Exertional Heat Stroke, Modality Cooling Rate, and Survival Outcomes: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Quality Assessment
2.3. Descriptive Analysis
3. Results
4. Discussion
4.1. Patient Outcomes
4.2. Cooling Rate and Influence on Patient Outcomes
4.3. Implications for Practice
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A. Search Terms Used for the Review
| Search Engine | Search Number | Search Term |
| PubMed | 1 | (mortal * OR death * OR died OR fatal OR fatally OR fatality OR survive OR survival OR survivor * OR saves OR saved) AND (“exertional heat stroke” OR “exercise”(mesh)OR exercise(tiab) OR “exercises” OR exercising OR postexercise OR running(mesh)OR Runner * OR running(ti) OR biker OR biking OR bicyclist * OR bicycling(mesh)OR bicycling OR bicycle * OR cyclist * OR cycling(ti) OR triathlon * OR triathlete * OR marathon * OR ultramarathon * OR “trail race” OR “trail running” OR “road race” OR “road racing” OR athlete * OR treadmill * OR ergometer * OR “endurance training” OR (“physical” AND “conditioning”) OR “speed training” OR “circuit training” OR “training duration” OR “training frequency” OR “training intensity” OR “aerobic endurance” OR “aerobic training” OR “interval training” OR “combination training” OR “combined training” OR “HIIT” OR “Sports”(mesh)OR sport(tiab) OR sports(tiab) OR military(tiab) OR “military medicine” OR “armed forces” OR army(tiab) OR navy OR marines OR “air force” OR “coast guard” OR “special forces” OR walking(mesh)OR walking(ti) OR swimming OR soccer OR football OR futbol OR “cricket” OR rugby OR Skier * OR Skiing OR Basketball OR Tennis OR Judo OR Karate OR Boxing OR Lacrosse OR “field hockey” OR Golfing OR Golf OR Hockey OR Frisbee OR quidditch OR Horseback OR Wrestling OR “Water Polo” OR Snowboarding OR “Scuba Diving” OR “Rock Climbing” OR “Martial Arts” OR Kayaking OR Hiking OR “Cross Country” OR “Adventure Race” OR “Adventure Racing” OR cyclocross OR Baseball OR gymnastics OR gymnast OR rugby OR crossfit OR “cross-fit” OR skiing OR pre-season OR preseason OR recreational OR riding OR tournament OR workout * OR “return to activity” OR “return to duty”) AND (“exertional heat stroke” OR “Heat Stroke”(mesh)OR “heat exhaustion”(mesh)OR “heat illness” OR “heat illnesses” OR “heat related illness” OR “heat related illnesses” OR “heat stroke” OR “heat strokes” OR Heatstroke * OR “EHS” OR “EHI” OR “sun stroke” OR sunstroke * OR “heat exhaustion” OR “exercise collapse” OR (collapse * AND heat) OR (collapse * AND temperature) OR “heat injury” OR “heat injuries” OR “Hyperthermia” OR Hyperthermi *) NOT ((animals(mesh)NOT humans(mesh)) OR Comment(sb)OR review(pt)OR letter(pt)OR editorial(pt)OR veterinary * OR bovine OR animal * (ti) OR pig OR pigs OR porcine OR rat OR rats OR monkey * OR mouse OR mice OR canine OR feline OR acclimate * (ti) OR acclimitizat * (ti) OR “air conditioning”(ti) OR “nursing home”(ti) OR “nursing homes”(ti) OR “non-exertional”(ti) OR “computer simulation”(mesh)OR “passive heat stress” OR “classic heat stroke” OR “classic heatstroke” OR cancer OR cancers OR neoplasm * OR MDMA OR ecstasy OR ketamine OR “Lysergic Acid” OR “music festival” OR “Music festivals” OR hernia * OR “heat shock” OR “Legal Case”[pt]) |
| Scopus | 1 | TITLE-ABS-KEY(mortal * OR death * OR died OR fatal OR fatally OR fatality OR survive OR survival OR survivor * OR saves OR saved) AND (TITLE(running OR cycling) OR TITLE-ABS-KEY({exertional heat stroke} OR exercise OR exercises OR exercising OR postexercise OR post-exercis * OR Runner * OR biker OR biking OR bicyclist * OR bicycling OR bicycle * OR cyclist * OR triathlon * OR triathlete * OR marathon * OR ultramarathon * OR {trail race} OR {trail running} OR {road race} OR {road racing} OR athlet * OR treadmill * OR ergometer * OR {endurance training} OR {speed training} OR {circuit training} OR {training duration} OR {training frequency} OR {training intensity} OR {aerobic endurance} OR {aerobic training} OR {interval training} OR {combination training} OR {combined training} OR HIIT OR sport OR sports OR military OR {armed forces} OR army OR navy OR marines OR {air force} OR {coast guard} OR {special forces} OR walking OR swimming OR soccer OR football OR futbol OR cricket OR rugby OR Skier * OR Skiing OR Basketball OR Tennis OR Judo OR Karate OR Boxing OR Lacrosse OR {field hockey} OR Golfing OR Golf OR Hockey OR Frisbee OR quidditch OR Horseback OR Wrestling OR {Water Polo} OR Snowboarding OR {Scuba Diving} OR {Rock Climbing} OR {Martial Arts} OR Kayaking OR Hiking OR {Cross Country} OR {Adventure Race} OR {Adventure Racing} OR cyclocross OR Baseball OR gymnastics OR gymnast OR rugby OR crossfit OR cross-fit OR skiing OR pre-season OR preseason OR recreational OR riding OR tournament OR workout * OR {return to activity} OR {return to duty}) OR (physical w/5 conditioning)) AND TITLE-ABS-KEY({Heat Stroke} OR {heat exhaustion} OR {heat illness} OR {heat illnesses} OR {heat related illness} OR {heat related illnesses} OR {heat stroke} OR {heat strokes} OR Heatstroke * OR EHS OR EHI OR {sun stroke} OR sunstroke * OR {heat injury} OR {heat injuries} OR Hyperthermia OR Hyperthermi * OR (collapse * w/5 heat) OR (collapse * w/5 temperature) OR (exercise w/5 collapse *)) AND NOT (INDEX(MEDLINE) OR TITLE(animal * OR Comment * OR review OR letter OR editorial OR acclimat * OR acclimitizat * OR {air conditioning} OR {nursing home} OR {nursing homes} OR {non-exertional}) OR TITLE-ABS-KEY(veterinar * OR bovine OR pig OR pigs OR porcine OR rat OR rats OR monkey * OR mouse OR mice OR canine OR feline OR {computer simulation} OR {passive heat stress} OR {classic heat stroke} OR {classic heatstroke} OR cancer OR cancers OR neoplasm * OR MDMA OR ecstasy OR ketamine OR {Lysergic Acid} OR {music festival} OR {Music festivals} OR hernia * OR {heat shock})) AND (LIMIT-TO (DOCTYPE, “ar”) OR LIMIT-TO (DOCTYPE, “cp”)) AND (LIMIT-TO (SRCTYPE, “j”) OR LIMIT-TO (SRCTYPE, “p”)) |
