted for age to predict the composite outcome of mortality, cardiac arrest or unplanned intensive care unit admission using observational vital-sign data: A multicentre development and validation. BMJ Open 2019, 9, e033301. [Google Scholar] [CrossRef]
- Solevag, A.L.; Eggen, E.H.; Schroder, J.; Nakstad, B. Use of modified pediatric early warning score in a department pediatric adolescent medicine. PLoS ONE 2013, 8, e72534. [Google Scholar] [CrossRef]
- Parrott, A.C. Mood fluctuation and psychobiological instability: The same core functions are disrupted by novel psychoactive substances and established recreational drugs. Brain Sci. 2018, 8, 43. [Google Scholar] [CrossRef]
- Palamar, J.J.; Ecosta, P.; Sherman, S.; Ompad, D.C.; Cleland, C.M. Self-reported use of novel psychoactive substances among attendees of electronic dance music venues. Am. J. Drug Alcohol Abus. 2016, 42, 624–632. [Google Scholar] [CrossRef]
- Khaled, S.M.; Hughes, E.; Bressington, D.; Zolezzi, M.; Radwan, A.; Badnapurkar, A.; Gray, R. The prevalence of novel psychoactive substances (NPS) use in non-clinical populations: A systematic review protocol. Syst. Rev. 2016, 5, 1–7. [Google Scholar] [CrossRef]
- Altintop, I.; Karakukcu, C. The chameleon-like properties of psychoactive drugs: Examinations with HR LC-MS/MS technology of patients presenting at the emergency department following the use of synthetic cannabinoids: A case series and literature review. Behav. Sci. 2018, 8, 88. [Google Scholar] [CrossRef]
- Henshall, D.E.; Wd Innes, C.; Morrison, S.R.; Wilson, B.; Brown, R.A.; McAlister, S.M.; Culshaw, S.L.; Reda, E. A prospective observational study of emergency department presentations following novel psychoactive substance use. Scott. Med. J. 2018, 63, 39–44. [Google Scholar] [CrossRef]
- Stevenson, G.; Richardson, A. New psychoactive substances in England [online]. London: Crime and Policing Analysis Unit, Home Office Science. 2014. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/368587/NPSevidenceReview.pdf (accessed on 5 January 2018).
- Winstock, A.R.; Barrett, M.; Ferris, J.; Maier, L. What We Learned from GDS2016 An Overview of Our Key Findings. 2016. Available online: https://www.globaldrugsurvey.com/gds-surveys/ (accessed on 5 January 2018).
- Adamowicz, P.; Gieron, J.; Gil, D.; Lechowicz, W.; Skulska, A.; Tokarczyk, B. The prevalence of new psychoactive substances in biological material—A three-year review of casework in Poland. Drug. Test. Anal. 2016, 8, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Sawicka, J.; Czyzewska, S.; Winnicka, R.; Politanski, P.; Swiderska-Kielbik, S.; Kolaczynski, Z.; Czerniak, P.; Krakowiak, A. Acute novel drugs poisoning among patients of Nofer Institute of Occupational Medicine in Lodz, Toxicology Unit, hospitalized in the years 2008–2012—Epidemiology, clinical state. Prz. Lek. 2013, 70, 520–524. [Google Scholar] [PubMed]
- European Drug Report: Trends and Developments; European Monitoring Center for Drugs and Drug Abuse (EMCDDA): Lisbon, Portugal, 2015; Available online: http://www.emcdda.europa.eu/publications/edr/trends-developments/2015_en (accessed on 10 October 2018).
