A Rare Consequence after Shoulder Dislocation in a Professional Cyclist: A Case Report
Abstract
:1. Introduction
1.1. Anterior Shoulder Dislocation
1.2. Comorbidities Associated with Shoulder Dislocation
1.3. Bicycle Injury Costs
2. Case Presentation
2.1. Patient History
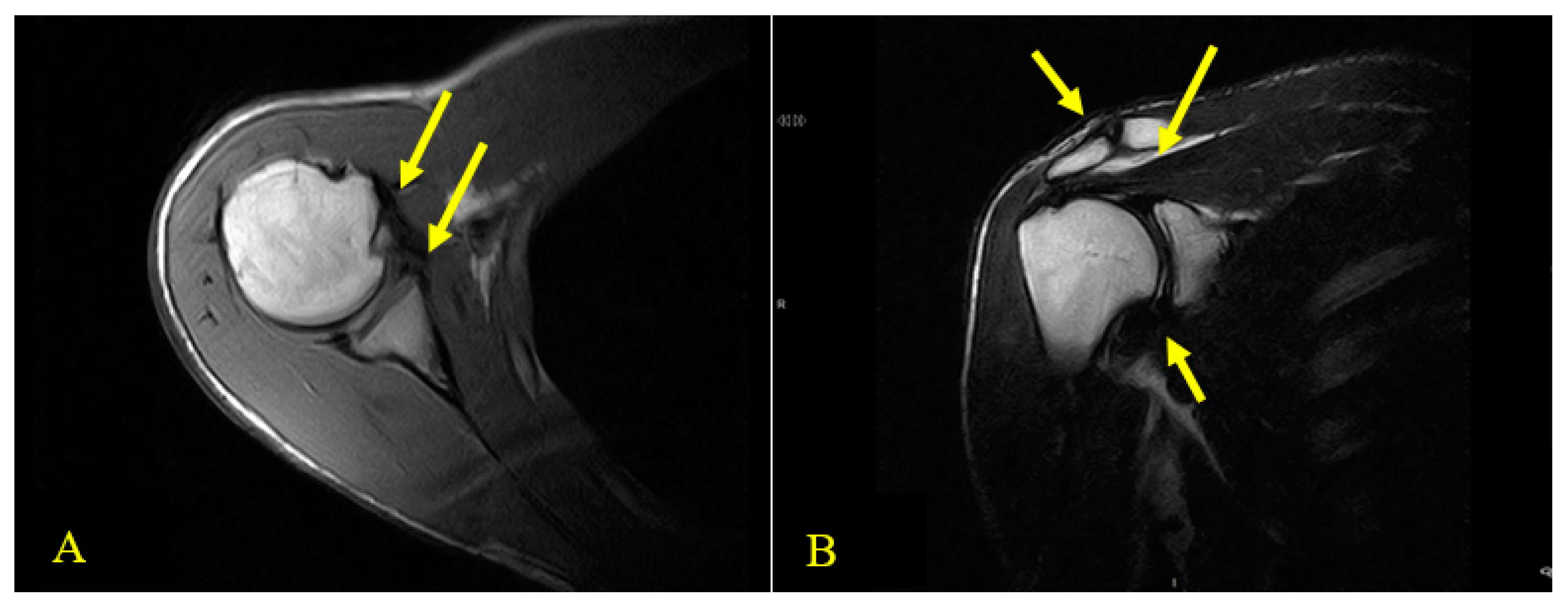
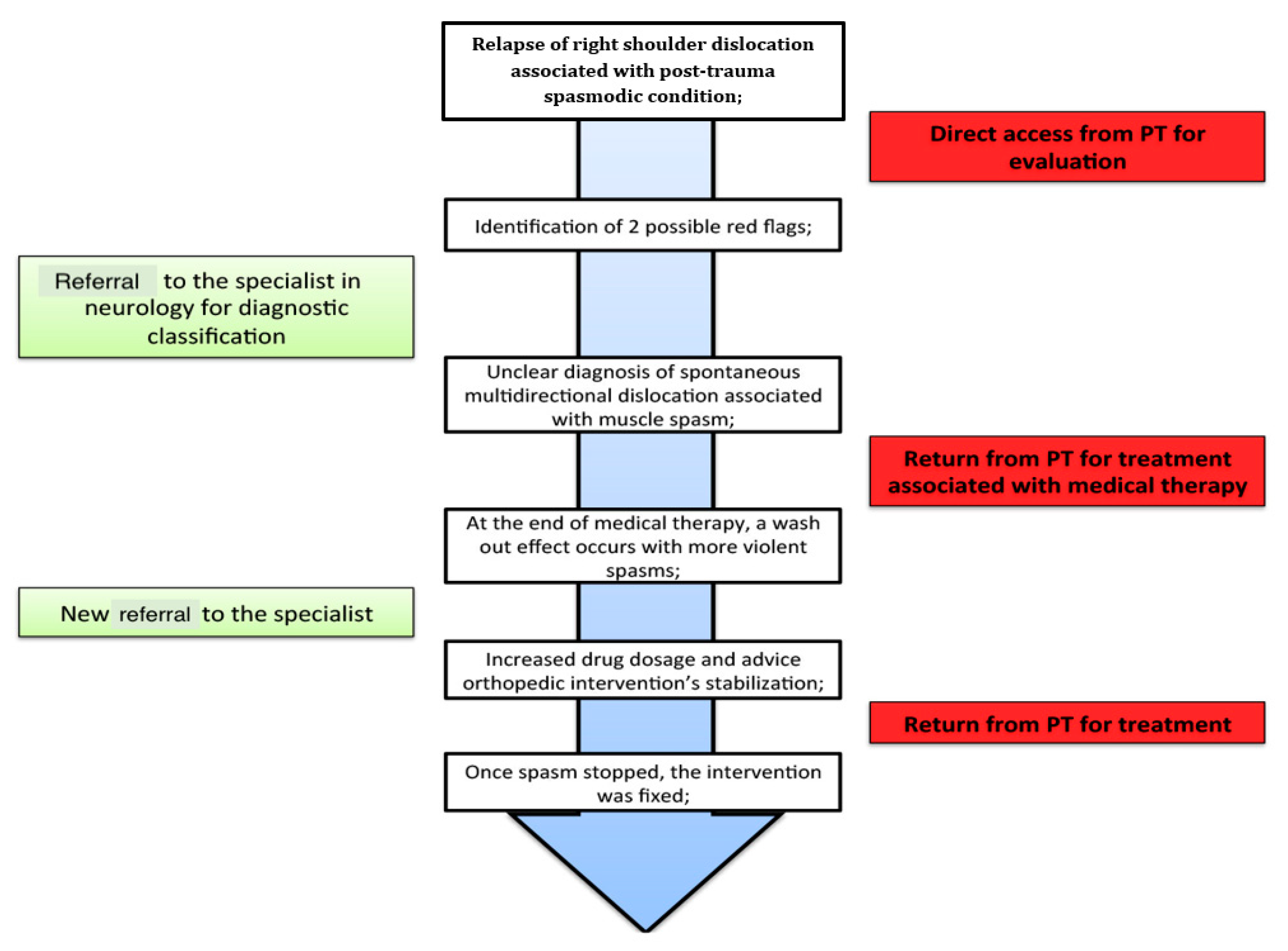
2.2. Physical Examination and the Physical Therapist’s Diagnosis
3. Intervention
3.1. Initial Physical Therapist’s Intervention
3.2. Neurology Referral
3.3. Rehabilitation Phase
3.4. Additional Presentation of Spasm
3.5. Second Medical Intervention
3.6. Surgery and Rehabilitation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Ethics Approval and Consent to Participate
Consent for Publication
Abbreviations
| US | United States |
| ACJ | Acromioclavicular joint |
| SC | Sternoclavicular |
| GHJ | Glenohumeral joint |
| PT | Physical therapist |
| MRI | Magnetic resonance image |
| NPRS | Numeric pain rating scale |
| DASH | Disability of the arm, shoulder, and hand |
| WOSI | Western Ontario shoulder instability |
| ADL | Activities of daily living |
| CT scan | Computed tomography scan |
| SAB | Subacromial bursa |
| ROM | Range of motion |
| STJ | Scapulothoracic joint |
| TCC | Thiocolchicoside |
References
- McAdams, R.J.; Swidarski, K.; Clark, R.M.; Roberts, K.J.; Yang, J.; Mckenzie, L.B. Bicycle-related injuries among children treated in US emergency departments. Accid. Anal. Prev. 2018, 118, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Ye, Y.; Lu, Y.; Li, L.; Gao, Y. An intervention to reduce bicycle injuries among middle school students in rural China. Int. J. Environ. Res. Public Health 2017, 14, 690. [Google Scholar] [CrossRef] [PubMed]
- Laurie, F.B.; Dellinger, A.M.; O’Neill, M.E. Motor vehicle crash injury rates by mode of travel, United States: Using exposure-based methods to quantify differences. Am. J. Epidemiol. 2007, 166, 212–218. [Google Scholar]
- Silberman, M. Bicycling injuries. Curr. Sports Med. Rep. 2013, 12, 337–345. [Google Scholar] [CrossRef] [PubMed]
- De Bernardo, N.; Barrios, C.; Vera, P.; Laiz, C.; Hadala, M. Incidence and risk for traumatic and overuse injuries in top-level road cyclists. J. Sports Sci. 2012, 30, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Greve, M.W.; Modabber, M.R. An epidemic of traumatic brain injury in professional cycling: A call to action. Clin. J. Sport Med. 2012, 22, 81–82. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, K. Cyclist injuries. Duodecim 2016, 132, 1352–1356. [Google Scholar]