| SportDiscus | 1 | Line 1: mortal * OR death * OR died OR fatal OR fatally OR fatality OR survive OR survival OR survivor * OR saves OR saved AND Line 2: “Heat Stroke” OR “heat exhaustion” OR “heat illness” OR “heat illnesses” OR “heat related illness” OR “heat related illnesses” OR “heat stroke” OR “heat strokes” OR Heatstroke * OR EHS OR EHI OR “sun stroke” OR sunstroke * OR “heat injury” OR “heat injuries” OR Hyperthermia OR Hyperthermi * OR (collapse * AND heat) OR (collapse * AND temperature) OR (exercise AND collapse *) |
| 2 | Line 1 (use pulldown to select title): running OR cycling OR Line2: “exertional heat stroke” OR exercise OR exercises OR exercising OR postexercise OR post-exercis * OR Runner * OR biker OR biking OR bicyclist * OR bicycling OR bicycle * OR cyclist * OR triathlon * OR triathlete * OR marathon * OR ultramarathon * OR “trail race” OR “trail running” OR “road race” OR “road racing” OR athlet * OR treadmill * OR ergometer * OR “endurance training” OR “speed training” OR “circuit training” OR “training duration” OR “training frequency” OR “training intensity” OR “aerobic endurance” OR “aerobic training” OR “interval training” OR “combination training” OR “combined training” OR HIIT OR sport OR sports OR military OR “armed forces” OR army OR navy OR marines OR “air force” OR “coast guard” OR “special forces” OR walking OR swimming OR soccer OR football OR futbol OR cricket OR rugby OR Skier * OR Skiing OR Basketball OR Tennis OR Judo OR Karate OR Boxing OR Lacrosse OR “field hockey” OR Golfing OR Golf OR Hockey OR Frisbee OR quidditch OR Horseback OR Wrestling OR “Water Polo” OR Snowboarding OR “Scuba Diving” OR “Rock Climbing” OR “Martial Arts” OR Kayaking OR Hiking OR “Cross Country” OR “Adventure Race” OR “Adventure Racing” OR cyclocross OR Baseball OR gymnastics OR gymnast OR rugby OR crossfit OR cross-fit OR skiing OR pre-season OR preseason OR recreational OR riding OR tournament OR workout * OR “return to activity” OR “return to duty” OR (physical AND conditioning) | |
| 3 | Line 1 (use pulldown to select title): animal * OR Comment * OR review OR letter OR editorial OR acclimat * OR acclimitizat * OR “air conditioning” OR “nursing home” OR “nursing homes” OR “non-exertional” OR Line 2: veterinar * OR bovine OR pig OR pigs OR porcine OR rat OR rats OR monkey * OR mouse OR mice OR canine OR feline OR “computer simulation” OR “passive heat stress” OR “classic heat stroke” OR “classic heatstroke” OR cancer OR cancers OR neoplasm * OR MDMA OR ecstasy OR ketamine OR “Lysergic Acid” OR “music festival” OR “Music festivals” OR hernia * OR “heat shock” | |
| CINAHL | 1 | Line 1: mortal * OR death * OR died OR fatal OR fatally OR fatality OR survive OR survival OR survivor * OR saves OR saved AND Line 2: “Heat Stroke” OR “heat exhaustion” OR “heat illness” OR “heat illnesses” OR “heat related illness” OR “heat related illnesses” OR “heat stroke” OR “heat strokes” OR Heatstroke * OR EHS OR EHI OR “sun stroke” OR sunstroke * OR “heat injury” OR “heat injuries” OR Hyperthermia OR Hyperthermia * OR (collapse * AND heat) OR (collapse * AND temperature) OR (exercise AND collapse *) |
| 2 | running OR cycling OR Line2: “exertional heat stroke” OR exercise OR exercises OR exercising OR postexercise OR post-exercis * OR Runner * OR biker OR biking OR bicyclist * OR bicycling OR bicycle * OR cyclist * OR triathlon * OR triathlete * OR marathon * OR ultramarathon * OR “trail race” OR “trail running” OR “road race” OR “road racing” OR athlet * OR treadmill * OR ergometer * OR “endurance training” OR “speed training” OR “circuit training” OR “training duration” OR “training frequency” OR “training intensity” OR “aerobic endurance” OR “aerobic training” OR “interval training” OR “combination training” OR “combined training” OR HIIT OR sport OR sports OR military OR “armed forces” OR army OR navy OR marines OR “air force” OR “coast guard” OR “special forces” OR walking OR swimming OR soccer OR football OR futbol OR cricket OR rugby OR Skier * OR Skiing OR Basketball OR Tennis OR Judo OR Karate OR Boxing OR Lacrosse OR “field hockey” OR Golfing OR Golf OR Hockey OR Frisbee OR quidditch OR Horseback OR Wrestling OR “Water Polo” OR Snowboarding OR “Scuba Diving” OR “Rock Climbing” OR “Martial Arts” OR Kayaking OR Hiking OR “Cross Country” OR “Adventure Race” OR “Adventure Racing” OR cyclocross OR Baseball OR gymnastics OR gymnast OR rugby OR crossfit OR cross-fit OR skiing OR pre-season OR preseason OR recreational OR riding OR tournament OR workout * OR “return to activity” OR “return to duty” OR (physical AND conditioning) | |
| 3 | Line 1 (use pulldown to select title): animal * OR Comment * OR review OR letter OR editorial OR acclimat * OR acclimitizat * OR “air conditioning” OR “nursing home” OR “nursing homes” OR “non-exertional” OR Line 2: veterinar * OR bovine OR pig OR pigs OR porcine OR rat OR rats OR monkey * OR mouse OR mice OR canine OR feline OR “computer simulation” OR “passive heat stress” OR “classic heat stroke” OR “classic heatstroke” OR cancer OR cancers OR neoplasm * OR MDMA OR ecstasy OR ketamine OR “Lysergic Acid” OR “music festival” OR “Music festivals” OR hernia * OR “heat shock” | |
