Exertional Heat Illness Preparedness Strategies: Environmental Monitoring Policies in United States High Schools
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Questionnaire
2.3. Data Analysis
3. Results
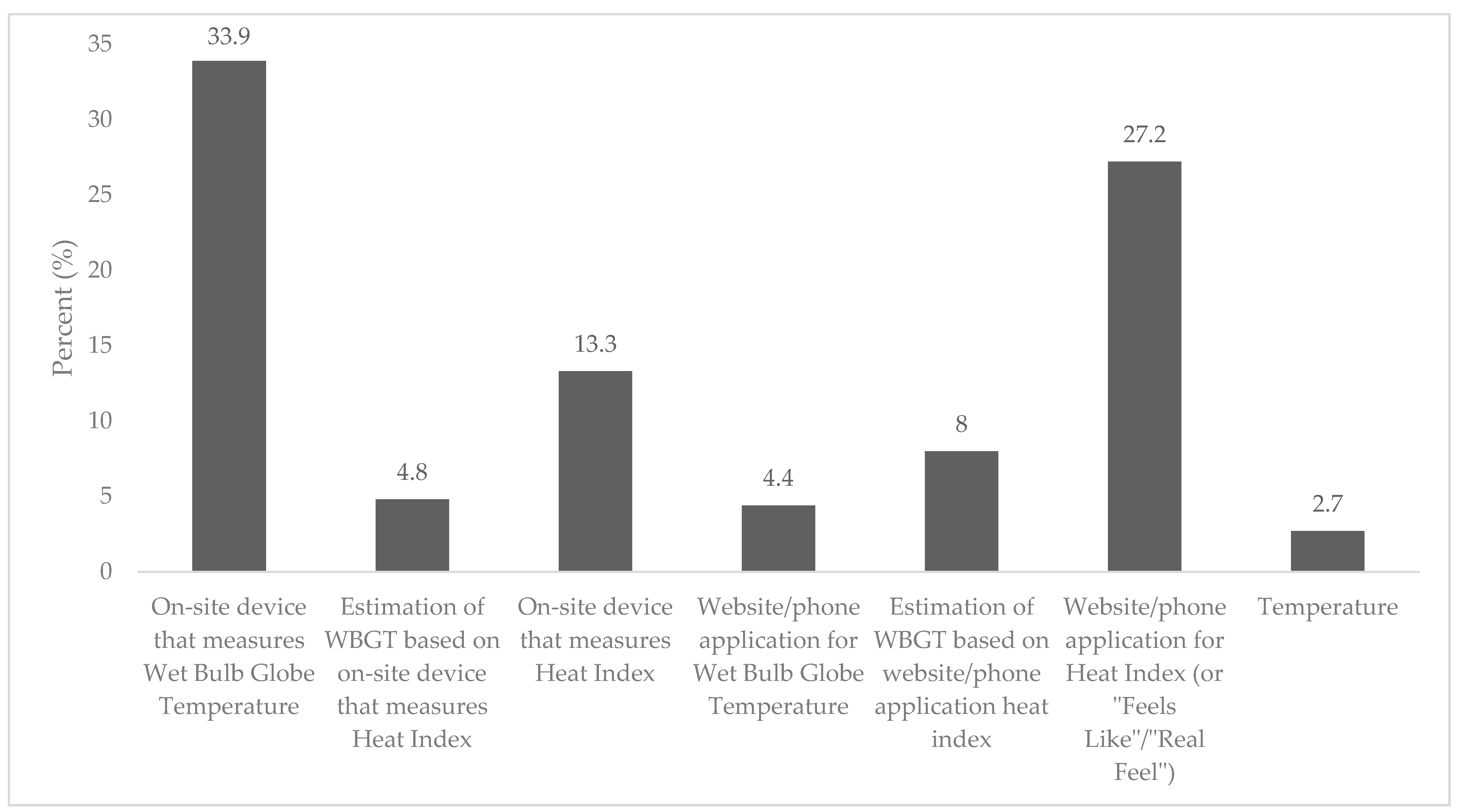
3.1. Adoption
3.2. Facilitators and Barriers for Adoption of a Comprehensive Environmental Monitoring Policy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Meehl, G.A. More Intense, More Frequent, and Longer Lasting Heat Waves in the 21st Century. Science 2004, 305, 994–997. [Google Scholar] [CrossRef] [PubMed]
- Yeargin, S.W.; Dompier, T.P.; Casa, D.J.; Hirschhorn, R.M.; Kerr, Z.Y. Epidemiology of Exertional Heat Illnesses in National Collegiate Athletic Association Athletes During the 2009–2010 Through 2014–2015 Academic Years. J. Athl. Train. 2019, 54, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Kerr, Z.Y.; Register-Mihalik, J.K.; Pryor, R.R.; Pierpoint, L.A.; Scarneo, S.E.; Adams, W.M.; Kucera, K.L.; Casa, D.J.; Marshall, S.W. The Association between Mandated Preseason Heat Acclimatization Guidelines and Exertional Heat Illness during Preseason High School American Football Practices. Environ. Health Perspect. 2019, 127, 047003. [Google Scholar] [CrossRef] [PubMed]
- Kerr, Z.Y.; Casa, D.J.; Marshall, S.W.; Comstock, R.D. Epidemiology of Exertional Heat Illness Among U.S. High School Athletes. Am. J. Prev. Med. 2013, 44, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, Y.; Casa, D.J.; Trtanj, J.M.; Belval, L.N.; Deuster, P.A.; Giltz, S.M.; Grundstein, A.J.; Hawkins, M.D.; Huggins, R.A.; Jacklitsch, B.; et al. Activity modification in heat: Critical assessment of guidelines across athletic, occupational, and military settings in the USA. Int. J. Biometeorol. 2019, 63, 405–427. [Google Scholar] [CrossRef]
- Cooper, E.R.; Grundstein, A.J.; Miles, J.D.; Ferrara, M.S.; Curry, P.; Casa, D.J.; Hosokawa, Y. Heat Policy Revision for Georgia High School Football Practices Based on Data-Driven Research. J. Athl. Train. 2020. [Google Scholar] [CrossRef]
- Budd, G.M. Wet-bulb globe temperature (WBGT)—Its history and its limitations. J. Sci. Med. Sport 2008, 11, 20–32. [Google Scholar] [CrossRef]
- Minard, D. Prevention of heat casualties in Marine Corps recruits. Period of 1955–60, with comparative incidence rates and climatic heat stresses in other training categories. Mil. Med. 1961, 126, 261–272. [Google Scholar] [CrossRef]
- Armstrong, L.E.; Johnson, E.C.; Casa, D.J.; Ganio, M.S.; McDermott, B.P.; Yamamoto, L.M.; Lopez, R.M.; Emmanuel, H. The American football uniform: Uncompensable heat stress and hyperthermic exhaustion. J. Athl. Train. 2010, 45, 117–127. [Google Scholar] [CrossRef]
- Casa, D.; DeMartini, J.K.; Bergeron, M.F.; Csillan, D.; Eichner, E.R.; Lopez, R.M.; Ferrara, M.S.; Miller, K.C.; O’Connor, F.; Sawka, M.N.; et al. National Athletic Trainers’ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2015, 50, 986–1000. [Google Scholar] [CrossRef]
