Relationships between Physical Activity, Sleeping Time, and Psychological Distress in Community-Dwelling Elderly Japanese
Abstract
1. Introduction
2. Materials and Methods
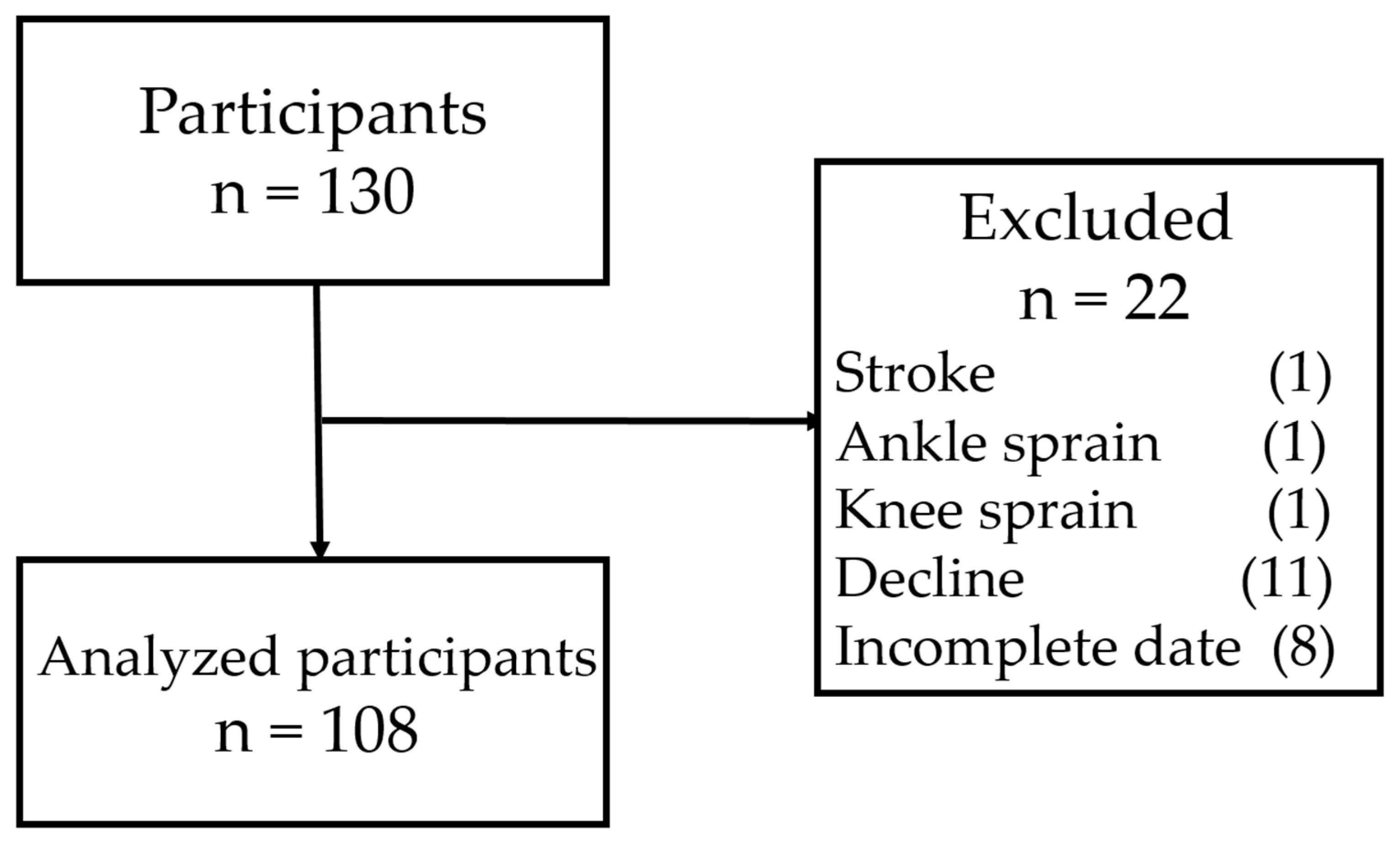
2.1. Participants
2.2. Clinical Parameters
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cabinet Office. Annual Report on the Ageing Society: 2018 (Summary). Available online: https://www8.cao.go.jp/kourei/english/annualreport/2018/pdf/c1-1.pdf (accessed on 2 April 2019).
