Risk Factors for Emergency Department Unscheduled Return Visits
Abstract
1. Introduction
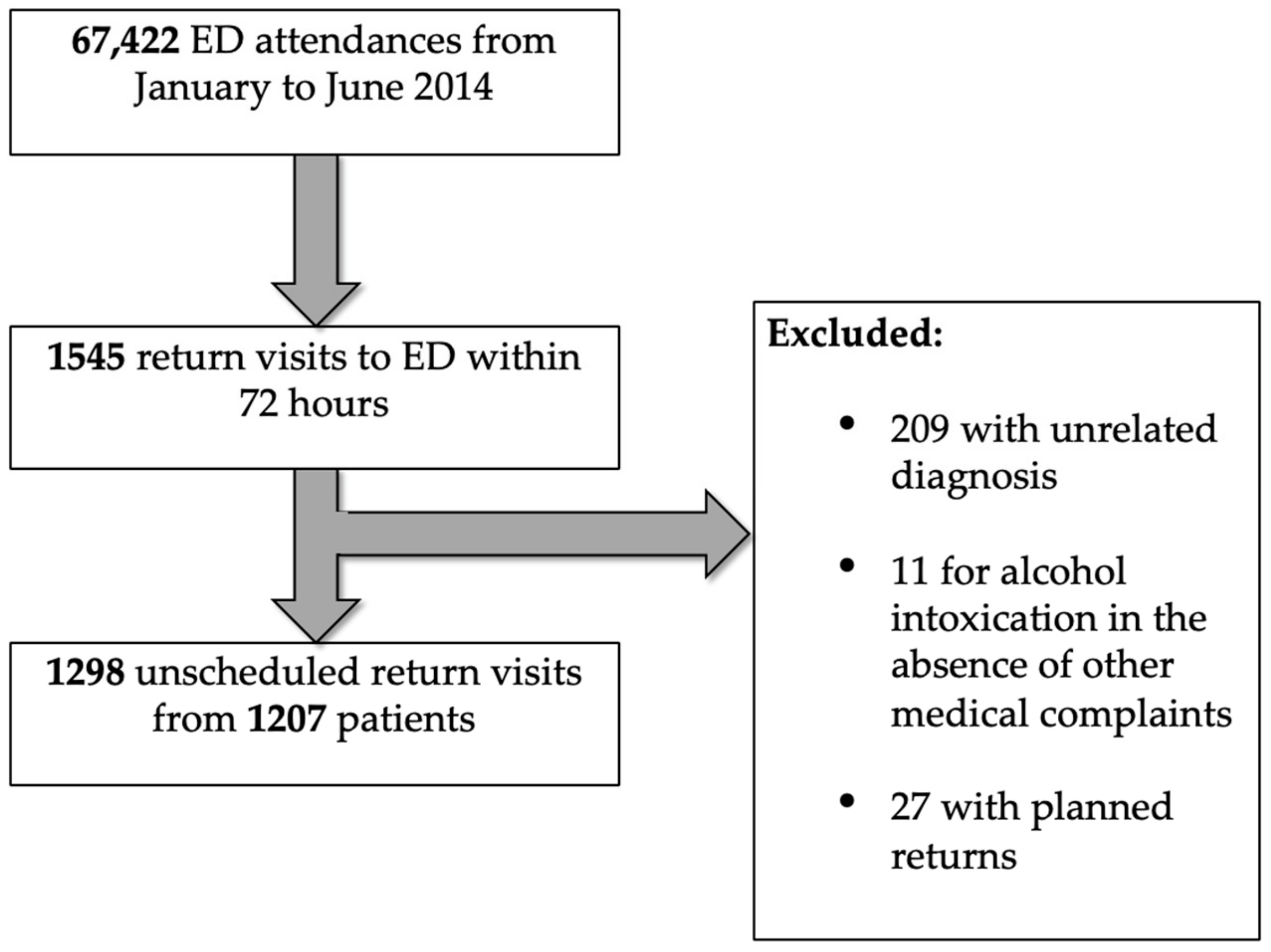
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Primary Outcome
3.3. Secondary Outcome
3.4. Comparison with Results in 2005 Study
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Hao, S.; Jin, B.O.; Shin, A.Y.; Zhao, Y.; Zhu, C.; Li, Z.; Hu, Z.; Fu, C.; Ji, J.; Wang, Y.; et al. Risk prediction of emergency department revisit 30 Days post discharge: A prospective study. PLoS ONE 2014, 9, e112944. [Google Scholar] [CrossRef] [PubMed]
- Trivedy, C.R.; Cooke, M.W. Unscheduled return visits (URV) in adults to the emergency department (ED): A rapid evidence assessment policy review. Emerg. Med. J. 2015, 32, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Schull, M.J.; Guttmann, A.; Leaver, C.A.; Vermeulen, M.; Hatcher, C.M.; Rowe, B.H.; Zwarenstein, M.; Anderson, G.M. Prioritizing performance measurement for emergency department care: Consensus on evidence-based quality of care indicators. Can. J. Emerg. Med. 2011, 13, 300–309. [Google Scholar] [CrossRef]
- Calder, L.; Pozgay, A.; Riff, S.; Rothwell, D.; Youngson, E.; Mojaverian, N.; Cwinn, A.; Forster, A. Adverse events in patients with return emergency department visits. BMJ Qual. Saf. 2015, 24, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Forster, A.J.; Rose, N.G.; van Walraven, C.; Stiell, I. Adverse events following an emergency department visit. Qual. Saf. 2007, 16, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Shroff, A.; Khan, N.; Jain, S. Emergency Department Return Visits Resulting in Admission: Do They Reflect Quality of Care? Am. J. Med. Qual. 2016, 31, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.W.; Lam, K.W. Reattendance audit in an inner-city emergency department. J. Accid. Emerg. Med. 1994, 11, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Baer, R.B.; Pasternack, J.S.; Zwemer, F.L. Recently discharged inpatients as a source of emergency department overcrowding. Acad. Emerg. Med. 2001, 8, 1091–1094. [Google Scholar] [CrossRef]
- Derlet, R.W.; Richards, J.R.; Kravitz, R.L. Frequent overcrowding in U.S. emergency departments. Acad. Emerg. Med. 2001, 8, 151–155. [Google Scholar] [CrossRef]
