Subclinical Atrial Fibrillation and Risk of Stroke: Past, Present and Future
Abstract
1. Background
2. Importance of SCAF
3. Stroke Risk
4. SCAF Burden
5. Progression
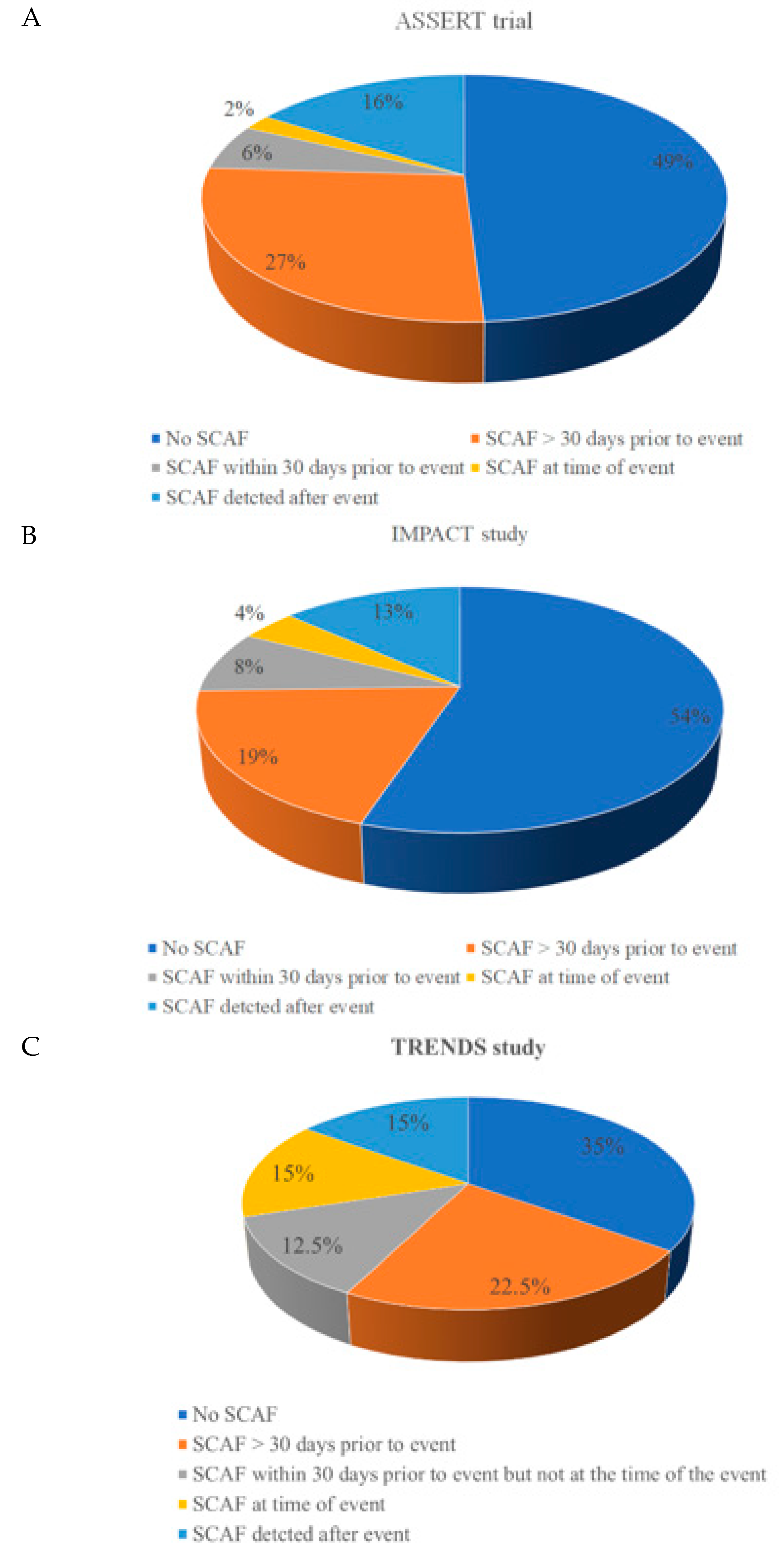
6. Mechanism of Increased Stroke in SCAF
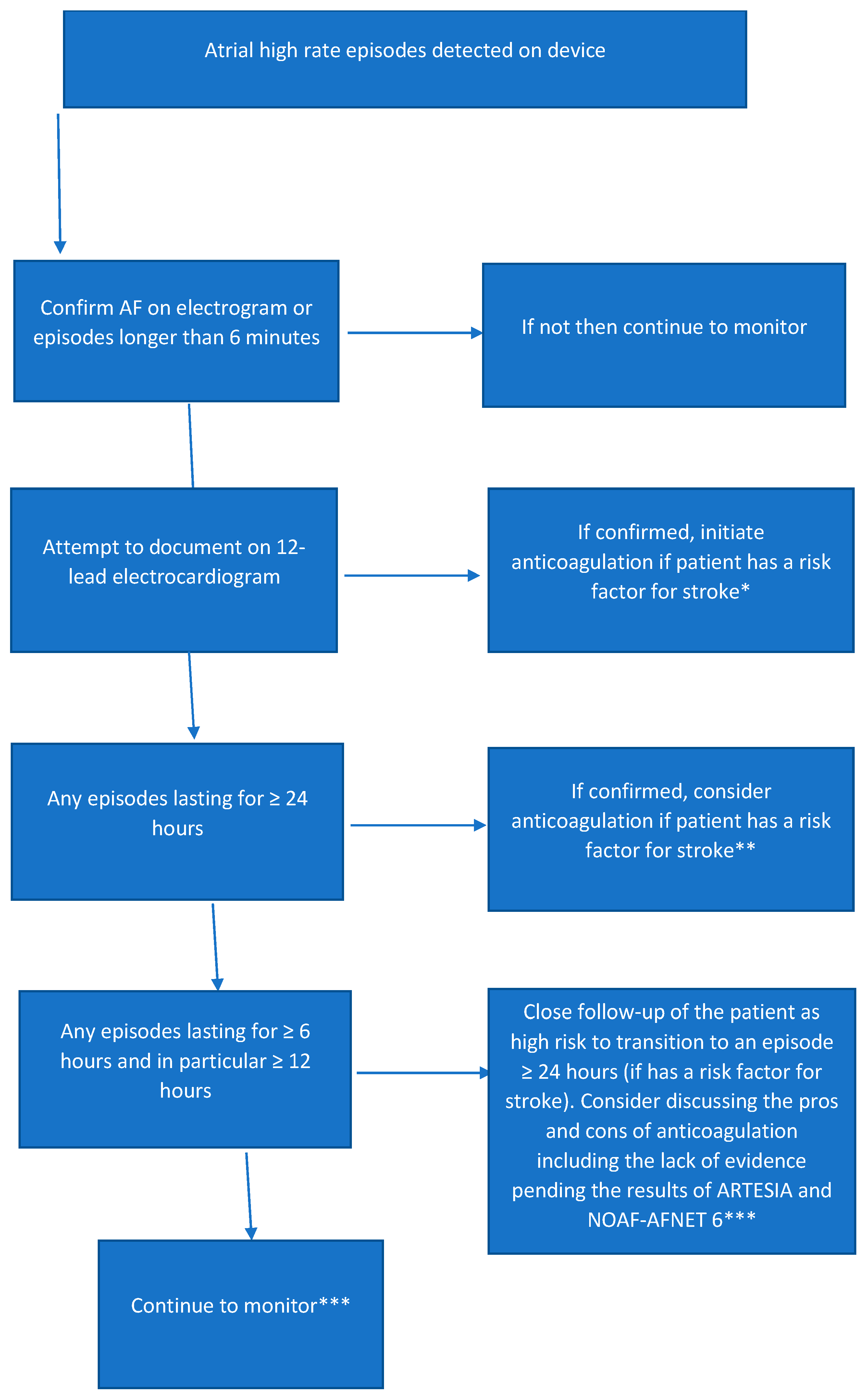
7. Treatment
8. Future Directions
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Healey, J.S.; Connolly, S.J.; Gold, M.R.; Israel, C.W.; Van Gelder, I.C.; Capucci, A.; Lau, C.P.; Fain, E.; Yang, S.; Bailleul, C.; et al. Subclinical Atrial Fibrillation and the Risk of Stroke. N. Engl. J. Med. 2012, 366, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.-C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed]
- Nattel, S.; Guasch, E.; Savelieva, I.; Cosio, F.G.; Valverde, I.; Halperin, J.L.; Conroy, J.M.; Al-Khatib, S.M.; Hess, P.L.; Kirchhof, P.; et al. Early management of atrial fibrillation to prevent cardiovascular complications. Eur. Heart J. 2014, 35, 1448–1456. [Google Scholar] [CrossRef] [PubMed]
- Lubitz, S.A.; Yin, X.; McManus, D.D.; Weng, L.-C.; Aparicio, H.J.; Walkey, A.J.; Romero, J.R.; Kase, C.S.; Ellinor, P.T.; Wolf, P.A.; et al. Stroke as the Initial Manifestation of Atrial Fibrillation. Stroke 2017, 48, 490–492. [Google Scholar] [CrossRef]
- Mond, H.G.; Proclemer, A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: Calendar year 2009—A World Society of Arrhythmia’s project. Pacing Clin. Electrophysiol. 2011, 34, 1013–1027. [Google Scholar] [CrossRef] [PubMed]
- Birnie, D.; Williams, K.; Guo, A.; Mielniczuk, L.; Davis, D.; Lemery, R.; Green, M.; Gollob, M.; Tang, A. Reasons for Escalating Pacemaker Implants. Am. J. Cardiol. 2006, 98, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Saver, J.L. Cryptogenic Stroke. N. Engl. J. Med. 2016, 374, 2065–2074. [Google Scholar] [CrossRef] [PubMed]
- Kishore, A.; Vail, A.; Majid, A.; Dawson, J.; Lees, K.R.; Tyrrell, P.J.; Smith, C.J. Detection of Atrial Fibrillation After Ischemic Stroke or Transient Ischemic Attack. Stroke 2014, 45, 520–526. [Google Scholar] [CrossRef]
