Nutrition, BMI and Motor Competence in Children with Autism Spectrum Disorder
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instrument
The Movement Assessment Battery for Children-Second Edition (MABC-2)
2.3. The Nutrition Knowledge Survey
2.4. Body Mass Index
2.5. Procedures
2.6. Data Analysis
2.7. Ethical Approval
3. Results
4. Discussion
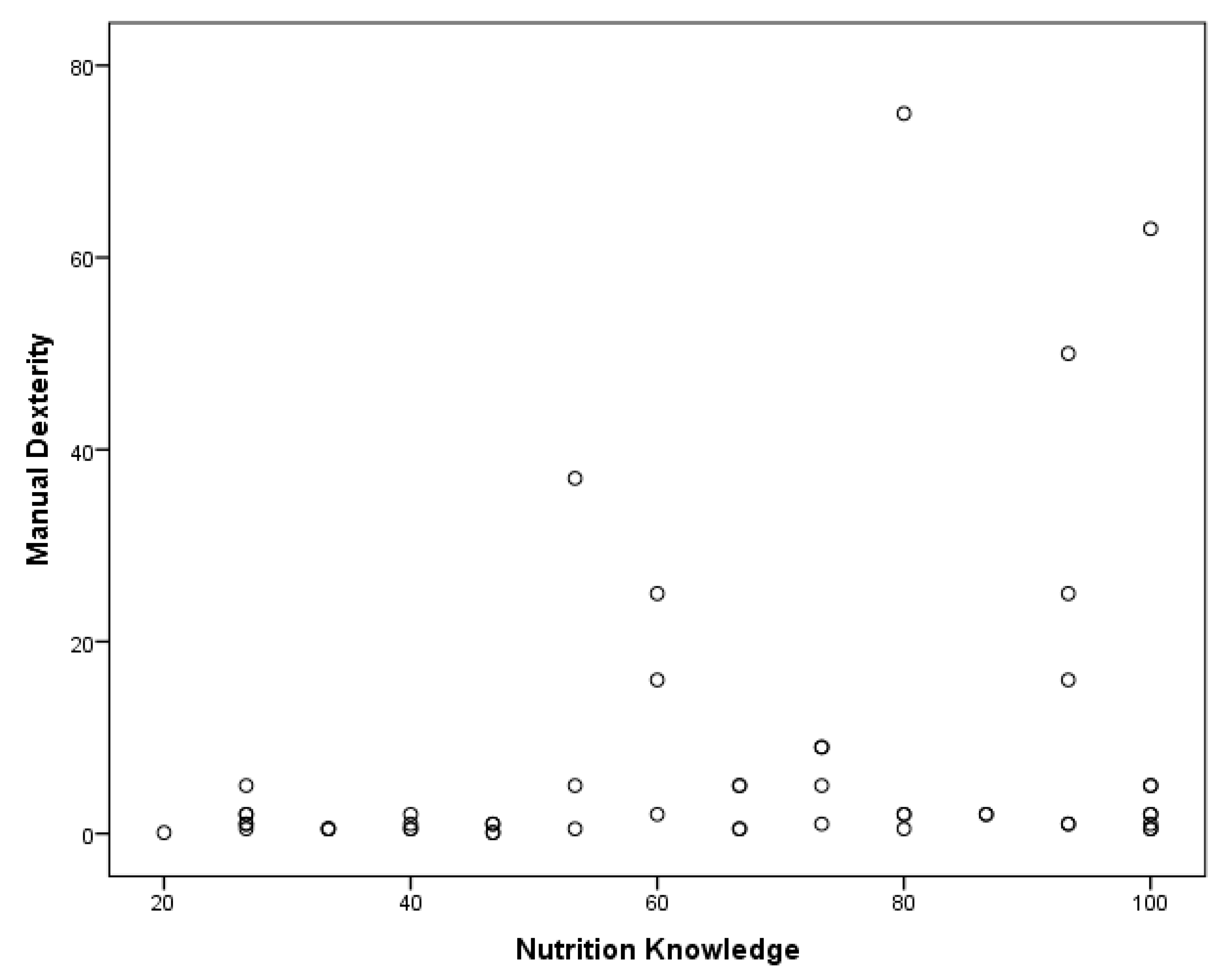
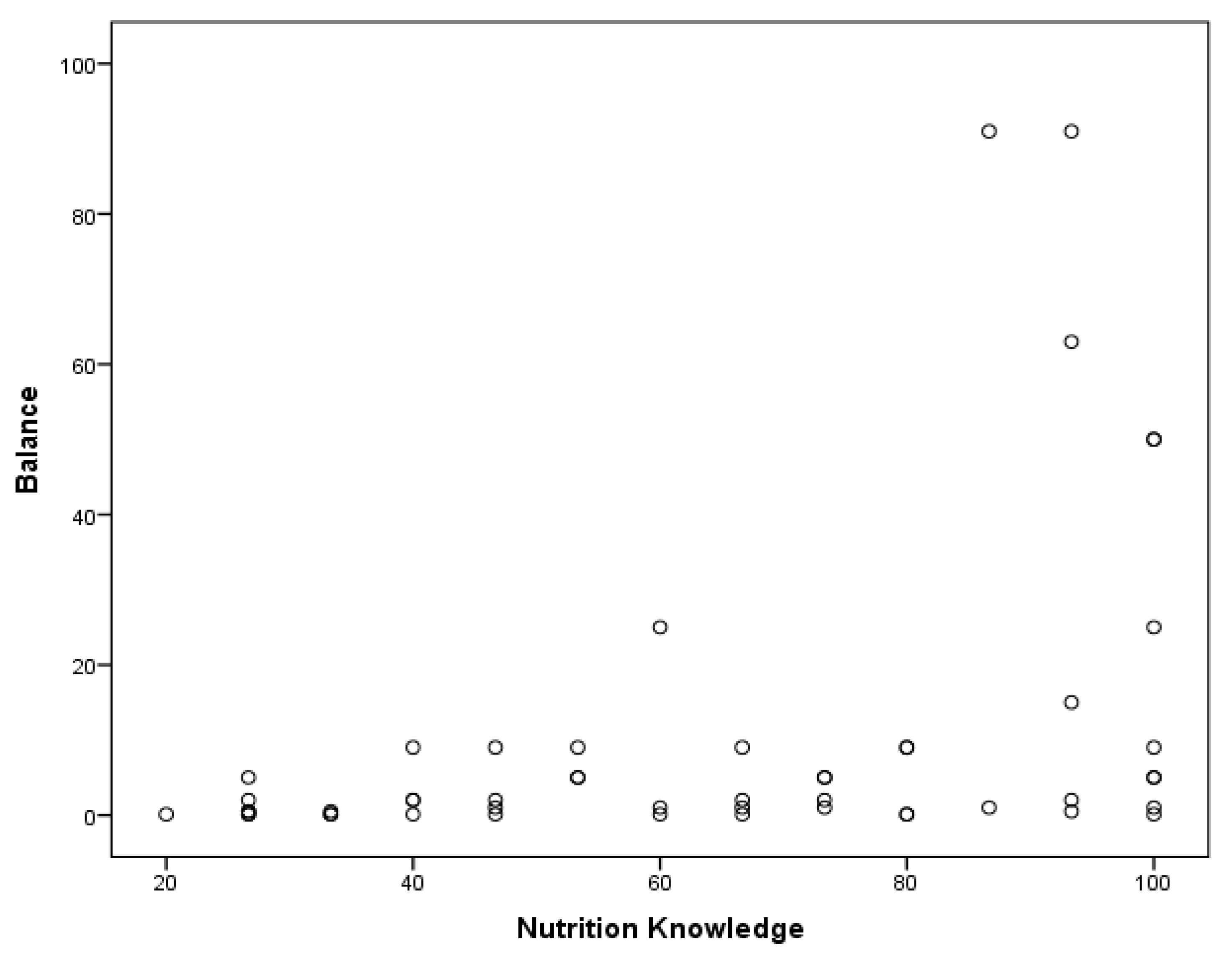
4.1. Nutrition Knowledge and Motor Competence
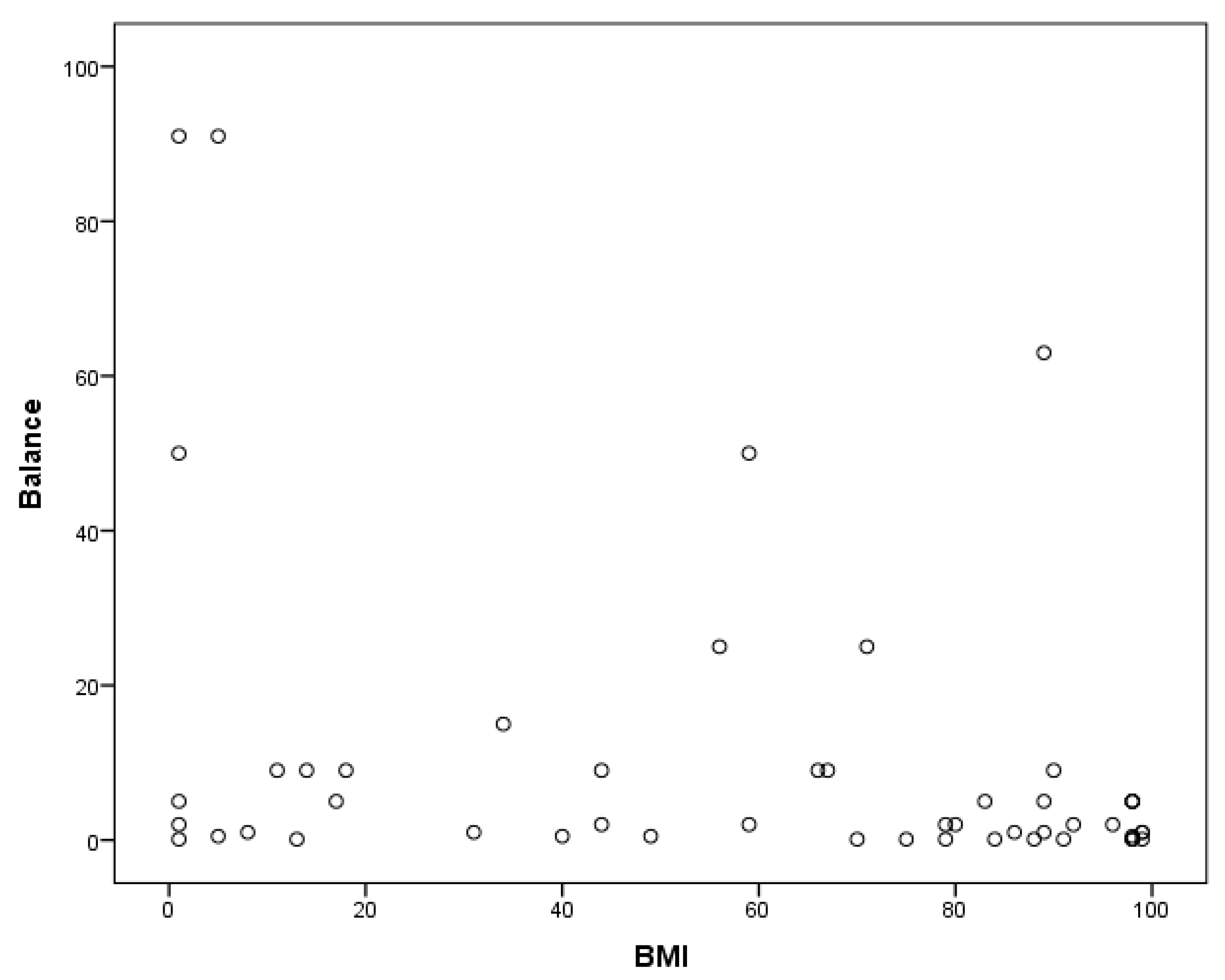
4.2. BMI and Motor Competence
4.3. Nutrition Knowledge and BMI
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. J. Am. Med. Assoc. 2014, 311, 806–814. [Google Scholar] [CrossRef]
- Macdonald, M.; Esposito, P.; Ulrich, D. The physical activity patterns of children with autism. BMC Res. Notes 2011, 4, 422. [Google Scholar] [CrossRef] [PubMed]
- Memari, A.H.; Ghaheri, B.; Ziaee, V.; Kordi, R.; Hafizi, S.; Moshayedi, P. Physical activity in children and adolescents with autism assessed by triaxial accelerometry. Pediat. Obes. 2013, 8, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Curtin, C.; Anderson, S.E.; Must, A.; Bandini, L. The prevalence of obesity in children with autism: A secondary data analysis using nationally representative data from the national survey of children’s health. BMC Pediat. 2010, 106, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Egan, A.M.; Dreyer, M.L.; Odar, C.C.; Beckwith, M.; Garrison, C.B. Obesity in young children with autism spectrum disorders: Prevalence and associated factors. Child. Obes. 2013, 2, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Strahan, B.E.; Elder, J.H. Obesity in adolescents with autism spectrum disorders. Res. Autism Spectr. Disord. 2013, 7, 1497–1500. [Google Scholar] [CrossRef]
- Phillips, K.L.; Schieve, L.A.; Visser, S.; Boulet, S.; Sharma, A.J.; Kogan, M.D.; Yeargin-Allsopp, M. Prevalence and impact of unhealthy weight in a national sample of us adolescents with autism and other learning and behavioral disabilities. Maternal Child Health J. 2014, 18, 1964–1975. [Google Scholar] [CrossRef] [PubMed]
- Zuckerman, K.; Hill, A.; Guion, K.; Voltolina, L.; Fombonne, E. Overweight and obesity: Prevalence and correlates in a large clinical sample of children with autism spectrum disorder. J. Autism Dev. Disord. 2014, 44, 1708–1719. [Google Scholar] [CrossRef] [PubMed]
