Prognostic Factors for All-Cause Mortality in Thai Patients with Fragility Fracture of Hip: Comorbidities and Laboratory Evaluations
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
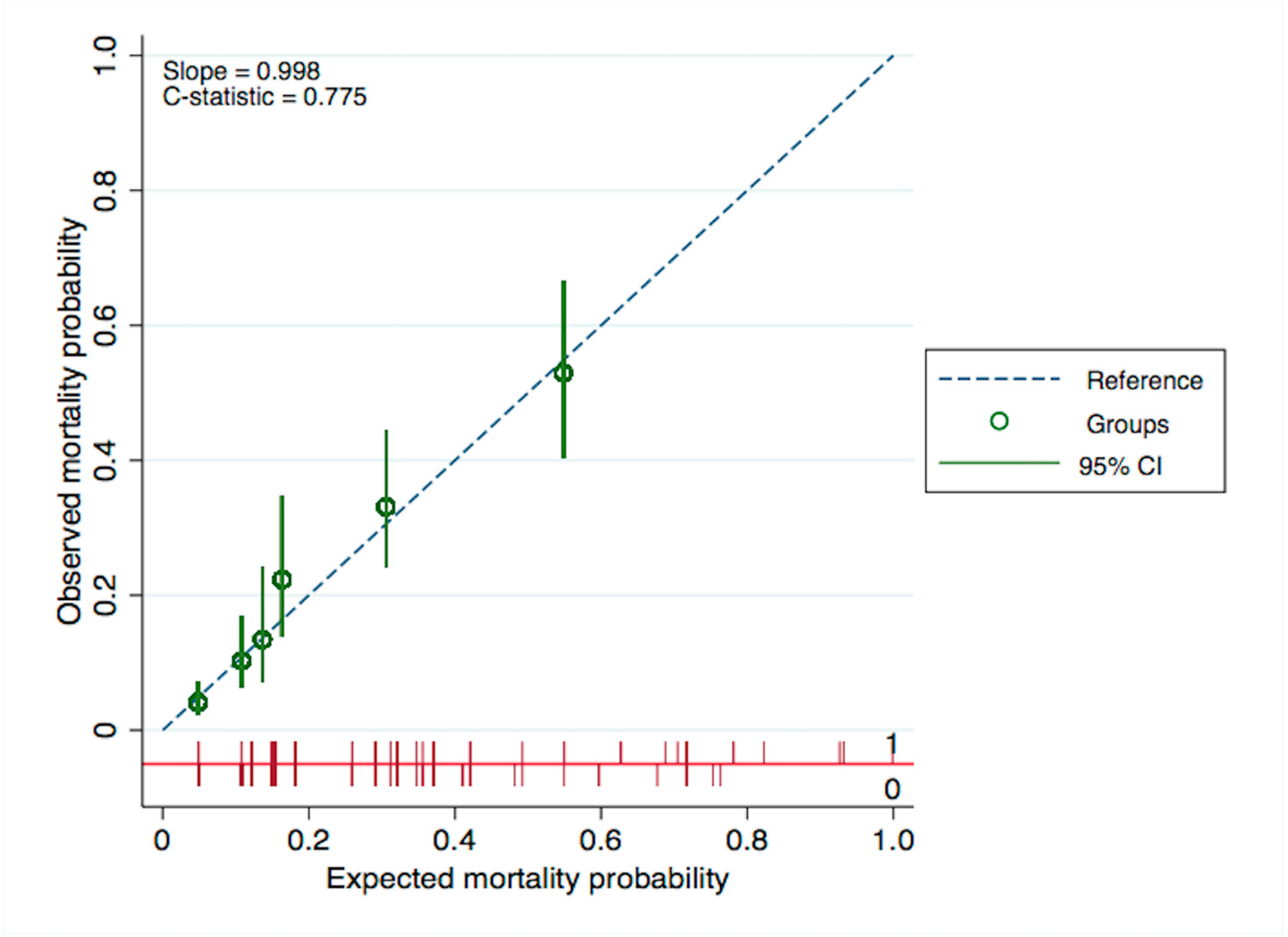
2.2. Statistical Analysis
3. Results
4. Discussions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hartholt, K.A.; van Beeck, E.F.; Polinder, S.; van der Velde, N.; van Lieshout, E.M.M.; Panneman, M.J.M.; van der Cammen, T.J.M.; Patka, P. Societal Consequences of Falls in the Older Population: Injuries, Healthcare Costs, and Long-Term Reduced Quality of Life. J. Trauma: Inj. Infect. Crit. Care 2011, 71, 748–753. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Campion, G.; Melton, L.J., III. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992, 2, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Nijmeijer, W.S.; Folbert, E.C.; Vermeer, M.; Slaets, J.P.; Hegeman, J.H. Prediction of early mortality following hip fracture surgery in frail elderly: The Almelo Hip Fracture Score (AHFS). Injury 2016, 47, 2138–2143. [Google Scholar] [CrossRef] [PubMed]
- Tarantino, U.; Cannata, G.; Lecce, D.; Celi, M.; Cerocchi, I.; Iundusi, R. Incidence of fragility fractures. Aging Clin. Exp. Res. 2007, 19, 7–11. [Google Scholar]
- Abrahamsen, B.; van Staa, T.; Ariely, R.; Olson, M.; Cooper, C. Excess mortality following hip fracture: A systematic epidemiological review. Osteoporos. Int. 2009, 20, 1633–1650. [Google Scholar] [CrossRef]
- Gullberg, B.; Johnell, O.; Kanis, J.A. World-wide Projections for Hip Fracture. Osteoporos. Int. 1997, 7, 407–413. [Google Scholar] [CrossRef]
- Ferguson, K.B.; Halai, M.; Winter, A.; Elswood, T.; Smith, R.; Hutchison, J.D.; Holt, G. National audits of hip fractures: Are yearly audits required? Injury 2016, 47, 439–443. [Google Scholar] [CrossRef]
- Voeten, S.C.; Krijnen, P.; Voeten, D.M.; Hegeman, J.H.; Wouters, M.W.J.M.; Schipper, I.B. Quality indicators for hip fracture care, a systematic review. Osteoporos. Int. 2018, 29, 1963–1985. [Google Scholar] [CrossRef]
- Freeman, C.; Todd, C.; Camilleri-Ferrant, C.; Laxton, C.; Murrell, P.; Palmer, C.R.; Parker, M.; Payne, B.; Rushton, N. Quality improvement for patients with hip fracture: Experience from a multi-site audit. Qual. Saf. Health Care 2002, 11, 239–245. [Google Scholar] [CrossRef]
- Haleem, S.; Lutchman, L.; Mayahi, R.; Grice, J.E.; Parker, M.J. Mortality following hip fracture: Trends and geographical variations over the last 40 years. Injury 2008, 39, 1157–1163. [Google Scholar] [CrossRef]
- Jürisson, M.; Raag, M.; Kallikorm, R.; Lember, M.; Uusküla, A. The impact of hip fracture on mortality in Estonia: A retrospective population-based cohort study. BMC Musculoskelet. Disord. 2017, 18, 243. [Google Scholar] [CrossRef] [PubMed]