- Kassai, S.; Pintér, J.N.; Rácz, J.; Borondi, B.; Toth-Kariko, T.; Kerekes, K.; Gyarmathy, V.A. Assessing the experience of using synthetic cannabinoids by means of interpretative phenomenological analysis. Harm Reduct. J. 2017, 14, 9. [Google Scholar] [CrossRef]
- Sutherland, R.; Bruno, R.; Peacock, A.; Lenton, S.; Mathews, A.; Salom, C.; Dietze, P.; Butler, K.; Burns, L.; Barratt, M.J. Motivations for new psychoactive substance use among regular psychostimulant users in Australia. Int. J. Drug Policy 2017, 43, 23–32. [Google Scholar] [CrossRef]
- Jang, M.; Yang, W.; Choi, H.; Chang, H.; Lee, S.; Kim, E.; Chung, H. Monitoring of urinary metabolites of JWH-018 and JWH-073 in legal cases. Forensic Sci. Int. 2013, 231, 13–19. [Google Scholar] [CrossRef]
- Zimmermann, U.S.; Winklemann, P.R.; Pilhatsch, M.; Nees, J.A.; Spanagel, R.; Schulz, K. Withdrawal phenomena and dependence syndrome after the consumption of “spice gold”. Dtsch. Arztebl. Int. 2009, 106, 464–467. [Google Scholar] [CrossRef]
- der Veer, N.V.; Friday, J. Persistent psychosis following the use of spice. Schizophr. Res. 2011, 130, 285–286. [Google Scholar] [CrossRef]
- Hohmann, N.; Mikus, G.; Czock, D. Effects and risks associated with novel psychoactive substances: Mislabeling and sale as bath salts, spice, and research chemicals. Dtsch. Arztebl. Int. 2014, 111, 139–147. [Google Scholar] [CrossRef][Green Version]
- Cohen, K.; Weinstein, A. The effects of synthetic cannabinoids on executive function. Psychopharmacology 2017, 234, 1121–1134. [Google Scholar] [CrossRef]
- Pirona, A.; Atkins, A. Health Responses to New Psychoactive Substances; European Monitoring Centre for Drugs and Drug Addiction (EMCDDA): Lisbon, Portugal, 2016; Available online: https://www.emcdda.europa.eu/system/files/publications/2812/TD0216555ENN.pdf (accessed on 1 June 2020).
- Byard, R.W.; Cox, M.; Stockham, P. Blunt craniofacial trauma as a manifestation of excited delirium caused by new psychoactive substances. J. Forensic Sci. 2016, 61, 1546–1548. [Google Scholar] [CrossRef]
- Yun, J.; Gu, S.M.; Lee, T.; Song, Y.J.; Seong, S.; Kim, Y.-H.; Cha, H.J.; Han, K.M.; Shin, J.; Oh, H.; et al. Synthetic cannabinoid-induced immunosuppression augments cerebellar dysfunction in tetanus-toxin treated mice. Biomol. Ther. 2017, 25, 266–271. [Google Scholar] [CrossRef]
| All | PED | ED | p | ||||
