Validity of the STOP-Bang Questionnaire in Identifying OSA in a Dental Patient Cohort
Abstract
1. Introduction
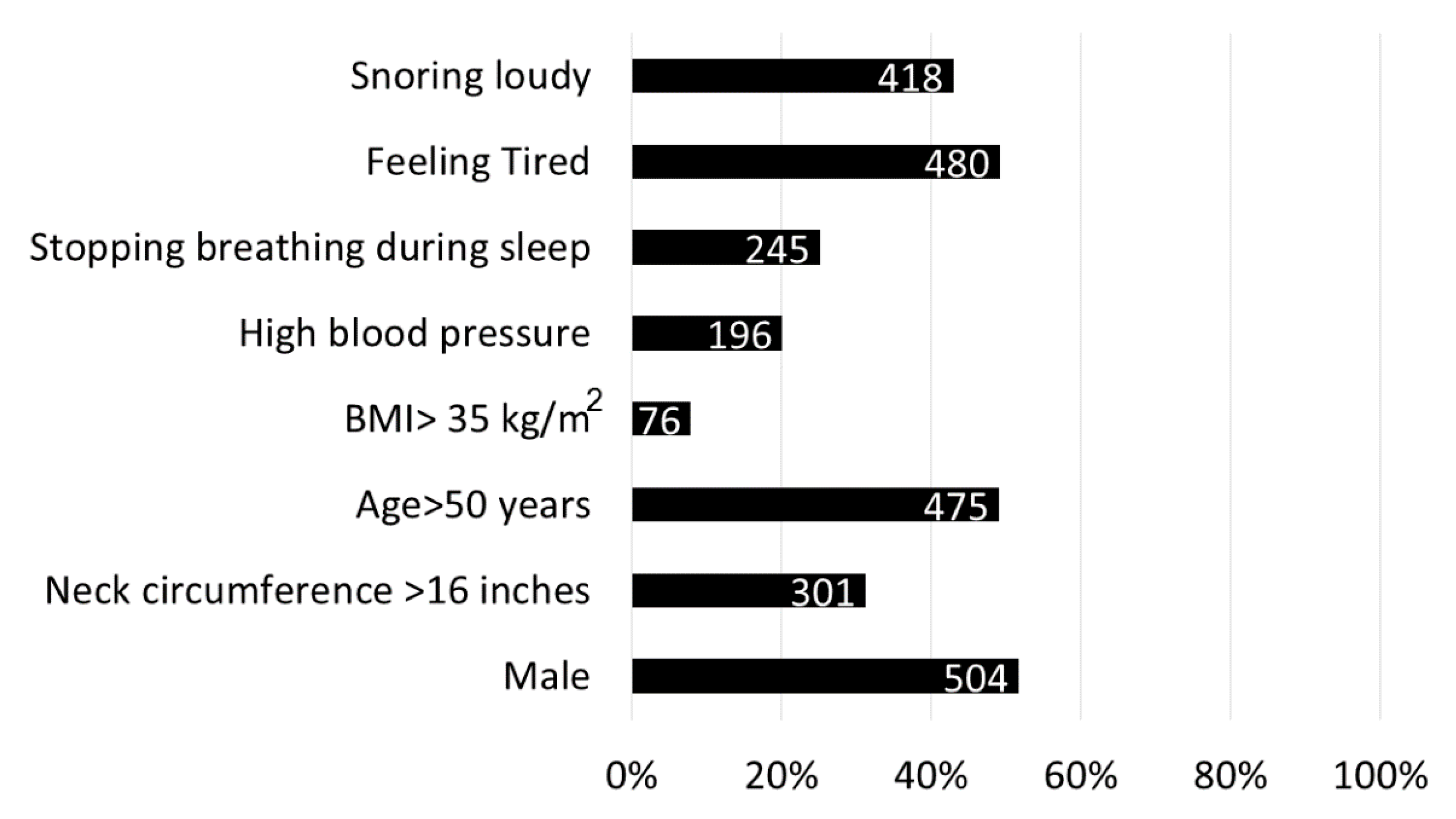
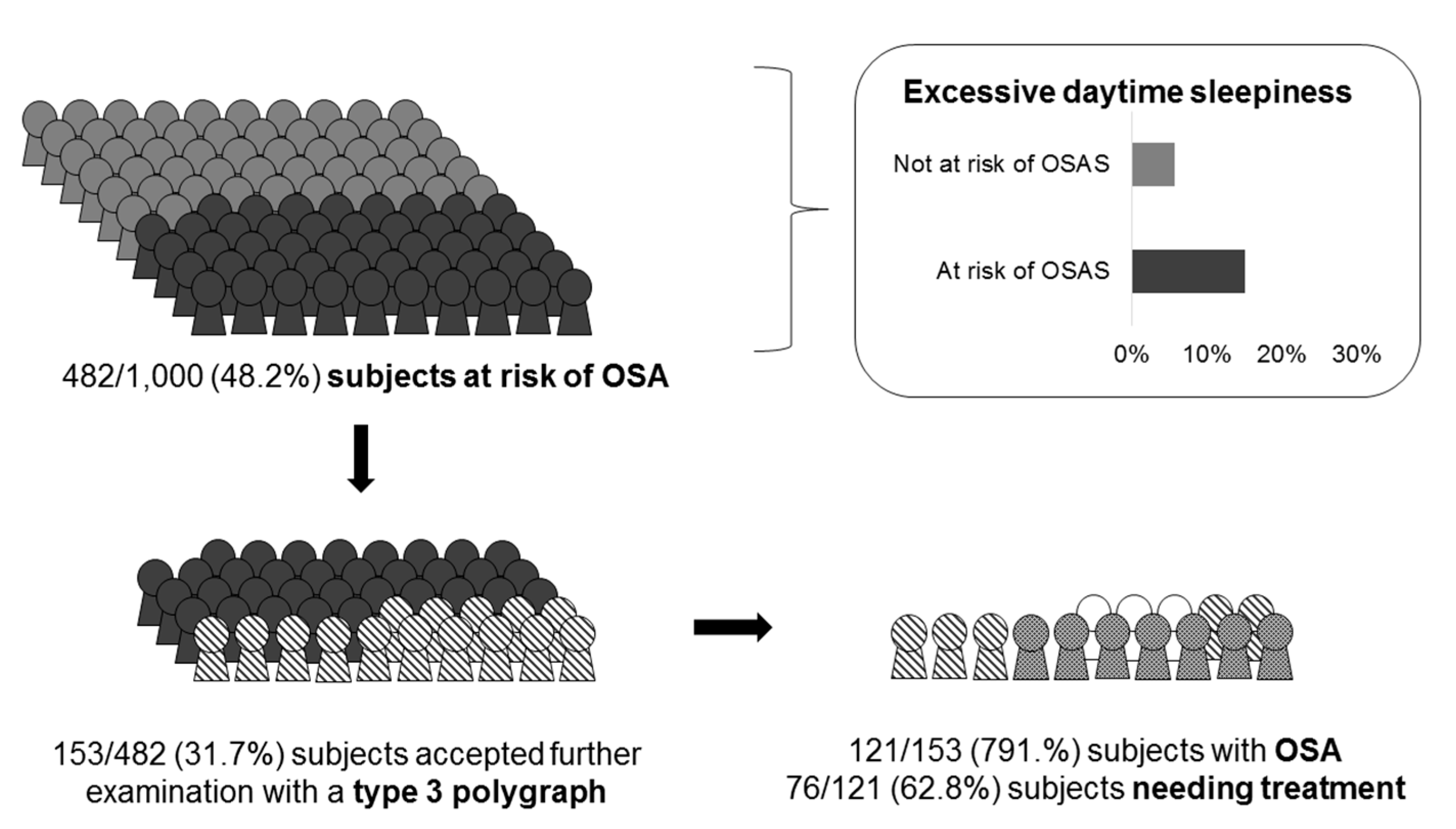
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Racineux, J.L. Epidemiological definition of obstructive sleep apnea syndrome. Rev. Neurol. 2003, 159, 88–90. [Google Scholar]
- Cillo, J.E.; Thayer, S.; Dasheiff, R.M.; Finn, R. Relations between obstructive sleep apnea syndrome and specific cephalometric measurements, body mass index, and apnea-hypopnea index. J. Oral Maxillofac. Surg. 2012, 70, 78–83. [Google Scholar] [CrossRef]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.L.D.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef]
- Garvey, J.F.; Taylor, C.T.; McNicholas, W.T. Cardiovascular disease in obstructive sleep apnoea syndrome: The role of intermittent hypoxia and inflammation. Eur. Respir. J. 2009, 33, 195–205. [Google Scholar] [CrossRef]
- Peppard, P.E.; Young, T.; Barnet, J.H.; Palta, M.; Hagen, E.W.; Hla, K.M. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 2013, 177, 1006–1014. [Google Scholar] [CrossRef]
- Trzepizur, W.; Gagnadoux, F. Epidemiology of obstructive sleep apnoea syndrome. Rev. Mal. Respir. 2014, 31, 68–77. [Google Scholar]
- Altree, T.; Bartlett, D.J.; Marshall, N.; Hoyos, C.; Phillips, C.; Berry, C.; Serinel, Y.; Wong, K.K.W.; Yee, B.; Grunstein, R.; et al. Predictors of weight loss in obesity and obstructive sleep apnoea. J. Sleep Res. 2019, 28, e12913. [Google Scholar]
- Salvador, J.; Iriarte, J.; Silva, C.; Gómez Ambrosi, J.; Díez Caballero, A.; Frühbeck, G. The obstructive sleep apnoea syndrome in obesity: A conspirator in the shadow. Rev. Med. Univ. Navarra 2004, 48, 55–62. [Google Scholar] [PubMed]
- Gibson, G.J. Obstructive sleep apnoea syndrome: Underestimated and undertreated. Br. Med. Bull. 2004, 72, 49–65. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, A.C.T.; Martinez, D.; Vasconcelos, L.F.T.; Gonçalves, S.C.; Lenz, M.D.C.; Fuchs, S.C.; Gus, M.; De Abreu-Silva, E.O.; Moreira, L.B.; Fuchs, F.D. Diagnosis of obstructive sleep apnea syndrome and its outcomes with home portable monitoring. Chest 2009, 135, 330–336. [Google Scholar] [CrossRef] [PubMed]