- Diener, H.-C.; Sacco, R.L.; Easton, J.D.; Granger, C.B.; Bernstein, R.A.; Uchiyama, S.; Kreuzer, J.; Cronin, L.; Cotton, D.; Grauer, C.; et al. Dabigatran for Prevention of Stroke after Embolic Stroke of Undetermined Source. N. Engl. J. Med. 2019, 380, 1906–1917. [Google Scholar] [CrossRef]
- Hart, R.G.; Sharma, M.; Mundl, H.; Kasner, S.E.; Bangdiwala, S.I.; Berkowitz, S.D.; Swaminathan, B.; Lavados, P.; Wang, Y.; Wang, Y.; et al. Rivaroxaban for Stroke Prevention after Embolic Stroke of Undetermined Source. N. Engl. J. Med. 2018, 378, 2191–2201. [Google Scholar] [CrossRef]
- Sanna, T.; Diener, H.-C.; Passman, R.S.; Di Lazzaro, V.; Bernstein, R.A.; Morillo, C.A.; Rymer, M.M.; Thijs, V.; Rogers, T.; Beckers, F.; et al. Cryptogenic Stroke and Underlying Atrial Fibrillation. N. Engl. J. Med. 2014, 370, 2478–2486. [Google Scholar] [CrossRef] [PubMed]
- Gladstone, D.J.; Spring, M.; Dorian, P.; Panzov, V.; Thorpe, K.E.; Hall, J.; Vaid, H.; O’Donnell, M.; Laupacis, A.; Côté, R.; et al. Atrial Fibrillation in Patients with Cryptogenic Stroke. N. Engl. J. Med. 2014, 370, 2467–2477. [Google Scholar] [CrossRef] [PubMed]
- Wein, T.; Lindsay, M.P.; Cote, R.; Foley, N.; Berlingieri, J.; Bhogal, S.; Bourgoin, A.; Buck, B.H.; Cox, J.; Davidson, D.; et al. Canadian stroke best practice recommendations: Secondary prevention of stroke, sixth edition practice guidelines, update 2017. Int. J. Stroke 2018, 13, 420–443. [Google Scholar] [CrossRef] [PubMed]
- Hart, R.G.; Diener, H.C.; Coutts, S.B.; Easton, J.D.; Granger, C.B.; O’Donnell, M.J.; Sacco, R.L.; Connolly, S.J.; Cryptogenic Stroke, E.I.W.G. Embolic strokes of undetermined source: The case for a new clinical construct. Lancet Neurol. 2014, 13, 429–438. [Google Scholar] [CrossRef]
- Glotzer, T.V.; Daoud, E.G.; Wyse, D.G.; Singer, D.E.; Ezekowitz, M.D.; Hilker, C.; Miller, C.; Qi, D.; Ziegler, P.D. The Relationship Between Daily Atrial Tachyarrhythmia Burden from Implantable Device Diagnostics and Stroke Risk. Circ. Arrhythmia Electrophysiol. 2009, 2, 474–480. [Google Scholar] [CrossRef]
- Glotzer, T.V.; Hellkamp, A.S.; Zimmerman, J.; Sweeney, M.O.; Yee, R.; Marinchak, R.; Cook, J.; Paraschos, A.; Love, J.; Radoslovich, G.; et al. Atrial High Rate Episodes Detected by Pacemaker Diagnostics Predict Death and Stroke. Circulation 2003, 107, 1614–1619. [Google Scholar] [CrossRef]