- Tripp, B.; Vincent, H.K.; Bruner, M.; Smith, M.S. Comparison of wet bulb globe temperature measured on-site vs estimated and the impact on activity modification in high school football. Int. J. Biometeorol. 2020, 64, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Pryor, J.L.; Pryor, R.R.; Grundstein, A.; Casa, D.J. The Heat Strain of Various Athletic Surfaces: A Comparison Between Observed and Modeled Wet-Bulb Globe Temperatures. J. Athl. Train. 2017, 52, 1056–1064. [Google Scholar] [CrossRef] [PubMed]
- Grundstein, A.; Williams, C.; Phan, M.; Cooper, E. Regional heat safety thresholds for athletics in the contiguous United States. Appl. Geogr. 2015, 56, 55–60. [Google Scholar] [CrossRef]
- Armstrong, L.E.; Casa, D.J.; Millard-Stafford, M.; Moran, D.S.; Pyne, S.W.; Roberts, W.O.; American College of Sports Medicine. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med. Sci. Sport Exerc. 2007, 39, 556–572. [Google Scholar] [CrossRef]
- Scarneo, S.E.; Distefano, L.J.; Stearns, R.L.; Register-Mihalik, J.K.; Denegar, C.R.; Casa, D.J. Emergency Action Planning in Secondary-School Athletics: A Comprehensive Evaluation of Current Adoption of Best Practice Standards. J. Athl. Train. 2019, 54, 99–105. [Google Scholar] [CrossRef]
- Scarneo-Miller, S.E.; DiStefano, L.J.; Register-Mihalik, J.K.; Stearns, R.L.; Denegar, C.R.; Casa, D.J. Athletic Administrators Report of Emergency Action Plan Adoption in Secondary School Athletics. Appl. J. Sport Manag. 2019, 11, 1–10. [Google Scholar] [CrossRef]
- Kerr, Z.Y.; Register-Mihalik, J.K.; Pryor, R.R.; Hosokawa, Y.; Scarneo-Miller, S.E.; Casa, D.J. Compliance with the National Athletic Trainers’ Association Inter-Association Task Force Preseason Heat-Acclimatization Guidelines in High School Football. J. Athl. Train. 2019, 54, 749–757. [Google Scholar] [CrossRef]
- Murata, Y.; Scarneo-Miller, S.E.; McMahon, L.; Casa, D. Adoption of Emergency Action Plans in Secondary Schools: A Study of School Nurses’ Knowledge and Behavior. J. School Health 2020, 90, 694–702. [Google Scholar] [CrossRef]
- Scarneo-Miller, S.E.; DiStefano, L.J.; Singe, S.M.; Register-Mihalik, J.K.; Stearns, R.L.; Casa, D.J. Emergency Action Plans in Secondary Schools: Barriers, Facilitators, and Social Determinants Affecting Implementation. J. Athl. Train. 2020, 55, 80–87. [Google Scholar] [CrossRef]
- Adams, W.M.; Scarneo, S.E.; Casa, D.J. State-Level Implementation of Health and Safety Policies to Prevent Sudden Death and Catastrophic Injuries Within Secondary School Athletics. Orthop. J. Sports Med. 2017, 5, 1–8. [Google Scholar] [CrossRef]
- Athletic Training Locations and Services (ATLAS Project). Available online: https://ksi.uconn.edu/nata-atlas/ (accessed on 15 February 2018).