- Wada, T.; Ishine, M.; Sakagami, T.; Okumiya, K.; Fujisawa, M.; Murakami, S.; Otsuka, K.; Yano, S.; Kita, T.; Matsubayashi, K.; et al. Depression in Japanese community-dwelling elderly-prevalence and association with ADL and QOL. Arch. Gerontol. Geriatr. 2004, 39, 15–23. Available online: https://www.ncbi.nlm.nih.gov/pubmed/15158577 (accessed on 5 June 2019). [CrossRef]
- Haseda, M.; Kondo, N.; Takagi, D.; Kondo, K. Community social capital and inequality in depressive symptoms among older Japanese adults: A multilevel study. Health Place 2018, 52, 8–17. Available online: https://www.ncbi.nlm.nih.gov/pubmed/29775833 (accessed on 5 June 2019). [CrossRef]
- Chang, Y.-C.; Lu, M.-C.; Hu, I.-H.; Wu, W.-C.I.; Hu, S.C. Effects of different amounts of exercise on preventing depressive symptoms in community-dwelling older adults: A prospective cohort study in Taiwan. BMJ Open 2017, 7, e014256. Available online: http://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2016-014256 (accessed on 2 April 2019). [CrossRef]
- Ishihara, T.; Tou, K.; Takizawa, K.; Mizuno, M. Effects of daily exercises on executive function and mental health in elderly individuals: Comparison between low intensity and moderate/vigorous intensity exercise. Jpn. J. Physiol. Anthropol. 2015, 20, 127–133. Available online: https://www.jstage.jst.go.jp/article/jjpa/20/3/20_KJ00010051702/_pdf (accessed on 2 April 2019). (In Japanese).
- Kanamori, S.; Takamiya, T.; Inoue, S.; Kai, Y.; Tsuji, T.; Kondo, K. Frequency and pattern of exercise and depression after two years in older Japanese adults: The JAGES longitudinal study. Sci. Rep. 2018, 8, 11224. Available online: http://www.nature.com/articles/s41598-018-29053-x (accessed on 2 April 2019). [CrossRef]
- Mc Dowell, C.P.; Carlin, A.; Capranica, L.; Dillon, C.; Harrington, J.M.; Lakerveld, J.; Loyen, A.; Ling, F.C.M.; Brug, J.; MacDonncha, C.; et al. Associations of self-reported physical activity and depression in 10,000 Irish adults across harmonised datasets: A DEDIPAC-study. BMC Public Health 2018, 18, 779. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-5702-4 (accessed on 2 April 2019). [CrossRef]
- Okoro, C.A.; Stoodt, G.; Rohrer, J.E.; Strine, T.W.; Li, C.; Balluz, L.S. Physical Activity Patterns among U.S. Adults with and without Serious Psychological Distress. Public Health Rep. 2014, 129, 30–38. Available online: http://journals.sagepub.com/doi/10.1177/003335491412900106 (accessed on 2 April 2019). [CrossRef]
- Takeda, F.; Noguchi, H.; Monma, T.; Tamiya, N. How Possibly Do Leisure and Social Activities Impact Mental Health of Middle-Aged Adults in Japan: An Evidence from a National Longitudinal Survey. PLoS ONE 2015, 10, e0139777. Available online: https://dx.plos.org/10.1371/journal.pone.0139777 (accessed on 2 April 2019). [CrossRef]
- Grønning, K.; Espnes, G.A.; Nguyen, C.; Rodrigues, A.M.F.; Gregorio, M.J.; Sousa, R.; Canhão, H.; André, B. Psychological distress in elderly people is associated with diet, wellbeing, health status, social support and physical functioning—A HUNT3 study. BMC Geriatr. 2018, 18, 891. Available online: https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-018-0891-3 (accessed on 2 April 2019). [CrossRef]
- Tolmunen, T.; Voutilainen, S.; Hintikka, J.; Rissanen, T.; Tanskanen, A.; Viinamäki, H.; Kaplan, G.A.; Salonen, J.T. Dietary Folate and Depressive Symptoms Are Associated in Middle-Aged Finnish Men. J. Nutr. 2003, 133, 3233–3236. Available online: https://academic.oup.com/jn/article/133/10/3233/4768420 (accessed on 2 April 2019). [CrossRef]