- Committee on Diagnostic Error in Health Care; Board on Health Care Services; Institute of Medicine; The National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care; Balogh, E.P., Miller, B.T., Ball, J.R., Eds.; Overview of Diagnostic Error in Health Care; National Academies Press: Washington, DC, USA, 29 December 2015. Available online: https://www.ncbi.nlm.nih.gov/books/NBK338594/ (accessed on 23 March 2017).
- Kuan, W.S.; Mahadevan, M. Emergency unscheduled returns: Can we do better? Singap. Med. J. 2009, 50, 1068–1071. [Google Scholar]
- Chan, A.H.S.; Ho, S.F.; Fook-Chong, S.M.C.; Lian, S.W.Q.; Liu, N.; Ong, M.E.H. Characteristics of patients who made a return visit within 72 h to the emergency department of a Singapore tertiary hospital. Singap. Med. J. 2016, 57, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Pham, J.C.; Kirsch, T.D.; Hill, P.M.; DeRuggerio, K.; Hoffmann, B. Seventy-two-hour returns may not be a good indicator of safety in the emergency department: A national study. Acad. Emerg. Med. 2011, 18, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, S.; Nicholl, J.; Dixon, S.; Cross, E.; Angelini, K.; Arnold, J.; Revill, S.; Locker, T.; Capewell, S.J.; Quinney, D.; et al. Randomised controlled trial and economic evaluation of a chest pain observation unit compared with routine care. BMJ 2004, 328, 254. [Google Scholar] [CrossRef]
- American College of Emergency Physicians. ACEP emergency ultrasound guidelines-2001. Ann. Emerg. Med. 2001, 38, 470–481. [Google Scholar] [CrossRef]
- Summers, S.M.; Scruggs, W.; Menchine, M.D.; Lahham, S.; Anderson, C.; Amr, O.; Lotfipour, S.; Cusick, S.S.; Fox, J.C. A prospective evaluation of emergency department bedside ultrasonography for the detection of acute cholecystitis. Ann. Emerg. Med. 2010, 56, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Duong, V.T.; Lin, I.F.; Sorensen, K.; Pelikan, J.M.; Van Den Broucke, S.; Lin, Y.C.; Chang, P.W. Health Literacy in Taiwan: A Population-Based Study. Asia Pac. J. Public Health 2015, 27, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.K.; Fisher, J.; Joyce, N.R.; Edlow, J.A. A prospective evaluation of indications for neurological consultation in the emergency department. Int. J. Emerg. Med. 2015, 8, 74. [Google Scholar] [CrossRef][Green Version]
- Wong, F.K.Y.; Chow, S.; Chang, K.; Lee, A.; Liu, J. Effects fects of nurse follow-up on emergency room revisits: A randomized controlled trial. Soc. Sci. Med. 2004, 59, 2207–2218. [Google Scholar] [CrossRef]
