1. Introduction
Class III skeletal deformities are the most frequent types of malocclusion requiring correction by orthognathic surgery [
1,
2]. Correction of skeletal Class III dentofacial deformities can be accomplished by maxillary advancement, mandibular setback, or bimaxillary surgery. Bimaxillary surgery with a simultaneous maxillary advancement and mandibular setback has become a common procedure as it provides a satisfactory facial appearance [
3], preserves the volume of the upper airways [
4] and is considered to be a stable procedure [
5,
6].
Mandibular osteotomies with consequent relocation and fixation of bony segments for the correction of skeletal dentofacial deformities can lead to condylar displacement and rotation within the glenoid fossa [
7,
8]. Condylar positional changes may develop due to several reasons, including ineffective interosseous fixation [
9,
10], misalignment of bone fragments [
11,
12], or tension in the surrounding muscles [
13]. Maxillary osteotomies may indirectly alter the position of the condyle within the glenoid fossa by causing the autorotation of the mandible [
14,
15]. Only a few previous studies reported on alterations of the condyle after the isolated maxillary surgery [
16,
17,
18,
19].
Altered condylar position in orthognathic surgery patients causes mechanical stress on the condylar surface, and subsequent condylar dimensional changes occur in the postoperative period as areas of bone apposition and resorption form. Depending on the extent to which bone is lost, condylar changes can be physiological, defined as condylar remodeling, or pathological—condylar resorption [
20,
21].
Altered functional load, which is due to orthognathic surgery-induced condylar displacement, can compromise condylar bone structure and, consequently, radiological signs of bone degeneration may be detected [
22,
23,
24,
25,
26]. Degenerative joint disease (DJD) is a process of tissue deterioration in which soft tissue, cartilage, and bone are converted into or replaced by inferior quality tissue [
23]. The normal osseous components of the temporomandibular joints exhibit smooth, rounded articular surfaces without evidence of subchondral defects. As DJD progresses, the onset of erosive lesions occurs in loaded areas, and late-stage changes include the formation of osteophytes and subchondral bone cysts [
25].
Condylar changes following the orthognathic surgery were mainly studied in skeletal Class II patients. The necessity of further studies, which utilize 3D images, volume rendering techniques and volume calculations in skeletal Class III patients has been recommended [
27]. Cone-beam computed tomography (CBCT) scans allow us to compute and superimpose three-dimensional (3D) reconstructions of the mandibular condyles [
28,
29,
30,
31]. Using this novel image modality, accurate quantitative analyses of postoperative condylar volumetric changes can be performed [
32,
33]. In addition, the CBCT provides multiplanar reformatted (MPR) images for accurate and reliable linear measurements and identification of condylar bone structural changes [
26,
34,
35,
36,
37].
The current study utilized cone-beam computed tomography to evaluate condylar positional, structural, and volumetric changes that may have occurred after bimaxillary or maxillary single-jaw orthognathic surgeries in skeletal Class III patients.
2. Materials and Methods
The database of all patients who received orthognathic surgery treatments from 2009 to 2018 at the Department of Maxillofacial Surgery of Rīga Stradiņš University, Latvia, was reviewed. The inclusion criteria comprised patients with a skeletal Class III malocclusion (cephalometric parameter: angle formed between the A point, Nasion point and B point (ANB angle) less than 2°) and those who had undergone bimaxillary (one-piece Le Fort I osteotomy for maxillary advancement and bilateral sagittal split osteotomy (BSSO) for mandibular setback) or single-jaw (one-piece Le Fort I osteotomy for maxillary advancement only) orthognathic surgery. Patients with syndromes, facial trauma, cleft lip and palate, signs and symptoms of temporomandibular joint disorders, or severe facial asymmetry (i.e., menton deviations of more than 4 mm from the facial midline) were excluded.