- Crossway, A.; Rogers, S.M.; Nye, E.A.; Games, K.E.; Eberman, L.E. Lesbian, Gay, Bisexual, Transgender, and Queer Athletic Trainers: Collegiate Student-Athletes’ Perceptions. J. Athl. Train. 2019, 54, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; Almquist, J.; Anderson, S.A.; Baker, L.; Bergeron, M.F.; Biagioli, B.; Boden, B.; Brenner, J.S.; Carroll, M.; Colgate, B.; et al. The inter-association task force for preventing sudden death in secondary school athletics programs: Best-practices recommendations. J. Athl. Train. 2013, 48, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Casa, D.J.; Guskiewicz, K.M.; Anderson, S.A.; Courson, R.W.; Heck, J.F.; Jimenez, C.C.; McDermott, B.P.; Miller, M.G.; Stearns, R.L.; Swartz, E.E.; et al. National athletic trainers’ association position statement: Preventing sudden death in sports. J. Athl. Train. 2012, 47, 96–118. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, N.D.; Sandman, P.M.; Blalock, S.J. The Precaution Adoption Process Model. In Health Behavior and Health Education; Jossey-Bass: San Francisco, CA, USA, 2008; Volume 21, pp. 123–147. [Google Scholar]
- Binkley, H.M.; Beckett, J.; Casa, D.J.; Kleiner, D.M.; Plummer, P.E. National Athletic Trainers’ Association Position Statement: Exertional Heat Illnesses. J. Athl. Train. 2002, 37, 329–343. [Google Scholar]
- Grundstein, A.; Cooper, E. Assessment of the Australian Bureau of Meteorology wet bulb globe temperature model using weather station data. Int. J. Biometeorol. 2018, 62, 2205–2213. [Google Scholar] [CrossRef]
- Cooper, E.R.; Ferrara, M.S.; Casa, D.J.; Powell, J.W.; Broglio, S.P.; Resch, J.E.; Courson, R.W. Exertional Heat Illness in American Football Players: When Is the Risk Greatest? J. Athl. Train. 2016, 51, 593–600. [Google Scholar] [CrossRef]
- Grundstein, A.J.; Hosokawa, Y.; Casa, D.J. Fatal Exertional Heat Stroke and American Football Players: The Need for Regional Heat-Safety Guidelines. J. Athl. Train. 2018, 53, 43–50. [Google Scholar] [CrossRef]


| Age | 35 ± 9 years | Students | 1297 ± 1044 students |
| Years in Profession | Years at High School | ||
| Less than 1 year | 5 (0.9) | Less than 1 year | 30 (5.7) |
| 1–5 years | 169 (31.9) | 1–5 years | 288 (54.5) |
| 6–10 years | 125 (23.6) | 6–10 years | 95 (18) |
| 11–15 years | 73 (13.8) | 11–15 years | 53 (10) |
| 15 or more years | 158 (29.8) | 15 or more years | 61 (11.7) |
| States | |||
| AL | 7 (1.3) | MS | 2 (0.4) |
| AR | 6 (1.1) | MT | 6 (1.1) |
| AZ | 8 (1.5) | NC | 31 (5.8) |
| CA | 26 (4.9) | NE | 5 (0.9) |
| CO | 7 (1.3) | NH | 2 (0.4) |
| CT | 5 (0.9) | NJ | 24 (4.5) |
| DC | 1 (0.2) | NM | 6 (1.1) |
| FL | 28 (5.3) | NV | 2 (0.4) |
| GA | 16 (3) | NY | 12 (2.3) |
| HI | 3 (0.6) | OH | 23 (4.3) |
| IA | 6 (1.1) | OK | 6 (1.1) |
| ID | 3 (0.6) | OR | 8 (1.5) |
| IL | 10 (1.9) | PA | 23 (4.3) |
| IN | 19 (3.6) | RI | 2 (0.4) |
| KS | 2 (0.4) | SC | 12 (2.3) |
| KY | 5 (0.9) | TN | 9 (1.7) |
| LA | 10 (1.9) | TX | 59 (11.1) |
| MA | 13 (2.4) | UT | 6 (1.1) |
| MD | 10 (1.9) | VA | 24 (4.5) |
| ME | 5 (0.9) | VT | 2 (0.4) |