- Ahearn, W.H.; Castine, T.; Nault, K.; Green, G. An assessment of food acceptance in children with autism or pervasive developmental disorder-not otherwise specified. J. Autism Dev. Dis. 2001, 31, 505–511. [Google Scholar] [CrossRef]
- Bandini, L.G.; Gleason, J.; Curtin, C.; Lividini, K.; Anderson, S.E.; Cermak, S.A.; Must, A. Comparison of physical activity between children with autism spectrum disorders and typically developing children. Autism 2013, 17, 44–54. [Google Scholar] [CrossRef] [PubMed]
- Schreck, K.A.; Williams, K. Food preferences and factors influencing food selectivity for children with autism spectrum disorders. Res. Dev. Disabil. 2006, 27, 353–363. [Google Scholar] [CrossRef] [PubMed]
- Schreck, K.A.; Williams, K.; Smith, A.F. A comparison of eating behaviors between children with and without autism. J. Autism Dev. Disord. 2004, 34, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Must, A.; Phillips, S.; Bandini, L. Longitudinal fruit and vegetable consumption, fiber, and glycemic load as predictors of fatness and relative weight change over adolescence in girls. Obes. Res. 2005, 13, A152–A153. [Google Scholar]
- Gase, L.N.; Robles, B.; Barragan, N.C.; Kuo, T. Relationship between nutritional knowledge and the amount of sugar-sweetened beverages consumed in los Angeles county. Health Educ. Behav. 2014, 41, 431–439. [Google Scholar] [CrossRef]
- Ludwig, D.S.; Peterson, K.E.; Gortmaker, S.L. Relation between consumption of sugar-sweetened drinks and childhood obesity: A prospective, observational analysis. Lancet 2001, 357, 505–508. [Google Scholar] [CrossRef]
- Must, A.; Tybor, D.J. Physical activity and sedentary behavior: A review of longitudinal studies of weight and adiposity in youth. Int. J. Obes. 2005, 29, S84–S96. [Google Scholar] [CrossRef]
- Tam, C.S.; Garnett, S.P.; Cowell, C.T.; Campbell, K.; Cabrera, G.; Baur, L.A. Soft drink consumption and excess weight gain in Australian school students: Results from the Nepean study. Int. J. Obes. 2006, 30, 1091–1093. [Google Scholar] [CrossRef] [PubMed]
- Rimmer, J.H.; Rubin, S.S.; Braddock, D. Barriers to exercise in African American women with physical disabilities. Arch. Phys. Med. Rehab. 2000, 81, 182–188. [Google Scholar] [CrossRef]
- Rimmer, J.H.; Riley, B.; Wang, E.; Rauworth, A.; Jurkowski, J. Physical activity participation among persons with disabilities: Barriers and facilitators. Am. J. Prev. Med. 2004, 26, 419–425. [Google Scholar] [CrossRef]