Subsequently, information about 69 eligible patients (138 condyles) was retrieved. CBCT images from after the surgery (T1) were missing for 11 patients in the bimaxillary surgery group and 14 patients in the single-jaw surgery group; full CBCT records were available for 44 patients (88 condyles). These patients were selected for the current study and comprised two study groups. The bimaxillary surgery group was composed of 28 patients (24 females and 4 males), and their mean age at the time of surgery was 23.8 ± 6.0 years. The maxillary single-jaw surgery group included 16 patients (8 females and 8 males), and their mean age at the time of surgery was 23.7 ± 5.1 years. During the BSSO procedure, the mandibular condyles were positioned using bi-vectoral seating method and fixed using a 2.0 mm miniplate and one positioning screw on each side. The mean amount of surgical movement for the maxillary advancement was 4.6 ± 1.0 mm and for the mandibular setback—4.8 ± 1.0 mm. The Le Fort I osteotomy was fixed using two 2.0 mm L-shaped miniplates on each side. The mean amount of maxillary advancement in single-jaw surgery group was 5.7 ± 1.4 mm. All patients underwent orthodontic treatment before and after surgery at the Department of Orthodontics of Rīga Stradiņš University, Latvia. The study was approved by the Ethical Committee of Rīga Stradiņš University (Ethical Committee Approval Nr. E-9(2), approval date: 27 Feb 2014), and written informed consent was obtained from all patients.
The CBCT images were obtained before surgery (0.8 ± 0.9 months), after surgery (0.6 ± 0.7 months), and at follow-up (13.1 ± 2.6 months). An i-CAT New Generation (Imaging Sciences International, Inc. Hatfield, PA, USA) CBCT machine was used for this, with patients seated in an upright position, their head in a natural position and teeth in maximum intercuspation. A standardized protocol was used for the equipment (voltage 120 kV; current 38 mA; FOV 17 cm; resolution 0.4 voxels; an approximate radiation dose of 36 μSv). The CBCT images were processed and analyzed using OsiriX MD 10.0.1 software, Pixmeo, Switzerland.
Two examiners performed the measurements. The first examiner, J.P. (Orthodontist) took linear, angular measurements and performed the cephalometric analysis. The first examiner was trained and calibrated by an experienced maxillofacial radiologist (L.N.) to identify condylar bone structural changes. The standardization (level of agreement) concerning image interpretations was high (Cohen’s Kappa coefficient was 0.819). After the standardization, the first examiner evaluated all study sample twice, 2 weeks apart and a high level of the intra-examiner agreement was found (intraclass correlation coefficient was above 0.840 for numerical variables; Cohen’s Kappa was above 0.819 for categorical variables). The second examiner, the medical engineer was responsible for condylar three-dimensional reconstructions, superimpositions, and volume calculations. Moreover, the second examiner assessed volumes twice, with a 2-week interval in-between the duplicate assessments, the intraclass correlation coefficient was above 0.840, which indicates a high level of intra-examiner agreement.
2.1. Condylar Displacement
To evaluate changes in the anteroposterior condylar position (Χ) in the glenoid fossa, the anterior and posterior interarticular spaces on sagittal CBCT MPR images were measured in millimeters. The anterior space (A) was the distance between the most anterior condylar point to the corresponding glenoid fossa bone, and the posterior space (P) was the distance between the most posterior condylar point to the corresponding glenoid fossa bone.
Standardized orientation for measurements in the sagittal plane was achieved by sectioning the CBCT image parallel to the line passing through the tip of the coronoid process and anterior margin of external auditory meatus as described by Hilgers et al. [
35]. Measurements were analyzed using Pullinger and Hollender’s formula [
38] (
Figure 1). The condylar position (Χ) was determined as either concentric (−12% < Χ < 12%), anterior (Χ > 12%), or posterior (Χ < 12%).
2.2. Condylar Axial Changes
To evaluate changes in the condylar axis, angular measurements between the reference planes and the axes (
Table 1) were obtained on axial, sagittal, and coronal CBCT MPR images (
Figure 2).
On the axial view of the MPR image, the angle formed by the axial condylar axis and the coronal reference plane was defined as the axial plane angle (
Figure 2A). On the coronal view of the MPR image, the angle between the coronal condylar axis and the Frankfurt horizontal plane, measured at the internal part of the intersection, was defined as the coronal plane angle (
Figure 2B). On the sagittal view, the angle formed by the sagittal condylar axis and the Frankfurt plane was defined as the sagittal plane angle (
Figure 2C).
