Cross-Cultural Adaptation and Quantitative Evaluation of Dysfunctional Voiding and Incontinence Scoring System in Pediatric Serbian Population
Abstract
1. Introduction
2. Material and Methods
2.1. Study Group
2.2. Methodological Instrument
2.3. Translation Process
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Feldman, A.S.; Bauer, S.B. Diagnosis and management of dysfunctional voiding. Curr. Opin. Pediatr. 2006, 18, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Altan, M.; Çitamak, B.; Bozaci, A.C.; Mammadov, E.; Doğan, H.S.; Tekgül, S. Is there any difference between questionnaires on pediatric lower urinary tract dysfunction? Urology 2017, 103, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Akbal, C.; Genc, Y.; Burgu, B.; Ozden, E.; Tekgul, S. Dysfunctional voiding and incontinence scoring system: Quantitative evaluation of incontinence symptoms in pediatric population. J. Urol. 2005, 173, 969–973. [Google Scholar] [CrossRef] [PubMed]
- Tuygun, C.; Sertcelik, N.; Bakirtas, H.; Cakici, H.; Cetin, K.; Imamoglu, A.M. Usefulness of a new dysfunctional voiding and incontinence scoring system in predicting treatment effect in children with voiding dysfunction. Urol. Int. 2007, 79, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Bullinger, M.; Alonso, J.; Apolone, G.; Leplège, A.; Sullivan, M.; Wood-Dauphinee, S.; Gandek, B.; Wagner, A.; Aaronson, N.; Bech, P.; et al. Translating health status questionnaires and evaluating their quality: The IQOLA Project approach. International Quality of Life Assessment. J. Clin. Epidemiol. 1998, 51, 913–923. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila PA 1976) 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P. ISPOR Task Force for Translation and Cultural Adaptation. Principles of good practice for the translation and cultural adaptation process for Patient-Reported Outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Cirovic, D.; Petronic, I.; Nikolic, D.; Knezevic, T.; Vukadinovic, V.; Pavicevic, P. Validation of Serbian Version of Dysfunctional Voiding Symptom Score (DVSS) Questionnaire. J. Clin. Med. 2018, 7, 217. [Google Scholar] [CrossRef] [PubMed]
- Bael, A.; Lax, H.; de Jong, T.P.; Hoebeke, P.; Nijman, R.J.; Sixt, R.; Verhulst, J.; Hirche, H.; van Gool, J.D. European Bladder Dysfunction Study (European Union BMH1-CT94-1006). The relevance of urodynamic studies for Urge syndrome and dysfunctional voiding: A multicenter controlled trial in children. J. Urol. 2008, 180, 1486–1493. [Google Scholar] [CrossRef] [PubMed]
