Does Thyroidectomy Impact Quality of Life: Retrospective Case–Control Study of Post-Thyroidectomy Patients and Matched Individuals from the General Population
Abstract
1. Introduction
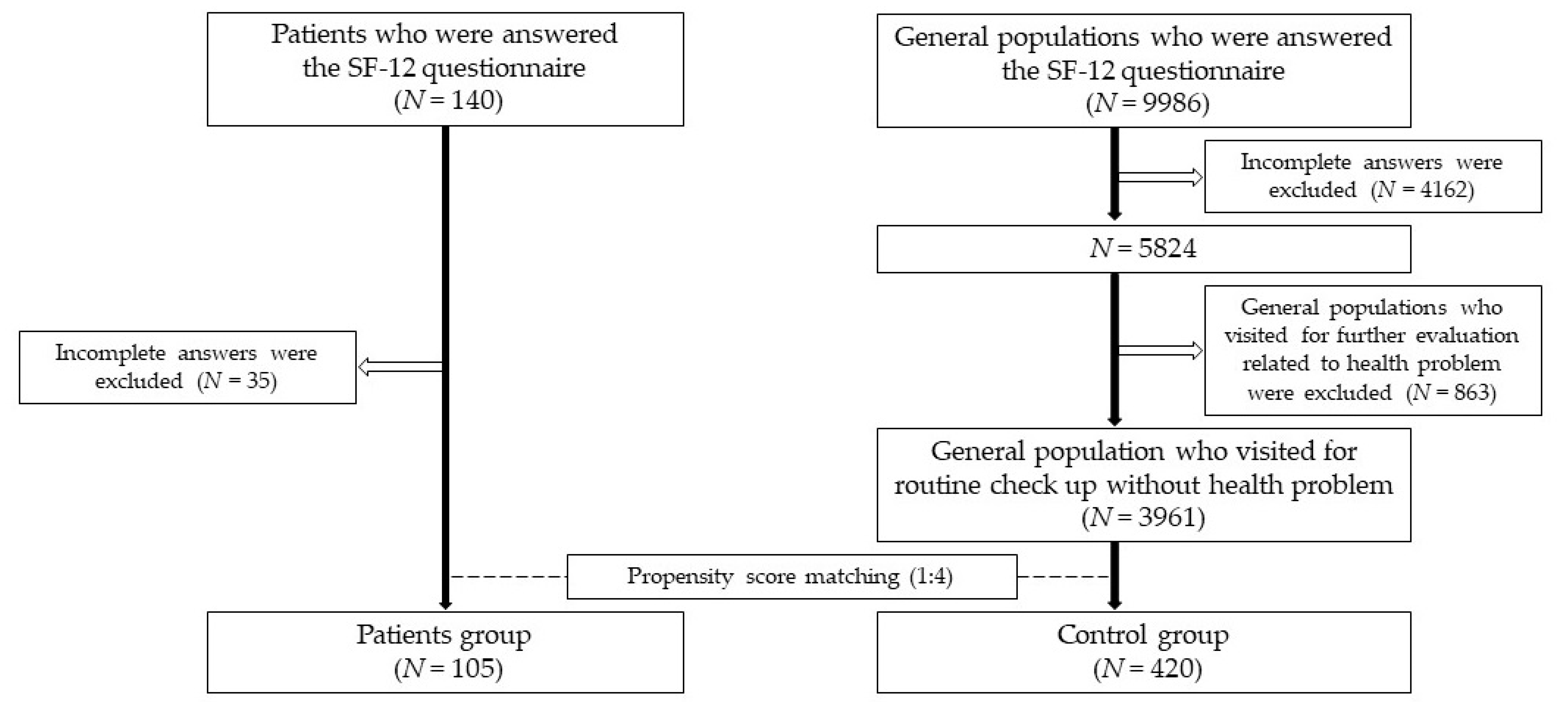
2. Materials and Methods
2.1. Patient Group
2.2. Control Group
2.3. Propensity Score Matching
2.4. Measurement of QoL
2.5. Statistics
2.6. Compliance with Ethical Standards
3. Results
3.1. Sociodemographic Characteristics of Patients and Controls
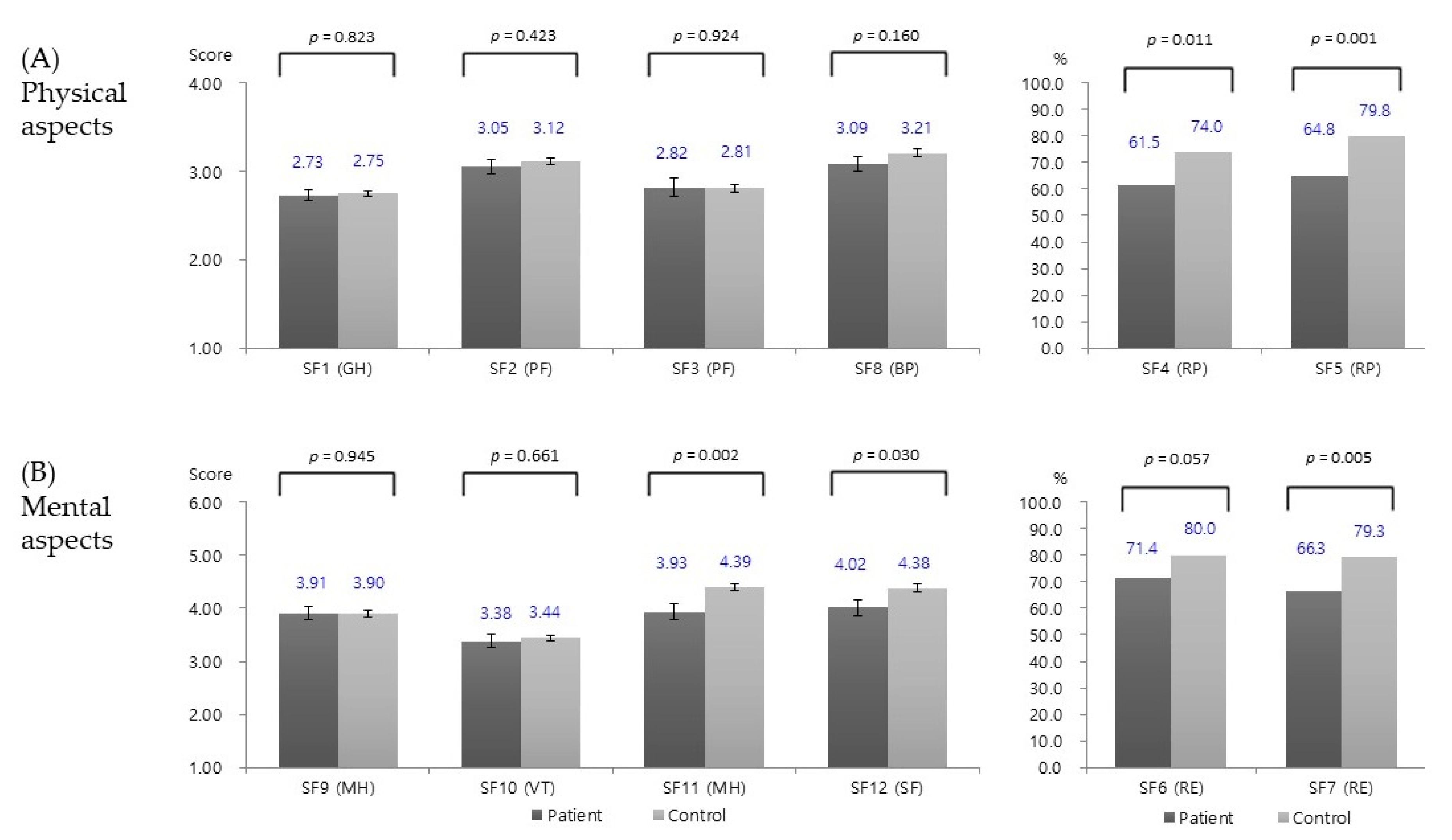
3.2. Comparison of QoL between Patients and Controls
3.3. Factors Associated with QoL Impairment in Patients
3.4. Patients with Less Than 1 Year Follow-Up vs. More Than 1 Year Follow-Up
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- The Whoqol Group. The World Health Organization quality of life assessment (WHOQOL): Development and general psychometric properties. Soc. Sci. Med. 1998, 46, 1569–1585. [Google Scholar] [CrossRef]
- Kaplan, R.M.; Ries, A.L. Quality of life: Concept and definition. COPD J. Chronic Obstr. Pulm. Dis. 2007, 4, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Hamidou, Z.; Dabakuyo-Yonli, T.S.; Guillemin, F.; Conroy, T.; Velten, M.; Jolly, D.; Causeret, S.; Graesslin, O.; Gauthier, M.; Mercier, M.; et al. Impact of response shift on time to deterioration in quality of life scores in breast cancer patients. PLoS ONE 2014, 9, e96848. [Google Scholar] [CrossRef] [PubMed]
- Scarpa, M.; Griggio, L.; Rampado, S.; Ruffolo, C.; Citton, M.; Pozza, A.; Borsetto, L.; Dall’olmo, L.; Angriman, I. Long-term health-related quality of life after minimally invasive surgery for diverticular disease. Langenbeck’s Arch. Surg. 2011, 396, 833–843. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.W.; Won, Y.J.; Kong, H.J.; Oh, C.M.; Lee, D.H.; Lee, J.S. Cancer statistics in Korea: Incidence, mortality, survival and prevalence in 2011. Cancer Res. Treat. 2014, 46, 109–123. [Google Scholar] [CrossRef] [PubMed]
