Endoscopic Sclerotherapy with a Large Volume of High Concentration of Cyanoacrylate for Jejunal Variceal Bleeding bys Single-Balloon Enteroscopy
Abstract
1. Introduction
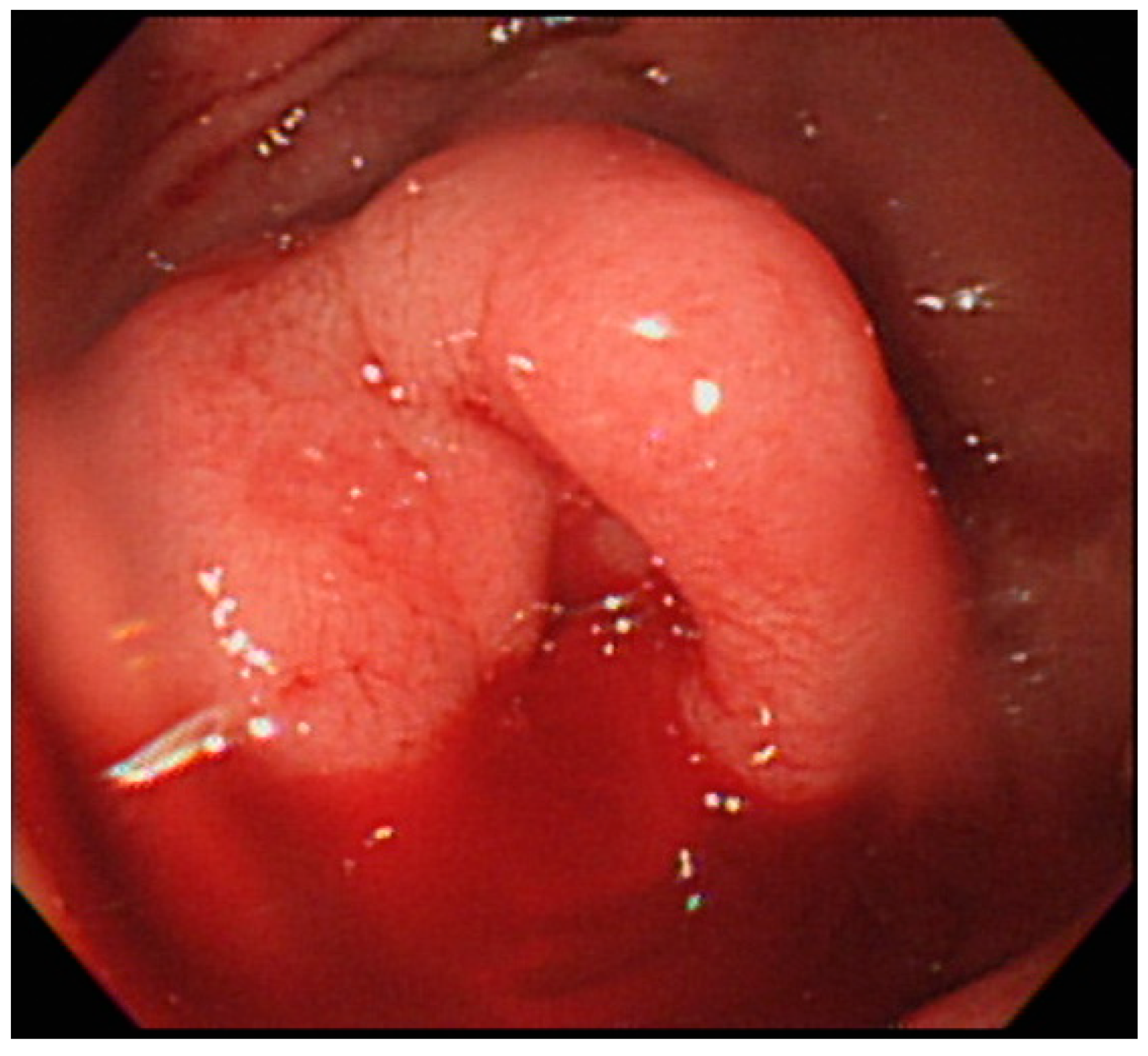