| MI | 15 (2.8) | WA | 15 (2.8) |
| MN | 7 (1.3) | WI | 12 (2.3) |
| MO | 10 (1.9) | WY | 3 (0.6) |
| Not reported | 16 (3.0) | ||
| Components of Best Practice Standards Q: My School’s Policies and Procedures | Aggregate (Both Fall + Spring) | Fall | Spring |
|---|---|---|---|
| Include exertional heat illness (prevention and treatment) (total sample sizes for aggregate = 529, fall = 311, spring = 218) | 368 (69.6) | 217 (69.8) | 151 (69.3) |
| Are based on environmental conditions measured by an on-site wet-bulb globe thermometer (total sample sizes for aggregate = 364, fall = 214, spring = 150) | 205 (56.31) | 115 (53.7) | 90 (60.0) |
| Are based on environmental conditions that are specific to my region of the country (regionally specific) (total sample sizes for aggregate = 362, fall = 212, spring = 150) | 300 (82.9) | 171 (80.7) | 129 (86.0) |
| Include a minimum of 4 levels of modification, including the modification of practice time based on environmental conditions (total sample sizes for aggregate = 364, fall = 215, spring = 149) | 284 (78.0) | 171 (79.5) | 113 (75.8) |
| Include modification of work: rest ratios based on environmental conditions (total sample sizes for aggregate = 365, fall = 215, spring = 150) | 283 (77.5) | 168 (78.1) | 115 (76.7) |
| Include modification of protective equipment (if applicable to sport) (total sample sizes for aggregate = 364, fall = 214, spring = 150) | 312 (85.7) | 181 (84.6) | 131 (87.3) |
| Mention the use of shaded areas for rest breaks (total sample sizes for aggregate = 363, fall = 213, spring = 150) | 280 (77.1) | 155 (72.8) | 125 (83.3) |
| Q: My School’s Policies and Procedures… | Unaware Needed | Unaware If Have | Decided Not to Act | Unengaged | Undecided | Decided to Act | Acting | Maintaining |
|---|---|---|---|---|---|---|---|---|
| Include exertional heat illness (prevention and treatment) (n = 515) | 14 (2.6) | 26 (4.9) | 8 (1.5) | 34 (6.4) | 42 (7.9) | 37 (7) | 39 (7.4) | 329 (62.2) |
| Are based on environmental conditions measured by an on-site wet-bulb globe thermometer (n = 351) | 13 (3.6) | 25 (6.9) | 36 (9.9) | 30 (8.2) | 36 (9.9) | 16 (4.4) | 32 (8.8) | 176 (48.4) |
| Are based on environmental conditions that are specific to my region of the country (regionally specific) (n = 351) | 11 (3) | 13 (3.6) | 7 (1.9) | 7 (1.9) | 14 (3.9) | 10 (2.8) | 34 (9.4) | 266 (73.5) |
| Include a minimum of four levels of modification, including the modification of practice time based on environmental conditions (n = 352) | 12 (3.3) | 19 (5.2) | 9 (2.5) | 9 (2.5) | 9 (2.5) | 22 (6) | 30 (8.2) | 254 (69.8) |
| Include modification of work: rest ratios based on environmental conditions (n = 347) | 18 (4.9) | 20 (5.5) | 9 (2.5) | 9 (2.5) | 12 (3.3) | 14 (3.8) | 33 (9) | 250 (68.5) |
| Include modification of protective equipment (if applicable to sport) (n = 354) | 10 (2.7) | 8 (2.2) | 8 (2.2) | 6 (1.6) | 8 (2.2) | 12 (3.3) | 30 (8.2) | 282 (77.5) |