- Almeida, J.P.; Vartanian, J.G.; Kowalski, L.P. Clinical predictors of quality of life in patients with initial differentiated thyroid cancers. Arch. Otolaryngol. Head Neck Surg. 2009, 135, 342–347. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pellegriti, G.; Frasca, F.; Regalbuto, C.; Squatrito, S.; Vigneri, R. Worldwide increasing incidence of thyroid cancer: Update on epidemiology and risk factors. J. Cancer Epidemiol. 2013, 2013, 965212. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Sabaretnam, M.; Chand, G.; Agarwal, G.; Agarwal, A.; Verma, A.K.; Mishra, S.K. Quality of life (QoL) in patients with benign thyroid goiters (pre- and post-thyroidectomy): A prospective study. World J. Surg. 2013, 37, 2322–2329. [Google Scholar] [CrossRef] [PubMed]
- Cramon, P.; Bonnema, S.J.; Bjorner, J.B.; Ekholm, O.; Feldt-Rasmussen, U.; Frendl, D.M.; Groenvold, M.; Hededüs, L.; Rasmussen, Å.K.; Watt, T. Quality of life in patients with benign nontoxic goiter: Impact of disease and treatment response, and comparison with the general population. Thyroid 2015, 25, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.D.; Witterick, I.J.; Eski, S.J.; Pinto, R.; Freeman, J.L. Quality of life in patients undergoing thyroid surgery. J. Otolaryngol. 2006, 35, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.G.; Nan, L.; Thumboo, J.; Sundram, F.; Tan, L.K. Health-related quality of life in thyroid cancer survivors. Laryngoscope 2007, 117, 507–510. [Google Scholar] [CrossRef] [PubMed]
- Malterling, R.R.; Andersson, R.E.; Falkmer, S.; Falkmer, U.; Niléhn, E.; Järhult, J. Differentiated thyroid cancer in a Swedish county—Long-term results and quality of life. Acta Oncol. 2010, 49, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Duan, H.; Gamper, E.; Becherer, A.; Hoffmann, M. Quality of life aspects in the management of thyroid cancer. Oral Oncol. 2015, 51, S1–S5. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.B. On principles for modeling propensity scores in medical research. Pharmacoepidemiol. Drug Saf. 2004, 13, 855–857. [Google Scholar] [CrossRef] [PubMed]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Kudo, T.; Takamura, Y.; Kobayashi, K.; Miya, A.; Miyauchi, A. Prognostic factors of papillary thyroid carcinoma vary according to sex and patient age. World J. Surg. 2011, 35, 2684–2690. [Google Scholar] [CrossRef] [PubMed]
- Dingle, I.F.; Mishoe, A.E.; Nguyen, S.A.; Overton, L.J.; Gillespie, M.B. Salivary morbidity and quality of life following radioactive iodine for well-differentiated thyroid cancer. Otolaryngol. Head Neck Surg. 2013, 148, 746–752. [Google Scholar] [CrossRef] [PubMed]
- Stover, A.M.; Mayer, D.K.; Muss, H.; Wheeler, S.B.; Lyons, J.C.; Reeve, B.B. Quality of life changes during the pre- to postdiagnosis period and treatment-related recovery time in older women with breast cancer. Cancer 2014, 120, 1881–1889. [Google Scholar] [CrossRef] [PubMed]
- Tsunoda, A.; Nakao, K.; Hiratsuka, K.; Tsunoda, Y.; Kusano, M. Prospective analysis of quality of life in the first year after colorectal cancer surgery. Acta Oncol. 2007, 46, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Gambardella, C.; Polistena, A.; Sanguinetti, A.; Patrone, R.; Napolitano, S.; Esposito, D.; Testa, D.; Marotta, V.; Faggiano, A.; Calò, P.G.; et al. Unintentional recurrent laryngeal nerve injuries following thyroidectomy: Is it the surgeon who pays the bill? Int. J. Surg. 2017, 41 (Suppl. 1), S55–S59. [Google Scholar] [CrossRef] [PubMed]
| SF | Items (Abbreviation) | Aspect | Types of Variables | Answers | Question |
|---|---|---|---|---|---|
| SF-1 | General Health (GH) | Physical | Ordinal | 1 (Poor) ⇔ 4 (Excellent) | In general, would you say your health is |
| SF-2 | Physical Functioning (PF) | Physical | Ordinal | 1 (Limited a lot) ⇔ 4 (Not limited at all) | Limitation in moderate activities |
| SF-3 | Physical Functioning (PF) | Physical | Ordinal | 1 (Limited a lot) ⇔ 4 (Not limited at all) | Limitation in climbing several flights of stairs |
