Dropped Head Syndrome Attenuation by Hybrid Assistive Limb: A Preliminary Study of Three Cases on Cervical Alignment during Walking
Abstract
1. Introduction
2. Materials and Methods
2.1. Case Presentations
2.2. HAL Gait Training
2.3. Assessment of Cervical Alignment during Gait
2.4. Measurement and Data Processing
2.5. Statistical Analyses
3. Results
3.1. Immediate Effects
3.2. Lasting Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics Statement
References
- Sharan, A.D.; Kaye, D.; Charles Malveaux, W.M.; Daniel Riew, K. Dropped head syndrome: Etiology and management. J. Am. Acad. Orthop. Surg. 2012, 20, 766–774. [Google Scholar] [CrossRef] [PubMed]
- Drain, J.P.; Virk, S.S.; Nikhil, J.; Elizabeth, Y. Dropped Head Syndrome A Systematic Review. Clin. Spine Surg. 2019, 32, 423–429. [Google Scholar] [CrossRef]
- Katz, J.S.; Wolfe, G.I.; Burns, D.K.; Bryan, W.W.; Fleckenstein, J.L.; Barohn, R.J. Isolated neck extensor myopathy: A common cause of dropped head syndrome. Neurology 1996, 46, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.N.; Nagaoka, M.; Hayashi, Y.; Yonezawa, I. Pathological analysis of dropped head syndrome caused by various diagnosis. Based on surface EMG findings and responses to physiotherapy. Clin. Neurol. 2013, 53, 430–438. (In Japanese) [Google Scholar]
- Mace, Y.; Yahia, M.; Rannou, F.; Leferve-Colau, M.M.; Poiraudeau, S.; Revel, M. Value intensive rehabilitation in dropped head syndrome. Ann. Readapt. Med. Phys. 2005, 48, 207–211. (In French) [Google Scholar] [PubMed]
- Deneufgermain, O.; Solau-Gervais, E.; Bera-Louville, A.; Vermersch, P.; Hachulla, E.; Flipo, R.M. Dropped head syndrome: Report of two cases. Rev. Med. Interne 2005, 26, 61–64. (In French) [Google Scholar] [CrossRef] [PubMed]
- Bahnof, R. The dropped head syndrome: Rehabilitation of cervical focal myositis. Disabil. Rehabil. 1999, 21, 563–565. [Google Scholar] [CrossRef]
- Gourie-Devi, M.; Nalini, A.; Sandhya, S. Early or late appearance of “dropped head syndrome” in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry 2003, 74, 683–686. [Google Scholar] [CrossRef]
- Igawa, T.; Isogai, N.; Suzuki, A.; Kusano, S.; Sasao, Y.; Nishiyama, M.; Funao, H.; Ishii, K. Establishment of a novel rehabilitation program for patients with dropped head syndrome: Short and intensive rehabilitation (SHAiR) program. J. Clin. Neurosci. 2020, 73, 57–61. [Google Scholar] [CrossRef]
