Alcohol and Cannabis Intake in Nursing Students
Abstract
1. Introduction
- -
- Examine the intake of alcohol, marijuana/hashish, and other illicit drugs in nursing students.
- -
- Explore the social and personal consequences of substance misuse and the moderating effects of sociodemographic variables.
2. Materials and Methods
2.1. Design and Participants
2.2. Sociodemographic Data
2.3. Evaluation of Alcohol Consumption
2.4. Evaluation of Substance Misuse
2.5. Statistical Analysis
3. Results
3.1. Study Sample
3.2. Evaluation of Alcohol Consumption
3.3. Evaluation of Substance Misuse and Its Consequences
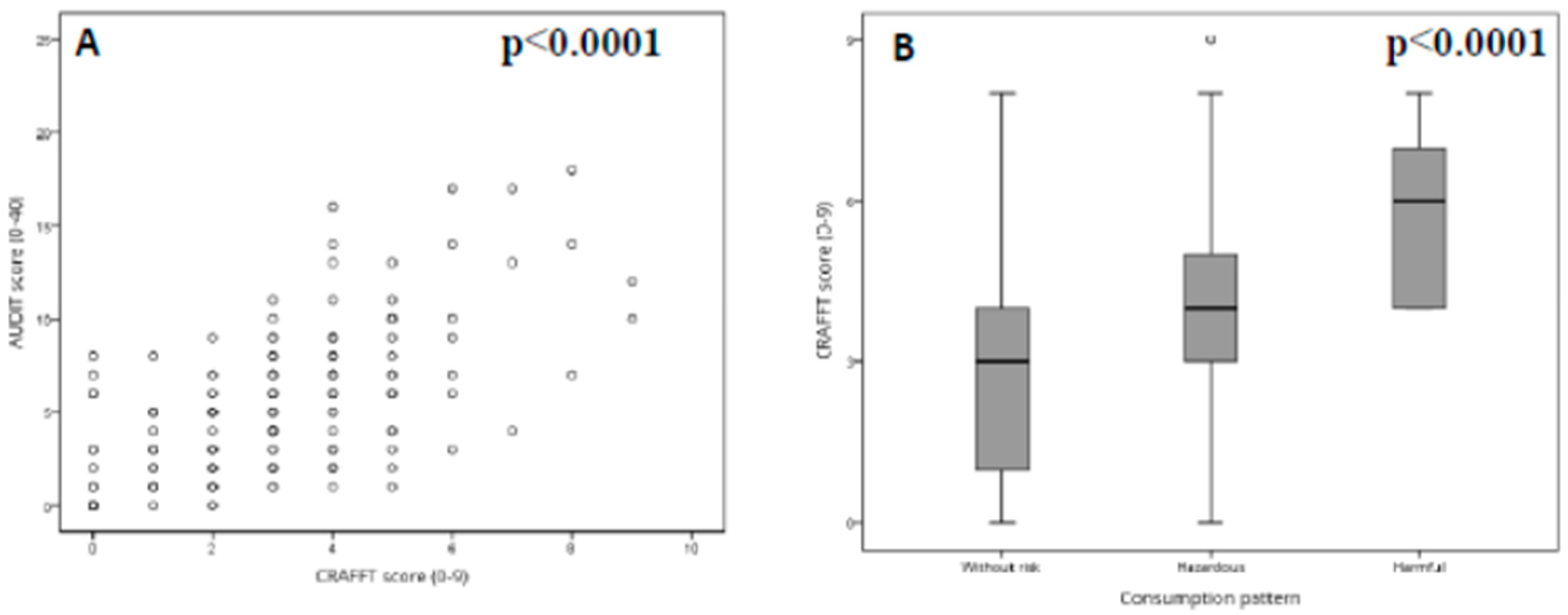
3.4. Analysis of the Associations between the AUDIT and CRAFFT Scales
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Hawkins, J.D.; Catalano, R.F.; Miller, J.Y. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychol. Bull. 1992, 112, 64–105. [Google Scholar] [CrossRef] [PubMed]
- Aresi, G.; Moore, S.; Marta, E. Drinking, drug use, and related consequences among university students completing study abroad experiences: A systematic review. Subst. Use Misuse 2016, 51, 1888–1904. [Google Scholar] [CrossRef] [PubMed]
- Carey, K.B.; Scott-Sheldon, L.A.J.; Carey, M.P.; DeMartini, K.S. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addict. Behav. 2007, 32, 2469–2494. [Google Scholar] [CrossRef] [PubMed]
- Davoren, M.P.; Shiely, F.; Byrne, M.; Perry, I.J. Hazardous alcohol consumption among university students in Ireland: A cross-sectional study. BMJ Open 2015, 5, e006045. [Google Scholar] [CrossRef] [PubMed]
- Garcia Montes, J.M.; Zaldivar Basurto, F.; Moreno Montoya, M.; Flores Cubos, P. Relationship between drug use and psychopathological variables of risk in university students. Psicothema 2013, 25, 433–439. [Google Scholar] [PubMed]
- Primack, B.A.; Kim, K.H.; Shensa, A.; Sidani, J.E.; Barnett, T.E.; Switzer, G.E. Tobacco, marijuana, and alcohol use in university students: A cluster analysis. J. Am. Coll. Health 2012, 60, 374–386. [Google Scholar] [CrossRef] [PubMed]
- Wicki, M.; Kuntsche, E.; Gmel, G. Drinking at European universities? A review of students’ alcohol use. Addict. Behav. 2010, 35, 913–924. [Google Scholar] [CrossRef] [PubMed]
- Craigs, C.L.; Bewick, B.M.; Gill, J.; O’May, F.; Radley, D. UK student alcohol consumption: A cluster analysis of drinking behaviour typologies. Health Educ. J. 2012, 71, 516–526. [Google Scholar] [CrossRef]
- Hepworth, J.; Schofield, T.; Leontini, R.; Germov, J. Alcohol-related harm minimization practices among university students: Does the type of residence have an impact? Br. J. Health Psychol. 2018, 23, 843–856. [Google Scholar] [CrossRef]
- Trostler, M.; Li, Y.; Plankey, M.W. Prevalence of binge drinking and associated co-factors among medical students in a U.S. Jesuit University. Am. J. Drug Alcohol Abuse 2014, 40, 336–341. [Google Scholar] [CrossRef]
- Tosevski, D.L.; Milovancevic, M.P.; Gajic, S.D. Personality and psychopathology of university students. Curr. Opin. Psychiatry 2010, 23, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Charlet, K.; Heinz, A. Harm reduction-a systematic review on effects of alcohol reduction on physical and mental symptoms. Addict. Biol. 2017, 22, 1119–1159. [Google Scholar] [CrossRef] [PubMed]
