1. Introduction
Abdominoplasty is one of the most commonly performed cosmetic procedures [
1,
2]. The excess skin in the conventional abdominoplasty is transversely excised leading to a single horizontal closure scar. In some cases, the tension following horizontal closure can be high which can result in a hypertrophic and superiorly displaced scar. “Fleur de lis” abdominoplasty with a vertical scar was defined by Dellon [
3], especially for post-bariatric patients with vertical skin excess. Despite the usefulness of the technique, it was not very popular among surgeons because of the fear that it might cause high complication rates. [
4]. However, several studies have shown similar complication rates with “Fleur-de-lis” when compared to conventional abdominoplasty with better results in selected patients with vertical skin excess [
4].
The mini inverse t-scar abdominoplasty has a similar approach to the “Fleur-de-lis” technique and involves the use of a small vertical incision in comparison to the long vertical incision which is usually defined to up to the level of the xiphoid process [
5]. This technique aims to lower the position of the final abdominal scar instead of addressing the horizontal laxity. This method can be useful in selected patients with a risk of superior displacement of the scar. This technique can also be utilized in transverse rectus abdominis flap (TRAM) and deep inferior epigastric flap (DIEP) patients to place the scar at a lower level while eliminating the need for a small or superiorly placed flap. Since the skin tension following the closure is also distributed among the horizontal axis we have predicted that the inverse t-scar technique could result in better scar healing.
In this study, we compare the width and height of the scar and the aesthetic satisfaction of patients and surgeons between conventional abdominoplasty and mini inverted t-scar abdominoplasty.
2. Materials and Methods
Thirty patients undergoing abdominoplasty and breast reconstruction with transverse rectus abdominis flap (TRAM) or deep inferior epigastric flap (DIEP) were included in the study. Informed patient consents were obtained prior to surgery. Patients with previous abdominal surgery, systemic diseases, or a body mass index lower than 18 kg/m2 or higher than 30 kg/m2 were excluded from the study.
Mean patient age was 37 (range: 26–49). In 15 patients abdominal closure with conventional transverse scar was performed. In the remaining 15 patients closure with an inverse t-scar was performed. Mean body mass index (BMI) was 24.3 (range: 20–30) (