| Academic Search Premier | 1 | Line 1: mortal * OR death * OR died OR fatal OR fatally OR fatality OR survive OR survival OR survivor * OR saves OR saved AND Line 2: “Heat Stroke” OR “heat exhaustion” OR “heat illness” OR “heat illnesses” OR “heat related illness” OR “heat related illnesses” OR “heat stroke” OR “heat strokes” OR Heatstroke * OR EHS OR EHI OR “sun stroke” OR sunstroke * OR “heat injury” OR “heat injuries” OR Hyperthermia OR Hyperthermi * OR (collapse * AND heat) OR (collapse * AND temperature) OR (exercise AND collapse *) |
| 2 | running OR cycling OR Line2: “exertional heat stroke” OR exercise OR exercises OR exercising OR postexercise OR post-exercis * OR Runner * OR biker OR biking OR bicyclist * OR bicycling OR bicycle * OR cyclist * OR triathlon * OR triathlete * OR marathon * OR ultramarathon * OR “trail race” OR “trail running” OR “road race” OR “road racing” OR athlet * OR treadmill * OR ergometer * OR “endurance training” OR “speed training” OR “circuit training” OR “training duration” OR “training frequency” OR “training intensity” OR “aerobic endurance” OR “aerobic training” OR “interval training” OR “combination training” OR “combined training” OR HIIT OR sport OR sports OR military OR “armed forces” OR army OR navy OR marines OR “air force” OR “coast guard” OR “special forces” OR walking OR swimming OR soccer OR football OR futbol OR cricket OR rugby OR Skier * OR Skiing OR Basketball OR Tennis OR Judo OR Karate OR Boxing OR Lacrosse OR “field hockey” OR Golfing OR Golf OR Hockey OR Frisbee OR quidditch OR Horseback OR Wrestling OR “Water Polo” OR Snowboarding OR “Scuba Diving” OR “Rock Climbing” OR “Martial Arts” OR Kayaking OR Hiking OR “Cross Country” OR “Adventure Race” OR “Adventure Racing” OR cyclocross OR Baseball OR gymnastics OR gymnast OR rugby OR crossfit OR cross-fit OR skiing OR pre-season OR preseason OR recreational OR riding OR tournament OR workout * OR “return to activity” OR “return to duty” OR (physical AND conditioning) | |
| 3 | Line 1 (use pulldown to select title): animal * OR Comment * OR review OR letter OR editorial OR acclimat * OR acclimitizat * OR “air conditioning” OR “nursing home” OR “nursing homes” OR “non-exertional” OR Line 2: veterinar * OR bovine OR pig OR pigs OR porcine OR rat OR rats OR monkey * OR mouse OR mice OR canine OR feline OR “computer simulation” OR “passive heat stress” OR “classic heat stroke” OR “classic heatstroke” OR cancer OR cancers OR neoplasm * OR MDMA OR ecstasy OR ketamine OR “Lysergic Acid” OR “music festival” OR “Music festivals” OR hernia * OR “heat shock” | |
| Cochrane Library: CENTRAL Registry of Clinical Trials | 1 | Line 1 (use pulldown to select title abstract keyword): mortal * OR death * OR died OR fatal OR fatally OR fatality OR survive OR survival OR survivor * OR saves OR saved AND Line 2 (use pulldown to select title abstract keyword): “Heat Stroke” OR “heat exhaustion” OR “heat illness” OR “heat illnesses” OR “heat related illness” OR “heat related illnesses” OR “heat stroke” OR “heat strokes” OR Heatstroke * OR EHS OR EHI OR “sun stroke” OR sunstroke * OR “heat injury” OR “heat injuries” OR Hyperthermia OR Hyperthermia * AND Line 3 (use pulldown to select title abstract keyword): running OR cycling OR “exertional heat stroke” OR exercise OR exercises OR exercising OR postexercise OR post-exercis * OR Runner * OR biker OR biking OR bicyclist * OR bicycling OR bicycle * OR cyclist * OR triathlon * OR triathlete * OR marathon * OR ultramarathon * OR “trail race” OR “trail running” OR “road race” OR “road racing” OR athlet * OR treadmill * OR ergometer * OR “endurance training” OR “speed training” OR “circuit training” OR “training duration” OR “training frequency” OR “training intensity” OR “aerobic endurance” OR “aerobic training” OR “interval training” OR “combination training” OR “combined training” OR HIIT OR sport NOT Line 4 (use pulldown to select record title): animal * OR Comment * OR review OR letter OR editorial OR acclimat * OR acclimitizat * OR “air conditioning” OR “nursing home” OR “nursing homes” OR “non-exertional” OR veterinar * OR bovine OR pig OR pigs OR porcine OR rat OR rats OR monkey * OR mouse OR mice OR canine OR feline OR “computer simulation” OR “passive heat stress” OR “classic heat stroke” OR “classic heatstroke” OR cancer OR cancers OR neoplasm * OR MDMA OR ecstasy OR ketamine OR “Lysergic Acid” OR “music festival” OR “Music festivals” OR hernia * OR “heat shock” |
| 2 | Line 1 (use pulldown to select title abstract keyword): mortal * OR death * OR died OR fatal OR fatally OR fatality OR survive OR survival OR survivor * OR saves OR saved AND Line 2 (use pulldown to select title abstract keyword): “Heat Stroke” OR “heat exhaustion” OR “heat illness” OR “heat illnesses” OR “heat related illness” OR “heat related illnesses” OR “heat stroke” OR “heat strokes” OR Heatstroke * OR EHS OR EHI OR “sun stroke” OR sunstroke * OR “heat injury” OR “heat injuries” OR Hyperthermia OR Hyperthermi * AND Line 3 (use pulldown to select title abstract keyword): sports OR military OR “armed forces” OR army OR navy OR marines OR “air force” OR “coast guard” OR “special forces” OR walking OR swimming OR soccer OR football OR futbol OR cricket OR rugby OR Skier * OR Skiing OR Basketball OR Tennis OR Judo OR Karate OR Boxing OR Lacrosse OR “field hockey” OR Golfing OR Golf OR Hockey OR Frisbee OR quidditch OR Horseback OR Wrestling OR “Water Polo” OR Snowboarding OR “Scuba Diving” OR “Rock Climbing” OR “Martial Arts” OR Kayaking OR Hiking OR “Cross Country” OR “Adventure Race” OR “Adventure Racing” OR cyclocross OR Baseball OR gymnastics OR gymnast OR rugby OR crossfit OR cross-fit OR skiing OR pre-season OR preseason OR recreational OR riding OR tournament OR workout * OR “return to activity” OR “return to duty” OR “physical conditioning” NOT Line 4 (use pulldown to select record title): animal * OR Comment * OR review OR letter OR editorial OR acclimat * OR acclimitizat * OR “air conditioning” OR “nursing home” OR “nursing homes” OR “non-exertional” OR veterinar * OR bovine OR pig OR pigs OR porcine OR rat OR rats OR monkey * OR mouse OR mice OR canine OR feline OR “computer simulation” OR “passive heat stress” OR “classic heat stroke” OR “classic heatstroke” OR cancer OR cancers OR neoplasm * OR MDMA OR ecstasy OR ketamine OR “Lysergic Acid” OR “music festival” OR “Music festivals” OR hernia * OR “heat shock” |