- Atkins, J.; Naismith, S.L.; Luscombe, G.M.; Hickie, I.B. Psychological distress and quality of life in older persons: Relative contributions of fixed and modifiable risk factors. BMC Psychiatry 2013, 13, 249. Available online: http://bmcpsychiatry.biomedcentral.com/articles/10.1186/1471-244X-13-249 (accessed on 2 April 2019). [CrossRef]
- Cunningham, T.J.; Wheaton, A.G.; Giles, W.H. The Association between Psychological Distress and Self-Reported Sleep Duration in a Population-Based Sample of Women and Men. Sleep Disord. 2015, 2015, 172064. Available online: http://www.hindawi.com/journals/sd/2015/172064/ (accessed on 2 April 2019). [CrossRef]
- Glozier, N.; Martiniuk, A.; Patton, G.; Ivers, R.; Li, Q.; Hickie, I.; Senserrick, T.; Woodward, M.; Norton, R.; Stevenson, M. Short sleep duration in prevalent and persistent psychological distress in young adults: The DRIVE study. Sleep 2010, 33, 1139–1145. Available online: https://www.ncbi.nlm.nih.gov/pubmed/20857859 (accessed on 2 April 2019). [CrossRef]
- Hori, D.; Tsujiguchi, H.; Kambayashi, Y.; Hamagishi, T.; Kitaoka, M.; Mitoma, J.; Asakura, H.; Suzuki, F.; Anyenda, E.O.; Nguyen, T.T.T.; et al. The associations between lifestyles and mental health using the General Health Questionnaire 12-items are different dependently on age and sex: A population-based cross-sectional study in Kanazawa, Japan. Environ. Health Prev. Med. 2016, 21, 410–421. Available online: http://link.springer.com/10.1007/s12199-016-0541-3 (accessed on 2 April 2019). [CrossRef]
- Kim, H.-M.; Lee, S.W. Beneficial Effects of Appropriate Sleep Duration on Depressive Symptoms and Perceived Stress Severity in a Healthy Population in Korea. Korean J. Fam. Med. 2018, 39, 57–61. Available online: http://kjfm.or.kr/journal/view.php?doi=10.4082/kjfm.2018.39.1.57 (accessed on 2 April 2019). [CrossRef]
- Seixas, A.A.; Vallon, J.; Barnes-Grant, A.; Butler, M.; Langford, A.T.; Grandner, M.A.; Schneeberger, A.R.; Huthchinson, J.; Zizi, F.; Jean-Louis, G.; et al. Mediating effects of body mass index, physical activity, and emotional distress on the relationship between short sleep and cardiovascular disease. Medicine 2018, 97, e11939. Available online: http://Insights.ovid.com/crossref?an=00005792-201809140-00004 (accessed on 2 April 2019). [CrossRef]
- Fujiwara, M.; Inagaki, M.; Nakaya, N.; Fujimori, M.; Higuchi, Y.; Kakeda, K.; Uchitomi, Y.; Yamada, N. Smoking among adults with serious psychological distress: Analysis of anonymized data from a national cross-sectional survey in Japan. J. Affect. Disord. 2018, 239, 131–137. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0165032718310589 (accessed on 2 April 2019). [CrossRef]
- Sung, H.-Y.; Prochaska, J.J.; Ong, M.K.; Shi, Y.; Max, W. Cigarette Smoking and Serious Psychological Distress: A Population-Based Study of California Adults. Nicotine Tob. Res. 2011, 13, 1183–1192. Available online: https://academic.oup.com/ntr/article-lookup/doi/10.1093/ntr/ntr148 (accessed on 2 April 2019). [CrossRef]
- Loscalzo, E.; Sterling, R.C.; Weinstein, S.P.; Salzman, B. Alcohol and other drug use in older adults: Results from a community needs assessment. Aging Clin. Exp. Res. 2017, 29, 1149–1155. Available online: http://link.springer.com/10.1007/s40520-016-0718-z (accessed on 2 April 2019). [CrossRef]