Table 1).
Operation Technique
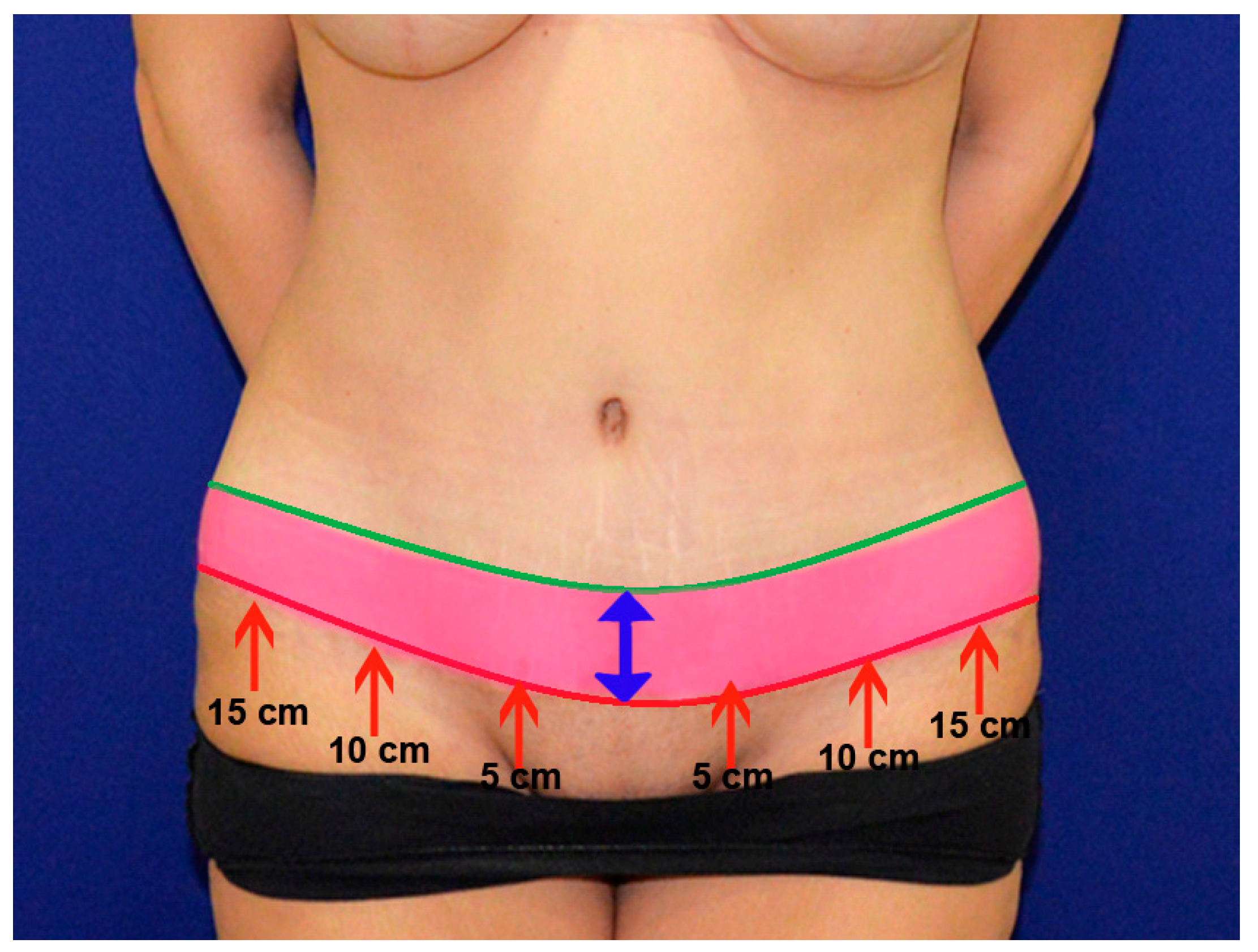
A low transverse skin incision was made 6–7 cm from the anterior vulvar commissure in the conventional transverse scar group and 8–10 cm from the anterior vulvar commissure in the mini inverted t-scar group. Anterior superior iliac spine was used as a landmark on the lateral edges. The skin flap was dissected while leaving a small amount of loose adipose tissue over the fascia up to the xiphoid process. Umbilicus was separated from the flap with its stalk. The patient was positioned in 30 degrees of flexion, and excess skin was marked and excised. Skin closure in the inverse t-scar group was performed with the addition of a 3–5 cm midline vertical scar to the horizontal scar. Incisions were closed in two layers in both groups. The deeper layer was closed with 2–0 absorbable monofilament sutures and skin layer was closed with 3–0 absorbable monofilament sutures in a subcuticular fashion. Liposuction was performed on all abdominoplasty patients on the flank and anterior abdominal regions. Liposuction was not performed on DIEP/TRAM patients (
Figure 1 and
Figure 2) (
Table 2). None of the patients had major complications such as infection, hematoma, or seroma. Two patients from the conventional scar group and three patients from the inverse t-scar group encountered minor wound healing problems.
Patients were evaluated at postoperative one, three, and six months following surgery. Scars were measured at the postoperative 6-month follow up visit. Scar width was measured at 5, 10, and 15 cm from midline and abdominal incisions, and also at the middle of the vertical incision in inverse t-scar patients (
Figure 3). Satisfaction was evaluated by the patient and two independent plastic surgeons who were not involved in the study. The patients and surgeons were asked to rate their scar based on the pigmentation, vascularity, pliability, and height, partially based on the modified Vancouver scar scale [
6]. A rating system from 1 to 5 was used (1: worst, 5: best). The distance between the midpoint of the transverse incision scar and the line connecting the anterior superior iliac spines and symphysis pubis was measured to the determine the height of the final scar.
Statistical analysis was performed with Prism 7 software (Version 7.00 for Windows, GraphPad Software, La Jolla California USA). The data was not in normal distribution. A non-parametric Mann–Whitney test was used for comparison of the groups.