|---|---|---|---|---|---|---|---|
| All n (%) | 282 | (100) | 186 | (66) | 96 | (34) | |
| Sex n (%) | |||||||
| female | 53 | (19) | 47 | (25) | 6 | (6) | <0.001 |
| male | 229 | (81) | 139 | (75) | 90 | (94) | |
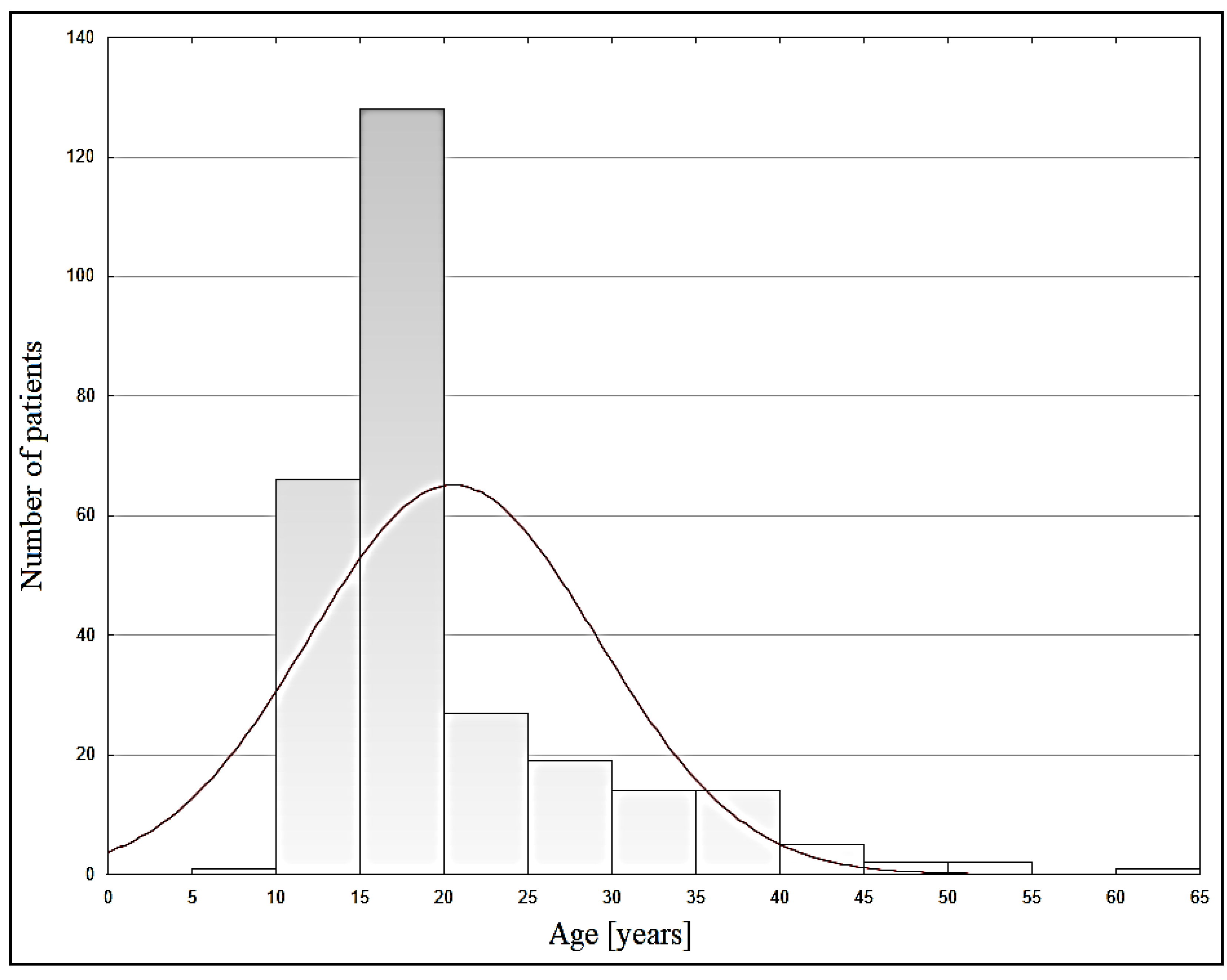
| Age [years] (median, IQR) | 279 | 17 (16–23) | 16 (15–17) | 28 (23–36) | <0.001 | ||
| no data | 3 | 3 | |||||
| Risk factors | |||||||
| Mental disorders n (%) | 37 | (13) | 20 | (11) | 17 | (18) | 0.135 |
| Other diseases n (%) | 19 | (7) | 5 | (3) | 14 | (15) | <0.001 |
| Other addictions n (%) | 74 | (26) | 40 | (22) | 34 | (35) | 0.015 |
| Addictions | |||||||
| THC n (%) | 9 | (3) | 6 | (3) | 3 | (3) | 0.964 |
| Amfetamin n (%) | 5 | (2) | 2 | (1) | 3 | (3) | 0.217 |
| GBL n (%) | 6 | (2) | 2 | (1) | 4 | (4) | 0.088 |
| Alcohol n (%) | 20 | (7) | 7 | (4) | 13 | (14) | 0.002 |
| Main symptoms of NPS | |||||||
| Aggression n (%) | 61 | (22) | 25 | (13) | 36 | (37.5) | <0.001 |
| Hallucinations | 31 | (11) | 22 | (12) | 9 | (9) | 0.533 |
| Seizures | 16 | (6) | 12 | (6) | 4 | (4) | 0.432 |
| Co-ordination disorders n (%) | 58 | (21) | 45 | (24) | 13 | (14) | 0.043 |
| Tachycardia n (%) | 50 | (18) | 24 | (13) | 26 | (27) | 0.005 |
| During hospitalization: | |||||||
| Positive test of alcohol n (%) | 43 | (15) | 19 | (10) | 24 | (25) | 0.002 |
| The need for hospitalization in WZLP n (%) | 27 | (10) | 8 | (4) | 19 | (20) | <0.001 |
| Earlier hospitalizations due to NPS n (%) | 84 | (30) | 54 | (29) | 30 | (31) | 0.78 |
| Transferred to another department/consulted n (%) | 29 | (10) | 13 | (7) | 16 | (17) | 0.021 |
| Medical Condition n (%) | |||||||
| good | 163 | (58) | 101 | (54) | 62 | (65) | 0.25 |
| moderate | 104 | (37) | 74 | (40) | 30 | (31) | |
| severe | 15 | (5) | 11 | (6) | 4 | (4) | |
| 2013–2014 | 2015–2016 | 2017–2018 | p | ||||
|---|---|---|---|---|---|---|---|
| All n (%) | 99 | (35) | 116 | (41) | 67 | (24) | |
| Sex n (%) | |||||||
| female | 22 | (22) | 24 | (21) | 7 | (10) | 0.129 |
| male | 77 | (78) | 92 | (79) | 60 | (90) | |
| Age [years] (median, IQR) | 16 (14–17) | 17 (14–36) | 23 (15–39) | <0.001 | |||
| no data | 3 | 2 | 1 | ||||
| Risk factors | |||||||
| Mental diseases n (%) | 4 | (4) | 19 | (16) | 14 | (21) | 0.003 § |
| Other diseases n (%) | 1 | (1) | 9 | (8) | 9 | (13) | 0.006 † |
| Other addictions n (%) | 21 | (21) | 35 | (30) | 18 | (27) | 0.327 |