| SF-4 | Role Physical (RP) | Physical | Binary | 1 (Limited), 2 (Not limited) | Accomplished less than you would like due to physical problem (past 4 weeks) |
| SF-5 | Role Physical (RP) | Physical | Binary | 1 (Limited), 2 (Not limited) | Were limited in the kind of work or other activities due to physical problem (past 4 weeks) |
| SF-6 | Role Emotional (RE) | Mental | Binary | 1 (Depressed), 2 (Not depressed) | Accomplished less than you would like due to emotional problems (past 4 weeks) |
| SF-7 | Role Emotional (RE) | Mental | Binary | 1 (Depressed), 2 (Not depressed) | Did not do work or other activities as carefully as usual due to emotional problems (past 4 weeks) |
| SF-8 | Bodily Pain (BP) | Physical | Ordinal | 1 (Extreme pain) ⇔ 4 (Not at all) | How much did pain interfere with your normal work? (past 4 weeks) |
| SF-9 | Mental Health (MH) | Mental | Ordinal | 1 (Depressed) ⇔ 6 (Not depressed) | Have you felt calm and peaceful? (past 4 weeks) |
| SF-10 | Vitality (VT) | Mental | Ordinal | 1 (Depressed) ⇔ 6 (Not depressed) | Did you have a lot of energy? (past 4 weeks) |
| SF-11 | Mental Health (MH) | Mental | Ordinal | 1 (Depressed) ⇔ 6 (Not depressed) | Have you felt downhearted and blue? (past 4 weeks) |
| SF-12 | Social Functioning (SF) | Mental | Ordinal | 1 (Depressed) ⇔ 6 (Not depressed) | How much of the time has your physical health or emotional problems interfered with your social activities? |
| Patient Group (n = 105) | Control Group (n = 420) | |||||
|---|---|---|---|---|---|---|
| n | % | n | % | p Value | ||
| Age | Mean ± SD | 49.2 ± 12.6 | 49.9 ± 13.1 | 0.609 | ||
| Sex | Male | 17 | 16.2 | 63 | 15.0 | 0.761 |
| Female | 88 | 83.8 | 357 | 85.0 | ||
| Smoking | No | 89 | 84.8 | 368 | 87.6 | 0.435 |
| Yes | 16 | 15.2 | 52 | 12.4 | ||
| Alcohol consumption | No | 76 | 72.4 | 277 | 72.4 | 0.209 |
| Yes | 29 | 27.6 | 143 | 34.0 | ||
| Spouse | Yes | 80 | 77.7 | 306 | 75.2 | 0.599 |
| No | 23 | 22.3 | 101 | 24.8 | ||
| Education | ≥College above | 50 | 48.1 | 244 | 58.1 | 0.065 |