3. Results
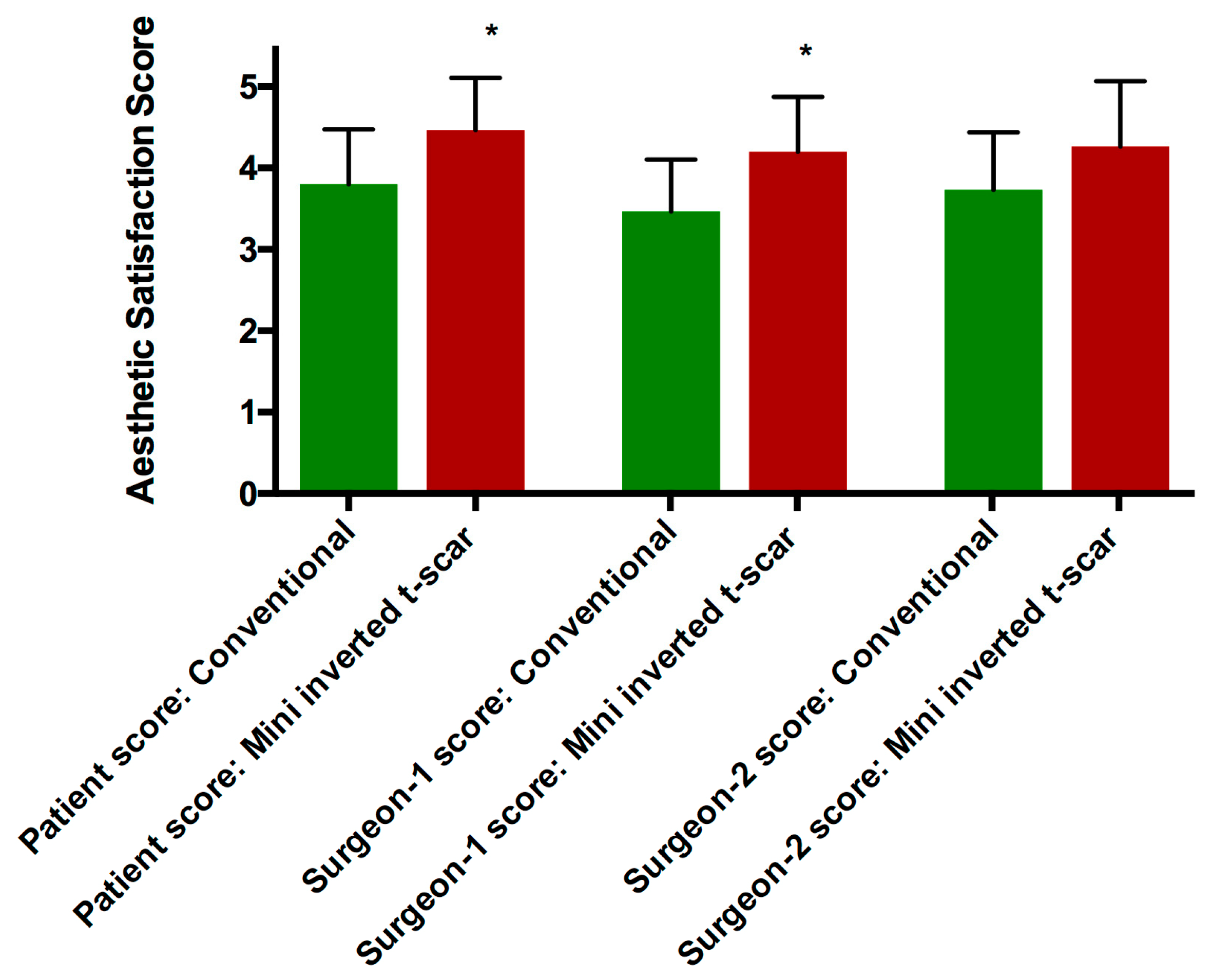
The mean of patient aesthetic satisfaction scores were 3.8 ± 0.6 and 4.46 ± 0.6 in the conventional transverse scar and mini inverted t-scar groups, respectively (
p = 0.0165). The mean of surgeon-1 aesthetic satisfaction scores were 3.46 ± 0.6 and 4.2 ± 0.6 in the conventional transverse scar and mini inverted t-scar groups, respectively (
p = 0.0081). The mean of surgeon-2 aesthetic satisfaction scores were 3.73 ± 0.7 and 4.26 ± 0.8 in the conventional transverse scar and mini inverted t-scar groups, respectively (
p = 0.1023) (
Figure 4,
Table 3).