- Vosoughi, A.R.; Emami, M.J.; Pourabbas, B.; Mahdaviazad, H. Factors increasing mortality of the elderly following hip fracture surgery: Role of body mass index, age, and smoking. Musculoskelet. Surg. 2017, 101, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Sun, T.; Liu, Z. Excess mortality of 1 year in elderly hip fracture patients compared with the general population in Beijing, China. Arch. Osteoporos. 2016, 11, 35. [Google Scholar] [CrossRef] [PubMed]
- von Friesendorff, M.; McGuigan, F.E.; Wizert, A.; Rogmark, C.; Holmberg, A.H.; Woolf, A.D.; Akesson, K. Hip fracture, mortality risk, and cause of death over two decades. Osteoporos. Int. 2016, 27, 2945–2953. [Google Scholar] [CrossRef] [PubMed]
- Man, L.p.; Ho, A.W.; Wong, S.H. Excess mortality for operated geriatric hip fracture in Hong Kong. Hong Kong Med. J. 2016, 22, 6–10. [Google Scholar] [CrossRef]
- Maxwell, M.J.; Moran, C.G.; Moppett, I.K. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br. J. Anaesth. 2008, 101, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, A.; Ozkan, Y.; Akgöz, S.; Yalçýn, N.; Ozdemir, R.M.; Aykut, S. The risk factors for mortality in elderly patients with hip fractures: Postoperative one-year results. Singap. Med J. 2010, 51, 137–143. [Google Scholar]
- Khan, M.A.A.; Hossain, F.S.; Ahmed, I.; Muthukumar, N.; Mohsen, A. Predictors of early mortality after hip fracture surgery. Int. Orthop. 2013, 37, 2119–2124. [Google Scholar] [CrossRef]
- Aranguren-Ruiz, M.I.; Acha-Arrieta, M.V.; de Tejerina, J.C.-F.; Arteaga-Mazuelas, M.; Jarne-Betrán, V.; Arnáez-Solis, R. Risk Factors for Mortality After Surgery of Osteoporotic Hip Fracture in Patients Over 65 Years of Age. Rev. Esp. Cir. Ortop Traumatol. 2017, 61, 185–192. [Google Scholar] [CrossRef]
- Heyes, G.J.; Tucker, A.; Marley, D.; Foster, A. Predictors for 1-year mortality following hip fracture: A retrospective review of 465 consecutive patients. Eur. J. Trauma Emerg. Surg. 2017, 43, 113–119. [Google Scholar] [CrossRef]
- Sofu, H.; Ucpunar, H.; Camurcu, Y.; Duman, S.; Konya, M.N.; Gursu, S.; Sahin, V. Predictive factors for early hospital readmission and 1-year mortality in elder patients following surgical treatment of a hip fracture. Turk. J. Trauma Emerg. Surg. 2017, 23, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Endo, A.; Baer, H.J.; Nagao, M.; Weaver, M.J. Prediction Model of In-Hospital Mortality After Hip Fracture Surgery. J. Orthop. Trauma 2018, 32, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Lo, L.W.T.; Yanling, X.; Chou, A.; Howe, T.S.; Allen, J.C.; Koh, J.S.B. End-Stage Renal Failure Is an Independent Risk Factor for 1-Year Mortality After Hip Fracture Surgery. Geriatr. Orthop. Surg. Rehabil. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Reig, J.; Marín, J.S.; Martínez, J.F.; Beltrán, D.O.; López, J.M.; Rico, J.Q. Prognostic factors and predictive model for in-hospital mortality following hip fractures in the elderly. Chin. J. Traumatol. 2018, 21, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Karres, J.; Kieviet, N.; Eerenberg, J.-P.; Vrouenraets, B.C. Predicting Early Mortality After Hip Fracture Surgery. J. Orthop. Trauma 2018, 32, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Temiz, A.; Ersozlu, S. Admission Neutrophile to Lymphocyte Ratio and Postoperative Mortality in Elderly Hip Fracture Patients. Turk. J. Trauma Emerg. Surg. 2019, 25, 71–74. [Google Scholar] [CrossRef]
- Traven, S.A.; Reeves, R.A.; Althoff, A.D.; Slone, H.S.; Walton, Z.J. New Five-Factor Modified Frailty Index Predicts Morbidity and Mortality in Geriatric Hip Fractures. J. Orthop. Trauma 2019, 33, 319–323. [Google Scholar] [CrossRef]
- Chao, C.-T.; Yang, R.-S.; Huang, W.-J.; Tsai, K.-S.; Chan, D.-C. Risk Factors for Poor Functional Recovery, Mortality, Recurrent Fractures, and Falls Among Patients Participating in a Fracture Liaison Service Program. J. Am. Med Dir. Assoc. 2019, 20, 1129–1136.e1. [Google Scholar] [CrossRef]
- Belangero, W.D.; Barla, J.D.; Bergalli, D.H.R.; Salazar, C.M.O.; Fernandez, D.S.; Vivar, M.A.M.; Zylberberg, A.; Carabelli, G.S.; Kfuri, M. Nutrition and Inflammation Influence 1-Year Mortality of Surgically Treated Elderly Intertrochanteric Fractures: A Prospective International Multicenter Case Series. Geriatr. Orthop. Surg. Rehabil. 2019, 10. [Google Scholar] [CrossRef]
- Whitehouse, M.R.; Berstock, J.R.; Kelly, M.B.; Gregson, C.L.; Judge, A.; Sayers, A.; Chesser, T.J. Higher 30-day mortality associated with the use of intramedullary nails compared with sliding hip screws for the treatment of trochanteric hip fractures. Bone Jt. J. 2019, 83–91. [Google Scholar] [CrossRef]
- Yoo, J.; Lee, J.S.; Kim, S.; Kim, B.S.; Choi, H.; Song, D.Y.; Kim, W.B.; Won, C.W. Length of hospital stay after hip fracture surgery and 1-year mortality. Osteoporos. Int. 2018, 30, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Norring-Agerskov, D.; Bathum, L.; Pedersen, O.B.; Abrahamsen, B.; Lauritzen, J.B.; Jørgensen, N.R.; Jørgensen, H.L. Biochemical markers of inflammation are associated with increased mortality in hip fracture patients: The Bispebjerg Hip Fracture Biobank. Aging Clin. Exp. Res. 2019, 31, 1727–1734. [Google Scholar] [CrossRef] [PubMed]
- Guzón-Illescas, O.; Fernandez, E.P.; Villarias, N.C.; Donate, F.J.Q.; Peña, M.; Alonso-Blas, C.; García-Vadillo, A.; Mazzucchelli, R. Mortality after osteoporotic hip fracture: Incidence, trends, and associated factors. J. Orthop. Surg. Res. 2019, 14, 203. [Google Scholar] [CrossRef] [PubMed]