- Su, S.; Baroody, F.M.; Kohrman, M.; Suskind, D. A comparison of polysomnography and a portable home sleep study in the diagnosis of obstructive sleep apnea syndrome. Otolaryngol. Head Neck Surg. 2004, 131, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Álvarez, M.L.; Terán-Santos, J.; Ordax Carbajo, E.; Cordero-Guevara, J.A.; Navazo-Egüia, A.I.; Kheirandish-Gozal, L.; Gozal, D. Reliability of home respiratory polygraphy for the diagnosis of sleep apnea in children. Chest 2015, 147, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.Y.; Chen, P.Y.; Chuang, L.P.; Chen, N.H.; Tu, Y.K.; Hsieh, Y.J.; Wang, Y.C.; Guilleminault, C. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: A bivariate meta-analysis. Sleep Med. Rev. 2017, 36, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Amra, B.; Rahmati, B.; Soltaninejad, F.; Feizi, A. Screening questionnaires for obstructive sleep apnea: An updated systematic review. Oman Med. J. 2018, 33, 184–192. [Google Scholar] [CrossRef]
- Johns, M.W. Daytime sleepiness, snoring, and obstructive sleep apnea; The Epworth Sleepiness Scale. Chest 1993, 103, 30–36. [Google Scholar] [CrossRef]
- Kim, B.; Lee, E.M.; Chung, Y.S.; Kim, W.S.; Lee, S.A. The utility of three screening questionnaires for obstructive sleep apnea in a sleep clinic setting. Yonsei Med. J. 2015, 56, 84–90. [Google Scholar] [CrossRef]
- Nagappa, M.; Liao, P.; Wong, J.; Auckley, D.; Ramachandran, S.K.; Memtsoudis, S.; Mokhlesi, B.; Chung, F. Validation of the stop-bang questionnaire as a screening tool for obstructive sleep apnea among different populations: A systematic review and meta-Analysis. PLoS ONE 2015, 10, 14–36. [Google Scholar] [CrossRef]
- Nagappa, M.; Patra, J.; Wong, J.; Subramani, Y.; Singh, M.; Ho, G.; Wong, D.T.; Chung, F. Association of STOP-Bang Questionnaire as a Screening Tool for Sleep Apnea and Postoperative Complications: A Systematic Review and Bayesian Meta-analysis of Prospective and Retrospective Cohort Studies. Anesth. Analg. 2017, 125, 1301–1308. [Google Scholar] [CrossRef]