Appendix B. Joanna Briggs Institute Critical Appraisal Checklist for Case Reports and Case Series
| Yes | No | Unclear | Not Applicable | |
| 1. Were patient’s demographic characteristics clearly described? | □ | □ | □ | □ |
| 2. Was the patient’s history clearly described and presented as a timeline? | □ | □ | □ | □ |
| 3. Was the current clinical condition of the patient on presentation clearly described? | □ | □ | □ | □ |
| 4. Were diagnostic tests or assessment methods and the results clearly described? | □ | □ | □ | □ |
| 5. Was the intervention(s) or treatment procedure(s) clearly described? | □ | □ | □ | □ |
| 6. Was the post-intervention clinical condition clearly described? | □ | □ | □ | □ |
| 7. Were adverse events (harms) or unanticipated events identified and described? | □ | □ | □ | □ |
| 8. Does the case report provide takeaway lessons? | □ | □ | □ | □ |
| Yes | No | Unclear | Not Applicable | |
| 1. Were there clear criteria for inclusion in the case series? | □ | □ | □ | □ |
| 2. Was the condition measured in a standard, reliable way for all participants included in the case series? | □ | □ | □ | □ |
| 3. Were valid methods used for identification of the condition for all participants included in the case series? | □ | □ | □ | □ |
| 4. Did the case series have consecutive inclusion of participants? | □ | □ | □ | □ |
| 5. Did the case series have complete inclusion of participants? | □ | □ | □ | □ |
| 6. Was there clear reporting of the demographics of the participants in the study? | □ | □ | □ | □ |
| 7. Was there clear reporting of clinical information of the participants? | □ | □ | □ | □ |
| 8. Were the outcomes or follow up results of cases clearly reported? | □ | □ | □ | □ |
| 9. Was there clear reporting of the presenting site(s)/clinic(s) demographic information? | □ | □ | □ | □ |
| 10. Was statistical analysis appropriate? | □ | □ | □ | □ |
Appendix C. Case Series Definitions
References
- Bouchama, A.; Knochel, J.P. Heat Stroke. New Engl. J. Med. 2002, 346, 1978–1988. [Google Scholar] [CrossRef]
- Casa, D.J.; DeMartini, J.K.; Bergeron, M.F.; Csillan, D.; Eichner, E.R.; Lopez, R.M.; Ferrara, M.S.; Miller, K.C.; O’Connor, F.; Sawka, M.N.; et al. National Athletic Trainers’ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2015, 50, 986–1000. [Google Scholar] [CrossRef]
- American College of Sports Medicine; Armstrong, L.E.; Casa, D.J.; Millard-Stafford, M.; Moran, D.S.; Pyne, S.W.; Roberts, W.O. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med. Sci. Sports Exerc. 2007, 39, 556–572. [Google Scholar] [CrossRef] [PubMed]
- Epstein, Y.; Yanovich, R. Heatstroke. N. Engl. J. Med. 2019, 380, 2449–2459. [Google Scholar] [CrossRef]
- Belval, L.N.; Casa, D.J.; Adams, W.M.; Chiampas, G.T.; Holschen, J.C.; Hosokawa, Y.; Jardine, J.; Kane, S.F.; Labotz, M.; Lemieux, R.S.; et al. Consensus Statement—Prehospital Care of Exertional Heat Stroke. Prehosp. Emerg. Care. 2018, 22, 392–397. [Google Scholar] [CrossRef]
- Casa, D.J.; Guskiewicz, K.M.; Anderson, S.A.; Courson, R.W.; Heck, J.F.; Jimenez, C.C.; McDermott, B.P.; Miller, M.G.; Stearns, R.L.; Swartz, E.E.; et al. National athletic trainers’ association position statement: Preventing sudden death in sports. J. Athl. Train. 2012, 47, 96–118. [Google Scholar] [CrossRef]
- Casa, D.J.; McDermott, B.P.; Lee, E.C.; Yeargin, S.W.; Armstrong, L.E.; Maresh, C.M. Cold water immersion: The gold standard for exertional heatstroke treatment. Exerc. Sport Sci. Rev. 2007, 35, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Zeller, L.; Novack, V.; Barski, L.; Jotkowitz, A.; Almog, Y. Exertional heatstroke: Clinical characteristics, diagnostic and therapeutic considerations. Eur. J. Intern. Med. 2011, 22, 296–299. [Google Scholar] [CrossRef]
- DeMartini, J.K.; Casa, D.J.; Stearns, R.L.; Belval, L.N.; Crago, A.; Davis, R.; Jardine, J. Effectiveness of cold water immersion in the treatment of exertional heat stroke at the Falmouth Road Race. Med. Sci. Sports Exerc. 2015, 47, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Adams, W.M.; Hosokawa, Y.; Casa, D.J. The Timing of Exertional Heat Stroke Survival Starts prior to Collapse. Curr. Sports Med. Rep. 2015, 14, 273–274. [Google Scholar] [CrossRef] [PubMed]
- McDermott, B.P.; Casa, D.J.; Ganio, M.S.; Lopez, R.M.; Yeargin, S.W.; Armstrong, L.E.; Maresh, C.M. Acute whole-body cooling for exercise-induced hyperthermia: A systematic review. J. Athl. Train. 2009, 44, 84–93. [Google Scholar] [CrossRef]
- O’Connor, F.G.; Williams, A.D.; Blivin, S.; Heled, Y.; Deuster, P.; Flinn, S.D. Guidelines for return to duty (play) after heat illness: A military perspective. J. Sport Rehabil. 2007, 16, 227–237. [Google Scholar] [CrossRef]
