Acute Disseminated Encephalomyelitis with Seizures and Myocarditis: A Fatal Triad
Abstract
1. Introductions
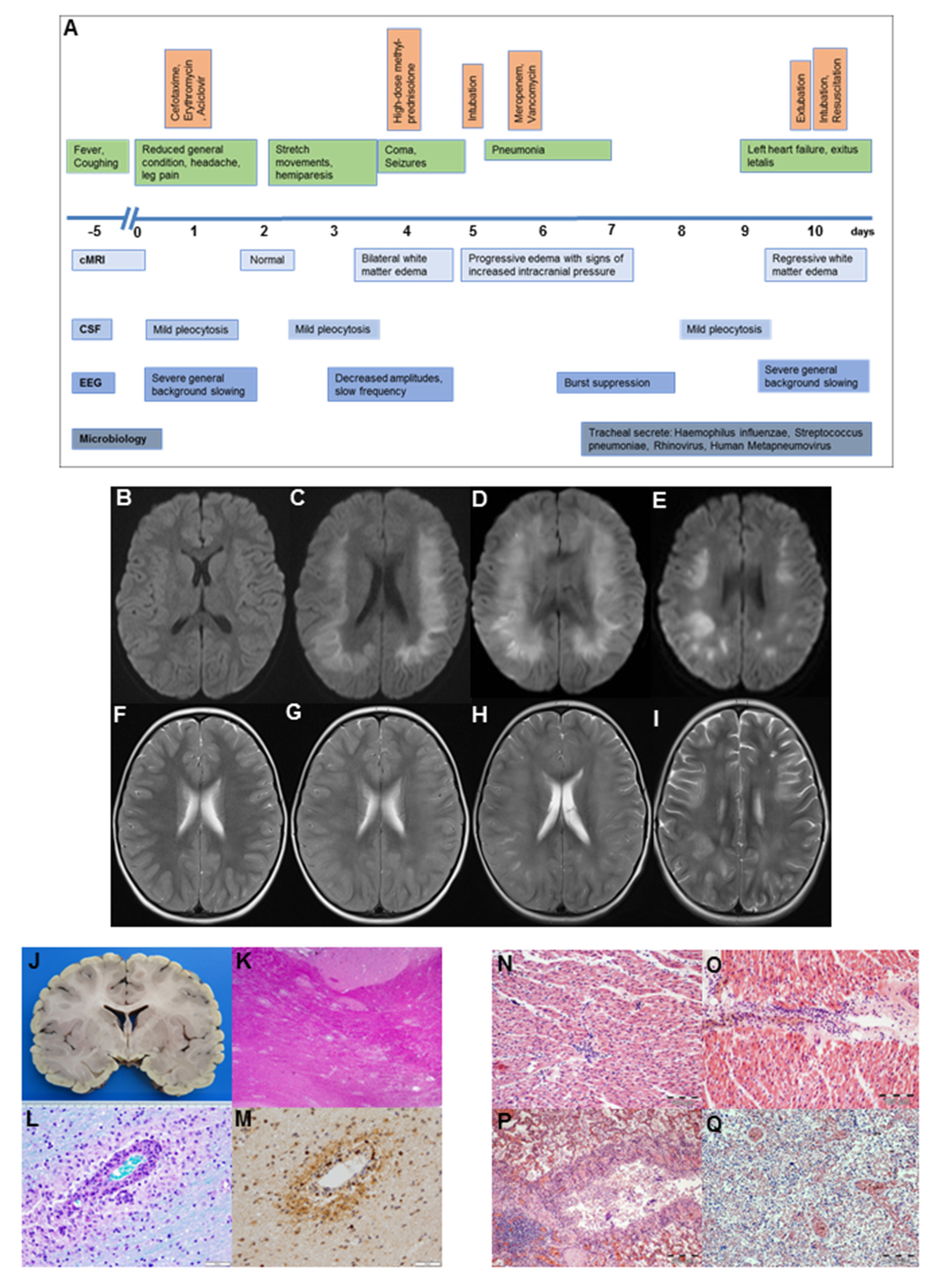
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dale, R.C.; de Sousa, C.; Chong, W.K.; Cox, T.C.S.; Harding, B.; Neville, B.G.R. Acute disseminated encephalomyelitis, multiphasic disseminated encephalomyelitis and multiple sclerosis in children. Brain 2000, 123, 2407–2422. [Google Scholar] [CrossRef] [PubMed]
- Mawhinney, E.; Watt, M.; McDonnell, G.V. Transient cardiomyopathy as the presenting feature of acute disseminated encephalomyelitis. Mult. Scler. 2009, 15, 1534–1536. [Google Scholar] [CrossRef] [PubMed]
- Werner, K.M.; Doshi, M.P. Atypical ADEM and Cardiogenic Shock in a 14-Year-Old Female. Pediatrics 2018, 142, 471. [Google Scholar]
- Tsunoda, I.; Sato, F.; Omura, S.; Fujita, M.; Sakiyama, N.; Park, A.-M. Three immune-mediated disease models induced by Theiler’s virus: Multiple sclerosis, seizures and myocarditis. Clin. Exp. Neuroimmunol. 2016, 7, 330–345. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.T. Acute disseminated Encephalopathy and progressive multifocal leukencephalopathy. In Neurology and Clinical Neuroscience; Schapira, A.H.V., Byrne, E., DiMauro, S., Frackowiak, R.S.J., Johnson, R.T., Mizuno, Y., Eds.; Mosby: Philadelphia, Pennsylvania, 2007; pp. 1057–1063. [Google Scholar]
- Burton, K.L.O.; Williams, T.A.; Catchpoole, S.E.; Brunsdon, R.K. Long-Term Neuropsychological Outcomes of Childhood Onset Acute Disseminated Encephalomyelitis (ADEM): A Meta-Analysis. Neuropsychol. Rev. 2017, 2, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Iype, M.; Kunju, P.A.M.; Saradakutty, G.; Anish, T.; Sreedharan, M.; Ahamed, S.M. Short term outcome of ADEM: Results from a retrospective cohort study from South India. Mult. Scler. Relat. Disord. 2017, 18, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Yae, Y.; Kawano, G.; Yokochi, T.; Imagi, T.; Akita, Y.; Ohbu, K.; Matsuishi, T. Fulminant acute disseminated encephalomyelitis in children. Brain Dev. 2019, 41, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Magun, R.; Verschoor, C.P.; Bowdish, D.M.E.; Provias, J. Mycoplasma pneumoniae, a trigger for Weston Hurst syndrome. Neurol. Neuroimmunol. Neuroinflamm. 2016, 3, e187. [Google Scholar] [CrossRef] [PubMed]
- Mardekian, S.K.; Fortuna, D.; Nix, A.; Bhatti, T.; Wiley, C.A.; Flanders, A.; Urtecho, J.; Sloane, J.; Ahmad, J.; Curtis, M. Severe human parechovirus type 3 myocarditis and encephalitis in an adolescent with hypogammaglobulinemia. Int. J. Infect. Dis. 2015, 36, 6–8. [Google Scholar] [CrossRef]
- Sagar, S.; Liu, P.P.; Cooper, L.T. Myocarditis. Lancet 2012, 379, 738–747. [Google Scholar] [CrossRef]