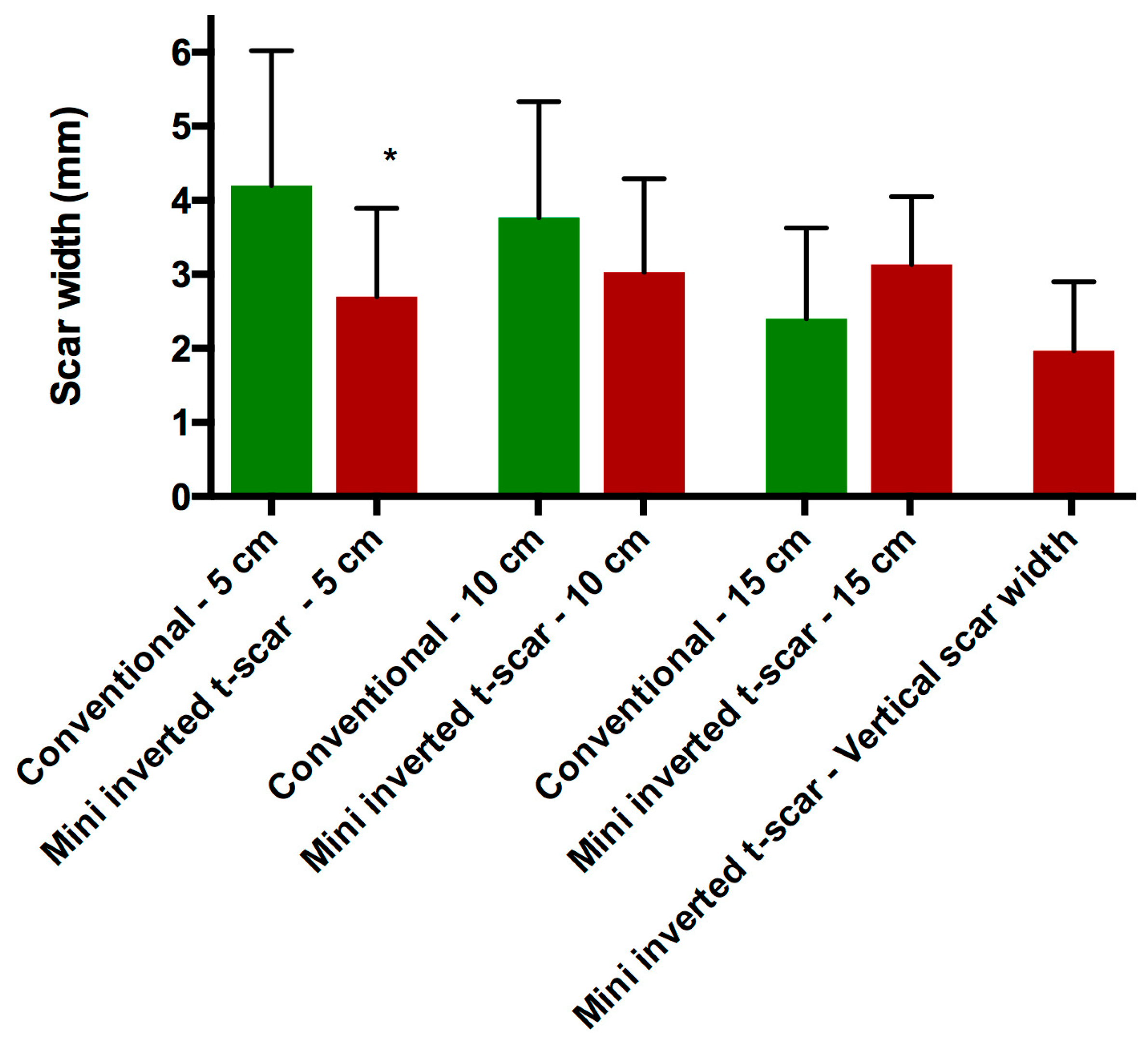
The mean width of the final scar five cm from the midline was 4.2 ± 1.8 mm and 2.7 ± 1.19 mm in the conventional transverse scar and the mini inverted t-scar groups, respectively (
p = 0.0244). The mean width of the final scar 10 cm from the midline was 3.76 ± 1.56 mm and 3.03 ± 1.26 mm in the conventional transverse scar and the mini inverted t-scar groups, respectively (
p = 0.2189). The mean width of the final scar 15 cm from the midline was 2.4 ± 1.22 mm and 3.13 ± 0.91 mm in the conventional transverse scar and the mini inverted t-scar groups, respectively (
p = 0.0553). The mean width of the vertical scar was 1.96 ± 0.93 mm in the mini inverted t-scar group (
Figure 5,
Table 3).
