Angiolipoma in the Head and Neck: Imaging, Diagnosis and Management
Abstract
1. Introduction
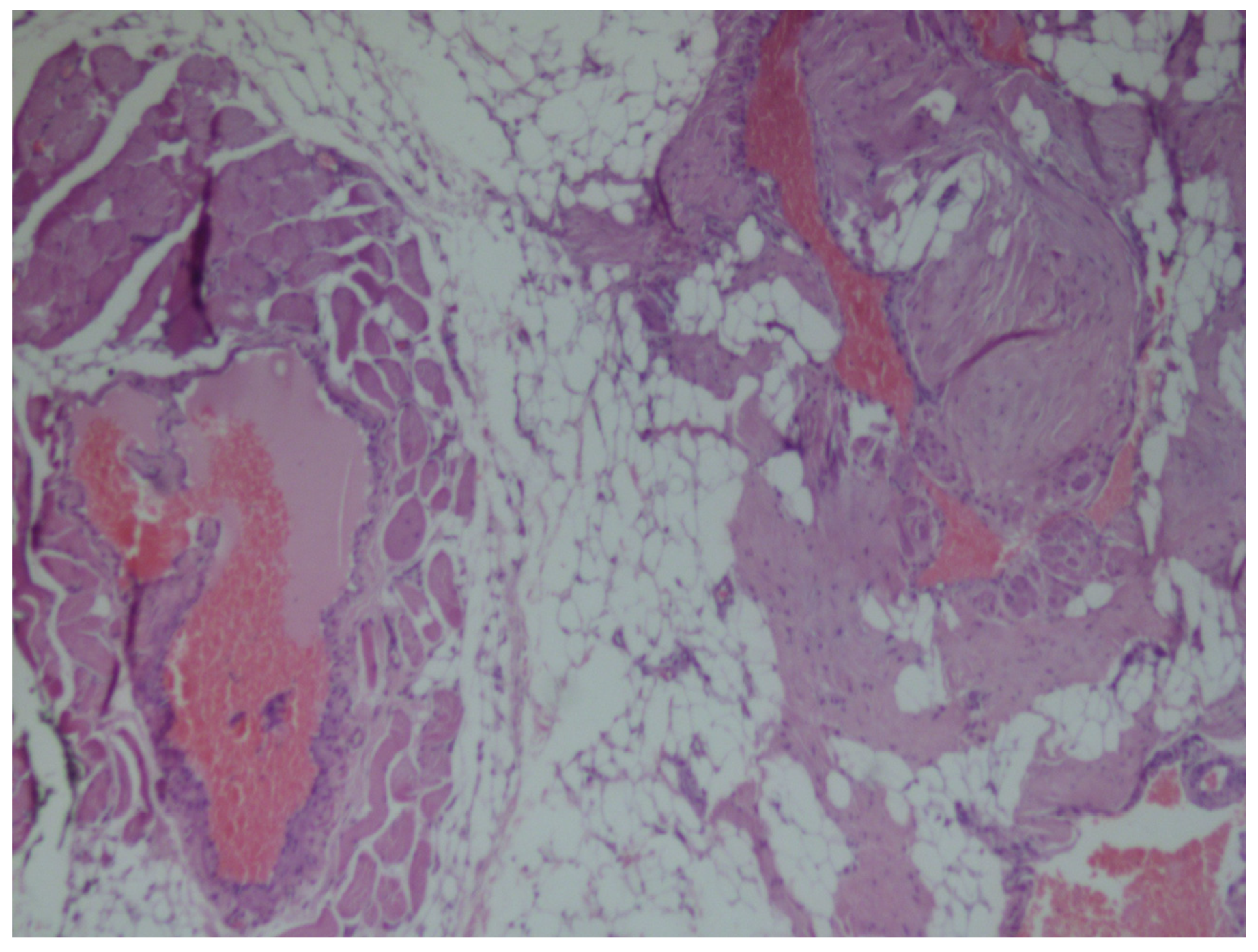
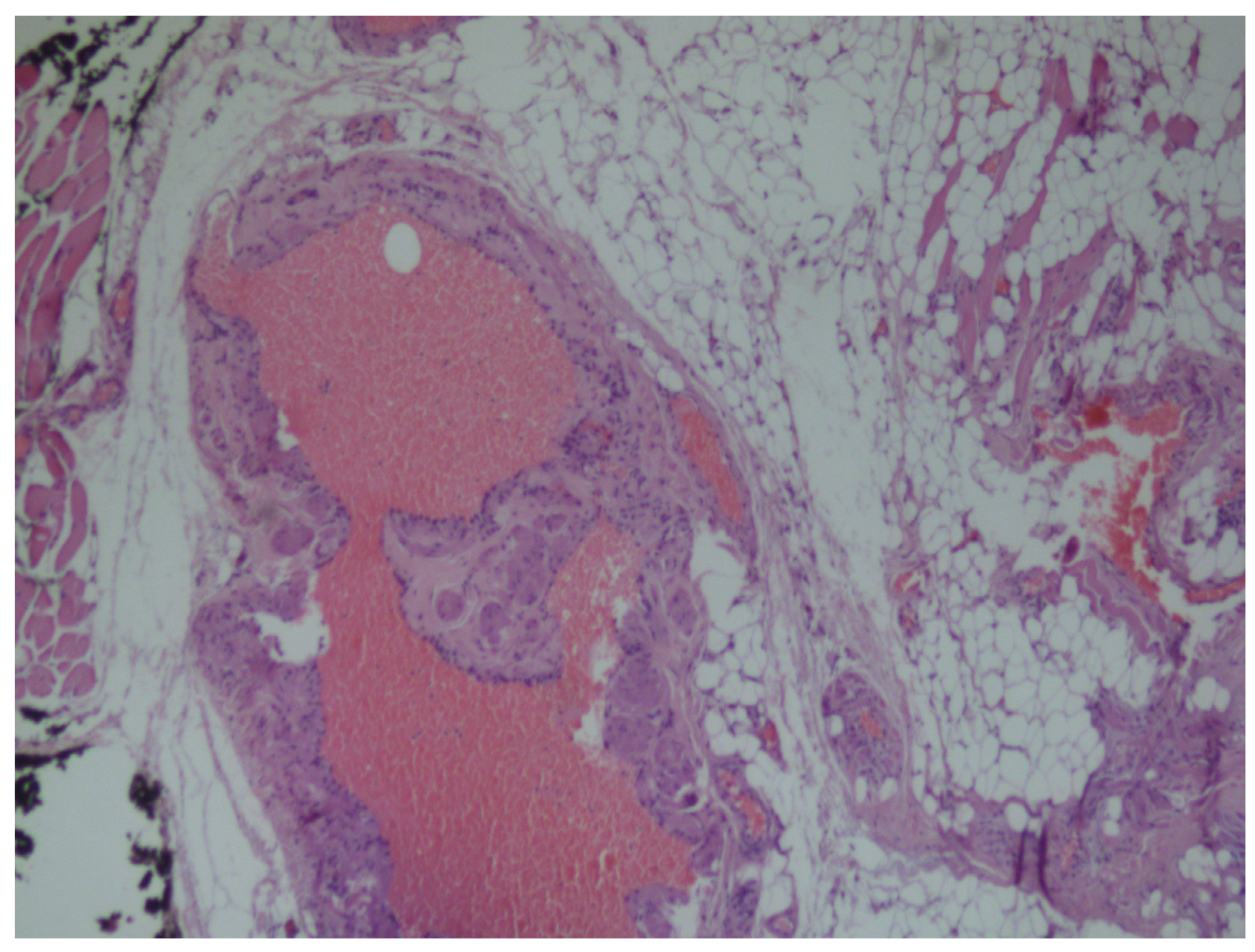
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Shah, V.S.; Harish, M.; Patel, J.R.; Shah, N. Infiltrating angiolipoma of the cheek. BMJ Case Rep. 2013. [Google Scholar] [CrossRef] [PubMed]
- Shahi, A.K.; Ash, H.; Chatterji, K.; Singh, R. Cellular infiltrative angiolipoma of cheek in an infant. Natl. J. Maxillofac. Surg. 2014, 5, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Campos, G.M.; Grandini, S.A.; Lopes, R.A. Angiolipoma of the cheek. Int. J. Oral Surg. 1980, 9, 486–490. [Google Scholar] [CrossRef]
- Aniceto, G.S.; Saez, R.S.; Peńin, A.G. Angiolipoma of the cheek: Report of a case. J. Oral Maxillofac. Surg. 1990, 48, 512–515. [Google Scholar] [CrossRef]
- Ali, M.H.; el-Zuebi, F. Angiolipoma of the cheek: Report of a case. J. Oral Maxillofac. Surg. 1996, 54, 213–215. [Google Scholar] [CrossRef]
- Brahney, C.P.; Aria, A.A.; Koval, M.H.; Najjar, T.A. Angiolipoma of the tongue: Report of case and review of literature. J. Oral Surg. 1981, 39, 451–453. [Google Scholar] [PubMed]
- Flaggert, J.J.; Heldt, L.V.; Keaton, W.M. Angiolipoma of the palate. Report of a case. Oral Surg. Oral Med. Oral Pathol. 1986, 61, 333–336. [Google Scholar] [CrossRef]
- Reilly, J.S.; Kelly, D.R.; Royal, S.A. Angiolipoma of the parotid: Case report and review. Laryngoscope 1988, 98, 818–821. [Google Scholar] [CrossRef] [PubMed]
- Hamdan, A.L.; Mahfoud, L.; Rifai, H.; Rameh, C.; Fuleihan, N. Infiltrative angiolipoma of the neck. Middle East J. Anesthesiol. 2011, 21, 433–434. [Google Scholar] [PubMed]