2.3. Condylar Bone Structural Changes
Qualitative changes in the condylar bone structure were assessed on the sagittal and coronal CBCT MPR images following the radiographic criteria for condylar bone degeneration [
25]. The condyles were evaluated for the presence or absence of the following radiographic features:
Surface flattening—a loss of the rounded contour of the surface;
Subcortical sclerosis—an area of increased cortical bone density extending into the bone marrow;
Subcortical cyst—a cavity below the articular surface that deviates from the normal marrow pattern;
Surface erosion—an area of decreased density or discontinuity or irregularity in the cortical bone;
Osteophyte—marginal hypertrophy with sclerotic borders and exophytic angular formation of osseous tissue arising from the surface.
According to the detected radiographic structural changes, condyles were classified as normal, having condylar remodeling, or having active or stable degenerative joint disease.
2.4. Condylar Volume
The condylar module volumetric measurements were acquired using two software programs: 3D Slicer, Version 4.10.0 (open-source software,
www.slicer.org) [
39,
40] to create surface models of the mandible and the cranial base accompanied by a module to enable model cutting and volume calculations, and Autodesk Meshmixer, Version 3.5 (open-source software,
www.meshmixer.com) to trim the models to increase the computational speed and separate the cranial base from the mandible. After separation, each condylar region was exported as a separate model in stereolithography (STL) file format. Subsequently, these models were then imported back into the 3D Slicer software and cut using the EasyClip module, which provides the option of using up to three cutting planes.
Patients’ Digital Imaging and Communications in Medicine (DICOM) files were exported in a DICOM series format into the 3D Slicer software in which the segmentation tool was used for the creation of surface models using a semi-automatic approach. First, a lower threshold level of 130–250 HU (Hounsfield units), depending on the quality of the CBCT scan, was applied to maximize the signal-to-noise ratio and minimize manual work thereafter. Then, a manual approach was taken to edit any condylar boundary areas as deemed necessary. Lastly, the inside of each condylar surface model was filled just past the identified sigmoid notch using the island selection tool, thereby removing the effect of model wall thickness on the volume measurement. Once completed, the models were exported in STL format for further processing.
The exported STL models were then imported into the Autodesk Meshmixer software (Version 3.5). Here, each model was trimmed down to remove unnecessary data, including noise and artifacts, and to increase the computation time. For each patient, the mandibular regions containing the condyles and part of the cranial base were exported as separate new models in STL format.
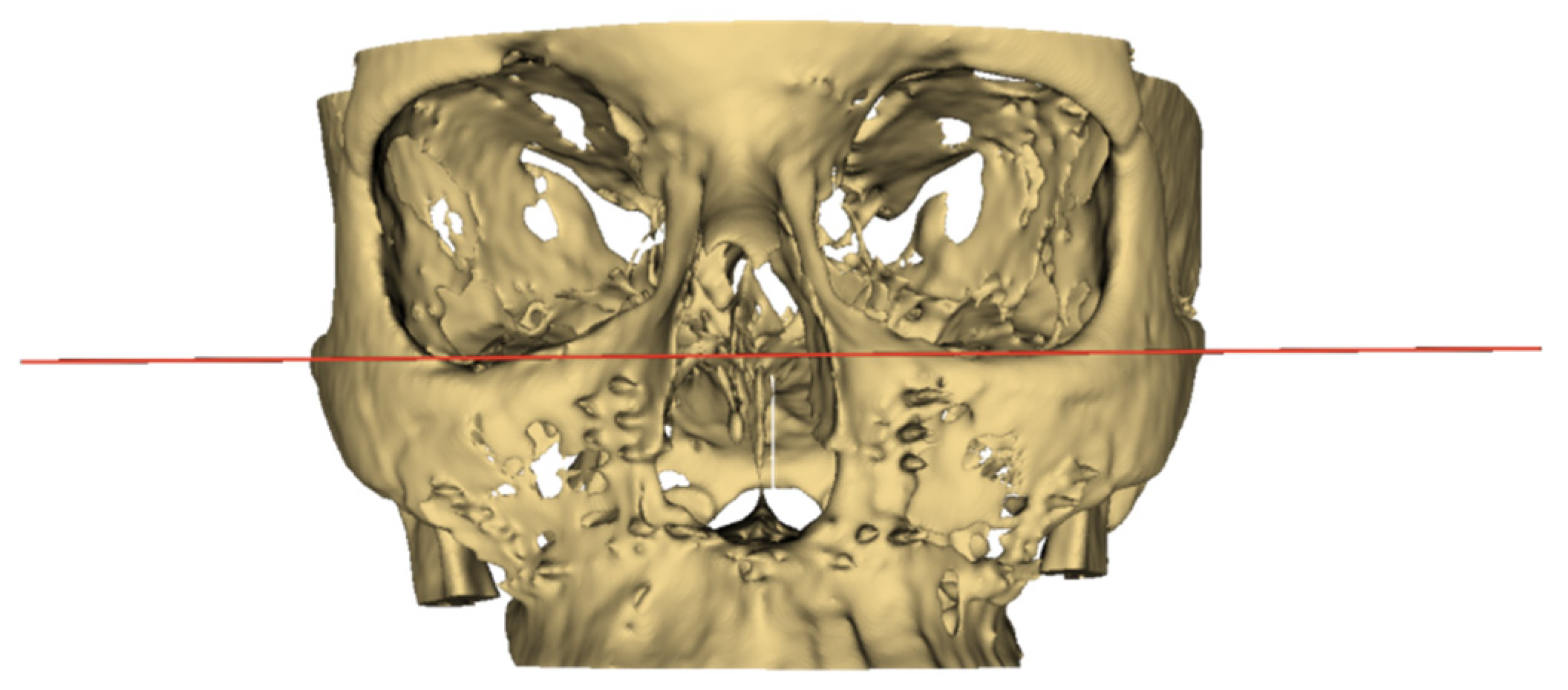
These new models were then imported back into the 3D Slicer software, and the EasyClip module was applied. This is where the cranial base model was used as a reference to position the main cutting plane—in
Figure 3, the red plane was positioned as the Frankfurt horizontal plane. Once set, the cranial base model was hidden, and the horizontal cutting plane was moved downwards without changing its angular position to go through the sigmoid notch of each mandibular model separately. The coronal cutting plane (indicated by the green line in