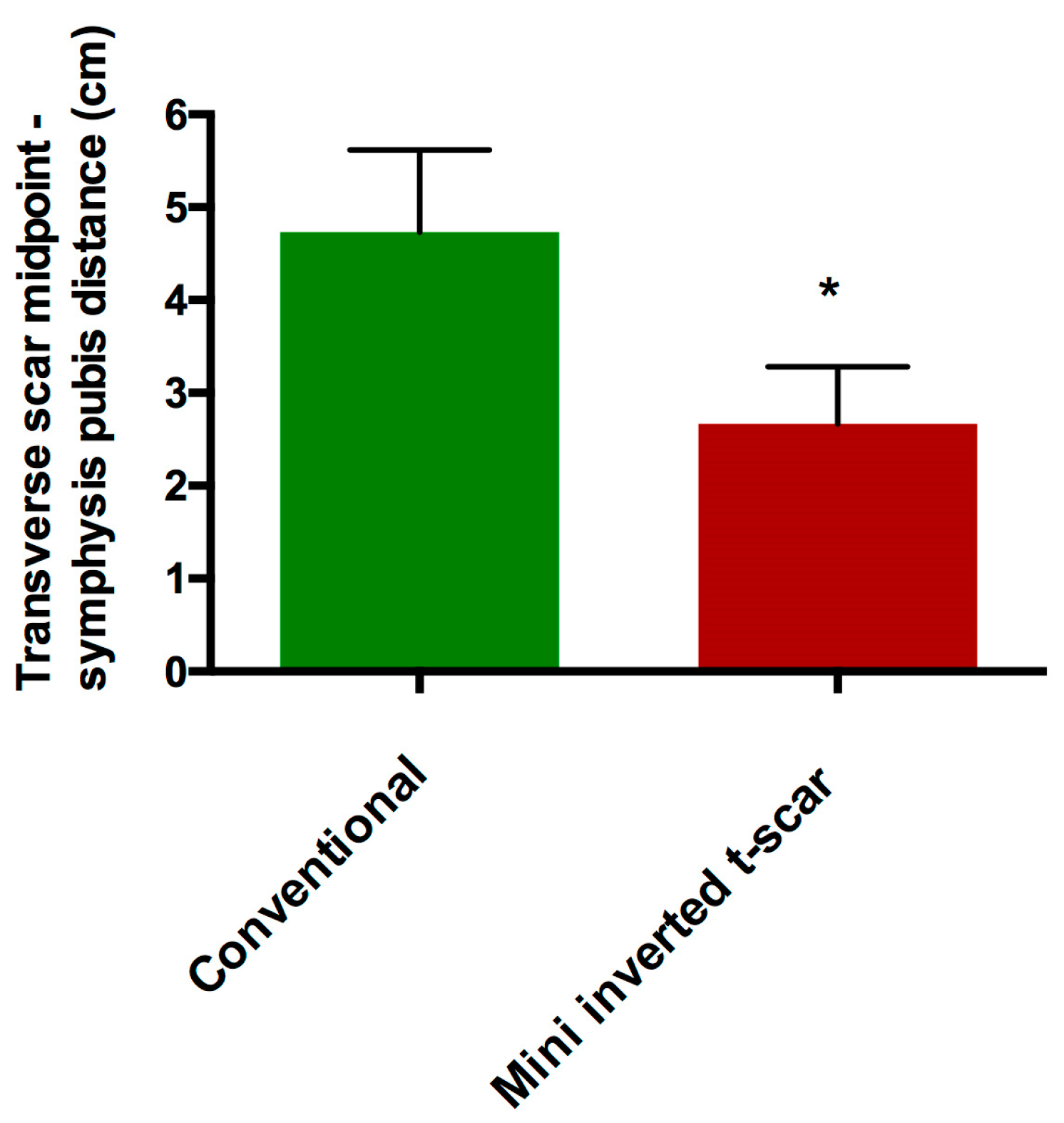
The mean distance from the midpoint of the transverse incision scar to the line connecting the anterior superior iliac spines and symphysis pubis was 4.73 ± 0.88 cm and 2.66 ± 0.61 cm in the conventional transverse scar and the mini inverted t-scar groups, respectively (
p < 0.0001) (
Figure 3,
Figure 4,
Figure 5 and
Figure 6,
Table 3).