- Vaseenon, T.; Luevitoonvechkij, S.; Wongtriratanachai, P.; Rojanasthien, S. Long-Term Mortality After Osteoporotic Hip Fracture in Chiang Mai, Thailand. J. Clin. Densitom. 2010, 13, 63–67. [Google Scholar] [CrossRef]
- Chaysri, R.; Leerapun, T.; Klunklin, K.; Chiewchantanakit, S.; Luevitoonvechkij, S.; Rojanasthien, S. Factors related to mortality after osteoporotic hip fracture treatment at Chiang Mai University Hospital, Thailand, during 2006 and 2007. J. Med Assoc. Thail. 2015, 98, 59–64. [Google Scholar]
- Chariyalertsak, S.; Suriyawongpisal, P.; Thakkinstain, A. Mortality after hip fractures in Thailand. Int. Orthop. 2001, 25, 294–297. [Google Scholar] [CrossRef]
- Chang, W.; Lv, H.; Feng, C.; Yuwen, P.; Wei, N.; Chen, W.; Zhang, Y. Preventable risk factors of mortality after hip fracture surgery: Systematic review and meta-analysis. Int. J. Surg. 2018, 52, 320–328. [Google Scholar] [CrossRef]
- Stijacic-Cenzer, I.; Tang, V.; Boscardin, W.J.; Smith, A.K.; Ritchie, C.; Wallhagen, M.I.; Espaldon, R.; E Covinsky, K. One-Year Mortality After Hip Fracture: Development and Validation of a Prognostic Index. J. Am. Geriatr. Soc. 2016, 64, 1863–1868. [Google Scholar] [CrossRef]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G.M. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. BMJ 2015, 350, g7594. [Google Scholar] [CrossRef]
- Madley-Dowd, P.; Hughes, R.; Tilling, K.; Heron, J. The proportion of missing data should not be used to guide decisions on multiple imputation. J. Clin. Epidemiol. 2019, 110, 63–73. [Google Scholar] [CrossRef]
- Vittinghoff, E.; McCulloch, C.E. Relaxing the Rule of Ten Events per Variable in Logistic and Cox Regression. Am. J. Epidemiol. 2007, 165, 710–718. [Google Scholar] [CrossRef] [PubMed]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef]
- Peduzzi, P.; Concato, J.; Feinstein, A.R.; Holford, T.R. Importance of events per independent variable in proportional hazards regression analysis II. Accuracy and precision of regression estimates. J. Clin. Epidemiol. 1995, 48, 1503–1510. [Google Scholar] [CrossRef]
- Concato, J.; Peduzzi, P.; Holford, T.R.; Feinstein, A.R. Importance of events per independent variable in proportional hazards analysis I. Background, goals, and general strategy. J. Clin. Epidemiol. 1995, 48, 1495–1501. [Google Scholar] [CrossRef]
- Härstedt, M.; Rogmark, C.; Sutton, R.; Melander, O.; Fedorowski, A. Impact of comorbidity on 6-month hospital readmission and mortality after hip fracture surgery. Injury 2015, 46, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Tolppanen, A.-M.; Taipale, H.; Tanskanen, A.; Tiihonen, L.; Hartikainen, S. Comparison of predictors of hip fracture and mortality after hip fracture in community-dwellers with and without Alzheimer’s disease—Exposure-matched cohort study. BMC Geriatr. 2016, 16, 204. [Google Scholar] [CrossRef]