- Rimmer, J.H.; Rowland, J.L.; Yamaki, K. Obesity and secondary conditions in adolescents with disabilities: Addressing the needs of an underserved population. J. Adolesc. Health 2007, 41, 224–229. [Google Scholar] [CrossRef]
- Bryant, E.S.; Duncan, M.J.; Birch, S.L. Fundamental movement skills and weight status in British primary school children. Eur. J. Sport Sci. 2014, 14, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Cliff, D.P.; Okely, A.D.; Smith, L.M.; McKeen, K. Relationships between fundamental movement skills and objectively measured physical activity in preschool children. Pediatr. Exerc. Sci. 2009, 21, 436–449. [Google Scholar] [CrossRef] [PubMed]
- Erwin, H.E.; Castelli, D.M. National physical education standards: A summary of student performance and its correlates. Res. Q. Exerc. Sport 2008, 79, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Bandini, L.G.; Anderson, S.E.; Curtin, C.; Cermak, S.; Evans, E.W.; Scampini, R.; Must, A. Food selectivity in children with autism spectrum disorders and typically developing children. J. Pediatr. 2010, 157, 259–264. [Google Scholar] [CrossRef]
- Obrusnikova, I.; Cavalier, A. Perceived barriers and facilitators of participation in after-school physical activity by children with autism spectrum disorders. J. Dev. Phys. Disabil. 2011, 23, 195–211. [Google Scholar] [CrossRef]
- Rimmer, J.H.; Rowland, J.L. Health promotion for people with disabilities: Implications for empowering the person and promoting disability-friendly environments. Am. J. Lifes. Med. 2008, 2, 409–420. [Google Scholar] [CrossRef]
- Liu, T.; Hamilton, M.; Davis, L.; ElGarhy, S. Gross motor performance by children with autism spectrum disorder and typically developing children on TGMD-2. Child Adolesc. Behav. 2014, 2, 1–4. [Google Scholar] [CrossRef]
- Pan, C.; Tsai, C.; Chu, C. Fundamental movement skills in children diagnosed with autism spectrum disorders and attention deficit hyperactivity disorder. J. Autism Dev. Disord. 2009, 39, 1694–1705. [Google Scholar] [CrossRef] [PubMed]
- Provost, B.; Heimerl, S.; Lopez, B. Levels of gross and fine motor development in young children with autism spectrum disorder. Phys. Occup. Ther. Pediat. 2007, 27, 21–36. [Google Scholar] [CrossRef]
- Staples, K.; Reid, G. Fundamental movement skills and autism spectrum disorders. J. Autism Dev. Disord. 2010, 40, 209–217. [Google Scholar] [CrossRef]