4. Discussion
Scar visibility is an important concern in all cosmetic procedures. High tension closure should be avoided to prevent hypertrophic scars [
7,
8,
9]. An ideal scar following a cosmetic surgery should be concealed or should not be easily visible. This is especially true for abdominoplasty which results in a long horizontal scar. The scar should be placed as low as possible to decrease visibility.
Various devices or materials such as scar therapy devices [
10], intradermal injection therapies [
11], Dermabond [
12], and dermal staplers [
6] have been utilized to improve the scar quality in abdominoplasties. In order to hide the scar in the lower abdomen the incision is usually planned 6 to 7 cm above the anterior vulvar commissure [
13]. However, despite careful planning the incision scar can have a tendency to shift superiorly.
The final height of the abdominoplasty scar depends on the laxity of the mons pubis skin, and the amount of excess skin above the umbilicus. In our experience, in cases with high mons pubis skin laxity or low amount of excess skin, there is a greater risk for superior displacement of the scar. Since these components are highly variable for each patient, it is difficult make a clear definition or to predict the final position of the scar. The addition of the vertical component shifts the position of the transverse scar inferiorly and reduces the tension of the closure. The only disadvantage of this technique is the remaining vertical scar. The length of the vertical scar depends on the amount of skin. In our study, this length was between 3 to 5 cm.
A ‘T’ incision could be used for massive weight loss patient where the skin laxity is present in both the vertical and horizontal dimensions. The ‘T’ incision can also be used in thin patients to address the excess skin. It can also be used to close the original umbilical skin opening that has been pulled down lower.
T-scar closure is not commonly used in abdominoplasty. This is probably due to the concern regarding the visibility of a vertical scar. Due to this concern, inverse t-scar is rarely used in abdominoplasty except in postbariatric patients [
3,
4,
14,
15,
16,
17]. In this study, we have compared the scar quality of conventional horizontal scar abdominoplasties with t-scar abdominoplasties. We have seen that with the conventional horizontal scar technique, the final scar displayed a tendency to displace superiorly despite initial planning. This resulted in a decrease in the distance between the scar and the umbilicus. The mini inverted t-scar technique can reduce the skin tension during the closure and can help position the transverse scar in a lower position on the abdomen.
5. Conclusions
In our study, the vertical component of the scar healed very well. This is most probably due to the low amount of tension during the closure. The patients did not complain about the appearance of the vertical scars and did not feel the need to use high waist swimwear following the surgery. In conclusion, the visibility of the vertical scar alone should not be a reason to avoid mini reverse t-scar abdominoplasty. Inverse t-incision can be an option to achieve a less visible scar with an improved aesthetic satisfaction.