- Mesollela, M.; Di Martino, M.; Laguardia, M.; Galera, F.; Galli, V. Angiolipoma of the larynx. Otolaryngol. Head Neck Surg. 2007, 136, 142–143. [Google Scholar] [CrossRef] [PubMed]
- Furlong, M.A.; Fanburg-Smith, J.C.; Childers, E.L.B. Lipoma of the oral and maxillofacial region: Site and sub classification of 125 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2004, 98, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Búa, J.A.; Luáces, R.; Franco, F.L.; García-Rozado, A.; Escudero, J.C.; Capdevila, E.F.; López-Cedruún, J.L. Angiolipoma in head and neck: Report of two cases and review of the literature. Int. J. Oral Maxillofac. Surg. 2010, 39, 610–615. [Google Scholar]
- Hoeft, S.; Luettges, J.; Werner, J.A. Infiltrating angiolipoma of the M. temporalis. Auris Nasus Larynx 2000, 27, 265–269. [Google Scholar] [CrossRef]
- Saydam, L.; Bozkurt, M.K.; Ugur, M.B.; Ozcelik, T.; Kutluay, L. Angiolipoma of the neck: A case report. Ear Nose Throat J. 2005, 84, 375–377. [Google Scholar] [CrossRef]
- Auo, H.J.; Kang, J.M. Infiltrating angiolipoma of the nasopharynx: Adjacent to an aberrant internal carotid artery. Auris Nasus Larynx 2009, 36, 247–250. [Google Scholar] [CrossRef]
- Lin, J.J.; Lin, F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer 1974, 34, 720–727. [Google Scholar] [CrossRef]
- Gerard, N.; Schultz, D.A. Angiolipoma of the upper lip: Report of a case. J. Oral Maxillofac. Surg. 2009, 67, 1340–1341. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, B.; Prendergast, T.; Myers, E.M. Angiolipoma of the neck. Am. Surg. 2012, 78, 325–326. [Google Scholar]