- Sallis, J.F.; Glanz, K. The role of built environments in physical activity, eating, and obesity in childhood. Future Child. 2006, 16, 89–108. [Google Scholar] [CrossRef]
- Must, A.; Parisi, S.M. Sedentary behavior and sleep: Paradoxical effects in association with childhood obesity. Int. J. Obes. 2009, 33, S82–S86. [Google Scholar] [CrossRef]
- Must, A.; Phillips, S.M.; Curtin, C.; Anderson, S.E.; Maslin, M.; Lividini, K.; Bandini, L.G. Comparison of sedentary behaviors between children with autism spectrum disorders and typically developing children. Autism Int. J. Res. Pract. 2014, 18, 376–384. [Google Scholar] [CrossRef]
- Elbaum, B.; Vaughn, S. Can school-based interventions enhance the self-concept of students with learning disabilities? Except. Parent 1999, 29, 92–94. [Google Scholar]
- Griffiths, L.J.; Parsons, T.J.; Hill, A.J. Self-esteem and quality of life in obese children and adolescents: A systematic review. Int. J. Pediat. Obes. 2010, 5, 282–304. [Google Scholar] [CrossRef]
- Simpson, C.G.; Swicegood, P.R.; Gaus, M.D. Nutrition and fitness curriculum: Designing instructional interventions for children with developmental disabilities. Teach. Except. Child. 2006, 38, 50–53. [Google Scholar] [CrossRef]
- Henderson, S.E.; Sugden, D.A.; Barnett, A.L.; Brown, T.; Lalor, A. Movement assessment battery for children—Second edition. Phys. Occup. Ther. Pediat. 2009, 29, 86–103. [Google Scholar]
- Carlson, A.; Rowe, E.; Curby, T. Disentangling fine motor skills’ relations to academic achievement: The relative contributions of visual-spatial integration and visual-motor coordination. J. Genet. Psychol. 2013, 174, 514–533. [Google Scholar] [CrossRef]
- Dinehart, L.; Manfra, L. Associations between low-income children’s fine motor skills in preschool and academic performance in second grade. Early Educ. Dev. 2013, 24, 138–161. [Google Scholar] [CrossRef]
- Francis, M.; Dalrymple, N.; Nichols, S.S.D. The effects of a school-based intervention program on dietary intakes and physical activity among primary-school children in Trinidad and Tobago. Public Health Nutr. 2010, 13, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Klohe-Lehman, D.; Freeland-Graves, J.; Anderson, E.R.; McDowell, T.; Clarke, K.K.; Hanss-Nuss, H.; Milani, T.J. Nutrition knowledge is associated with greater weight loss in obese and overweight low-income mothers. J. Am. Dietet. Assoc. 2006, 106, 65–75. [Google Scholar] [CrossRef]