- Heled, Y.; Rav-Acha, M.; Shani, Y.; Epstein, Y.; Moran, D.S. The “golden hour” for heatstroke treatment. Mil. Med. 2004, 169, 184–186. [Google Scholar] [CrossRef]
- Armed Forces Health Surveillance Branch. Update: Heat Illness, active component, U.S. Armed Forces 2017. MSMR 2018, 25, 6–12. [Google Scholar]
- Armed Forces Health Surveillance Branch. Update: Heat illness, active component, U.S. Armed Forces 2016. MSMR 2017, 24, 9–13. [Google Scholar]
- Armed Forces Health Surveillance Branch. Update: Heat illness, active component, U.S. Armed Forces 2015. MSMR 2016, 23, 16–19. [Google Scholar]
- Armed Forces Health Surveillance Branch. Update: Heat illness, active component, U.S. Armed Forces 2014. MSMR 2015, 22, 17–20. [Google Scholar]
- Armed Forces Health Surveillance Branch. Update: Heat illness, active component, U.S. Armed Forces 2013. MSMR 2014, 21, 10–13. [Google Scholar]
- Armed Forces Health Surveillance Branch. Update: Heat injuries, active component, U.S. Armed Forces, 2012. MSMR 2013, 20, 17–20. [Google Scholar]
- Armed Forces Health Surveillance Branch. Update: Heat injuries, active component, U.S. Armed Forces, 2011. MSMR 2012, 19, 14–16. [Google Scholar]
- Armed Forces Health Surveillance Branch. Update: Heat injuries, active component, U.S. Armed Forces, 2010. MSMR 2011, 18, 6–8. [Google Scholar]
- Armed Forces Health Surveillance Branch. Update: Heat injuries, active component, U.S. Armed Forces, 2009. MSMR 2010, 17, 6–8. [Google Scholar]
- Armed Forces Health Surveillance Branch. Update: Heat injuries, active component, U.S. Armed Forces, 2008. MSMR 2009, 17, 6–8. [Google Scholar]
- Lopez, R.M.; Casa, D.J.; McDermott, B.P.; Stearns, R.L.; Armstrong, L.E.; Maresh, C.M. Exertional Heat Stroke in the Athletic Setting: A Review of the Literature. Athl. Train. Sports Heal. Care 2010, 3, 189–200. [Google Scholar] [CrossRef]
- Rav-Acha, M.; Hadad, E.; Epstein, Y.; Heled, Y.; Moran, D.S. Fatal exertional heat stroke: A case series. Am. J. Med. Sci. 2004, 328, 84–87. [Google Scholar] [CrossRef]
- Asserraji, M.; Benameur, I.; Maoujoud, O.; El Kharras, A.; Hajbi, H.; Filali, K. Late care in marathon runs leading to exertional heat stroke with multiple organ failure. Asian J. Sports Med. 2014, 5, 136–138. [Google Scholar]
- Assia, E.; Epstein, Y.; Shapiro, Y. Fatal heatstroke after a short march at night: A case report. Aviat. Space Environ. Med. 1985, 56, 441–442. [Google Scholar]
- Grundstein, A.; Knox, J.A.; Vanos, J.; Cooper, E.R.; Casa, D.J. American football and fatal exertional heat stroke: A case study of Korey Stringer. Int. J. Biometeorol. 2017, 61, 1471–1480. [Google Scholar] [CrossRef]
- Barthel, H.J. Exertion-induced heat stroke in a military setting. Mil. Med. 1990, 155, 116–119. [Google Scholar] [CrossRef]
- Kerr, Z.Y.; Marshall, S.W.; Comstock, R.D.; Casa, D.J. Exertional heat stroke management strategies in United States high school football. Am. J. Sports Med. 2014, 42, 70–77. [Google Scholar] [CrossRef]
- Beller, G.A.; Boyd, A.E., 3rd. Heat stroke: A report of 13 consecutive cases without mortality despite severe hyperpyrexia and neurologic dysfunction. Mil. Med. 1975, 140, 464–467. [Google Scholar] [CrossRef]
- Goforth, C.W.; Kazman, J.B. Exertional heat stroke in navy and marine personnel: A hot topic. Crit. Care Nurs. 2015, 35, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Abriat, A.; Brosset, C.; Brégigeon, M.; Sagui, E. Report of 182 cases of exertional heatstroke in the French Armed Forces. Mil. Med. 2014, 179, 309–314. [Google Scholar] [CrossRef]
- Nelson, D.A.; Deuster, P.A.; O’Connor, F.G.; Kurina, L.M. Timing and Predictors of Mild and Severe Heat Illness among New Military Enlistees. Med. Sci. Sports Exerc. 2018, 50, 1603–1612. [Google Scholar] [CrossRef]
- Kark, J.A.; Burr, P.Q.; Wenger, C.B.; Gastaldo, E.; Gardner, J.W. Exertional heat illness in Marine Corps recruit training. Aviat. Space Environ. Med. 1996, 67, 354–360. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Munn, Z.; Moola, S.; Riitano, D.; Lisy, K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int. J. Health Policy Manag. 2014, 3, 123–128. [Google Scholar] [CrossRef]
- Porritt, K.; Gomersall, J.; Lockwood, C. JBI’s Systematic Reviews: Study selection and critical appraisal. Am. J. Nurs. 2014, 114, 47–52. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; et al. Chapter 7: Systematic Reviews of Etiology and Risk. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E.M.Z., Ed.; Joanna Briggs Institute: Adelaide, Australia, 2017; p. 1. [Google Scholar]
- Munn, Z.; Tufanaru, C.; Aromataris, E. JBI’s systematic reviews: Data extraction and synthesis. Am. J. Nurs. 2014, 114, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Field, A. Discovering Statistics Using IBM SPSS Statistics: North American Edition; Sage: New York, NY, USA, 2017. [Google Scholar]
- Zhang, Y.; Davis, J.K.; Casa, D.J.; Bishop, P.A. Optimizing Cold Water Immersion for Exercise-Induced Hyperthermia: A Meta-analysis. Med. Sci. Sports Exerc. 2015, 47, 2464–2472. [Google Scholar] [CrossRef]
- Proulx, C.I.; Ducharme, M.B.; Kenny, G.P. Effect of water temperature on cooling efficiency during hyperthermia in humans. J. Appl. Physiol. (1985) 2003, 94, 1317–1323. [Google Scholar] [CrossRef]
- Proulx, C.I.; Ducharme, M.B.; Kenny, G.P. Safe cooling limits from exercise-induced hyperthermia. Eur. J. Appl. Physiol. 2006, 96, 434–445. [Google Scholar] [CrossRef] [PubMed]
- Bursey, M.M.; Galer, M.; Oh, R.C.; Weathers, B.K. Successful Management of Severe Exertional Heat Stroke with Endovascular Cooling After Failure of Standard Cooling Measures. J. Emerg. Med. 2019, 57, e53–e56. [Google Scholar] [CrossRef]