- Boriani, G.; Glotzer, T.V.; Santini, M.; West, T.M.; De Melis, M.; Sepsi, M.; Gasparini, M.; Lewalter, T.; Camm, J.A.; Singer, D.E. Device-detected atrial fibrillation and risk for stroke: An analysis of >10 000 patients from the SOS AF project (Stroke prevention Strategies based on Atrial Fibrillation information from implanted devices). Eur. Heart J. 2013, 35, 508–516. [Google Scholar] [CrossRef]
- Capucci, A.; Santini, M.; Padeletti, L.; Gulizia, M.; Botto, G.; Boriani, G.; Ricci, R.; Favale, S.; Zolezzi, F.; Di Belardino, N.; et al. Monitored Atrial Fibrillation Duration Predicts Arterial Embolic Events in Patients Suffering from Bradycardia and Atrial Fibrillation Implanted with Antitachycardia Pacemakers. J. Am. Coll. Cardiol. 2005, 46, 1913–1920. [Google Scholar] [CrossRef]
- Shanmugam, N.; Boerdlein, A.; Proff, J.; Ong, P.; Valencia, O.; Maier, S.K.G.; Bauer, W.R.; Paul, V.; Sack, S. Detection of atrial high-rate events by continuous Home Monitoring: Clinical significance in the heart failure–cardiac resynchronization therapy population. Europace 2011, 14, 230–237. [Google Scholar] [CrossRef]
- Pollak, W.M.; Simmons, J.D.; Interian, A., Jr.; Atapattu, S.A.; Castellanos, A.; Myerburg, R.J.; Mitrani, R.D. Clinical utility of intraatrial pacemaker stored electrograms to diagnose atrial fibrillation and flutter. Pacing Clin. Electrophysiol. 2001, 24, 424–429. [Google Scholar] [CrossRef]
- Healey, J.S.; Alings, M.; Ha, A.; Leong-Sit, P.; Birnie, D.H.; Graaf JJd Freericks, M.; Verma, A.; Wang, J.; Leong, D.; Dokainish, H.; et al. Subclinical Atrial Fibrillation in Older Patients. Circulation 2017, 136, 1276–1283. [Google Scholar] [CrossRef] [PubMed]
- Healey, J.S.; Wong, J.A. Subclinical atrial fibrillation: The significance of progression to longer episodes. Heart Rhythm 2018, 15, 384–385. [Google Scholar] [CrossRef] [PubMed]