Figure 4) was positioned to pass through this intersection between the cutting plane and the sigmoid notch in case the horizontal plane was positioned too low. The result for a single sample is exemplified in
Figure 4. Once complete, each model’s information tab was opened to record the volume.
2.5. Statistical Analyses
IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp, Armonk, NY, USA) software was used for all statistical analyses. The results were considered statistically significant when p < 0.05.
Both, the condylar position relative to the glenoid fossa and the morphological status before the surgery, after the surgery, and at the subsequent follow-up were compared by the chi-square test for non-related comparisons or McNemar test for related comparisons, or Fisher’s exact test (when conditions for the chi-square test were not met). Condylar axis changes in each group were examined at three time-points, and time-related changes were analyzed using a paired samples t-test (for normally distributed data) or Mann–Whitney test (for non-normally distributed data). Condylar volume statuses between the surgery and after the surgery were compared using a paired samples t-test. An independent sample t-test was employed to compare mean changes in the condylar volume and axis between the two surgery groups.
4. Discussion
Orthognathic surgery-induced changes in the condylar position may often result in condylar remodeling [
41,
42]. The current study utilized 3D CBCT images to assess condylar displacement, axial changes, and structural and volumetric changes after bimaxillary and maxillary single-jaw orthognathic surgeries in skeletal Class III patients.
In the present study, the condylar displacements were not significantly different between the maxillary single-jaw and bimaxillary surgery groups at pre-surgical, post-surgical, or one-year follow-up time points. In the bimaxillary surgery group, the condyles had anterior or concentric positions in the glenoid fossa before surgery. After surgery, the pattern of condylar locations remained the same. At the one-year follow-up, the condyles tended to move more concentrically as compared with before or immediately after surgery. The proportions of anteriorly positioned condyles decreased only minimally. This finding is in accordance with the previous research of Kim et al. [
43,
44], Iguchi et al. [
45], and Choi et al. [
46,
47]. In the maxillary single-jaw surgery group, the condyles were positioned anteriorly or concentrically before the surgery. The proportion of posteriorly positioned condyles significantly increased after surgery; however, one year after surgery, the condyles had moved to their original pre-surgical position. There are several reasons why condylar displacement may develop after maxillary single-jaw surgery. The mandibular autorotation that ensues from superior maxillary repositioning results in rotation of the condyle along its long axis, which may subsequently result in posterior displacement of the condyle as it rotates in the fossa. Soft tissue tension along with resistance within the maxillomandibular complex and a new occlusal position may also change the relationship between the condyle and the fossa [
14,
15].