- Altug, H.A.; Sahin, S.; Sencimen, M.; Dogan, N.; Erdogan, Ö. Non-infiltrating angiolipoma of the cheek: A case report and review of the literature. J. Oral Sci. 2009, 51, 137–139. [Google Scholar] [CrossRef]
- Alvi, A.; Garner, C.; Thomas, W. Angiolipoma of the head and neck. J. Otolaryngol. 1998, 27, 100–103. [Google Scholar] [PubMed]
- Yanase, S.; Nomura, J.; Matsumura, Y.; Kato, H.; Takeoka, T.; Imura, H.; Matsuura, R.; Nakanishi, K.; Tagawa, T. Angiolipoma of the cheek: A case report with a literature review. Asian J. Oral Maxillofac. Surg. 2011, 23, 35–37. [Google Scholar] [CrossRef]
- Blythe, J.; Pearce, O.J.; Tilley, E.A.; Brennan, P.A. Contemporary Use of Imaging Modalities in Neck Mass Evaluation. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2015, 23, 1–14. [Google Scholar] [CrossRef] [PubMed]



© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reiser, V.; Haj Yahya, B.; Chaushu, G.; Kaplan, I.; Hamzani, Y. Angiolipoma in the Head and Neck: Imaging, Diagnosis and Management. Medicina 2020, 56, 283. https://doi.org/10.3390/medicina56060283
Reiser V, Haj Yahya B, Chaushu G, Kaplan I, Hamzani Y. Angiolipoma in the Head and Neck: Imaging, Diagnosis and Management. Medicina. 2020; 56(6):283. https://doi.org/10.3390/medicina56060283
Chicago/Turabian StyleReiser, Vadim, Bahaa Haj Yahya, Gavriel Chaushu, Ilana Kaplan, and Yafit Hamzani. 2020. "Angiolipoma in the Head and Neck: Imaging, Diagnosis and Management" Medicina 56, no. 6: 283. https://doi.org/10.3390/medicina56060283
APA StyleReiser, V., Haj Yahya, B., Chaushu, G., Kaplan, I., & Hamzani, Y. (2020). Angiolipoma in the Head and Neck: Imaging, Diagnosis and Management. Medicina, 56(6), 283. https://doi.org/10.3390/medicina56060283