- Baker, N.L.; Cook, M.N.; Arrighi, M.H.; Bullock, R. Hip fracture risk and subsequent mortality among Alzheimer’s disease patients in the United Kingdom, 1988–2007. Age Ageing 2010, 40, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Seitz, D.P.; Gill, S.S.; Gruneir, A.; Austin, P.C.; Anderson, G.M.; Bell, C.M.; Rochon, P.A. Effects of Dementia on Postoperative Outcomes of Older Adults With Hip Fractures: A Population-Based Study. J. Am. Med Dir. Assoc. 2014, 15, 334–341. [Google Scholar] [CrossRef]
- Friedman, S.M.; Mendelson, D.A. Epidemiology of Fragility Fractures. Clin. Geriatr. Med. 2014, 30, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Stauder, R.; Valent, P.; Theurl, I. Anemia at older age: Etiologies, clinical implications, and management. Blood 2018, 131, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Webster, A.C.; Nagler, E.V.; Morton, R.L.; Masson, P. Chronic Kidney Disease. Lancet 2017, 389, 1238–1252. [Google Scholar] [CrossRef]
- Lameire, N.; Van Biesen, W.; Vanholder, R. Acute renal failure. Lancet 2005, 365, 417–430. [Google Scholar] [CrossRef]
- Prommik, P.; Kolk, H.; Sarap, P.; Puuorg, E.; Harak, E.; Kukner, A.; Pääsuke, M.; Märtson, A. Estonian hip fracture data from 2009 to 2017: High rates of nonoperative management and high 1-year mortality. Acta Orthop. 2019, 90, 159–164. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Dead n, (%) (n = 108) | Alive n, (%) (n = 667) | p-Value |
|---|---|---|---|
| General Factors | |||
| Gender, n (%) | |||
| Male | 36 (33.33) | 178 (26.69) | 0.164 |
| Female | 72 (66.67) | 489 (73.31) | |
| Age (years), Mean ± SD c | 81.63 ± 8.52 | 78.68 ± 9.65 | 0.003 |
| Age at admission ≥85 years, n (%) | 46 (42.59) | 188 (28.19) | 0.003 |
| BMI a at admission (kg/m2), Mean ± SD c (n = 769) | 19.82 ± 3.13 | 21.18 ± 4.05 | <0.001 |
| BMI a at admission ≥25 kg/m2, n (%) (n = 769) | 8 (7.48) | 96 (14.50) | 0.048 |
| Pre-fracture walking ability by oneself, n (%) (n = 606) | 72 (91.14) | 504 (95.64) | 0.095 |
| Living with family, n (%) (n = 774) | 108 (100) | 663 (99.55) | 1.000 |
| Comorbidities | |||
| Active malignancy, n (%) | 12 (11.11) | 9 (1.35) | <0.001 |
| Dementia or Alzheimer’s disease, n (%) | 13 (12.04) | 31 (4.65) | 0.005 |
| Hemiplegia, n (%) | 2 (1.85) | 34 (5.10) | 0.213 |
| Hypertension, n (%) | 69 (63.89) | 448 (67.17) | 0.510 |
| History of myocardial infraction, n (%) | 4 (3.70) | 11 (1.65) | 0.144 |
| Congestive heart failure, n (%) | 2 (1.85) | 5 (0.75) | 0.254 |
| Atrial fibrillation, n (%) | 9 (8.33) | 32 (4.80) | 0.160 |
| Chronic obstructive pulmonary disorder, n (%) | 18 (16.67) | 49 (7.35) | 0.003 |