- Poh, B.K.; Kathryn Tham, B.L.; Wong, S.N.; Winnie Chee, S.S.; Tee, E.S. Nutritional status, dietary intake patterns and nutrition knowledge of children aged 5–6 years attending kindergartens in the klang valley, Malaysia. Malays. J. Nutr. 2012, 18, 231–242. [Google Scholar] [PubMed]
- Triches, R.M.; Giugliani, E. Obesity, eating habits and nutritional knowledge among school children. Revista de Saude Publica 2005, 39, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Parmenter, K.; Waller, J. Nutrition knowledge and food intake. Appetite 2000, 34, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Jobling, A. Beyond sex and cooking: Health education for individuals with intellectual disability. Mental Retard. 2001, 39, 310–321. [Google Scholar] [CrossRef]
- Curtin, C.; Jojic, M.; Bandini, L.G. Obesity in children with autism spectrum disorder. Harv. Rev. Psychiat. 2014, 22, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.S.; Wu, W.; Chumlea, W.C.; Roche, A.F. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am. J. Clin. Nutr. 2002, 76, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Must, A.; Strauss, R.S. Risks and consequences of childhood and adolescent obesity. Int. J. Obes. Relat. Metab. Disord. 1999, 23, S2–S11. [Google Scholar] [CrossRef] [PubMed]
- Tyler, C.V.; Schramm, S.C.; Karafa, M.; Tang, A.S.; Jain, A.K. Chronic disease risks in young adults with autism spectrum disorder: Forewarned is forearmed. Am. J. Intell. Dev. Disab. 2011, 116, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Data and statistics. Available online: https://www.cdc.gov/ncbddd/autism/data.html (accessed on 16 September 2018).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- Gower, J.R.; Slater, H.; Jordan, K.C.; Moyer-Mileur, L.; Wilkinson, R.D. Validity and reliability of a nutrition knowledge survey for assessment in elementary school children. J. Am. Dietet. Assoc. 2010, 110, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S.; Grummer-Strawn, L.; Flegal, K.M.; Mei, Z.; Johnson, C.L. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat. 2002, 11, 1–190. [Google Scholar]
- Krebs, N.F.; Himes, J.H.; Jacobson, D.; Nicklas, T.A.; Guilday, P.; Styne, D. Assessment of child and adolescent overweight and obesity. Pediatrics 2007, 120, S193–S228. [Google Scholar] [CrossRef]