- Chung, F.; Subramanyam, R.; Liao, P.; Sasaki, E.; Shapiro, C.; Sun, Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br. J. Anaesth. 2012, 108, 68–75. [Google Scholar] [CrossRef]
- Chung, F.; Yegneswaran, B.; Liao, P.; Chung, S.A.; Vairavanathan, S.; Islam, S.; Khajehdehi, A.; Shapiro, C.M. STOP questionnaire: A tool to screen patients for obstructive sleep apnea. Anesthesiology 2008, 108, 12–21. [Google Scholar] [CrossRef]
- Tan, A.; Yin, J.D.C.; Tan, L.W.L.; van Dam, R.M.; Cheung, Y.Y.; Lee, C.H. Predicting obstructive sleep apnea using the STOP-Bang questionnaire in the general population. Sleep Med. 2016, 27, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Bignotti, D.; De Stefani, A.D.; Mezzofranco, L.; Bruno, G.; Gracco, A. Multidisciplinary approach in a 12-year-old patient affected by severe obstructive sleep apnea: A case-report. Sleep Med. Res. 2019, 10, 103–107. [Google Scholar] [CrossRef]
- De Stefani, A.; Bruno, G.; Mezzofranco, L.; Perri, A.; Marchese Ragona, R.; Gracco, A. Multidisciplinary ent-orthodontic treatment in a hypertensive patient affected by severe OSAS. ORAL Implantol. 2018, 11, 59–63. [Google Scholar]
- Levrini, L. Italian recommendations on dental support in the treatment of adult obstructive sleep apnea syndrome (OSAS). Ann. Stomatol. (Roma). 2015, 6, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Bailey, D.R. Oral evaluation and upper airway anatomy associated with snoring and obstructive sleep apnea. Dent. Clin. N. Am. 2001, 45, 15–32. [Google Scholar]
- Gracco, A.; Bruno, G.; De Stefani, A.; Marchese Ragona, R.; Stellini, E. Combined orthodontic and surgical treatment in a 8-years-old patient affected by severe OSA: A case-report. J. Clin. Pediatr. Dent. 2018, 42, 79–84. [Google Scholar] [CrossRef]
- Saglam-Aydinatay, B.; Uysal, S.; Taner, T. Facilitators and barriers to referral compliance among dental patients with increased risk of obstructive sleep apnea. Acta Odontol. Scand. 2018, 76, 86–91. [Google Scholar] [CrossRef]
- Fietze, I.; Laharnar, N.; Obst, A.; Ewert, R.; Felix, S.B.; Garcia, C.; Gläser, S.; Glos, M.; Schmidt, C.O.; Stubbe, B.; et al. Prevalence and association analysis of obstructive sleep apnea with gender and age differences—Results of SHIP-Trend. J. Sleep Res. 2019, 28, e12770. [Google Scholar] [CrossRef]