- Wybraniec, M.; Mizia-Stec, K.; Krzych, L. Stress cardiomyopathy: Yet another type of neurocardiogenic injury: ‘stress cardiomyopathy’. Cardiovasc. Pathol. 2014, 23, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Critchley, B.J.; Isalan, M.; Mielcarek, M. Neuro-Cardio Mechanisms in Huntington’s Disease and Other Neurodegenerative Disorders. Front. Physiol. 2018, 9, 559. [Google Scholar] [CrossRef] [PubMed]
- Kopelnik, A.; Zaroff, J.G. Neurocardiogenic injury in neurovascular disorders. Crit. Care Clin. 2006, 22, 733–752. [Google Scholar] [CrossRef]
- Robinson, C.P.; Busl, K.M. Neurologic Manifestations of Severe Respiratory Viral Contagions. Crit. Care Explor. 2020, 2, e0107. [Google Scholar] [CrossRef]
- Gerhauser, I.; Hansmann, F.; Ciurkiewicz, M.; Löscher, W.; Beineke, A. Facets of Theiler’s Murine Encephalomyelitis Virus-Induced Diseases: An Update. Int. J. Mol. Sci. 2019, 20, 448. [Google Scholar] [CrossRef] [PubMed]
- Kriesel, J.D.; Sibley, W.A. The case for rhinoviruses in the pathogenesis of multiple sclerosis. Mult. Scler. 2005, 11, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Thanh, D.T.M.; Lien, D.M.; Hanh, L.T.H. Myocarditis Related to Rhinovirus. Int. J. Cardiol. Res. 2017, 4, 78–81. [Google Scholar]
| 1 | 2 | 3 | 5 | 7 | 8 | 9 | 10 * | ||
|---|---|---|---|---|---|---|---|---|---|
| Blood | |||||||||
| White cell count | 109/L | 22 | 19 | 9 | 20 | 15 | 22 | 19 | 39 |
| CRP | mg/L | 9 | 12 | 7 | 4.55 | <1 | <1 | <1 | |
| PCT | ng/mL | 0.06 | 0.06 | 0.06 | 0.4 | 0.06 | 0.06 | 0.07 | 0.43 |
| CSF | |||||||||
| White cell count | 109/L | 97 | 95 | 94 | |||||
| Protein level | mg/L | 565 | 289 | 290 | |||||
| Lactate level | mmol/L | 2.7 | 2.0 | 2.5 | |||||
| Glucose level | mmol/L | 2.7 | 4.5 | 4.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lademann, H.; Bertsche, A.; Petzold, A.; Zack, F.; Büttner, A.; Däbritz, J.; Hauenstein, C.; Bahn, E.; Spang, C.; Reuter, D.; et al. Acute Disseminated Encephalomyelitis with Seizures and Myocarditis: A Fatal Triad. Medicina 2020, 56, 277. https://doi.org/10.3390/medicina56060277
Lademann H, Bertsche A, Petzold A, Zack F, Büttner A, Däbritz J, Hauenstein C, Bahn E, Spang C, Reuter D, et al. Acute Disseminated Encephalomyelitis with Seizures and Myocarditis: A Fatal Triad. Medicina. 2020; 56(6):277. https://doi.org/10.3390/medicina56060277
Chicago/Turabian StyleLademann, Hanne, Astrid Bertsche, Axel Petzold, Fred Zack, Andreas Büttner, Jan Däbritz, Christina Hauenstein, Erik Bahn, Christian Spang, Daniel Reuter, and et al. 2020. "Acute Disseminated Encephalomyelitis with Seizures and Myocarditis: A Fatal Triad" Medicina 56, no. 6: 277. https://doi.org/10.3390/medicina56060277
APA StyleLademann, H., Bertsche, A., Petzold, A., Zack, F., Büttner, A., Däbritz, J., Hauenstein, C., Bahn, E., Spang, C., Reuter, D., Warnke, P., & Ehler, J. (2020). Acute Disseminated Encephalomyelitis with Seizures and Myocarditis: A Fatal Triad. Medicina, 56(6), 277. https://doi.org/10.3390/medicina56060277