- Macpherson, A.; Spinks, A. Bicycle helmet legislation for the uptake of helmet use and prevention of head injuries. Cochrane Database Syst. Rev. 2008, 3, CD005401. [Google Scholar] [CrossRef]
- Brophy, R.H.; Marx, R.G. The treatment of Traumatic Anterior Instability of the Shoulder: Nonoperative and Surgical Treatment. Arthroscopy 2009, 25, 298–304. [Google Scholar] [CrossRef]
- Kirkley, A.; Werstine, R.; Ratjek, A.; Griffin, S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: Long-term evaluation. Arthroscopy 2005, 21, 55–63. [Google Scholar] [CrossRef]
- Hayes, K.; Callanan, M.; Walton, J.; Paxinos, A.; Murrell, G.A. Shoulder Instability: Management and Rehabilitation. J. Orthop. Sports Phys. Ther. 2002, 32, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Kraeutler, M.J.; Currie, D.W.; Kerr, Z.Y.; Roos, K.G.; McCarty, E.C.; Comstock, R.D. Epidemiology of Shoulder Dislocation in High School and Collegiate Athletics in the United States; 2004/2005 through 2013/2014. Sports Health 2018, 10, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Robinson, C.M.; Shur, N.; Sharpe, T.; Ray, A.; Murray, I.R. Injuries associated with Traumatic Anterior Glenohumeral Dislocations. J. Bone Jt. Surg. 2012, 94, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Yip, K.M.; Hung, L.K.; Maffulli, N.; Chan, K.M. Brachial plexus injury in association with fracture-dislocation of the shoulder. Bulletin 1996, 55, 92–94. [Google Scholar]
- Marko, B.; Lesic, A.; Vidakovic, A.; Sudic, V. Nerve lesions after acute anterior dislocation of the humero-scapular joint—Electrodiagnostic study. Med. Pregl. 1993, 46, 191–193. [Google Scholar]
- Dahianna, S.L.; Dharma, B.S.; Shirley, C.; Sarah, D.; Rochelle, A.D. Using trauma center data to identify missed bicycle injuries and their associated costs. J. Trauma Acute Care Surg. 2012, 73, 1602–1606. [Google Scholar]
- Ryan, J.L.; Pracht, E.E.; Orban, B.L. Inpatient and emergency department costs from sports injuries among youth aged 5–18 years. BMJ Open Sport Exerc. Med. 2019, 5, e000491. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A.; Milan, S.; Kendzerska, T.; Frenc, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NPRS), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63, 240–252. [Google Scholar]
- Ladeira, C.E. Physical therapy clinical specialization and management of red and yellow flags in patients with low back pain in the United States. J. Man. Manip. Ther. 2018, 26, 66–77. [Google Scholar] [CrossRef]