- Reiffel, J.A.; Verma, A.; Kowey, P.R.; Halperin, J.L.; Gersh, B.J.; Wachter, R.; Pouliot, E.; Ziegler, P.D. Incidence of Previously Undiagnosed Atrial Fibrillation Using Insertable Cardiac Monitors in a High-Risk Population: The Reveal AF Study. JAMA Cardiol. 2017, 2, 1120–1127. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.Y.; Chung, M.K.; Allen, L.A.; Ezekowitz, M.; Furie, K.L.; McCabe, P.; Noseworthy, P.A.; Perez, M.V.; Turakhia, M.P. Atrial Fibrillation Burden: Moving Beyond Atrial Fibrillation as a Binary Entity: A Scientific Statement from the American Heart Association. Circulation 2018, 137, e623–e644. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, R.; Perera, T.; Elliott, A.D.; Twomey, D.J.; Kumar, S.; Munwar, D.A.; Khokhar, K.B.; Thiyagarajah, A.; Middeldorp, M.E.; Nalliah, C.J.; et al. Subclinical device-detected atrial fibrillation and stroke risk: A systematic review and meta-analysis. Eur. Heart J. 2018, 39, 1407–1415. [Google Scholar] [CrossRef] [PubMed]
- Proietti, R.; Labos, C.; AlTurki, A.; Essebag, V.; Glotzer, T.V.; Verma, A. Asymptomatic atrial fibrillation burden and thromboembolic events: Piecing evidence together. Expert Rev. Cardiovasc. Ther. 2016, 14, 761–769. [Google Scholar] [CrossRef] [PubMed]
- Van Gelder, I.C.; Healey, J.S.; Crijns, H.J.G.M.; Wang, J.; Hohnloser, S.H.; Gold, M.R.; Capucci, A.; Lau, C.-P.; Morillo, C.A.; Hobbelt, A.H.; et al. Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur. Heart J. 2017, 38, 1339–1344. [Google Scholar] [CrossRef]
- Al-Khatib, S.M.; Thomas, L.; Wallentin, L.; Lopes, R.D.; Gersh, B.; Garcia, D.; Ezekowitz, J.; Alings, M.; Yang, H.; Alexander, J.H.; et al. Outcomes of apixaban vs. warfarin by type and duration of atrial fibrillation: Results from the ARISTOTLE trial. Eur. Heart J. 2013, 34, 2464–2471. [Google Scholar] [CrossRef]
- Steinberg, B.A.; Hellkamp, A.S.; Lokhnygina, Y.; Patel, M.R.; Breithardt, G.; Hankey, G.J.; Becker, R.C.; Singer, D.E.; Halperin, J.L.; Hacke, W.; et al. Investigator. Higher risk of death and stroke in patients with persistent vs. paroxysmal atrial fibrillation: Results from the ROCKET-AF Trial. Eur. Heart J. 2015, 36, 288–296. [Google Scholar] [CrossRef]
- De Vos, C.B.; Pisters, R.; Nieuwlaat, R.; Prins, M.H.; Tieleman, R.G.; Coelen, R.J.; van den Heijkant, A.C.; Allessie, M.A.; Crijns, H.J. Progression from paroxysmal to persistent atrial fibrillation clinical correlates and prognosis. J. Am. Coll. Cardiol. 2010, 55, 725–731. [Google Scholar] [CrossRef]