| Diabetes mellitus, n (%) | 36 (33.33) | 185 (27.74) | 0.251 |
| Asthma, n (%) | 1 (0.93) | 16 (2.40) | 0.492 |
| Rheumatologic disease, n (%) | 15 (13.89) | 73 (10.94) | 0.413 |
| Cerebrovascular disease, n (%) | 14 (12.96) | 79 (11.34) | 0.750 |
| Current pneumonia, n (%) | 1 (0.93) | 5 (0.75) | 0.595 |
| Peptic ulcer, n (%) | 3 (2.78) | 9 (1.35) | 0.227 |
| ASA score b, n (%) (n = 688) | <0.001 | ||
| Class 1 | 0 (0) | 7 (1.15) | |
| Class 2 | 29 (36.71) | 397 (65.19) | |
| Class 3 | 49 (62.03) | 202 (33.17) | |
| Class 4 | 1 (1.27) | 3 (0.49) | |
| Type of fracture, n (%) | |||
| Fractured neck of femur | 32 (29.63) | 255 (38.23) | 0.107 |
| Intertrochanteric fracture | 76 (70.37) | 412 (61.77) | |
| Investigative Factors | |||
| Admission hemoglobin (g/dL), Mean ± SD c | 9.93 ± 1.89 | 10.85 ± 1.83 | <0.001 |
| Admission hemoglobin concentration <10 g/dL, n (%) | 57 (52.78) | 202 (30.28) | <0.001 |
| Admission glomerular filtration rate (mL/min/1.73 m2), Mean ± SD c | 48.38 ± 56.90 | 67.31 ± 41.77 | <0.001 |
| Admission glomerular filtration rate <30 mL/min/1.73 m2, n (%) | 36 (33.33) | 87 (13.04) | <0.001 |
| Admission serum albumin level (g/dL), Mean ± SD c (n = 151) | 3.30 ± 0.63 | 3.58 ± 0.51 | 0.018 |
| Neutrophil to lymphocyte ratio, Median ± IQR d | 7.36 ± 5.74 | 6.08 ± 5.90 | 0.276 |
| Neutrophil to lymphocyte ratio ≥4.7, n (%) | 73 (67.59) | 433 (64.92) | 0.663 |
| Treatment Factors, n (%) | <0.001 | ||
| Nonoperative treatment | 29 (26.85) | 58 (8.70) | |
| Dynamic hip screw | 15 (13.89) | 100 (14.99) | |
| Cephalomedullary nailing | 36 (33.33) | 262 (39.28) | |
| Stable angle plating | 2 (1.85) | 15 (2.25) | |
| Multiple screw fixation | 2 (1.85) | 38 (5.70) | |
| Arthroplasty | 24 (22.22) | 194 (29.09) | |
| Time from injury to operation (days), Median ± IQR d (n = 688) | 9 ± 10 | 8 ± 8 | 0.020 |
| Time from injury to operation ≥48 h, n (%) (n = 688) | 78 (98.73) | 586 (96.22) | 0.508 |
| Peripheral nerve or spinal block, n (%) (n = 688) | 20 (25.32) | 146 (23.97) | 0.781 |
| Characteristics | Hazard Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| General Factors | |||
| Male | 1.36 | 0.91–2.03 | 0.131 |
| Age at admission ≥85 years | 1.83 | 1.25–2.69 | 0.002 |
| BMI a at admission ≥25 kg/m2 | 0.50 | 0.24–1.02 | 0.056 |
| Pre-fracture walking ability by oneself | 0.52 | 0.24–1.13 | 0.101 |
| Comorbidities | |||
| Active malignancy | 6.82 | 3.73–12.47 | <0.001 |
| Dementia or Alzheimer ’s disease | 2.63 | 1.47–4.70 | 0.001 |
| Hemiplegia | 0.35 | 0.09–1.41 | 0.139 |
| Hypertension | 0.88 | 0.59–1.30 | 0.520 |
| History of myocardial infraction | 2.02 | 0.74–5.48 | 0.168 |
| Congestive heart failure | 2.34 | 0.57–9.47 | 0.234 |
| Atrial fibrillation | 1.82 | 0.92–3.60 | 0.086 |