- Tembo, C.; Burns, S.; Kalembo, F. The association between levels of alcohol consumption and mental health problems and academic performance among young university students. PLoS ONE 2017, 12, e0178142. [Google Scholar] [CrossRef] [PubMed]
- Rassool, G.H. Nursing and substance misuse: Responding to the challenge. J. Adv. Nurs. 1993, 18, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Nair, J.M.; Nemeth, L.S.; Sommers, M.; Newman, S.; Amella, E. Alcohol use, misuse, and abuse among nursing students: A photovoice study. J. Addict. Nurs. 2016, 27, 12–23. [Google Scholar] [CrossRef]
- Rabanales Sotos, J.; Lopez Gonzalez, A.; Parraga Martinez, I.; Campos Rosa, M.; Simarro Herraez, M.J.; Lopez-Torres Hidalgo, J. Prevalence of hazardous drinking among nursing students. J. Adv. Nurs. 2015, 71, 581–590. [Google Scholar] [CrossRef] [PubMed]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the alcohol use disorders identification test (audit): Who collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Adewuya, A.O. Validation of the alcohol use disorders identification test (audit) as a screening tool for alcohol-related problems among Nigerian university students. Alcohol Alcohol. 2005, 40, 575–577. [Google Scholar] [CrossRef]
- Kokotailo, P.K.; Egan, J.; Gangnon, R.; Brown, D.; Mundt, M.; Fleming, M. Validity of the alcohol use disorders identification test in college students. Alcohol. Clin. Exp. Res. 2004, 28, 914–920. [Google Scholar] [CrossRef]
- García Carretero, M.Á.; Novalbos Ruiz, J.P.; Martínez Delgado, J.M.; O’Ferrall González, C. Validation of the Alcohol Use Disorders Identification Test in university students: AUDIT and AUDIT-C. Adicciones 2016, 28, 194–204. [Google Scholar] [CrossRef]
- Babor, T.F.; Higgins-Biddle, J.C.; Saunders, J.B.; Moneiro, M.G. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care, 2nd ed.; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Rickwood, D.; George, A.; Parker, R.; Mikhailovich, K. Harmful alcohol use on campus: Impact on young people at university. Youth Stud. Aust. 2011, 30, 34. [Google Scholar]
- Bertini, M.C.; Busaniche, J.; Baquero, F.; Eymann, A.; Krauss, M.; Paz, M.; Catsicaris, C. Transcultural adaptation and validation of the CRAFFT as a screening test for problematic alcohol and substance use, abuse and dependence in a group of Argentine adolescents. Arch. Argent. Pediatr. 2015, 13, 114–118. [Google Scholar]
- Rial, A.; Kim-Harris, S.; Knight, J.R.; Araujo, M.; Gómez, P.; Braña, T.; Varela, J.; Golpe, S. Validación empírica del CRAFFT Abuse Screening Test en una muestra de adolescentes españoles. Adicciones 2018, 2, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.B.; Moss, H.B. Providing alcohol-related screening and brief interventions to adolescents through health care systems: Obstacles and solutions. PLoS Med. 2010, 7, e1000214. [Google Scholar] [CrossRef] [PubMed]
- Nash, A.J.; Marcus, M.T.; Cron, S.; Scamp, N.; Truitt, M.; McKenna, Z. Preparing Nursing Students to Work With Patients With Alcohol or Drug-Related Problems. J Addict Nurs. 2017, 28, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Who.int. Alcohol. 2019. Available online: https://www.who.int/news-room/fact-sheets/detail/alcohol (accessed on 28 April 2019).