- Barrett, T.W.; Self, W.H.; Wasserman, B.S.; McNaughton, C.D.; Darbar, D. Evaluating the HATCH score for predicting progression to sustained atrial fibrillation in ED patients with new atrial fibrillation. Am. J. Emerg. Med. 2013, 31, 792–797. [Google Scholar] [CrossRef] [PubMed]
- Proietti, R.; Hadjis, A.; AlTurki, A.; Thanassoulis, G.; Roux, J.F.; Verma, A.; Healey, J.S.; Bernier, M.L.; Birnie, D.; Nattel, S.; et al. A Systematic Review on the Progression of Paroxysmal to Persistent Atrial Fibrillation: Shedding New Light on the Effects of Catheter Ablation. JACC Clin. Electrophysiol. 2015, 1, 105–115. [Google Scholar] [CrossRef]
- Boriani, G.; Glotzer, T.V.; Ziegler, P.D.; De Melis, M.; di Mangoni, S.S.L.; Sepsi, M.; Landolina, M.; Lunati, M.; Lewalter, T.; Camm, A.J. Detection of new atrial fibrillation in patients with cardiac implanted electronic devices and factors associated with transition to higher device-detected atrial fibrillation burden. Heart Rhythm 2018, 15, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.A.; Conen, D.; Van Gelder, I.C.; McIntyre, W.F.; Crijns, H.J.; Wang, J.; Gold, M.R.; Hohnloser, S.H.; Lau, C.P.; Capucci, A.; et al. Progression of Device-Detected Subclinical Atrial Fibrillation and the Risk of Heart Failure. J. Am. Coll. Cardiol. 2018, 71, 2603–2611. [Google Scholar] [CrossRef] [PubMed]
- Glotzer, T.V. The Cacophony of Silent Atrial Fibrillation. J. Am. Coll. Cardiol. 2018, 71, 2612–2615. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, A.; Butcher, K.S.; Buck, B.H. The Multiple Causes of Stroke in Atrial Fibrillation: Thinking Broadly. Can. J. Cardiol. 2018, 34, 1503–1511. [Google Scholar] [CrossRef] [PubMed]
- Kamel, H.; Okin, P.M.; Elkind, M.S.V.; Iadecola, C. Atrial Fibrillation and Mechanisms of Stroke: Time for a New Model. Stroke 2016, 47, 895–900. [Google Scholar] [CrossRef]
- Brambatti, M.; Connolly, S.J.; Gold, M.R.; Morillo, C.A.; Capucci, A.; Muto, C.; Lau, C.P.; Gelder, I.C.V.; Hohnloser, S.H.; Carlson, M.; et al. Temporal Relationship Between Subclinical Atrial Fibrillation and Embolic Events. Circulation 2014, 129, 2094–2099. [Google Scholar] [CrossRef]