- Johnston, J.; Donham, B. Exertional heat stroke: Clinical significance and practice indications for special operations medics and providers. J. Spec. Oper Med. 2012, 12, 1–7. [Google Scholar]
- Stearns, R.L.; Casa, D.J.; O’Connor, F.G.; Lopez, R.M. A Tale of Two Heat Strokes: A Comparative Case Study: Erratum. Curr. Sports Med. Rep. 2016, 15, 215–218. [Google Scholar] [CrossRef]
- Lew, H.L.; Lee, E.H.; Date, E.S.; Melnik, I. Rehabilitation of a patient with heat stroke: A case report. Am. J. Phys. Med. Rehabil. 2002, 81, 629–632. [Google Scholar] [CrossRef]
- Deshwal, R.; Tiwari, D.; Singh, R. Clinical and Biochemical Characteristics of Exertional Heat Stroke among Paratroopers in Agra, India. J. Assoc. Physicians India. 2017, 65, 57–61. [Google Scholar]
- Carvalho, A.S.; Rodeia, S.C.; Silvestre, J.; Póvoa, P. Exertional heat stroke and acute liver failure: A late dysfunction. BMJ Case Rep. 2016, 2016. [Google Scholar] [CrossRef]
- Giercksky, T.; Boberg, K.M.; Farstad, I.N.; Halvorsen, S.; Schrumpf, E. Severe liver failure in exertional heat stroke. Scand. J. Gastroenterol. 1999, 34, 824–827. [Google Scholar] [PubMed]
- Lopez, R.M.; Tanner, P.; Irani, S.; Mularoni, P.P. A Functional Return-to-Play Progression after Exertional Heat Stroke in a High School Football Player. J. Athl. Train. 2018, 53, 230–239. [Google Scholar] [CrossRef]
- Raj, V.M.; Alladin, A.; Pfeiffer, B.; Defreitas, M.; Edwards-Richards, A.; Chandar, J.; Seeherunvong, W.; McLaughlin, G.; Zilleruelo, G.; Abitbol, C.L. Therapeutic plasma exchange in the treatment of exertional heat stroke and multiorgan failure. Pediatr Nephrol. 2013, 28, 971–974. [Google Scholar] [CrossRef] [PubMed]
- Sithinamsuwan, P.; Piyavechviratana, K.; Kitthaweesin, T.; Chusri, W.; Orrawanhanothai, P.; Wongsa, A.; Wattanathum, A.; Chinvarun, Y.; Nidhinandana, S.; Satirapoj, B.; et al. Exertional heatstroke: Early recognition and outcome with aggressive combined cooling—A 12-year experience. Mil. Med. 2009, 174, 496–502. [Google Scholar] [CrossRef]
- Sloan, B.K.; Kraft, E.M.; Clark, D.; Schmeissing, S.W.; Byrne, B.C.; Rusyniak, D.E. On-site treatment of exertional heat stroke. Am. J. Sports Med. 2015, 43, 823–829. [Google Scholar] [CrossRef]
- Stewart, T.E.; Whitford, A.C. Dangers of Prehospital Cooling: A Case Report of Afterdrop in a Patient with Exertional Heat Stroke. J. Emerg. Med. 2015, 49, 630–633. [Google Scholar] [CrossRef]
- Takahashi, K.; Chin, K.; Ogawa, K.; Kasahara, M.; Sakaguchi, T.; Hasegawa, S.; Sumi, K.; Nakamura, T.; Tamaki, A.; Mishima, M.; et al. Living donor liver transplantation with noninvasive ventilation for exertional heat stroke and severe rhabdomyolysis. Liver Transpl. 2005, 11, 570–572. [Google Scholar] [CrossRef]
- Trujillo, M.H.; Bellorin-Font, E.; Fragachan, C.F.; Perret-Gentil, R. Multiple Organ Failure Following Near Fatal Exertional Heat Stroke. J. Intensive Care Med. 2009, 24, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Yue, H.; Zhou, F.; Liu, H.; Kang, H.; Pan, L.; Gu, B.; Song, Q. Fatal exertional heat stroke successfully treated with cold hemofiltration: A case report. Am. J. Emerg. Med. 2009, 27, 751. [Google Scholar] [CrossRef] [PubMed]
- Kurowski, J.A.; Lin, H.C.; Mohammad, S.; Krug, S.; Alonso, E.M. Exertional Heat Stroke in a Young Athlete Resulting in Acute Liver Failure. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 75–76. [Google Scholar] [CrossRef]
- Armstrong, L.E.; Crago, A.E.; Adams, R.; Roberts, W.O.; Maresh, C.M. Whole-body cooling of hyperthermic runners: Comparison of two field therapies. Am. J. Emerg. Med. 1996, 14, 355–358. [Google Scholar] [CrossRef]
- Rohe, S.T. Exertional heat illness in a Marine training on the endurance course. JAAPA 2012, 25, 34–38. [Google Scholar] [CrossRef] [PubMed]
- McDermott, B.P.; Casa, D.J.; O’Connor, F.G.; Adams, W.B.; Armstrong, L.E.; Brennan, A.H.; Lopez, R.M.; Stearns, R.L.; Troyanos, C.; Yeargin, S.W. Cold-water dousing with ice massage to treat exertional heat stroke: A case series. Aviat. Space Environ. Med. 2009, 80, 720–722. [Google Scholar] [CrossRef] [PubMed]
- Katch, R.K.; Scarneo, S.E.; Adams, W.M.; Armstrong, L.E.; Belval, L.N.; Stamm, J.M.; Casa, D.J. Top 10 Research Questions Related to Preventing Sudden Death in Sport and Physical Activity. Res. Q. Exerc. Sport. 2017, 88, 251–268. [Google Scholar] [CrossRef]
- Hosokawa, Y.; Adams, W.M.; Belval, L.N.; Vandermark, L.W.; Casa, D.J. Tarp-Assisted Cooling as a Method of Whole-Body Cooling in Hyperthermic Individuals. Ann. Emerg. Med. 2017, 69, 347–352. [Google Scholar] [CrossRef]
- Luhring, K.E.; Butts, C.L.; Smith, C.R.; Bonacci, J.A.; Ylanan, R.C.; Ganio, M.S.; McDermott, B.P. Cooling Effectiveness of a Modified Cold-Water Immersion Method after Exercise-Induced Hyperthermia. J. Athl. Train. 2016, 51, 946–951. [Google Scholar] [CrossRef] [PubMed]
- Parker, K.C.; Shelton, R.R.; Lopez, R.M. Do Alternative Cooling Methods Have Effective Cooling Rates for Hyperthermia Compared With Previously Established CWI Cooling Rates? J. Sport Rehabil. 2019, 1–6. [Google Scholar] [CrossRef] [PubMed]
- DeGroot, D.W.; Mok, G.; Hathaway, N.E. International Classification of Disease Coding of Exertional Heat Illness in U.S. Army Soldiers. Mil. Med. 2017, 182, e1946–e1950. [Google Scholar] [CrossRef] [PubMed]
- Howick, J.C.I.; Glasziou, P.; Greenhalgh, T.; Liberati, A.; Moschetti, I.; Philips, B.; Thornton, H.; Goddard, O.; Hodgkinson, M. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. Available online: http://www.cebm.net/index.aspx?o=5653 (accessed on 1 June 2020).