To the best of our knowledge, only a few studies have evaluated condylar positional changes after maxillary single-jaw surgery for correction of dentofacial deformities. Cevidanes et al. [
19] evaluated one-week post-surgery changes in condylar position using CBCT images of patients with different types of dentofacial deformities. Three-dimensional mandibular condyles and rami models were constructed from CBCT images and superimposed on the cranial base. Color maps were analyzed to assess the 3D condylar displacement. Only one out of 10 patients showed posterior mandibular rami displacement of more than 2 mm. Cortez et al. [
18] studied patients who had skeletal Class III orthognathic surgery and used submentovertex radiographs to assess condylar positional changes after maxillary advancement surgery; no changes were observed in condylar position from pre- to post-surgery (1–2 weeks and six months after surgery). Mavreas and coworkers [
17] studied tomograms of temporomandibular joints. Out of the 44 patients included in the study, 10 patients underwent isolated maxillary surgery for the correction of different types of dentofacial deformities. Posterior and anterior temporomandibular joint spaces were measured to assess condylar displacement before and 1 week and 6 months after orthognathic surgery. In that study, no changes in condylar position were found after the surgery.
In the current study, angular measurements in the axial, coronal, and sagittal planes were performed to assess condylar axial changes. A significant difference between the two groups was found for the condylar angular measurements in the axial plane when comparing post-surgery and one-year follow-up measurements. The bimaxillary surgery group showed, on average, a 4.0° higher inward rotation of the condylar head as compared with the maxillary single-jaw surgery group.
In the bimaxillary surgery group, the condyles showed significant inward rotation immediately after surgery. The one-year follow-up axial plane angle values were at the same level as immediately after the surgery. This finding is consistent with previous studies [
42,
43,
44,
48]. The available evidence regarding angular rotation in the axial plane is controversial. Several studies [
46,
47,
49,
50] found that condyles tend to rotate inwards immediately after surgery. However, longer-term follow-ups showed that condyles tend to regress to their original position. In contrast to our findings, a study by Ueki et al. [
51] found that condyles overcome outward rotation after surgery.
The coronal plane angle significantly increased after surgery, indicating mesial tilting of the condyles. However, one year later, the condyles tended to realign. This is in accordance with the findings from Choi et al. [
46]. Contrary to our findings, Ueki et al. [
51] reported lateral tilting in the coronal plane 1 year after orthognathic surgery. No change in the coronal plane angle was reported by Kim et al. [
43,
44].
In the sagittal plane, the angle between the condylar long axis and the Frankfort plane decreased after surgery and at the one-year follow-up; this indicates that condyles tend to have backward rotation. Our findings are in line with the findings of Kim et al. [
44] and Ueki et al. [
51,
52]. The Ueki et al. study [
51] reported backward condylar rotation 1 week after surgery; however, one year after surgery, the condylar sagittal angle regressed to pre-surgery status. By contrast, Kim et al. [
43] reported forward condylar rotation in the sagittal plane three months after orthognathic surgery.
Differences in findings could be broadly explained by factors such as differences in condylar reposition methods, types of internal fixation, amount and direction of surgical movement, intermaxillary immobilization period, and their multiple interactions [
53].
In the maxillary single-jaw surgery group, the only significant change in the coronal plane angle from the post-surgical to the one-year follow-up observation was found. However, the condylar coronal plane angle decrease on average by 0.4° is lacking clinical significance. Sanroman et al. [
16] and Cortez et al. [
18] studied condylar rotational displacement after the maxillary single-jaw surgery in patients with different types of malocclusions and they did not find condylar angular changes six months after the maxillary advancement orthognathic surgery. The absence of the condylar angular changes after the isolated maxillary advancement surgery could be explained by not substantial degree of maxillary repositioning to cause mandibular autorotation and masticatory muscles ability to adapt to a new environment.
No significant condylar morphology differences were found between the bimaxillary and maxillary single-jaw surgery groups either before or after surgery. In the bimaxillary surgery group, the most common radiographic findings before and after surgery were condylar surface flattening and subcortical sclerosis. Before surgery, the majority of condyles (83.9%) were classified under the remodeling status, and a similar proportion (82.9%) was observed one year after surgery. One condyle (1.8%) was classified under the stable degenerative joint disease status due to the presence of a subcortical cyst. However, the subcortical cyst was detected before orthognathic surgery and did not show any further development at the one-year follow-up.