Author Contributions
Data curation, S.K.Y.; Methodology, S.K.Y.; Project administration, S.K.Y.; Writing–original draft, M.S.; Writing–review & editing, M.S.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Richardson, C.; Mattison, G.; Workman, A.; Gupta, S. Pricing of common cosmetic surgery procedures: local economic factors trump supply and demand. Aesthet. Surg. J. 2015, 35, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Heidekrueger, P.I.; Juran, S.; Patel, A.; Tanna, N.; Broer, P.N. Plastic Surgery Statistics in the US: Evidence and Implications. Aesthet. Plast. Surg. 2016, 40, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Dellon, A.L. Fleur-de-lis abdominoplasty. Aesthet. Plast. Surg. 1985, 9, 27–32. [Google Scholar] [CrossRef]
- Mendes, F.H.; Donnabella, A.; Fagotti Moreira, A.R. Fleur-de-lis Abdominoplasty and Neo-umbilicus. Clin. Plast. Surg. 2019, 46, 49–60. [Google Scholar] [CrossRef] [PubMed]
- Dardour, J.C.; Vilain, R. Alternatives to the classic abdominoplasty. Ann. Plast. Surg. 1986, 17, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Bron, T.; Zakine, G. Placement of Absorbable Dermal Staples in Mammaplasty and Abdominoplasty: A 12-Month Prospective Study of 60 Patients. Aesthet. Surg. J. 2016, 36, 459–468. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.W.; Beasley, B.; Zepeda, J.; Dauskardt, R.H.; Yock, P.G.; Longaker, M.T.; Gurtner, G.C. A Mechanomodulatory Device to Minimize Incisional Scar Formation. Adv. Wound Care (New Rochelle) 2013, 2, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Trussler, A.P.; Kurkjian, T.J.; Hatef, D.A.; Farkas, J.P.; Rohrich, R.J. Refinements in abdominoplasty: a critical outcomes analysis over a 20-year period. Plast. Reconstr. Surg. 2010, 126, 1063–1074. [Google Scholar] [CrossRef] [PubMed]
- Le Louarn, C.; Pascal, J.F. The high-superior-tension technique: evolution of lipoabdominoplasty. Aesthet. Plast. Surg. 2010, 34, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Longaker, M.T.; Rohrich, R.J.; Greenberg, L.; Furnas, H.; Wald, R.; Bansal, V.; Seify, H.; Tran, A.; Weston, J.; Korman, J.M.; et al. A randomized controlled trial of the embrace advanced scar therapy device to reduce incisional scar formation. Plast. Reconstr. Surg. 2014, 134, 536–546. [Google Scholar] [CrossRef] [PubMed]
- Lanier, S.T.; Liu, J.; Chavez-Munoz, C.; Mustoe, T.A.; Galiano, R.D. The Northwestern Abdominoplasty Scar Model: A Novel Human Model for Scar Research and Therapeutics. Plast. Reconstr. Surg. Glob. Open 2016, 4, e867. [Google Scholar] [CrossRef] [PubMed]
- Koonce, S.L.; Eck, D.L.; Shaddix, K.K.; Perdikis, G. A prospective randomized controlled trial comparing N-butyl-2 cyanoacrylate (Histoacryl), octyl cyanoacrylate (Dermabond), and subcuticular suture for closure of surgical incisions. Ann. Plast. Surg. 2015, 74, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Villegas, F.J. A novel approach to abdominoplasty: TULUA modifications (transverse plication, no undermining, full liposuction, neoumbilicoplasty, and low transverse abdominal scar). Aesthet. Plast. Surg. 2014, 38, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.T.; Rubin, J.P. The Fleur-De-Lis abdominoplasty. Clin. Plast. Surg. 2014, 41, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, U.E.; Ziegler, S.N.; Zeplin, P.H. Modified Fleur-de-lis Abdominoplasty for Massive Weight Loss Patients. Ann. Plast. Surg. 2017, 79, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Eisenhardt, S.U.; Goerke, S.M.; Bannasch, H.; Stark, G.B.; Torio-Padron, N. Technical facilitation of the fleur-de-lis abdominoplasty for symmetrical resection patterns in massive weight loss patients. Plast. Reconstr. Surg. 2012, 129, 590e–593e. [Google Scholar] [CrossRef] [PubMed]
- Friedman, T.; O’Brien Coon, D.; Michaels, J.; Purnell, C.; Hur, S.; Harris, D.N.; Rubin, J.P. Fleur-de-Lis abdominoplasty: a safe alternative to traditional abdominoplasty for the massive weight loss patient. Plast. Reconstr. Surg. 2010, 125, 1525–1535. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).