- Graf, C.; Koch, B.; Kretschmann-Kandel, E.; Falkowski, G.; Christ, H.; Coburger, S.; Dordel, S. Correlation between BMI, leisure habits and motor abilities in childhood (CHILT-project). Int. J. Obes. Relat. Metab. Disord. 2004, 28, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Greier, K.; Riechelmann, H.; Burtscher, M. Prevalence of Obesity and Motor Performance Capabilities in Tyrolean Preschool Children; Springer: Friesach, Austria, 2014. [Google Scholar]
- Osmani, A.; Driton, M. Differences in the motoric abilities of students due to the body mass index (BMI). Sport Mont. 2014, 12, 89–92. [Google Scholar]
- D’Hondt, E.; Deforche, B.; Gentier, I.; Verstuyf, J.; Vaeyens, R.; Bourdeaudhuij, I.; Lenoir, M. A longitudinal study of gross motor coordination and weight status in children. Obesity 2014, 22, 1505–1511. [Google Scholar] [CrossRef]
- Frey, G.C.; Chow, B. Relationship between BMI, physical fitness, and motor skills in youth with mild intellectual disabilities. Int. J. Obes. 2006, 30, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Pitetti, K.H.; Yarmer, D.A.; Fernhall, B. Cardiovascular fitness and body composition of youth with and without mental retardation. Adapt. Phys. Activ. Q. 2001, 18, 127–141. [Google Scholar] [CrossRef]
- Burns, C.M.; Richman, R.; Caterson, I.D. Nutrition knowledge in the obese and overweight. Int. J. Obes. 1987, 11, 485–492. [Google Scholar] [CrossRef]
- Muehler, C.; Hobbs, J.; Lipira, P. Is body mass index (BMI) related to nutrition knowledge in children? Mo. J. Health Phys. Educ. Recr. Dance 2006, 16, 94–97. [Google Scholar]
- Reinehr, T.; Kersting, M.; Chahda, C.; Andler, W. Nutritional knowledge of obese and nonobese children. Nutr. Res. 2003, 23, 645–649. [Google Scholar] [CrossRef]
- Thakur, N.; D’Amico, F. Relationship of nutrition knowledge and obesity in adolescence. Family Med. 1999, 31, 122–127. [Google Scholar]
- Stankiewicz, M.; Pieszko, M.; Sliwinska, A.; Malgorzewicz, S.; Wierucki, L.; Zdrojewski, T.; Lysiak-Szydlowska, W. Obesity and diet awareness among polish children and adolescents in small towns and villages. Cent. Eur. J. Public Health 2014, 22, 12–16. [Google Scholar] [CrossRef]
- Srinivasan, S.M.; Pescatello, L.S.; Bhat, A.N. Current perspectives on physical activity and exercise recommendations for children and adolescents with autism spectrum disorders. Phys. Ther. 2014, 94, 875–889. [Google Scholar] [CrossRef] [PubMed]