- Kaya Narter, F.; Tarhan, F. , Narter, K.F.; Sabuncu, K.; Alay Eser, R.; Akın, Y.; Ay, P. Reliability and validity of the Bladder and Bowel Dysfunction Questionnaireamong Turkish children. Turk. J. Med. Sci. 2017, 47, 1765–1769. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
| Groups | p Value | ||
|---|---|---|---|
| DVI Group (n = 57) | Control Group (n = 30) | ||
| Basic characteristics | |||
| Age (years) | 7.1 ± 1.5 | 7.1 ± 1.3 | 0.927 a |
| Gender—female | 29 (50.1%) | 15 (50%) | 0.938 b |
| Education—elementary school | 31 (54.4%) | 19 (63.3%) | 0.422 b |
| DVISSSR score | |||
| Score 9+ | 47 (82.5%) | 0 | <0.001 c |
| Score median (IQR) | 17 (12) | 1 (2) | <0.001 d |
| Score (repeated) median (IQR) | 17 (11) | ||
| Test/Retest Items | ICC |
|---|---|
| Item 1 | 0.907 |
| Item 2 | 0.931 |
| Item 3 | 0.860 |
| Item 4 | 0.886 |
| Item 5 | 0.797 |
| Item 6 | 0.867 |
| Item 7 | 0.889 |
| Item 8 | 0.965 |
| Item 9 | 0.929 |
| Item 10 | 0.897 |
| Item 11 | 0.926 |
| Item 12 | 0.889 |
| Item 13 | 0.906 |
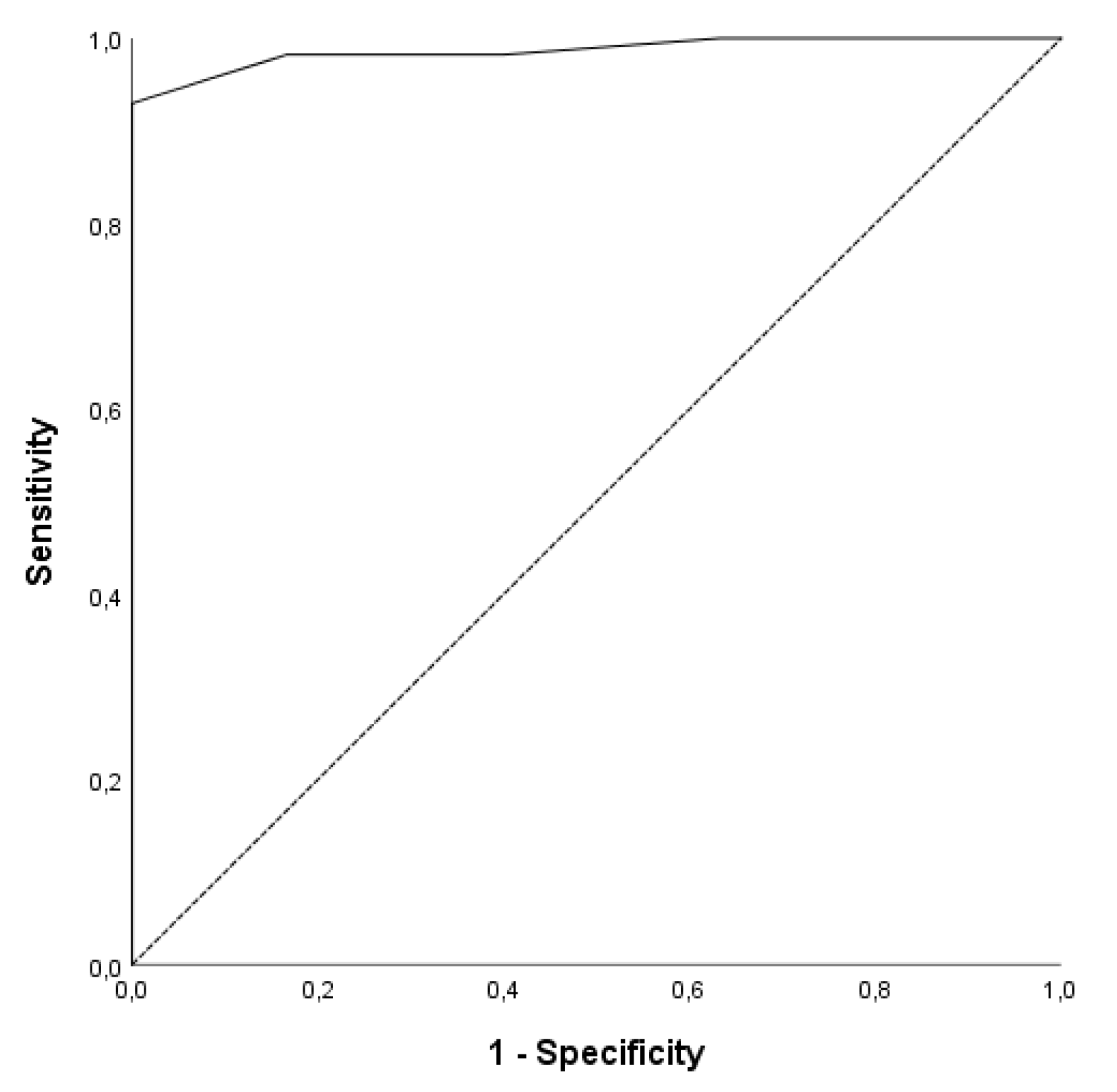
| Cut-Off | Sensitivity | Specificity | PPV | NPV | LR+ | LR- |
|---|---|---|---|---|---|---|
| 9+ | 0.82 | 1 | 1 | 0.75 | Inf. | 0.175 |
| 4+ | 0.93 | 1 | 1 | 0.88 | Inf. | 0.070 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cirovic, D.; Petronic, I.; Stojkovic, J.; Soldatovic, I.; Pavicevic, P.; Bizic, M.; Bokan-Mirkovic, V.; Knezevic, T.; Nikolic, D. Cross-Cultural Adaptation and Quantitative Evaluation of Dysfunctional Voiding and Incontinence Scoring System in Pediatric Serbian Population. Medicina 2019, 55, 100. https://doi.org/10.3390/medicina55040100
Cirovic D, Petronic I, Stojkovic J, Soldatovic I, Pavicevic P, Bizic M, Bokan-Mirkovic V, Knezevic T, Nikolic D. Cross-Cultural Adaptation and Quantitative Evaluation of Dysfunctional Voiding and Incontinence Scoring System in Pediatric Serbian Population. Medicina. 2019; 55(4):100. https://doi.org/10.3390/medicina55040100
Chicago/Turabian StyleCirovic, Dragana, Ivana Petronic, Jasna Stojkovic, Ivan Soldatovic, Polina Pavicevic, Marta Bizic, Vesna Bokan-Mirkovic, Tatjana Knezevic, and Dejan Nikolic. 2019. "Cross-Cultural Adaptation and Quantitative Evaluation of Dysfunctional Voiding and Incontinence Scoring System in Pediatric Serbian Population" Medicina 55, no. 4: 100. https://doi.org/10.3390/medicina55040100
APA StyleCirovic, D., Petronic, I., Stojkovic, J., Soldatovic, I., Pavicevic, P., Bizic, M., Bokan-Mirkovic, V., Knezevic, T., & Nikolic, D. (2019). Cross-Cultural Adaptation and Quantitative Evaluation of Dysfunctional Voiding and Incontinence Scoring System in Pediatric Serbian Population. Medicina, 55(4), 100. https://doi.org/10.3390/medicina55040100