In the maxillary single-jaw surgery group, condylar surface flattening was found in 26 (81.3%) and subcortical sclerosis in 2 (6.3%) out of the total 32 condyles. Increased frequency (12.5%; four new cases) of subcortical sclerosis was found 1 year after surgery. In general, most condyles had remodeling status both before (81.3%) and after (87.5%) orthognathic surgery. No features of condylar bone degeneration were observed in the maxillary single-jaw surgery group before or after surgery.
Little is known about the time-related condylar bone structural changes in patients who undergo orthognathic surgery for correction of skeletal Class III dentofacial deformities. Krisjane et al. [
54] evaluated the prevalence of condylar bone structural changes in skeletal Class I, Class II, and Class III patients who sought combined orthodontic and orthognathic surgery treatments. The most common radiographic finding in the skeletal Class III group was articular surface flattening (47.0%; 23 out of 49 condyles) followed by osteophyte formation (20.4%; 10 out of 49 condyles), and surface erosion (12.3%; 6 out of 49 condyles). Subcortical sclerosis (2.0%; 1 out of 49 condyles) and subcortical cyst formation (2.0%; 1 out of 49 condyles) were not prevalent. The post-surgical evaluation was not included in this study. The cross-sectional study of Yamada et al. [
55] assessed the pre-treatment helical CT images of 129 orthognathic surgery patients for the presence of condylar surface flattening, surface erosion, and osteophytes. Subcortical sclerosis or cysts were not observed in this study. Researchers concluded that the condylar bone changes were more frequent in mandibular retrusion and open bite cases. In the mandibular protrusion group, surface flattening was observed in 3.3% (3 out of 92 joints) and erosion in 2.2% (2 out of 92 joints) of all cases. In the maxillary retrusion group, the corresponding values were 8.3% (2 out of 24 joints) and 4.2% (1 out of 24 joints). No condylar bone structural changes were detected in the maxillary retrusion and mandibular protrusion groups. However, information about the post-surgery changes is not available.
Since mandibular condyles demonstrate adaptability to changed functional stimuli after the orthognathic surgery, progressive changes with a decrease in condylar volume may alter skeletal stability post-surgery. The extent of condylar volume decrease is an important factor to consider. A study by Xi et al. [
56] showed that loss of more than 17% of the original condylar volume is an indicator of pathological condylar resorption. In our study, condylar volume assessments showed no significant difference between the maxillary single-jaw and bimaxillary surgery groups for both the pre- and post-surgical mean values. Our study showed that in the bimaxillary surgery group, the condylar volume decreased, on average, by 9.2 ± 8 mm
3 one year after surgery, which represents 5.3% of the pre-operative volume. In the maxillary single-jaw surgery group at one year after surgery, condylar volume increased, on average, by 16.7 ± 1.9 mm
3, which represents 9.1% of the pre-operative volume. Lin et al. [
57] assessed condylar volumetric changes in skeletal Class III patients with an asymmetric mandibular prognathism. In the BSSO group, the average volume changes of the deviated and non-deviated sides of the condyles were 71.6 ± 11.9 and 59.3 ± 8.4 mm
3, respectively, one year after surgery. However, no data about the percentage decrease are available for the present study.
It is important to mention the study limitations. The scope of our study was to assess possible condylar changes in the context of different aspects such as position, structure, volume in the same sample at different time points. As clinical evaluation of the temporomandibular joint function was not the scope of the present study, our findings have limited clinical implications. We could speculate, that the absence of significant positional, structural or volumetric condylar changes indicates the absence of clinical signs and symptoms. However, these assumptions would require additional clinical evaluation which could be the focus of future studies. Our study groups were not homogenous, and the sample size of the maxillary single-jaw surgery group was relatively small; therefore, extrapolation of the present findings needs to be practiced with caution in terms of broader applicability. Due to the heterogeneity of the study groups we did not compare condylar changes with the degree of surgical movement. The standardization of the cross-sections in the assessment of multiplanar images for linear and angular measurements is challenging in longitudinal and across-subject studies. To mitigate this challenge, our examiner was trained and calibrated prior to the study. Furthermore, our assessment of condylar volumetric changes did not allow delimitation of the areas of bone resorption or apposition, nor assessment of whether these alterations were due to the repositioning of condyles. The use of color maps might be necessary in future research.