- Miura, K.; Koda, M.; Kadone, H.; Kubota, S.; Shimizu, Y.; Kumagai, H.; Nagashima, K.; Mataki, K.; Fujii, K.; Noguchi, H.; et al. Gait training using a hybrid assistive limb (HAL) attenuates head drop: A case report. J. Clin. Neurosci. 2018, 52, 141–144. [Google Scholar] [CrossRef]
- Kawamoto, H.; Kamibayashi, K.; Nakata, Y.; Yamawaki, K.; Ariyasu, R.; Sankai, Y.; Sakane, M.; Eguchi, K.; Ochiai, N. Pilot study of locomotion improvement using hybrid assistive limb in chronic stroke patients. BMC Neurol. 2013, 13, 141. [Google Scholar] [CrossRef] [PubMed]
- Sczesny-Kaiser, M.; Trost, R.; Aach, M.; Schildhauer, T.A.; Schwenkreis, P.; Tegenthoff, M. A Randomized and Controlled Crossover Study Investigating the Improvement of Walking and Posture Functions in Chronic Stroke Patients Using HAL Exoskeleton—The HALESTRO Study (HAL-Exoskeleton STROke Study). Front. Neurosci. 2019, 13, 259. [Google Scholar] [CrossRef] [PubMed]
- Kubota, S.; Abe, T.; Kadone, H.; Shimizu, Y.; Funayama, T.; Watanabe, H.; Marushima, A.; Koda, M.; Hada, Y.; Sankai, Y.; et al. Hybrid assistive limb (HAL) treatment for patients with severe thoracic myelopathy due to ossification of the posterior longitudinal ligament (OPLL) in the postoperative acute/subacute phase: A clinical trial. J. Spinal Cord Med. 2018, 42, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Aach, M.; Cruciger, O.; Sczesny-Kaiser, M.; Höffken, O.; Meindl, R.C.; Tegenthoff, M.; Schwenkreis, P.; Sankai, Y.; Schildhauer, T.A. Voluntary driven exoskeleton as a new tool for rehabilitation in chronic spinal cord injury: A pilot study. Spine J. 2014, 14, 2847–2853. [Google Scholar] [CrossRef]
- Jansen, O.; Schildhauer, T.; Meindl, R.C.; Tegenthoff, M.; Schwenkreis, P.; Sczesny-Kaiser, M.; Grasmücke, D.; Fisahn, C.; Aach, M. Functional Outcome of Neurologic-ControlledHAL-Exoskeletal Neurorehabilitationin Chronic Spinal Cord Injury: A PilotWith One Year Treatment and VariableTreatment Frequency. Glob. Spine J. 2017, 7, 735–743. [Google Scholar] [CrossRef]
- Shimizu, Y.; Kadone, H.; Kubota, S.; Suzuki, K.; Abe, T.; Ueno, T.; Soma, Y.; Sankai, Y.; Hada, Y.; Yamazaki, M. Voluntary Ambulation by Upper Limb-Triggered HAL® in Patients with Complete Quadri/Paraplegia Due to Chronic Spinal Cord Injury. Front. Neurosci. 2017, 11. [Google Scholar] [CrossRef]
- Jansen, O.; Grasmuecke, D.; Meindl, R.C.; Tegenthoff, M.; Schwenkreis, P.; Sczesny-Kaiser, M.; Wessling, M.; Schildhauer, T.A.; Fisahn, C.; Aach, M. Hybrid Assistive Limb Exoskeleton HAL in the Rehabilitation of Chronic Spinal Cord Injury: Proof of Concept; the Results in 21 Patients. World Neurosurg. 2018, 110, e73–e78. [Google Scholar] [CrossRef]