- Bhattacharyya, N.; Gubbels, S.P.; Schwartz, S.R.; Edlow, J.A.; El-Kashlan, H.; Fife, T.; Holmberg, J.M.; Mahoney, K.; Hollingsworth, D.B.; Roberts, R.; et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update) Executive Summary. Otolaryngol. Head Neck Surg. 2017, 156, 403–416. [Google Scholar] [CrossRef]
- Long, B.; Koyfman, A.; Lee, C.M. Emergency medicine evaluation and management of the end stage renal disease patient. Am. J. Emerg. Med. 2017, 35, 1946–1955. [Google Scholar] [CrossRef]
- Nuñez, S.; Hexdall, A.; Aguirre-Jaime, A. Unscheduled returns to the emergency department: an outcome of medical errors? Qual. Saf. Health Care 2006, 15, 102–108. [Google Scholar] [CrossRef] [PubMed]
- White, D.; Kaplan, L.; Eddy, L. Characteristics of patients who return to the emergency department within 72 h in one community hospital. Adv. Emerg. Nurs. J. 2011, 33, 344–353. [Google Scholar] [CrossRef] [PubMed]
| Variable | Re-Attendance within 72 h (N = 1207) | All ED Attendances (N = 67,422) |
|---|---|---|
| Age, median (IQR) | 34 (24–52) | 41 (26–60) |
| Age group, years | ||
| 16 to 20 | 64 (5.3) | 7066 (10.5) |
| 21 to 30 | 420 (34.8) | 16,246 (24.1) |
| 31 to 40 | 231 (19.1) | 10,636 (15.8) |
| 41 to 50 | 164 (13.6) | 8453 (12.5) |
| 51 to 60 | 134 (11.1) | 8882 (13.2) |
| 61 to 70 | 106 (8.8) | 6967 (10.3) |
| Above 70 | 88 (7.3) | 9172 (13.6) |
| Male sex | 721 (59.7) | 40,489 (60.1) |
| Race | ||
| Chinese | 655 (54.3) | 36,802 (54.6) |
| Malay | 212 (17.6) | 10,856 (16.1) |
| Indian | 188 (15.6) | 9517 (14.1) |
| Others | 152 (12.6) | 10,247 (15.2) |
| Activities of daily living status | ||
| Independent | 1197 (99.2) | |
| Assisted | 10 (0.8) | |
| Mobility | ||
| Independent | 1188 (98.4) | |
| Ambulant with assistance | 9 (0.7) | |
| Wheelchair | 9 (0.7) | |
| Bedbound | 1 (0.1) | |
| Presence of caregiver | 292 (24.2) | |
| Comorbidities | ||
| Diabetes mellitus (DM) | 120 (9.9) | |
| DM with end organ damage | 30 (2.5) | |
| Psychiatric history | 73 (6.0) | |
| Ischemic heart disease | 47 (3.9) | |
| Renal disease | 39 (3.2) | |
| Cancer | 33 (2.7) | |
| Cerebral vascular accident | 31 (2.6) | |
| Congestive heart failure | 17 (1.4) | |
| Peripheral vascular disease | 12 (1.0) | |
| Liver disease | 11 (0.9) | |
| Acquired immunodeficiency | 8 (0.6) | |
| Chronic obstructive pulmonary disease | 7 (0.6) | |
| Charlson comorbidity index | ||
| 0–3 | 1158 (95.9) | |
| 4–5 | 25 (2.1) | |
| 6–7 | 19 (1.6) | |
| 8 and above | 5 (0.4) | |