- Aceijas, C.; Waldhausl, S.; Lambert, N.; Cassar, S.; Bello-Corassa, R. Determinants of health-related lifestyles among university students. Perspect. Publ. Health. 2017, 137, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Strunin, L.; Diaz-Martinez, A.; Diaz-Martinez, L.R.; Kuranz, S.; Hernandez-Avila, C.; Fernandez-Varela, H. Changes in alcohol use among first year university students in Mexico. Subst. Use Misuse 2015, 50, 106–113. [Google Scholar] [CrossRef]
- Fugitt, J.L.; Ham, L.S.; Bridges, A.J. Undifferentiated Gender Role Orientation, Drinking Motives, and Increased Alcohol Use in Men and Women. Subst Use Misuse 2017, 52, 760–772. [Google Scholar] [CrossRef] [PubMed]
- Romo-Avilés, N. Cannabis, juventud y género: Nuevos patrones de consumo, nuevos modelos de intervención. Trastor Adict. 2011, 13, 91–93. [Google Scholar] [CrossRef]
- O’Malley, P.M.; Johnston, L.D.; Bachman, J.G. Alcohol use among adolescents. Alcohol. Res. 1998, 22, 85. [Google Scholar]
- Suerken, C.K.; Reboussin, B.A.; Egan, K.L.; Sutfin, E.L.; Wagoner, K.G.; Spangler, J.; Wolfson, M. Marijuana use trajectories and academic outcomes among college students. Drug Alcohol Depend. 2016, 162, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, J.A.; Stephens, V.; Allen, D.F. Race, sex, marihuana use and alcohol intoxication in college students. J. Stud. Alcohol 1983, 44, 733–738. [Google Scholar] [CrossRef]
- Phillips, K.T.; Phillips, M.M.; Duck, K.D. Factors associated with marijuana use and problems among college students in Colorado. Subst. Use Misuse 2018, 53, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Quintero, C.; Neumark, Y. Prevalence and determinants of resistance to use drugs among adolescents who had an opportunity to use drugs. Drug Alcohol Depend. 2015, 149, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Van Etten, M.L.; Anthony, J.C. Male-female differences in transitions from first drug opportunity to first use: Searching for subgroup variation by age, race, region, and urban status. J. Womens Health Gend. Based Med. 2001, 10, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Schulte, M.T.; Hser, Y.-I. Substance use and associated health conditions throughout the lifespan. Publ. Health Rev. 2014, 35, 3. [Google Scholar] [CrossRef]
- Cuttler, C.; Mischley, L.K.; Sexton, M. Sex differences in cannabis use and effects: A cross-sectional survey of cannabis users. Cannabis Cannabinoid Res. 2016, 1, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Sham, P.C.; MacLean, C.J.; Kendler, K.S. A typological model of schizophrenia based on age at onset, sex and familial morbidity. Acta Psychiatr. Scand. 1994, 89, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Ashton, C.H. Pharmacology and effects of cannabis: A brief review. Br. J. Psychiatry 2001, 178, 101–106. [Google Scholar] [CrossRef]
- Papazisis, G.; Siafis, S.; Tsakiridis, I.; Koulas, I.; Dagklis, T.; Kouvelas, D. Prevalence of cannabis use among medical students: A systematic review and meta-analysis. Subst. Abuse 2018, 12. [Google Scholar] [CrossRef]
- Solinas, M.; Yasar, S.; Goldberg, S.R. Endocannabinoid system involvement in brain reward processes related to drug abuse. Pharmacol. Res. 2007, 56, 393–405. [Google Scholar] [CrossRef] [PubMed]
- De Luca, M.A.; Di Chiara, G.; Cadoni, C.; Lecca, D.; Orsolini, L.; Papanti, D.; Corkery, J.; Schifano, F. Cannabis; epidemiological, neurobiological and psychopathological issues: An update. CNS Neurol. Disord. Drug Targets 2017, 16, 598–609. [Google Scholar] [CrossRef] [PubMed]