- Matsuda, M.; Mataki, Y.; Mutsuzaki, H.; Yoshikawa, K.; Takahashi, K.; Enomoto, K.; Sano, K.; Mizukami, M.; Tomita, K.; Ohguro, H.; et al. Immediate effects of a single session of robot-assisted gait training using Hybrid Assistive Limb (HAL) for cerebral palsy. J. Phys. Ther. Sci. 2018, 30, 207–212. [Google Scholar] [CrossRef]
- Miura, K.; Kadone, H.; Koda, M.; Kumagai, H.; Nagashima, K.; Fujii, K.; Noguchi, H.; Funayama, T.; Abe, T.; Furuya, T.; et al. Three-dimensional gait analysis reveals dynamic alignment change in a patient with dropped head syndrome: A case report. J. Clin. Neurosci. 2018, 48, 106–108. [Google Scholar] [CrossRef] [PubMed]
- Miura, K.; Kadone, H.; Koda, M.; Abe, T.; Funayama, T.; Noguchi, H.; Mataki, K.; Nagashima, K.; Kumagai, H.; Shibao, Y.; et al. Thoracic kyphosis and pelvic anteversion in patients with adult spinal deformity increase while walking: Analyses of dynamic alignment change using a three-dimensional gait motion analysis system. Eur. Spine J. 2020, 29, 840–848. [Google Scholar] [CrossRef]
- Shiba, Y.; Taneichi, H.; Inami, S.; Moridaira, H.; Takeuchi, D.; Nohara, Y. Dynamic global sagittal alignment evaluated by three-dimensionalgait analysis in patients with degenerative lumbar kyphoscoliosis. Eur. Spine J. 2016, 25, 2572–2579. [Google Scholar] [CrossRef]
- Iodice, P.; Cesinaro, S.; Romani, G.L.; Pezzulo, G. More gain less pain: Balance control learning shifts the activation patterns of leg and neck muscles and increases muscular parsimony. Exp. Brain Res. 2015, 233, 2103–2114. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, Y.; Kadone, H.; Kubota, S.; Ueno, T.; Sankai, Y.; Hada, Y.; Yamazaki, M. Voluntary Elbow Extension-Flexion Using Single Joint Hybrid Assistive Limb (HAL) for Patients of Spastic Cerebral Palsy: Two Cases Report. Front. Neurol. 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Tagliaferri, S.D.; Miller, C.; Owen, P.J.; Mitchell, U.H.; Brisby, H.; FitzGibbon, B.M.; Masse-Alarie, H.; Van Oosterwijck, J.; Belavy, D.L. Domains of Chronic Low Back Pain and Assessing Treatment Effectiveness: A Clinical Perspective. Pain Pract. 2019, 20, 211–225. [Google Scholar] [CrossRef] [PubMed]

| Case | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Age (y) | 75 | 66 | 81 |
| Sex | M | M | F |
| Height (cm) | 169 | 162 | 145 |
| Weight (kg) | 60 | 49 | 37 |
| Head-C7 SVA (mm) | +115 | +117 | +8.2 |
| Cervical Kyphosis | 40° | 37° | 0.3° |
| T1 slope | 39° | 0° | 11° |