| Designation of primary doctor at index visit | ||
| Resident/Medical officer | 768 (63.6) | |
| Locum | 390 (32.3) | |
| Senior resident | 49 (4.1) | |
| Initial shift at presentation | ||
| Morning (08:00 to 15:59) | 487 (40.3) | 31,650 (46.9) |
| Afternoon (16:00 to 21:59) | 357 (29.6) | 19,775 (29.3) |
| Night (22:00 to 07:59) | 363 (30.1) | 15,997 (23.7) |
| Initial disposition | ||
| Discharged with follow-up | 612 (50.7) | |
| Discharged without follow-up | 442 (36.6) | |
| Discharged against advice | 74 (6.1) | |
| Admission to EDOU | 42 (3.5) | |
| Admission to ward | 37 (3.1) |
| Vital Sign | n (%) |
|---|---|
| Temperature ≥37.5 °C | 145 (12.0) |
| Systolic blood pressure, mmHg | |
| above 140 | 214 (17.7) |
| below 90 | 8 (0.7) |
| Heart rate, beats per minute | |
| above 100 | 181 (15.0) |
| below 60 | 12 (1.0) |
| Respiratory rate above 20 breaths per minute | 51 (4.2) |
| Oxygen saturation below 95% | 6 (0.5) |
| Pain score 5 or higher | 326 (27.0) |
| Presenting Complaint | n (%) * |
|---|---|
| Abdominal pain | 288 (22.2) |
| Fever | 273 (21.0) |
| Gastrointestinal | 256 (19.7) |
| Upper respiratory tract infection | 219 (16.9) |
| Musculoskeletal pain | 166 (12.8) |
| Trauma | 135 (10.4) |
| Headache | 111 (8.6) |
| Lower back pain and sciatica | 99 (7.6) |
| Chest pain | 88 (6.8) |
| Giddiness and vertigo | 83 (6.4) |
| Ophthalmological and Otolaryngological | 69 (5.3) |
| Shortness of breath (excluding asthma) | 67 (5.2) |
| Urological | 63 (4.9) |
| Dermatological | 62 (4.8) |
| Renal colic | 48 (3.7) |
| Obstetric and Gynecological | 48 (3.7) |
| Cellulitis and abscess | 37 (2.9) |
| Neurological deficit | 35 (2.7) |
| Psychiatric | 32 (2.5) |
| Asthma | 22 (1.7) |
| Others | 182 (14.0) |
| Factors | Wrong/Delayed Diagnosis, n (%) | Odds Ratios (OR) (95% CI) | p Value | |
|---|---|---|---|---|
| Yes (N = 191) | No (N = 1016) | |||
| Age group, years | ||||
| 21 to 30 | 53 (27.7) | 367 (36.1) | 0.68 (0.47 to 0.97) | 0.026 |
| 51 to 60 | 30 (15.7) | 104 (10.2) | 1.63 (1.01 to 2.57) | 0.027 |
| Initial disposition | ||||
| Discharged with follow-up | 80 (41.9) | 532 (52.4) | 0.66 (0.47 to 0.91) | 0.008 |
| Discharged without follow-up | 88 (46.1) | 354 (34.8) | 1.60 (1.15 to 2.21) | 0.003 |
| Presenting complaint | ||||
| Abdominal pain | 79 (41.4) | 194 (19.1) | 2.99 (2.12 to 4.20) | <0.001 |
| Trauma | 7 (3.7) | 124 (12.2) | 0.27 (0.11 to 0.59) | <0.001 |