- Nakagawa, Y.; Mafune, K.; Inoue, A.; Hiro, H. Changes in drinking habits and psychological distress in Japanese non- or occasional drinking workers: A one-year prospective cohort study. Ind. Health 2017, 55, 243–251. Available online: https://www.jstage.jst.go.jp/article/indhealth/55/3/55_2016-0171/_article (accessed on 2 April 2019). [CrossRef]
- Ministry of Health, Labor and Welfare. National Health and Nutrition Survey. Available online: https://www.mhlw.go.jp/content/10904750/000351576.pdf (accessed on 1 June 2019). (In Japanese)
- Steele, B.G.; Holt, L.; Belza, B.; Ferris, S.; Lakshminaryan, S.; Buchner, D.M. Quantitating Physical Activity in COPD Using a Triaxial Accelerometer. Chest 2000, 117, 1359–1367. Available online: https://doi.org/10.1378/chest.117.5.1359 (accessed on 1 June 2019). [CrossRef]
- Shimizu, N.; Hashidate, H.; Ota, T.; Saito, A. The known-groups validity of intensity-based physical activity measurement using an accelerometer in people with subacute stroke. J. Phys. Ther. Sci. 2018, 30, 507–513. Available online: https://www.jstage.jst.go.jp/article/jpts/30/4/30_jpts-2017-616/_article (accessed on 1 June 2019). [CrossRef]
- Hamasaki, H.; Yanai, H.; Kakei, M.; Noda, M.; Ezaki, O. The validity of the non-exercise activity thermogenesis questionnaire evaluated by objectively measured daily physical activity by the triaxial accelerometer. BMC Sports Sci. Med. Rehabil. 2014, 6, 27. Available online: https://www.ncbi.nlm.nih.gov/pubmed/25075310 (accessed on 1 June 2019). [CrossRef]
- Shiga Federation of National Health Insurance Organization. Questionnaire on Specific Health Examination. Available online: http://www.shigakokuho.or.jp/cmsfiles/contents/0000000/60/englishi(H30kara).pdf (accessed on 2 April 2019).
- Ohkawara, K.; Oshima, Y.; Hikihara, Y.; Ishikawa-Takata, K.; Tabata, I.; Tanaka, S. Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. Br. J. Nutr. 2011, 105, 1681–1691. Available online: http://www.journals.cambridge.org/abstract_S0007114510005441 (accessed on 2 April 2019). [CrossRef]
- Oshima, Y.; Kawaguchi, K.; Tanaka, S.; Ohkawara, K.; Hikihara, Y.; Ishikawa-Takata, K.; Tabata, I. Classifying household and locomotive activities using a triaxial accelerometer. Gait Posture 2010, 31, 370–374. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0966636210000068 (accessed on 2 April 2019). [CrossRef]
- Owari, Y.; Miyatake, N.; Kataoka, H. Relationship between Social Participation, Physical Activity and Psychological Distress in Apparently Healthy Elderly People: A Pilot Study. Acta Med. Okayama 2018, 72, 31–37. Available online: https://www.ncbi.nlm.nih.gov/pubmed/29463936 (accessed on 2 April 2019).
- Harada, Y.; Oga, T.; Chin, K.; Takegami, M.; Takahashi, K.-I.; Sumi, K.; Nakamura, T.; Nakayama-Ashida, Y.; Minami, I.; Horita, S.; et al. Differences in relationships among sleep apnoea, glucose level, sleep duration and sleepiness between persons with and without type 2 diabetes: Obstructive sleep apnoea and diabetes. J. Sleep Res. 2012, 21, 410–418. Available online: http://doi.wiley.com/10.1111/j.1365-2869.2012.00997.x (accessed on 2 April 2019). [CrossRef]
- Asakura, R.; Miyatake, N.; Mochimasu, K.D.; Kurato, R.; Kuwana, S. Comparison of Psychological Distress between Type 2 Diabetes Patients with and without Proteinuria. Acta Med. Okayama 2017, 71, 309–314. Available online: https://www.ncbi.nlm.nih.gov/pubmed/28824186x (accessed on 2 April 2019).