- Ebell, M.H.; Siwek, J.; Weiss, B.D.; Woolf, S.H.; Susman, J.; Ewigman, B.; Bowman, M. Strength of recommendation taxonomy (SORT): A patient-centered approach to grading evidence in the medical literature. J. Am. Board Fam. Pract. 2004, 17, 59–67. [Google Scholar] [CrossRef]


| Author, Year | Military Location | Tb Method | Tb | Cooling Modality | Patient Outcomes (n) | Total Patients (n) | ||
|---|---|---|---|---|---|---|---|---|
| Fatality | S | SMC | ||||||
| Rav-Acha et al., 2004 | Israel Defense Force | NR | NR | None (n= 4); Water dousing + IV (n = 2) | 6 | 6 | ||
| Venuto et al., 2011 | U.S. Air Force | Rectal | 42.22 °C | NR | 1 | 1 | ||
| Parnell and Restall, 1986 | British Armed Forces | Rectal and Esophageal | Rectal = 40 °C, Esophageal = 42.8 °C | Tepid water sponging + Fan+ Cooling blanket | 1 | 1 | ||
| Shibolet et al., 1967 | Israel Defense Force | NR | Mean Tb 41.0 °C | NR | 8 | 28 | 36 | |
| Sithinamsuwan et al., 2009 | Thailand Military | NR | Median Tb 41.6 °C | Ice packs + Water dousing + Fan + Cooling blanket + Cold spray | 2 | 26 | 28 | |
| McDermott et al., 2009 | U.S. Marines | Rectal | 41.44 ± 0.71 °C | Cold water dousing + Ice bag massage | 9 | 9 | ||
| Beller and Boyd, 1975 | U.S. Army | Rectal | 42.0 ± 0.2 °C | CWI | 13 | 13 | ||
| Rohe, 2012 | U.S. Marines | Rectal | 41 °C | Ice packs on arteries + Cold water dousing + Fan | 1 | 1 | ||
| Barthel, 1990 | U.S. Army | NR | 41.1 °C | Tepid water sponging + Fan + Ice Massage | 1 | 1 | ||
| Stearns et al., 2016 | U.S. Marines | Rectal | 41.1 °C | CWI | 1 | 1 | ||
| U.S. Marines | Rectal | 41.2 °C | Ice Packs + Cooling Blanket | 1 | 1 | |||
| Johnston and Donham, 2012 | U.S. Army, Special Forces | NR | 40.5 °C * | Ice packs + Fan | 1 | 1 | ||
| Deshwal et al., 2017 | India Special Forces | Rectal | 41.41 ± 0.88 °C | Ice packs+ Fan + Cold spray + Cold Saline IV + O2 | 78 | 78 | ||
| Bursey et al. 2019 | U.S. Army | Rectal | 43.1 °C | Ice Sheeting | 1 | 1 | ||
| Lew et al., 2002 | U.S. Army | Oral | 41.4 °C | None | 1 | 1 | ||
| Stewart and Whitford, 2015 | U.S. Army | Rectal + Oral | 42.27 °C; 42.1 °C | None | 1 | 1 | ||
| Author, Year | Specific Activity | Tb Method | Tb | Cooling Modality | Patient Outcomes (n) | Total Patients (n) | ||
|---|---|---|---|---|---|---|---|---|
| F | S | SMC | ||||||
| Whitworth and Wolfman, 1983 | Marathon (42.2 km) | NR | 40 °C | Ice packs | 1 | 1 | ||
| Grundstein et al. 2016 | American Football | NR | 42.67 °C ** | None | 1 | 1 | ||
| Asserraji et al., 2015 | Marathon (42.2 km) | NR | 37.5 °C * | None | 1 | 1 | ||
| Rae et al., 2008 | Cycling | Rectal | 41.2 °C | NR | 1 | 1 | ||
| Cycling | Rectal | 41.8 °C | NR | 1 | 1 | |||
| Cycling | Rectal | 42 °C | Cold water dousing + Fan | 1 | 1 | |||
| Armstrong et al., 1995 | Road Race (11.26 km) | Rectal | 40.7 ± 0.6 °C | Air exposure + Ice Towels | 5 | 5 | ||
| Road Race (11.26 km) | Rectal | 41.7 ± 0.2 °C | CWI | 14 | 14 | |||
| Whitcar et al., 2007 | Recreational Run (9.6 km) | NR | 39.3 °C | Cold IV fluids + fan | 1 | 1 | ||
| DeMartini et al., 2015 | Road Race (11.26 km) | Rectal | 41.44 ± 0.63 °C | CWI | 274 | 274 | ||