| ≤High School | 54 | 51.3 | 176 | 41.9 | ||
| Monthly household income (KRW) | ≥4,000,000 | 47 | 47.5 | 215 | 53.0 | 0.328 |
| <4,000,000 | 52 | 52.5 | 191 | 47.0 | ||
| Employed | Yes | 56 | 53.3 | 191 | 46.5 | 0.209 |
| No | 49 | 46.7 | 220 | 53.5 | ||
| F/U duration | Mean ± SD (min–max) (mo) | 20.3 ± 29.5 (0.3–205.0) | ||||
| Op type | Total thyroidectomy | 83 | 79.0 | |||
| lobectomy | 22 | 21.0 | ||||
| Benign vs. Malignant | Malignancy (I and II/III and IV) | 75 (42/33) | 82.4 (56/44) | |||
| Benign | 16 | 17.6 | ||||
| SF-4 (aOR(95% CI)) | SF-5 (aOR(95% CI)) | SF-7 (aOR(95% CI)) | SF-11 (aOR(95% CI)) | SF-12 (aOR(95% CI)) | ||
|---|---|---|---|---|---|---|
| Age | <50 years (ref) vs. ≥50 years | 0.485 (0.210–1.122) | 0.957 (0.383–2.389) | 1.399 (0.592–3.305) | 0.283 (0.109–0.737) | / |
| Sex | Male (ref.) vs. Female | 0.332 (0.084–1.314) | 0.284 (0.052–1.545) | 0.122 (0.015–0.983) | 0.990 (0.283–3.467) | / |
| Alcohol | Yes (ref) vs. No and Past | 2.723 (0.959–7.734) | 1.731 (0.569–5.265) | 2.382 (0.781–7.262) | / | |
| Employed | Yes (ref) vs. No | / | 0.441 (0.170–1.145) | / | 2.531 (0.962–6.657) | / |
| F/U duration | <1 year (ref) vs. ≥1 year | / | 4.726 (1.862–11.999) | / | 2.2 (0.902–5.369) | / |
| Op type | Lobectomy (ref) vs. Total thyroidectomy | / | / | / | 2.784 (0.954–8.124) | / |
| Patients <1 Year (n = 48) vs. Controls (n = 420) | Patients ≥1 Year (n = 56) vs. Controls (n = 420) | |||
|---|---|---|---|---|
| p Value | p Value | |||
| SF-1 (GH) | 2.77 ± 0.074 vs. 2.75 ± 0.028 | 0.770 | 2.70 ± 0.095 vs. 2.75 ± 0.028 | 0.566 |
| SF-2 (PF) | 2.94 ± 0.109 vs. 3.12 ± 0.038 | 0.129 | 3.14 ± 0.121 vs. 3.12 ± 0.038 | 0.832 |
| SF-3 (PF) | 2.79 ± 0.143 vs. 2.81 ± 0.047 | 0.916 | 2.84 ± 0.146 vs. 2.81 ± 0.047 | 0.817 |
| SF-4 (RP) | 56.3% vs. 74.0% | 0.009 | 66.1% vs. 74.0% | 0.206 |
| SF-5 (RP) | 47.9% vs. 79.8% | <0.001 | 78.9% vs. 79.8% | 0.886 |
| SF-6 (RE) | 66.7% vs. 80.0% | 0.033 | 75.4% vs. 80.0% | 0.424 |