- Furukawa, T.A.; Kawakami, N.; Saitoh, M.; Ono, Y.; Nakane, Y.; Nakamura, Y.; Tachimori, H.; Iwata, N.; Uda, H.; Nakane, H.; et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 2008, 17, 152–158. Available online: https://onlinelibrary.wiley.com/doi/pdf/10.1002/mpr.257 (accessed on 1 June 2019). [CrossRef]
- Iwata, N.; Uno, B.; Suzuki, T. Psychometric properties of the 30-item version general health questionnaire in Japanese. Jpn. J. Psychiatry Neurol. 1994, 48, 547–556. Available online: https://www.ncbi.nlm.nih.gov/pubmed/7891417 (accessed on 1 June 2019). [CrossRef]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.T.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. Available online: https://www.ncbi.nlm.nih.gov/pubmed/12214795 (accessed on 1 June 2019). [CrossRef]
- Furukawa, T.A.; Kessler, R.C.; Slade, T.; Andrews, G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol. Med. 2003, 33, 357–362. Available online: https://www.ncbi.nlm.nih.gov/pubmed/12622315 (accessed on 1 June 2019). [CrossRef]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E.; Howes, M.J.; Normand, S.-L.T.; Manderscheid, R.W.; Walters, E.E.; et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 2003, 60, 184–189. Available online: https://www.ncbi.nlm.nih.gov/pubmed/12578436 (accessed on 1 June 2019). [CrossRef]
- Parker, G.; Brotchie, H. Gender differences in depression. Int. Rev. Psychiatry 2010, 22, 429–436. [Google Scholar] [CrossRef]
- Brodaty, H.; Luscombe, G.; Parker, G.; Wilhelm, K.; Hickie, I.; Austin, M.-P.; Mitchell, P. Increased rate of psychosis and psychomotor change in depression with age. Psychol. Med. 1997, 27, 1205–1213. Available online: https://www.ncbi.nlm.nih.gov/pubmed/9300524 (accessed on 1 June 2019). [CrossRef]
- Robertson, R.; Robertson, A.; Jepson, R.; Maxwell, M. Walking for depression or depressive symptoms: A systematic review and meta-analysis. Ment. Health Phys. Act. 2012, 5, 66–75. Available online: https://www.sciencedirect.com/science/article/abs/pii/S1755296612000099 (accessed on 1 June 2019). [CrossRef]
- Teychenne, M.; Ball, K.; Salmon, J. Sedentary Behavior and Depression Among Adults: A Review. Int. J. Behav. Med. 2010, 17, 246–254. Available online: https://www.ncbi.nlm.nih.gov/pubmed/20174982 (accessed on 1 June 2019). [CrossRef]
- Zhai, L.; Zhang, H.; Zhang, D. SLEEP DURATION AND DEPRESSION AMONG ADULTS: A META-ANALYSIS OF PROSPECTIVE STUDIES: Research Article: Sleep Duration and Depression. Depress. Anxiety 2015, 32, 664–670. Available online: https://www.ncbi.nlm.nih.gov/pubmed/26047492 (accessed on 1 June 2019). [CrossRef]
- NHK Broadcasting Culture Research Institute. The 2015 NHK Japanese Time Use Survey. Available online: https://www.nhk.or.jp/bunken/english/reports/pdf/report_16071301.pdf (accessed on 2 April 2019).
- Justino Borges, L.; Bertoldo Benedetti, T.R.; Zarpellon Mazo, G. The influence of physical exercise on depressive symptoms and functional fitness in elderly residents of south Brazil. Rev. Esp. Geriatr. Gerontol. 2010, 45, 72–78. Available online: https://www.ncbi.nlm.nih.gov/pubmed/20206416 (accessed on 2 April 2019). [CrossRef]
- Blake, M.; Waloszek, J.M.; Schwartz, O.; Raniti, M.; Simmons, J.G.; Blake, L.; Murray, G.; Dahl, R.E.; Bootzin, R.; Dudgeon, P.; et al. The SENSE study: Post intervention effects of a randomized controlled trial of a cognitive-behavioral and mindfulness-based group sleep improvement intervention among at-risk adolescents. J. Consult. Clin. Psychol. 2016, 84, 1039–1051. Available online: https://www.ncbi.nlm.nih.gov/pubmed/27775416 (accessed on 2 April 2019). [CrossRef]