- Alkon, A.; Crowley, A.A.; Benjamin Neelon, S.E.; Hill, S.; Pan, Y.; Nguyen, V.; Kotch, J.B. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health 2014, 14, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Hinckson, E.A.; Dickinson, A.; Water, T.; Sands, M.; Penman, L. Physical activity, dietary habits and overall health in overweight and obese children and youth with intellectual disability or autism. Res. Dev. Disabil. 2013, 34, 1170–1178. [Google Scholar] [CrossRef] [PubMed]
- Yu, O.K.C.; Rhee, Y.K.C.; Sohn, H.S.C.; Cha, Y.S.C. Effects of nutrition education on overweight and obese children in Chonbuk area—Focus on food habit, eating behaviors, dietary attitude, nutrition knowledge and nutrients intake. J. Korean Soc. Food Sci. Nutr. 2010, 39, 1286–1294. [Google Scholar] [CrossRef]
- Davison, K.K.; Birch, L.L. Childhood overweight: A contextual model and recommendations for future research. Obes. Rev. 2001, 2, 159–171. [Google Scholar] [CrossRef]
- Cermak, S.A.; Bandini, L.G.; Curtin, C. Food selectivity and sensory sensitivity in children with autism spectrum disorders. J. Am. Diet. Assoc. 2010, 110, 238–246. [Google Scholar] [CrossRef]
- Kohn, M.; Rees, J.M.; Brill, S.; Fonseca, H.; Jacobson, M.; Katzman, D.; Schneider, M. Preventing and treating adolescent obesity: A position paper of the society for adolescent medicine. J. Adolesc. Health 2006, 38, 784–787. [Google Scholar] [CrossRef]
| Model | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Regression | 6250.313 | 2 | 3125.157 | 5.385 | 0.008 |
| Residual | 27,854.028 | 48 | 580.292 | ||
| Total | 34,104.341 | 50 |
| Model | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Regression | 6815.148 | 1 | 6815.148 | 5.773 | 0.020 |
| Residual | 57,843.833 | 49 | 1180.486 | ||
| Total | 64,658.980 | 50 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, T.; Kelly, J.; Davis, L.; Zamora, K. Nutrition, BMI and Motor Competence in Children with Autism Spectrum Disorder. Medicina 2019, 55, 135. https://doi.org/10.3390/medicina55050135
Liu T, Kelly J, Davis L, Zamora K. Nutrition, BMI and Motor Competence in Children with Autism Spectrum Disorder. Medicina. 2019; 55(5):135. https://doi.org/10.3390/medicina55050135
Chicago/Turabian StyleLiu, Ting, Julie Kelly, Lyndsay Davis, and Krystal Zamora. 2019. "Nutrition, BMI and Motor Competence in Children with Autism Spectrum Disorder" Medicina 55, no. 5: 135. https://doi.org/10.3390/medicina55050135
APA StyleLiu, T., Kelly, J., Davis, L., & Zamora, K. (2019). Nutrition, BMI and Motor Competence in Children with Autism Spectrum Disorder. Medicina, 55(5), 135. https://doi.org/10.3390/medicina55050135