- Daoud, E.G.; Glotzer, T.V.; Wyse, D.G.; Ezekowitz, M.D.; Hilker, C.; Koehler, J.; Ziegler, P.D. Temporal relationship of atrial tachyarrhythmias, cerebrovascular events, and systemic emboli based on stored device data: A subgroup analysis of TRENDS. Heart Rhythm 2011, 8, 1416–1423. [Google Scholar] [CrossRef]
- Hirsh, B.J.; Copeland-Halperin, R.S.; Halperin, J.L. Fibrotic Atrial Cardiomyopathy Atrial, Fibrillation, and Thromboembolism: Mechanistic Links and Clinical Inferences. J. Am. Coll. Cardiol. 2015, 65, 2239–2251. [Google Scholar] [CrossRef]
- Klein, A.L.; Grimm, R.A.; Murray, R.D.; Apperson-Hansen, C.; Asinger, R.W.; Black, I.W.; Davidoff, R.; Erbel, R.; Halperin, J.L.; Orsinelli, D.A.; et al. Use of Transesophageal Echocardiography to Guide Cardioversion in Patients with Atrial Fibrillation. N. Engl. J. Med. 2001, 344, 1411–1420. [Google Scholar] [CrossRef] [PubMed]
- Macle, L.; Cairns, J.A.; Andrade, J.G.; Mitchell, L.B.; Nattel, S.; Verma, A.; Verma, A.; Macle, L.; Andrade, J.; Atzema, C.; et al. The 2014 Atrial Fibrillation Guidelines Companion: A Practical Approach to the Use of the Canadian Cardiovascular Society Guidelines. Can. J. Cardiol. 2015, 31, 1207–1218. [Google Scholar] [CrossRef] [PubMed]
- Healey, J.S.; Martin, J.L.; Duncan, A.; Connolly, S.J.; Ha, A.H.; Morillo, C.A.; Nair, G.M.; Eikelboom, J.; Divakaramenon, S.; Dokainish, H. Pacemaker-Detected Atrial Fibrillation in Patients with Pacemakers: Prevalence, Predictors, and Current Use of Oral Anticoagulation. Can. J. Cardiol. 2013, 29, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.T.; Bersohn, M.M.; Waldo, A.L.; Wathen, M.S.; Choucair, W.K.; Lip, G.Y.H.; Ip, J.; Holcomb, R.; Akar, J.G.; Halperin, J.L.; et al. Randomized trial of atrial arrhythmia monitoring to guide anticoagulation in patients with implanted defibrillator and cardiac resynchronization devices. Eur. Heart J. 2015, 36, 1660–1668. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Blank, B.F.; Calvert, M.; Camm, A.J.; Chlouverakis, G.; Diener, H.