- Abelman, D.D. Mitigating risks of students use of study drugs through understanding motivations for use and applying harm reduction theory: A literature review. Harm. Reduct. J. 2017, 14, 68. [Google Scholar] [CrossRef] [PubMed]
- Boland, M.; Fitzpatrick, P.; Scallan, E.; Daly, L.; Herity, B.; Horgan, J.; Bourke, G. Trends in medical student use of tobacco, alcohol and drugs in an Irish university, 1973-2002. Drug Alcohol Depend. 2006, 85, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Orsolini, L.; Chiappini, S.; Volpe, U.; Berardis, D.; Latini, R.; Papanti, G.D.; Corkery, A.J.M. Use of medicinal cannabis and synthetic cannabinoids in post-traumatic stress disorder (PTSD): A Systematic Review. Medicina (Kaunas) 2019, 55, 525. [Google Scholar] [CrossRef] [PubMed]
- Roncero, C.; Rodríguez-Cintas, L.; Egido, A.; Barral, C.; Pérez-Pazos, J.; Collazos, F.; Grau-López, L.; Casas, M. The influence of medical student gender and drug use on the detection of addiction in patients. J. Addict. Dis. 2014, 33, 277–288. [Google Scholar] [CrossRef]
- Slutske, W.S. Alcohol use disorders among US college students and their non-college-attending peers. Arch. Gen. Psychiatry 2005, 62, 321–327. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, P.M.; Johnston, L.D. Epidemiology of alcohol and other drug use among American college students. J. Stud. Alcohol Suppl. 2002, 14, 23–39. [Google Scholar] [CrossRef]
- Skidmore, C.R.; Kaufman, E.A.; Crowell, S.E. Substance Use Among College Students. Child. Adolesc. Psychiatr. Clin. N. Am. 2016, 25, 735–753. [Google Scholar] [CrossRef]
- Fuentes, M.C.; Alarcón, A.; García, F.; Gracia, E. Consumo de alcohol, tabaco, cannabis y otras drogas en la adolescencia: Efectos de la familia y el barrio [Use of alcohol, tobacco, cannabis and other drugs in adolescence: Effects of family and neighborhood]. An. Psicol. Psychol. 2015, 31, 1000–1007. [Google Scholar] [CrossRef]
- Bryden, A.; Roberts, B.; Petticrew, M.; McKee, M. A systematic review of the influence of community level social factors on alcohol use. Health Place 2013, 21, 70–85. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.; Mrug, S. School-level correlates of adolescent tobacco, alcohol, and marijuana use. Subst. Use Misuse 2015, 50, 1518–1528. [Google Scholar] [CrossRef] [PubMed]
- Alberdi-Erice, M.J.; Huizi-Egilegor, X.; Barandiaran-Lasa, M.; Zupiria-Gorostidi, X.; Uranga-Iturrioz, M.J. Trends in smoking and alcohol consumption among nursing students. Enferm. Clin. 2007, 17, 63–70. [Google Scholar] [PubMed]
- Platt, L.; Melendez-Torres, G.J.; O’Donnell, A.; Bradley, J.; Newbury-Birch, D.; Kaner, E.; Ashton, C. How effective are brief interventions in reducing alcohol consumption: Do the setting, practitioner group and content matter? Findings from a systematic review and metaregression analysis. BMJ Open 2016, 6, e011473. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.K.; Cameron, J.; Battams, S.; Roche, A. What works in school-based alcohol education: A systematic review. Health Educ. J. 2016, 75, 780–798. [Google Scholar] [CrossRef]
- Cameron, D.; Epton, T.; Norman, P.; Sheeran, P.; Harris, P.R.; Webb, T.L.; Julious, S.A.; Brennan, A.; Thomas, C.; Petroczi, A.; et al. A theory-based online health behaviour intervention for new university students (U@Uni:LifeGuide): Results from a repeat randomized controlled trial. Trials 2015, 16, 555. [Google Scholar] [CrossRef]