| Adams et al., 2016 | Road Race (11.26 km) | Rectal | 42.05 °C | CWI + Ice Towels | 1 | 1 | ||
| Sloan et al., 2015 | Marathon (42.2 km) | Rectal, Oral, Tympanic | 40.80 ± 2.4 °C | CWI + IV Fluids + Ice packs + Ice Towels † | 29 | 3 | 32 | |
| Raj et al., 2013 | Hiking | NR | 41.67 °C | IV fluids | 1 | 1 | ||
| Kurowski et al., 2016 | Wrestling | Oral | 40.5 °C | CWI ‡,* | 1 | 1 | ||
| Takahashi et al., 2005 | Rugby | Rectal | 42 °C | IV fluids | 1 | 1 | ||
| Trujlio et al., 2009 | Hiking | Oral | 39 °C | None | 1 | 1 | ||
| Giercksy et al., 1999 | Road Race (5 km) | NR | 42.1 °C | None | 1 | 1 | ||
| Lopez et al., 2018 | American Football | Oral | 39.6 °C | None | 1 | 1 | ||
| Carvalho et al., 2016 | Marathon (42.2 km) | Tympanic | 39.6 °C | NR | 1 | 1 | ||
| Yue et al., 2009 | Recreational Run (4.8 km) | Rectal | 42.2 °C | Surgical: Cold Hemofiltration‡ | 1 | 1 | ||
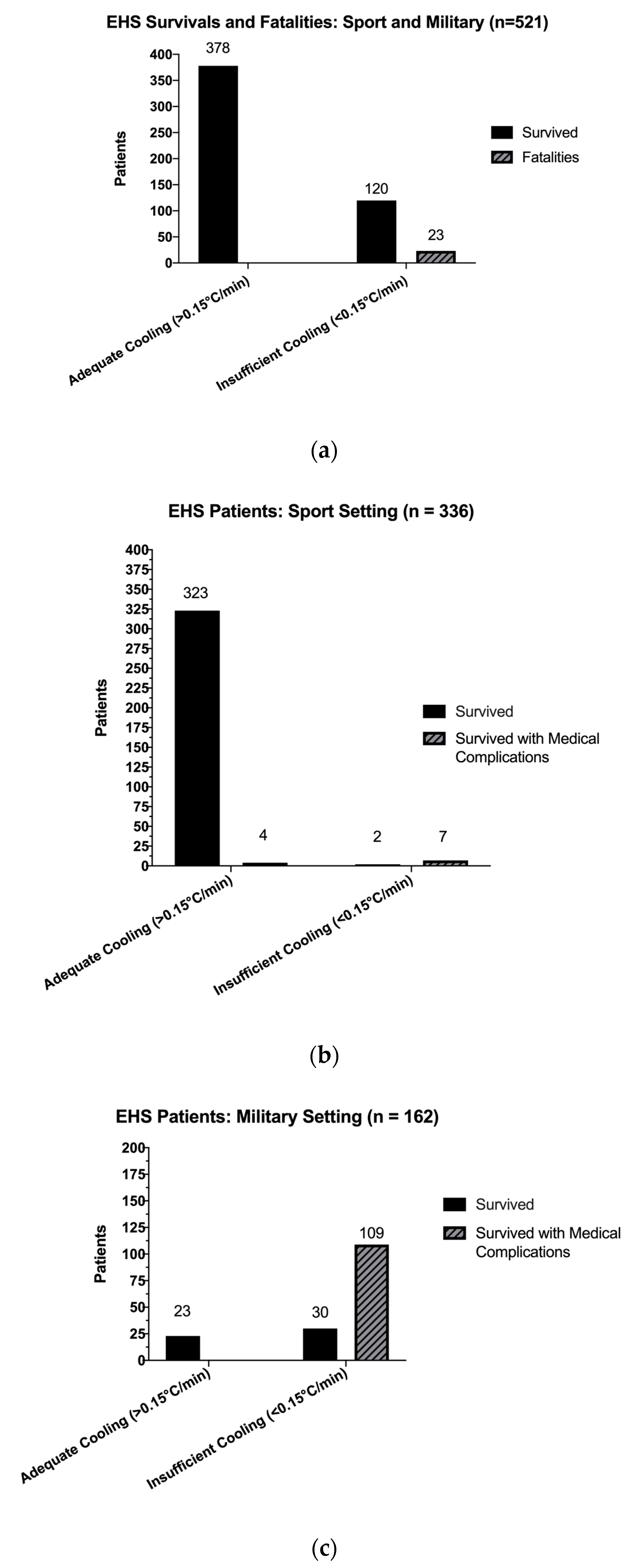
| Survived, n | Fatalities, n | Total n, (%) | |
|---|---|---|---|
| Adequate Cooling Rate (>0.15 °C/min) | 378 | 0 | 378 (72.55%) |
| Insufficient Cooling Rate (<0.15 °C/min) | 120 | 23 | 143 (27.44%) |
| Total n, (%) | 498 | 23 | 521 (100.00%) |
| a. Survived and Survived with Medical Complications, all settings. | |||
| Survived, n | Survived with Medical Complications, n | Total n, (%) | |
| Adequate Cooling Rate (>0.15 °C/min) | 346 | 4 | 350 (70.28%) |
| Insufficient Cooling Rate (<0.15 °C/min) | 32 | 116 | 148 (29.72%) |
| Total n, (%) | 378 | 120 | 498 (100.00%) |
| b. Patient Survival from EHS in Sport. | |||
| Survived, n | Survived with Medical Complications, n | Total n, (%) | |
| Adequate Cooling Rate (>0.15 °C/min) | 323 | 4 | 327 (97.32%) |
| Insufficient Cooling Rate (<0.15 °C/min) | 2 | 7 | 9 (2.68%) |
| Total n, (%) | 325 | 11 | 336 (100.00%) |
| c. Patient Survival from EHS in the Military | |||
| Survived, n | Survived with Medical Complications, n | Total n, (%) | |
| Adequate Cooling Rate (>0.15 °C/min) | 23 | 0 | 23 (14.20%) |
| Insufficient Cooling Rate (<0.15 °C/min) | 30 | 109 | 139 (85.80%) |
| Total n, (%) | 53 | 109 | 162 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Filep, E.M.; Murata, Y.; Endres, B.D.; Kim, G.; Stearns, R.L.; Casa, D.J. Exertional Heat Stroke, Modality Cooling Rate, and Survival Outcomes: A Systematic Review. Medicina 2020, 56, 589. https://doi.org/10.3390/medicina56110589
Filep EM, Murata Y, Endres BD, Kim G, Stearns RL, Casa DJ. Exertional Heat Stroke, Modality Cooling Rate, and Survival Outcomes: A Systematic Review. Medicina. 2020; 56(11):589. https://doi.org/10.3390/medicina56110589
Chicago/Turabian StyleFilep, Erica M., Yuki Murata, Brad D. Endres, Gyujin Kim, Rebecca L. Stearns, and Douglas J. Casa. 2020. "Exertional Heat Stroke, Modality Cooling Rate, and Survival Outcomes: A Systematic Review" Medicina 56, no. 11: 589. https://doi.org/10.3390/medicina56110589
APA StyleFilep, E. M., Murata, Y., Endres, B. D., Kim, G., Stearns, R. L., & Casa, D. J. (2020). Exertional Heat Stroke, Modality Cooling Rate, and Survival Outcomes: A Systematic Review. Medicina, 56(11), 589. https://doi.org/10.3390/medicina56110589