| Fever | 54 (28.3) | 207 (20.4) | 1.54 (1.06 to 2.21) | 0.015 |
| Renal colic | 1 (0.5) | 41 (40.4) | 0.13 (0.003 to 0.75) | 0.015 |
| Nausea/Vomiting | 40 (20.9) | 149 (14.7) | 1.54 (1.02 to 2.30) | 0.029 |
| Neurological deficit | 11 (5.8) | 20 (2.0) | 3.04 (1.29 to 6.79) | 0.002 |
| Factor | Admission to EDOU or Ward, n (%) | OR (95% CI) | p Value | |
|---|---|---|---|---|
| Yes (N = 459) | No (N = 748) | |||
| Age group, years | ||||
| 16 to 20 | 9 (2.0) | 55 (7.4) | 0.25 (0.11 to 0.52) | <0.001 |
| 21 to 30 | 97 (21.1) | 323 (43.2) | 0.35 (0.27 to 0.46) | <0.001 |
| 41 to 50 | 79 (17.2) | 85 (11.4) | 1.62 (1.15 to 2.29) | 0.004 |
| 51 to 60 | 68 (14.8) | 66 (8.8) | 1.80 (1.23 to 2.62) | 0.001 |
| 61 to 70 | 60 (13.1) | 46 (6.1) | 2.29 (1.50 to 3.51) | <0.001 |
| Above 70 | 64 (13.9) | 24 (3.2) | 4.89 (2.96 to 8.30) | <0.001 |
| Male gender | 229 (49.9) | 257 (34.4) | 1.90 (1.49 to 2.43) | <0.001 |
| Presence of caregiver | 133 (29.0) | 159 (21.3) | 1.51 (1.15 to 1.99) | 0.002 |
| Initial disposition | ||||
| Admission to ward | 29 (6.3) | 8 (1.1) | 6.24 (2.75 to 15.91) | <0.001 |
| Admission to EDOU | 30 (6.5) | 12 (1.6) | 4.29 (2.10 to 9.29) | <0.001 |
| Discharged without follow-up | 120 (26.1) | 322 (43.0) | 0.47 (0.36 to 0.61) | <0.001 |
| Discharged against advice | 55 (12.0) | 19 (2.5) | 5.22 (3.00 to 9.44) | <0.001 |
| Comorbidities | ||||
| Diabetes mellitus (DM) | 79 (17.2) | 41 (5.5) | 3.58 (2.37 to 5.47) | <0.001 |
| DM with end-organ damage | 24 (5.2) | 6 (0.8) | 6.82 (2.69 to 20.54) | <0.001 |
| Liver Disease | 8 (1.7) | 3 (0.4) | 4.41 (1.05 to 25.88) | 0.017 |
| Congestive heart failure | 14 (3.1) | 3 (0.4) | 7.81 (2.16 to 42.56) | <0.001 |
| Ischemic heart disease | 35 (7.6) | 12 (1.6) | 5.06 (2.53 to 10.82) | <0.001 |
| Cerebral vascular accident | 24 (5.2) | 7 (9.4) | 5.84 (2.41 to 16.16) | <0.001 |
| Renal disease | 36 (7.8) | 3 (0.4) | 21.13 (6.61 to 107.68) | <0.001 |
| Cancer | 22 (4.8) | 11 (1.5) | 3.37 (1.55 to 7.77) | <0.001 |
| Acquired Immunodeficiency | 6 (1.3) | 1 (0.1) | 9.89 (1.19 to 455.62) | 0.009 |
| Charlson comorbidity index | ||||
| 0–3 | 416 (9.1) | 742 (99.2) | 0.08 (0.03 to 0.19) | <0.001 |
| 4–5 | 21 (4.6) | 4 (0.5) | 8.92 (2.98 to 35.90) | <0.001 |
| 6–7 | 17 (3.7) | 2 (0.3) | 14.35 (3.37 to 128.35) | <0.001 |
| Presenting complaint | ||||
| Abdominal pain | 130 (28.3) | 143 (19.1) | 1.67 (1.26 to 2.22) | <0.001 |