- Jensen, C.; Forlini, C.; Partridge, B.; Hall, W. Australian university students’ coping strategies and use of pharmaceutical stimulants as cognitive enhancers. Front. Psychol. 2016, 7, 277. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; McEnroe-Petitte, D.M.; Gloe, D.; Thomas, L.; Papathanasiou, I.V.; Tsaras, K. A literature review on stress and coping strategies in nursing students. J. Ment. Health. 2017, 26, 471–480. [Google Scholar] [CrossRef]
- Javadi-Pashaki, N.; Darvishpour, A. Survey of stress and coping strategies to predict the general health of nursing staff. J. Educ. Health Promot. 2019, 8, 74. [Google Scholar]
- Sasaki, M.; Kitaoka-Higashiguchi, K.; Morikawa, Y.; Nakagawa, H. Relationship between stress coping and burnout in Japanese hospital nurses. J. Nurs. Manag. 2009, 17, 359–365. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, B.; Trace, A.; O’Donovan, M.; Brady-Nevin, C.; Murphy, M.; O’Shea, M.; O’Regan, P. Nursing and midwifery students’ stress and coping during their undergraduate education programmes: An integrative review. Nurse Educ Today. 2018, 61, 197–209. [Google Scholar] [CrossRef] [PubMed]


| Item | Answer | Frequency | Percentage | |
|---|---|---|---|---|
| PART A | Item 1. Drink any alcohol (more than a few sips)? (Do not count sips of alcohol taken during family or religious events) | Yes | 158 | 86.8 |
| No | 24 | 13.2 | ||
| Item 2. Smoke any marijuana or hashish? | Yes | 62 | 34.1 | |
| No | 120 | 65.9 | ||
| Item 3. Use anything else to get high? (“anything else” includes illegal drugs, over the counter and prescription drugs, and things that you sniff or “huff”) | Yes | 10 | 5.5 | |
| No | 172 | 94.5 | ||
| PART B | Item 4. Have you ever ridden in a car with someone (including yourself) who was “high” or had been using alcohol or drugs? | Yes | 121 | 75.6 |
| No | 39 | 24.4 | ||
| Item 5. Do your family or friends ever tell you that you should cut down on your drinking or drug use? | Yes | 17 | 10.6 | |
| No | 143 | 89.4 | ||
| Item 6. Do you ever use alcohol or drugs to relax, feel better about yourself, or fit in? | Yes | 48 | 30.0 | |
| No | 112 | 70.0 | ||
| Item 7. Have you ever gotten into trouble while you were using alcohol or drugs? | Yes | 17 | 10.6 | |
| No | 143 | 89.4 | ||
| Item 8. Do you ever forget things you did while using alcohol or drugs? | Yes | 84 | 52.5 | |
| No | 76 | 47.5 | ||
| Item 9. Do you ever use alcohol or drugs while you are by yourself, or alone? | Yes | 31 | 19.4 | |
| No | 129 | 80.6 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tejedor-Cabrera, C.; Cauli, O. Alcohol and Cannabis Intake in Nursing Students. Medicina 2019, 55, 628. https://doi.org/10.3390/medicina55100628
Tejedor-Cabrera C, Cauli O. Alcohol and Cannabis Intake in Nursing Students. Medicina. 2019; 55(10):628. https://doi.org/10.3390/medicina55100628
Chicago/Turabian StyleTejedor-Cabrera, Carlos, and Omar Cauli. 2019. "Alcohol and Cannabis Intake in Nursing Students" Medicina 55, no. 10: 628. https://doi.org/10.3390/medicina55100628
APA StyleTejedor-Cabrera, C., & Cauli, O. (2019). Alcohol and Cannabis Intake in Nursing Students. Medicina, 55(10), 628. https://doi.org/10.3390/medicina55100628