| Chronic obstructive pulmonary disorder | 2.26 | 1.36–3.75 | 0.002 |
| Diabetes mellitus | 1.29 | 0.86–1.92 | 0.216 |
| Asthma | 0.44 | 0.06–3.18 | 0.419 |
| Rheumatologic disease | 1.31 | 0.76–2.25 | 0.336 |
| Cerebrovascular disease | 1.05 | 0.60–1.85 | 0.854 |
| Current pneumonia | 1.34 | 0.19–9.60 | 0.771 |
| Peptic ulcer | 2.26 | 0.72–7.12 | 0.164 |
| ASA score b > 2 | 3.27 | 2.07–5.17 | <0.001 |
| Fracture neck of femur | 0.67 | 0.45–1.01 | 0.062 |
| Investigative Factors | |||
| Admission hemoglobin concentration <10 g/dL | 2.38 | 1.63–3.47 | <0.001 |
| Admission glomerular filtration rate <30 mL/min/1.73 m2 | 3.10 | 2.07–4.62 | <0.001 |
| Admission serum albumin level <3.5 g/dL | 1.49 | 0.68–3.27 | 0.318 |
| Neutrophil to lymphocyte ratio ≥4.7 | 1.14 | 0.76–1.70 | 0.534 |
| Treatment Factors | |||
| Nonoperative treatment | 3.53 | 2.30–5.40 | <0.001 |
| Time from injury to operation ≥48 h | 2.48 | 0.35–17.85 | 0.366 |
| Peripheral nerve or spinal block | 1.09 | 0.66–1.80 | 0.742 |
| Characteristics | Hazard Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Nonoperative treatment | 3.29 | 2.13–5.08 | <0.001 |
| Admission glomerular filtration rate <30 mL/min/1.73 m2 | 3.40 | 2.21–5.21 | <0.001 |
| Admission hemoglobin concentration <10 g/dL | 2.31 | 1.57–3.40 | <0.001 |
| Chronic obstructive pulmonary disorder | 2.63 | 1.56–4.42 | <0.001 |
| Dementia or Alzheimer’s disease | 4.06 | 2.22–7.41 | <0.001 |
| Active malignancy | 6.80 | 3.68–12.59 | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Atthakomol, P.; Manosroi, W.; Phinyo, P.; Pipanmekaporn, T.; Vaseenon, T.; Rojanasthien, S. Prognostic Factors for All-Cause Mortality in Thai Patients with Fragility Fracture of Hip: Comorbidities and Laboratory Evaluations. Medicina 2020, 56, 311. https://doi.org/10.3390/medicina56060311
Atthakomol P, Manosroi W, Phinyo P, Pipanmekaporn T, Vaseenon T, Rojanasthien S. Prognostic Factors for All-Cause Mortality in Thai Patients with Fragility Fracture of Hip: Comorbidities and Laboratory Evaluations. Medicina. 2020; 56(6):311. https://doi.org/10.3390/medicina56060311
Chicago/Turabian StyleAtthakomol, Pichitchai, Worapaka Manosroi, Phichayut Phinyo, Tanyong Pipanmekaporn, Tanawat Vaseenon, and Sattaya Rojanasthien. 2020. "Prognostic Factors for All-Cause Mortality in Thai Patients with Fragility Fracture of Hip: Comorbidities and Laboratory Evaluations" Medicina 56, no. 6: 311. https://doi.org/10.3390/medicina56060311
APA StyleAtthakomol, P., Manosroi, W., Phinyo, P., Pipanmekaporn, T., Vaseenon, T., & Rojanasthien, S. (2020). Prognostic Factors for All-Cause Mortality in Thai Patients with Fragility Fracture of Hip: Comorbidities and Laboratory Evaluations. Medicina, 56(6), 311. https://doi.org/10.3390/medicina56060311