| Addictions | |||||||
| THC n (%) | 3 | (3) | 3 | (3) | 3 | (4) | 0.777 |
| Amfetamin n (%) | 1 | (1) | 0 | (0) | 4 | (6) | 0.010 §§ |
| GBL n (%) | 2 | (2) | 4 | (3) | 0 | (0) | 0.296 |
| Alcohol n (%) | 2 | (2) | 8 | (7) | 10 | (15) | 0.006 ** |
| Main symptoms of NPS | |||||||
| Aggression n (%) | 6 | (6) | 32 | (28) | 23 | (34) | <0.001 ¥ |
| Hallucinations | 11 | (11) | 8 | (7) | 12 | (18) | 0.072 |
| Seizures | 5 | (5) | 7 | (6) | 4 | (6) | 0.946 |
| Co-ordination disorders n (%) | 24 | (24) | 17 | (15) | 17 | (25) | 0.119 |
| Tachycardia n (%) | 12 | (12) | 21 | (18) | 17 | (25) | 0.089 ^^ |
| During hospitalization: | |||||||
| Positive test of alcohol n (%) | 9 | (9) | 16 | (14) | 18 | (27) | 0.006 * |
| The need for hospitalization in WZLP n (%) | 5 | (5) | 8 | (7) | 14 | (21) | 0.001 $ |
| Earlier hospitalizations due to NPS n (%) | 25 | (25) | 38 | (33) | 21 | (31) | 0.463 |
| Transferred to another department/consulted n (%) | 7 | (7) | 14 | (12) | 8 | (12) | 0.426 |
| Medical Condition n (%) | |||||||
| good | 58 | (59) | 52 | (45) | 53 | (79) | <0.001 ^ |
| moderate | 36 | (36) | 54 | (47) | 14 | (21) | |
| severe | 5 | (5) | 10 | (8) | 0 | (0) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jalali, R.; Dmochowska, P.; Godlewska, I.; Balmas, J.; Młynarska, K.; Narkun, K.; Zawadzki, A.; Wojnar, M. Designers Drugs—A New Challenge to Emergency Departments—An Observational Study in Poland. Medicina 2020, 56, 354. https://doi.org/10.3390/medicina56070354
Jalali R, Dmochowska P, Godlewska I, Balmas J, Młynarska K, Narkun K, Zawadzki A, Wojnar M. Designers Drugs—A New Challenge to Emergency Departments—An Observational Study in Poland. Medicina. 2020; 56(7):354. https://doi.org/10.3390/medicina56070354
Chicago/Turabian StyleJalali, Rakesh, Paula Dmochowska, Izabela Godlewska, Justyna Balmas, Katarzyna Młynarska, Krzysztof Narkun, Andrzej Zawadzki, and Marcin Wojnar. 2020. "Designers Drugs—A New Challenge to Emergency Departments—An Observational Study in Poland" Medicina 56, no. 7: 354. https://doi.org/10.3390/medicina56070354
APA StyleJalali, R., Dmochowska, P., Godlewska, I., Balmas, J., Młynarska, K., Narkun, K., Zawadzki, A., & Wojnar, M. (2020). Designers Drugs—A New Challenge to Emergency Departments—An Observational Study in Poland. Medicina, 56(7), 354. https://doi.org/10.3390/medicina56070354