-C.; Goette, A.; Huening, A.; Lip, G.Y.H.; Simantirakis, E.; et al. Probing oral anticoagulation in patients with atrial high rate episodes: Rationale and design of the Non-Vitamin K antagonist Oral anticoagulants in patients with Atrial High rate episodes (NOAH–AFNET 6) trial. Am. Heart J. 2017, 190, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Vinereanu, D.; Lopes, R.D.; Bahit, M.C.; Xavier, D.; Jiang, J.; Al-Khalidi, H.R.; He, W.; Xian, Y.; Ciobanu, A.O.; Kamath, D.Y. A multifaceted intervention to improve treatment with oral anticoagulants in atrial fibrillation (IMPACT-AF): an international, cluster-randomised trial. The Lancet 2017, 390, 1737–1746.8. [Google Scholar] [CrossRef]
- Charitos, E.I.; Pürerfellner, H.; Glotzer, T.V.; Ziegler, P.D. Clinical Classifications of Atrial Fibrillation Poorly Reflect Its Temporal Persistence: Insights from 1195 Patients Continuously Monitored with Implantable Devices. J. Am. Coll. Cardiol. 2014, 63, 2840–2848. [Google Scholar] [CrossRef] [PubMed]
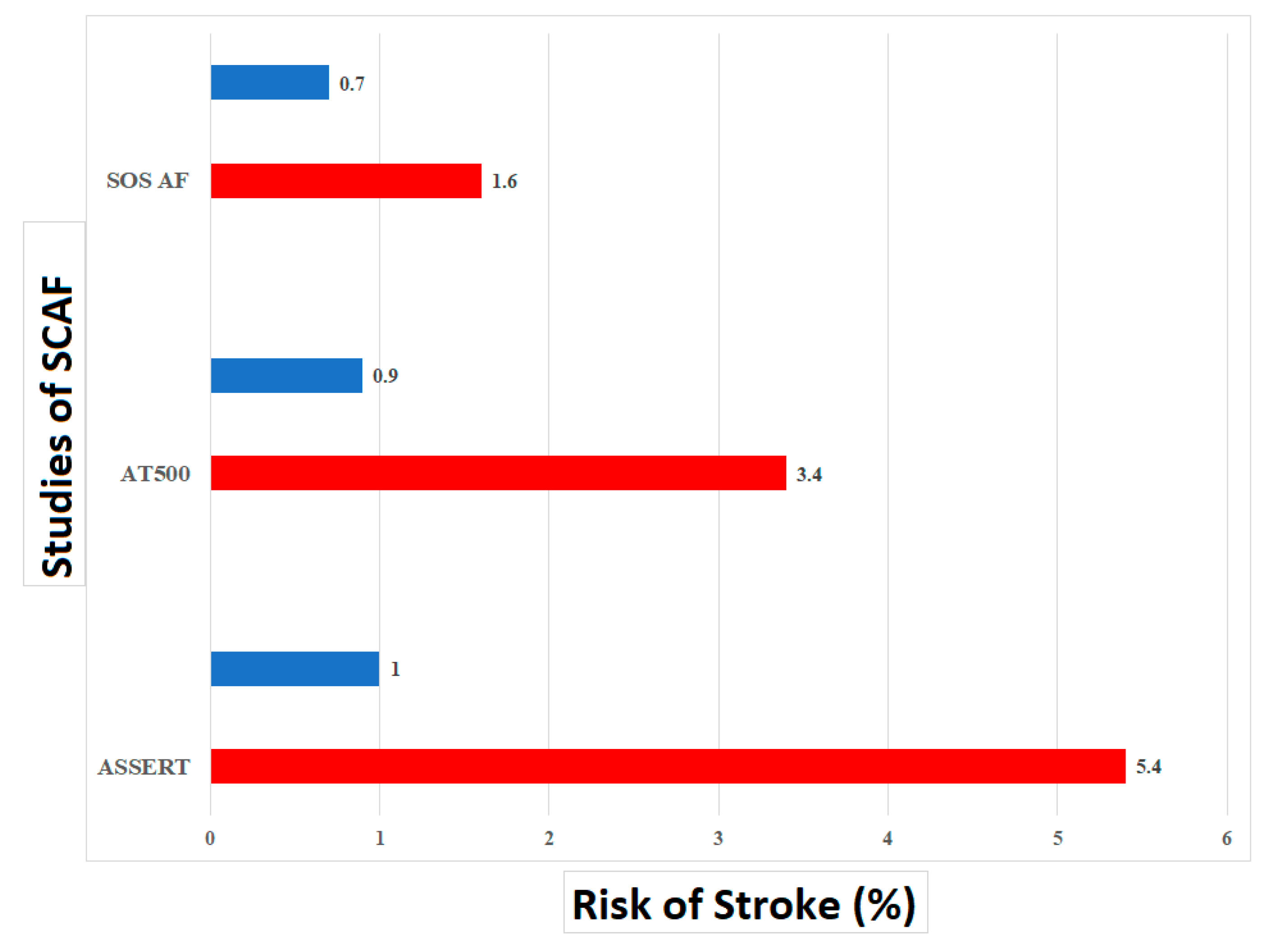
| Study (First Author, Year) | Study Population | Design | Mode of SCAF Detection | SCAF Criteria + Burden | Clinical Outcome | Annual Stroke and Systemic Embolism Event Rate (%) | Comparative Outcomes (HR, 95% CI) | F/u | Incidence of SCAF (%) |
|---|---|---|---|---|---|---|---|---|---|
| ASSERT (Healey et al., 2013) [1] | 2580 patients Inclusion criteria:
| Prospective cohort study | Dual chamber pacemaker or defibrillator | >190 bpm + ≥6 min | Stroke or systemic embolism | SCAF = 1.69 No SCAF = 0.69 | 5.56, 1.28–4.85 | 2.5 years | 10.1 |
| ASSERT II (Healey et al., 2017) [21] | 256 patients Inclusion criteria:
| Prospective cohort study | CONFIRM AF subcutaneous cardiac monitor | + ≥6 min | NA | 6 events occurred (4 stroke, 1 TIA and 1 systemic embolism) but none in patients who had SCAF detected | NA | 16 months | 34.4 |
| AT 500 registry (Capucci et al., 2005) [18] | 225 patients Inclusion criteria:
| Prospective cohort study | Dual chamber pacemaker | NA + 24 h | Stroke or systemic embolism | NA | 3.10, 1.10–10.50 | 22 months | NA |
| MOST (Glotzer et al., 2003) [16] | 312 patients Inclusion criteria:
| Prospective cohort study | Dual chamber pacemaker | >220 bpm + ≥5 min | Stroke and all-cause mortality | SCAF = 1.82 No SCAF = 0.48 | 2.79, 1.51–5.15 | 33 months | 51.3 |
| HOME CARE and EVEREST (Shanmugam et al., 2011) [19] | 560 patients All patients had heart failure and a biventricular pacemaker capable of continuous heart rhythm monitoring though home monitoring. Patients in sinus rhythm (including patients with a prior history of AF) with >70% home monitored transmissions during follow up (minimum >3 months follow-up) | Prospective cohort study | Biventricular pacemaker or defibrillator | >180 bpm + ≥3.8 h | Stroke or systemic embolism | NA | 9.40, 1.80–47.00 | 12 months | 40 |
| SOS-AF (Boriani et al., 2014) [17] | 10,016 patients Inclusion: CIED able to monitor for atrial high rate episodes At least 3 months of follow-up Device diagnostic data available Did not have permanent AF | Prospective cohort study | CIED | >175 bpm + ≥5 min | Stroke | SCAF = 0.49 No SCAF = 0.31 | 1.76, 1.02–3.02 | 24 months | 43 |
| TRENDS (Glotzer et al., 2009) [15] | 2486 patients Inclusion criteria:
| Prospective cohort study | CIED | >175 bpm + ≥5.6 h | Stroke or systemic embolism | SCAF = 2.4 No SCAF = 1.1 | 2.20, 0.96–5.05 | 1.4 years | 55.9 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlTurki, A.; Marafi, M.; Russo, V.; Proietti, R.; Essebag, V. Subclinical Atrial Fibrillation and Risk of Stroke: Past, Present and Future. Medicina 2019, 55, 611. https://doi.org/10.3390/medicina55100611
AlTurki A, Marafi M, Russo V, Proietti R, Essebag V. Subclinical Atrial Fibrillation and Risk of Stroke: Past, Present and Future. Medicina. 2019; 55(10):611. https://doi.org/10.3390/medicina55100611
Chicago/Turabian StyleAlTurki, Ahmed, Mariam Marafi, Vincenzo Russo, Riccardo Proietti, and Vidal Essebag. 2019. "Subclinical Atrial Fibrillation and Risk of Stroke: Past, Present and Future" Medicina 55, no. 10: 611. https://doi.org/10.3390/medicina55100611
APA StyleAlTurki, A., Marafi, M., Russo, V., Proietti, R., & Essebag, V. (2019). Subclinical Atrial Fibrillation and Risk of Stroke: Past, Present and Future. Medicina, 55(10), 611. https://doi.org/10.3390/medicina55100611