| Trauma | 27 (5.9) | 104 (13.9) | 0.39 (0.24 to 0.61) | <0.001 |
| Fever | 118 (25.7) | 143 (19.1) | 1.46 (1.10 to 1.95) | 0.007 |
| Upper respiratory tract infection | 56 (12.2) | 142 (19.0) | 0.59 (0.42 to 0.84) | 0.002 |
| Giddiness/Vertigo | 48 (10.5) | 31 (4.1) | 2.70 (1.65 to 4.46) | <0.001 |
| Cellulitis and Abscesses | 21 (4.6) | 16 (2.1) | 2.19 (1.08 to 4.54) | 0.017 |
| Chest Pain | 41 (8.9) | 41 (5.5) | 1.69 (1.05 to 2.72) | 0.021 |
| Obstetric and gynecological | 10 (2.2) | 34 (4.5) | 0.47 (0.20 to 0.98) | 0.033 |
| Ophthalmological | 8 (1.7) | 35 (4.7) | 0.36 (0.14 to 0.80) | 0.008 |
| Asthma | 14 (3.1) | 6 (0.8) | 3.89 (1.39 to 12.43) | 0.003 |
| Nausea or vomiting | 96 (20.9) | 93 (12.4) | 1.86 (1.35 to 2.58) | <0.001 |
| Shortness of breath (excluding asthma) | 42 (9.2) | 21 (2.8) | 3.49 (1.98 to 6.28) | <0.001 |
| Musculoskeletal pain | 48 (10.5) | 109 (14.6) | 0.68 (0.47 to 0.99) | 0.039 |
| Otolaryngological | 3 (0.7) | 18 (2.4) | 0.27(0.05 to 0.92) | 0.024 |
| Neurological deficits | 20 (4.4) | 11 (1.5) | 3.05 (1.38 to 7.12) | 0.002 |
| Initial vitals sign abnormal | 227 (49.5) | 237 (31.7) | 2.11 (1.65 to 2.70) | <0.001 |
| Initial primary doctor | ||||
| Resident/Medical officer | 255 (55.6) | 513 (68.6) | 0.57 (0.45 to 0.73) | <0.001 |
| Locum | 178 (38.8) | 212 (28.3) | 1.60 (1.24 to 2.06) | <0.001 |
| Senior resident | 26 (5.7) | 23 (3.1) | 1.89 (1.02 to 3.52) | 0.027 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soh, C.H.W.; Lin, Z.; Pan, D.S.T.; Ho, W.H.; Mahadevan, M.; Chua, M.T.; Kuan, W.S. Risk Factors for Emergency Department Unscheduled Return Visits. Medicina 2019, 55, 457. https://doi.org/10.3390/medicina55080457
Soh CHW, Lin Z, Pan DST, Ho WH, Mahadevan M, Chua MT, Kuan WS. Risk Factors for Emergency Department Unscheduled Return Visits. Medicina. 2019; 55(8):457. https://doi.org/10.3390/medicina55080457
Chicago/Turabian StyleSoh, Crystal Harn Wei, Ziwei Lin, Darius Shaw Teng Pan, Weng Hoe Ho, Malcolm Mahadevan, Mui Teng Chua, and Win Sen Kuan. 2019. "Risk Factors for Emergency Department Unscheduled Return Visits" Medicina 55, no. 8: 457. https://doi.org/10.3390/medicina55080457
APA StyleSoh, C. H. W., Lin, Z., Pan, D. S. T., Ho, W. H., Mahadevan, M., Chua, M. T., & Kuan, W. S. (2019). Risk Factors for Emergency Department Unscheduled Return Visits. Medicina, 55(8), 457. https://doi.org/10.3390/medicina55080457