| C7 SVA (mm) | −21 | −64 | 4.9 |
| Lumbar Lordosis | 40° | 63° | 28° |
| Number of HAL sessions | 10 | 10 | 10 |
| Frequency of HAL sessions | (1st) 5/week (2nd) 1/month | 1/week | 1/2–3 weeks |
| Duration of HAL sessions | (1st) 2 weeks (2nd) 10 months | 10 weeks | 6 months |
| Case | Outcome | Predictor | Post-Hoc | ||
|---|---|---|---|---|---|
| (Interaction) | PRE-POST | Lap | PRE-POST | ||
| Case 1 (1st) | C2C7 SVA | 0.9081 | 1.57 × 10−5 | 0.0347 | n/a |
| CT kyphosis | 0.8772 | 1.97 × 10−5 | 0.0331 | n/a | |
| C7 SVA | 0.00789 | n/a | n/a | 5.60 × 10−8 | |
| Case 1 (2nd) | C2C7 SVA | 0.000403 | n/a | n/a | 0.0024 |
| CT kyphosis | 0.000247 | n/a | n/a | 0.0013 | |
| C7 SVA | 0.297684 | 0.000237 | 0.490349 | n/a | |
| Case 2 | C2C7 SVA | 0.0453 | n/a | n/a | 0.9523 |
| CT kyphosis | 0.0339 | n/a | n/a | 0.8481 | |
| C7 SVA | 0.0184 | n/a | n/a | 0.1486 | |
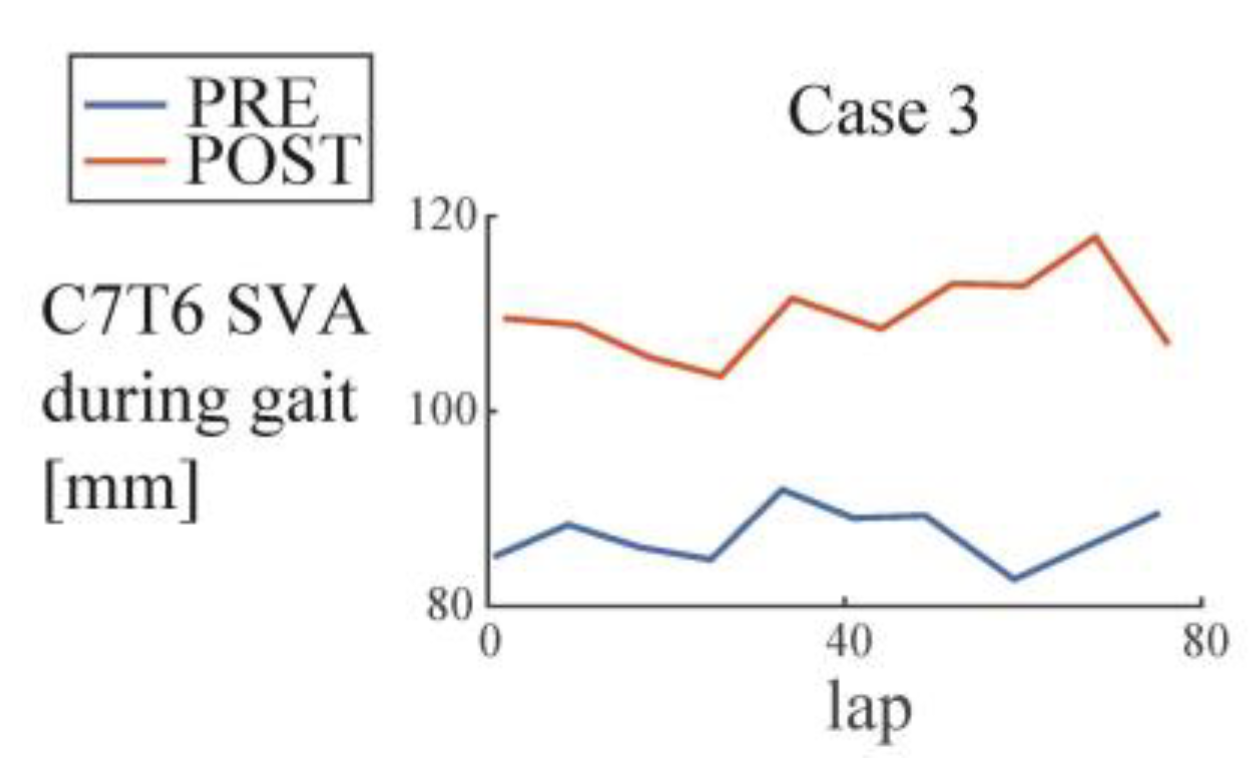
| Case 3 | C2C7 SVA | 0.299 | 0.448 | 5.68 × 10−5 | n/a |
| CT kyphosis | 0.9250 | 4.11 × 10−7 | 2.72 × 10−6 | n/a | |
| C7 SVA | 0.45344 | 0.23803 | 0.00127 | n/a | |
| C7T6 SVA | 0.305 | 4.67 × 10−6 | 0.886 | n/a |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kadone, H.; Miura, K.; Kubota, S.; Abe, T.; Shimizu, Y.; Hada, Y.; Suzuki, K.; Sankai, Y.; Koda, M.; Yamazaki, M. Dropped Head Syndrome Attenuation by Hybrid Assistive Limb: A Preliminary Study of Three Cases on Cervical Alignment during Walking. Medicina 2020, 56, 291. https://doi.org/10.3390/medicina56060291
Kadone H, Miura K, Kubota S, Abe T, Shimizu Y, Hada Y, Suzuki K, Sankai Y, Koda M, Yamazaki M. Dropped Head Syndrome Attenuation by Hybrid Assistive Limb: A Preliminary Study of Three Cases on Cervical Alignment during Walking. Medicina. 2020; 56(6):291. https://doi.org/10.3390/medicina56060291
Chicago/Turabian StyleKadone, Hideki, Kousei Miura, Shigeki Kubota, Tetsuya Abe, Yukiyo Shimizu, Yasushi Hada, Kenji Suzuki, Yoshiyuki Sankai, Masao Koda, and Masashi Yamazaki. 2020. "Dropped Head Syndrome Attenuation by Hybrid Assistive Limb: A Preliminary Study of Three Cases on Cervical Alignment during Walking" Medicina 56, no. 6: 291. https://doi.org/10.3390/medicina56060291
APA StyleKadone, H., Miura, K., Kubota, S., Abe, T., Shimizu, Y., Hada, Y., Suzuki, K., Sankai, Y., Koda, M., & Yamazaki, M. (2020). Dropped Head Syndrome Attenuation by Hybrid Assistive Limb: A Preliminary Study of Three Cases on Cervical Alignment during Walking. Medicina, 56(6), 291. https://doi.org/10.3390/medicina56060291