| Total (n = 108) | ||
|---|---|---|
| Age (years) | 74.0 | (65–88) |
| Height (cm) | 154.5 | (139–178) |
| Body weight (kg) | 54.5 | (36–89) |
| Body mass index (kg/m2) | 22.8 | ±2.9 |
| Exercise (Mets × h/w) | 4.6 | (0.32–13.4) |
| Number of Steps (steps/day) | 5456.6 | (525.9–20372.7) |
| Walking time (min/day) | 80.7 | (17.9–222.4) |
| ≦1.5 Mets (min/day) | 501.8 | ±124.0 |
| 1.6–2.9 Mets (min/day) | 285.0 | ±78.5 |
| ≧3 Mets (min/day) | 74.9 | (5.7–180.8) |
| ≦1.5 Mets (%/day) | 57.2 | ±10.7 |
| 1.6–2.9 Met (%/day) | 33.1 | ±8.4 |
| ≧3 Mets (%/day) | 9.0 | (0.61–23.28) |
| Total sleeping time (min/day) | 399.0 | ±70.3 |
| Time in bed (min/day) | 480.5 | (359–820) |
| K6 score | 1.0 | (0–18) |
| Psychological distress, n (%) | 18 (16.7) | |
| Medication | ||
| Hypertension, n (%) | 44 (40.7) | |
| Diabetes Mellitus, n (%) | 7 (6.5) | |
| Dyslipidemia, n (%) | 29 (26.9) | |
| Medical history | ||
| Stroke, n (%) | 5 (4.6) | |
| Heart disease, n (%) | 12 (11.1) | |
| Chronic kidney disease, n (%) | 1 (0.9) | |
| Anemia, n (%) | 16 (14.8) | |
| Smoking habits, n (%) | 2 (1.9) | |
| Exercise habits, n (%) | 48 (44.4) | |
| Drinking habits, n (%) | 28 (25.9) | |
| rs | p | |
|---|---|---|
| Sex | 0.075 | 0.462 |
| Age (years) | 0.041 | 0.671 |
| Body mass index (kg/m2) | –0.018 | 0.854 |
| Exercise (Mets/h/w) | –0.021 | 0.826 |
| Number of Steps (steps/day) | –0.084 | 0.387 |
| Walking time (min/day) | –0.095 | 0.326 |
| ≦1.5 Mets (min/day) | –0.042 | 0.667 |
| ≧3 Mets (min/day) | –0.016 | 0.867 |
| ≦1.5 Mets (%/day) | –0.019 | 0.847 |
| 1.6–2.9 Mets (%/day) | 0.054 | 0.579 |
| ≧3 Mets (%/day) | 0.006 | 0.952 |
| Total sleeping time (min/day) | –0.224 | 0.020 |
| Time in bed (min/day) | –0.078 | 0.424 |
| Objective Variable | Explanatory Variables | b | 95% Cl | Standardized β | p | VIF | ||
|---|---|---|---|---|---|---|---|---|
| Psychological distress | Constant | 16.214 | 3.053 | to | 29.376 | |||
| Sex | −0.055 | −1.513 | to | 1.734 | 0.013 | 0.893 | 1.125 | |
| Age (years) | −0.064 | −0.211 | to | 0.074 | −0.095 | 0.341 | 1.126 | |
| Walking time (min/day) | −0.026 | −0.048 | to | −0.004 | −0.276 | 0.019 | 1.548 | |
| ≦1.5 Mets (%/day) | −2.373 | −10.278 | to | 5.533 | −0.068 | 0.553 | 1.482 | |
| Total sleeping time (min/day) | −0.012 | −0.022 | to | −0.002 | −0.231 | 0.016 | 1.024 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, Y.; Suzuki, H.; Owari, Y.; Miyatake, N. Relationships between Physical Activity, Sleeping Time, and Psychological Distress in Community-Dwelling Elderly Japanese. Medicina 2019, 55, 318. https://doi.org/10.3390/medicina55070318
Yamamoto Y, Suzuki H, Owari Y, Miyatake N. Relationships between Physical Activity, Sleeping Time, and Psychological Distress in Community-Dwelling Elderly Japanese. Medicina. 2019; 55(7):318. https://doi.org/10.3390/medicina55070318
Chicago/Turabian StyleYamamoto, Yukio, Hiromi Suzuki, Yutaka Owari, and Nobuyuki Miyatake. 2019. "Relationships between Physical Activity, Sleeping Time, and Psychological Distress in Community-Dwelling Elderly Japanese" Medicina 55, no. 7: 318. https://doi.org/10.3390/medicina55070318
APA StyleYamamoto, Y., Suzuki, H., Owari, Y., & Miyatake, N. (2019). Relationships between Physical Activity, Sleeping Time, and Psychological Distress in Community-Dwelling Elderly Japanese. Medicina, 55(7), 318. https://doi.org/10.3390/medicina55070318