| SF-7 (RE) | 62.5% vs. 79.3% | 0.008 | 69.6% vs. 79.3% | 0.101 |
| SF-8 (BP) | 2.88 ± 0.132 vs. 3.21 ± 0.039 | 0.007 | 3.26 ± 0.102 vs. 3.21 ± 0.039 | 0.631 |
| SF-9 (MH) | 3.83 ± 0.200 vs. 3.90 ± 0.061 | 0.712 | 3.98 ± 0.171 vs. 3.90 ± 0.061 | 0.663 |
| SF-10 (VT) | 3.40 ± 0.175 vs. 3.44 ± 0.057 | 0.813 | 3.37 ± 0.185 vs. 3.44 ± 0.057 | 0.679 |
| SF-11 (MH) | 3.71 ± 0.223 vs. 4.39 ± 0.065 | 0.001 | 4.12 ± 0.191 vs. 4.39 ± 0.065 | 0.157 |
| SF-12 (SF) | 3.91 ± 0.213 vs. 4.38 ± 0.073 | 0.004 | 4.11 ± 0.218 vs. 4.38 ± 0.073 | 0.202 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, H.W.; An, A.R.; Kang, H.I.; Suh, Y.J.; Kwon, H.; Kim, S.-j.; Chai, Y.J.; Choi, J.Y.; Choi, H.; Lee, K.E.; et al. Does Thyroidectomy Impact Quality of Life: Retrospective Case–Control Study of Post-Thyroidectomy Patients and Matched Individuals from the General Population. Medicina 2020, 56, 603. https://doi.org/10.3390/medicina56110603
Yu HW, An AR, Kang HI, Suh YJ, Kwon H, Kim S-j, Chai YJ, Choi JY, Choi H, Lee KE, et al. Does Thyroidectomy Impact Quality of Life: Retrospective Case–Control Study of Post-Thyroidectomy Patients and Matched Individuals from the General Population. Medicina. 2020; 56(11):603. https://doi.org/10.3390/medicina56110603
Chicago/Turabian StyleYu, Hyeong Won, Ah Reum An, Hye In Kang, Yong Joon Suh, Hyungju Kwon, Su-jin Kim, Young Jun Chai, June Young Choi, Hochun Choi, Kyu Eun Lee, and et al. 2020. "Does Thyroidectomy Impact Quality of Life: Retrospective Case–Control Study of Post-Thyroidectomy Patients and Matched Individuals from the General Population" Medicina 56, no. 11: 603. https://doi.org/10.3390/medicina56110603
APA StyleYu, H. W., An, A. R., Kang, H. I., Suh, Y. J., Kwon, H., Kim, S.-j., Chai, Y. J., Choi, J. Y., Choi, H., Lee, K. E., & Cho, B. (2020). Does Thyroidectomy Impact Quality of Life: Retrospective Case–Control Study of Post-Thyroidectomy Patients and Matched Individuals from the General Population. Medicina, 56(11), 603. https://doi.org/10.3390/medicina56110603