| Mention the use of shaded areas for rest breaks (n = 350) | 13 (3.6) | 15 (4.1) | 12 (3.3) | 20 (5.5) | 11 (3) | 12 (3.3) | 26 (7.2) | 254 (70) |
| Facilitators | |
| Support from someone in an authoritative position (e.g., school leader, coach, nurse, etc.) | 298 (56) |
| Having medical professional(s) (e.g., athletic trainer) at the school | 260 (48.9) |
| State mandate from the high school athletics association | 261 (49.1) |
| State legislation to mandate this policy | 261 (49.1) |
| Seeing how other schools/programs implement this policy | 200 (37.6) |
| Model policy that can be adopted | 190 (35.7) |
| School stakeholders believing sport safety is important and buying into these policies | 185 (34.8) |
| Nothing would make it easier | 31 (5.8) |
| Training | 17 (3.2) |
| Barriers | |
| No barriers encountered | 232 (43.6) |
| Resistance or apprehension from head coaches to modify practices | 179 (33.6) |
| My school’s AT is not full-time | 60 (11.3) |
| My school would need more information, assistance, etc. in order to implement all of the heat modification guidelines | 57 (10.7) |
| Resistance or apprehension from parents or legal guardians to modify practices | 37 (7) |
| It’s not hot enough where I live; we have difficulty seeing the need for this | 31 (5.8) |
| Liability | 29 (5.5) |
| My school does not have the time to educate the parents or legal guardians on the importance of this policy | 21 (3.9) |
| My school does not have the time to train the coaches and school personnel on how to implement this policy | 20 (3.8) |
| We don’t think this policy is as important as other topics | 14 (2.6) |
| We are located in a location that makes it difficult for EMS to get to us | 5 (0.9) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarneo-Miller, S.E.; Belval, L.N.; Yeargin, S.W.; Hosokawa, Y.; Kerr, Z.Y.; Casa, D.J. Exertional Heat Illness Preparedness Strategies: Environmental Monitoring Policies in United States High Schools. Medicina 2020, 56, 486. https://doi.org/10.3390/medicina56100486
Scarneo-Miller SE, Belval LN, Yeargin SW, Hosokawa Y, Kerr ZY, Casa DJ. Exertional Heat Illness Preparedness Strategies: Environmental Monitoring Policies in United States High Schools. Medicina. 2020; 56(10):486. https://doi.org/10.3390/medicina56100486
Chicago/Turabian StyleScarneo-Miller, Samantha E., Luke N. Belval, Susan W. Yeargin, Yuri Hosokawa, Zachary Y. Kerr, and Douglas J. Casa. 2020. "Exertional Heat Illness Preparedness Strategies: Environmental Monitoring Policies in United States High Schools" Medicina 56, no. 10: 486. https://doi.org/10.3390/medicina56100486
APA StyleScarneo-Miller, S. E., Belval, L. N., Yeargin, S. W., Hosokawa, Y., Kerr, Z. Y., & Casa, D. J. (2020). Exertional Heat Illness Preparedness Strategies: Environmental Monitoring Policies in United States High Schools. Medicina, 56(10), 486. https://doi.org/10.3390/medicina56100486