- Kitis, A.; Celik, E.; Aslan, U.B.; Zercir, M. DASH questionnaire for the analysis of musculoskeletal symptoms in industry workers: A validity and reliability study. Appl. Ergon. 2009, 40, 251–255. [Google Scholar] [CrossRef]
- Cacchio, A.; Paoloni, M.; Sharon, H.G.; Rosa, F.; Properzi, G.; Padua, L.; Padua, R.; Carnelli, F.; Calvisi, V.; Santilli, V. Cross-cultural Adaptation and Measurement Properties of an Italian Version of the Western Ontario Shoulder Instability Index (WOSI). J. Orthop. Sports Phys. Ther. 2012, 42, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Gagnier, J.J.; Kienle, G.; Altman, D.G.; Moher, D.; Sox, H.; Riley, D.; The CARE Group. The CARE guidelines: Consensus-based clinical case reporting guideline development. J. Med. Case Rep. 2013, 7, 223. [Google Scholar] [CrossRef] [PubMed]
- Cools, A.M.; Borms, D.; Castelein, B.; Vanderstukken, F.; Johansson, F.R. Evidence-based rehabilitation of athletes with glenohumeral instability. Knee Surg. Sport Traumatol. Arthrosc. 2016, 24, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Warby, S.A.; Watson, L.; Ford, J.J.; Hahne, A.J.; Pizzari, T. Multidirectional instability of the glenohumeral joint: Etiology, classification, assessment, and management. J. Hand Ther. 2017, 30, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Carroll, L.T.; Hawley, J.S.; Ney, J.P. Post-traumatic shoulder dystonia in an active duty soldier. Mil. Med. 2006, 171, 494. [Google Scholar] [CrossRef] [PubMed]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceccarelli, C.; Brindisino, F.; Salomon, M.; Heick, J.D.; Maselli, F. A Rare Consequence after Shoulder Dislocation in a Professional Cyclist: A Case Report. Medicina 2019, 55, 529. https://doi.org/10.3390/medicina55090529
Ceccarelli C, Brindisino F, Salomon M, Heick JD, Maselli F. A Rare Consequence after Shoulder Dislocation in a Professional Cyclist: A Case Report. Medicina. 2019; 55(9):529. https://doi.org/10.3390/medicina55090529
Chicago/Turabian StyleCeccarelli, Claudio, Fabrizio Brindisino, Mattia Salomon, John Duane Heick, and Filippo Maselli. 2019. "A Rare Consequence after Shoulder Dislocation in a Professional Cyclist: A Case Report" Medicina 55, no. 9: 529. https://doi.org/10.3390/medicina55090529
APA StyleCeccarelli, C., Brindisino, F., Salomon, M., Heick, J. D., & Maselli, F. (2019). A Rare Consequence after Shoulder Dislocation in a Professional Cyclist: A Case Report. Medicina, 55(9), 529. https://doi.org/10.3390/medicina55090529