- Simou, E.; Britton, J.; Leonardi-Bee, J. Alcohol and the risk of sleep apnoea: A systematic review and meta-analysis. Sleep Med. 2018, 42, 38–46. [Google Scholar] [CrossRef]
- Crivellin, G.; Bruno, G.; De Stefani, A.; Mazzoli, A.; Mandolini, M.; Brunzini, A.; Gracco, A. Strength distribution on TMJ using mandibular advancement device for OSAS treatment: A Finite Element study. Dental Cadmos. 2018, 86, 757–764. [Google Scholar] [CrossRef]
- Bruno, G.; De Stefani, A.; Conte, E.; Caragiuli, M.; Mandolini, M.; Landi, D.; Gracco, A. A procedure for analyzing mandible roto-translation induced by Mandibular Advancement Devices. Materials 2020, 13, 1826. [Google Scholar] [CrossRef] [PubMed]
| N of subjects | 1000 |
| Age, years: median (IQR) | 50 (40–59) |
| Sex: n(%) | |
| Male | 514 (51.4) |
| Female | 486 (48.6) |
| Weight, kg: median (IQR) | 74 (62–84) |
| BMI, kg/m2: median (IQR) | 25.0 (22.3–28.5) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lonia, L.; Scalese, M.; Rossato, G.; Bruno, G.; Zalunardo, F.; De Stefani, A.; Gracco, A. Validity of the STOP-Bang Questionnaire in Identifying OSA in a Dental Patient Cohort. Medicina 2020, 56, 324. https://doi.org/10.3390/medicina56070324
Lonia L, Scalese M, Rossato G, Bruno G, Zalunardo F, De Stefani A, Gracco A. Validity of the STOP-Bang Questionnaire in Identifying OSA in a Dental Patient Cohort. Medicina. 2020; 56(7):324. https://doi.org/10.3390/medicina56070324
Chicago/Turabian StyleLonia, Letizia, Marco Scalese, Gianluca Rossato, Giovanni Bruno, Francesca Zalunardo, Alberto De Stefani, and Antonio Gracco. 2020. "Validity of the STOP-Bang Questionnaire in Identifying OSA in a Dental Patient Cohort" Medicina 56, no. 7: 324. https://doi.org/10.3390/medicina56070324
APA StyleLonia, L., Scalese, M., Rossato, G., Bruno, G., Zalunardo, F., De Stefani, A., & Gracco, A. (2020). Validity of the STOP-Bang Questionnaire in Identifying OSA in a Dental Patient Cohort. Medicina, 56(7), 324. https://doi.org/10.3390/medicina56070324