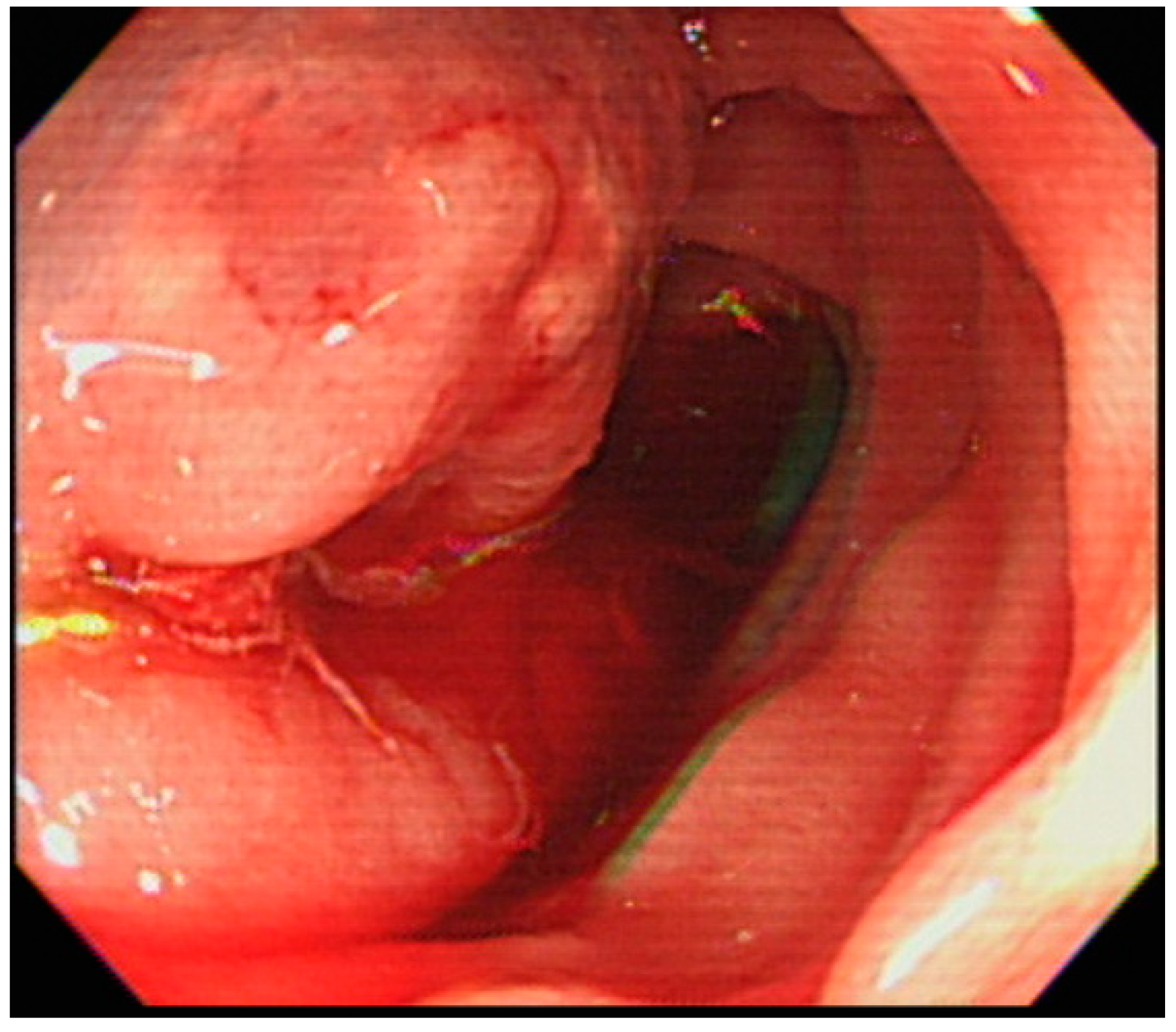
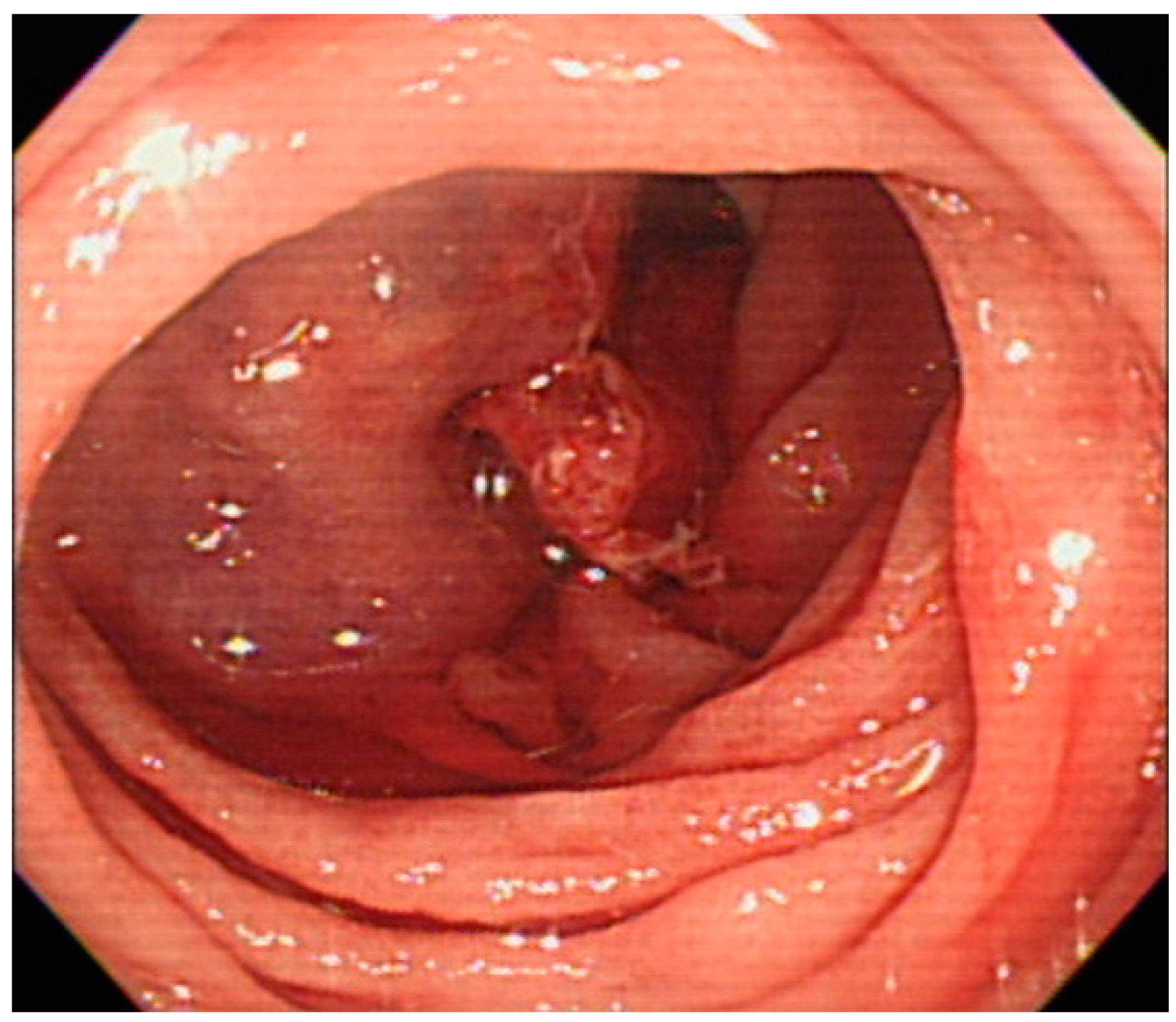
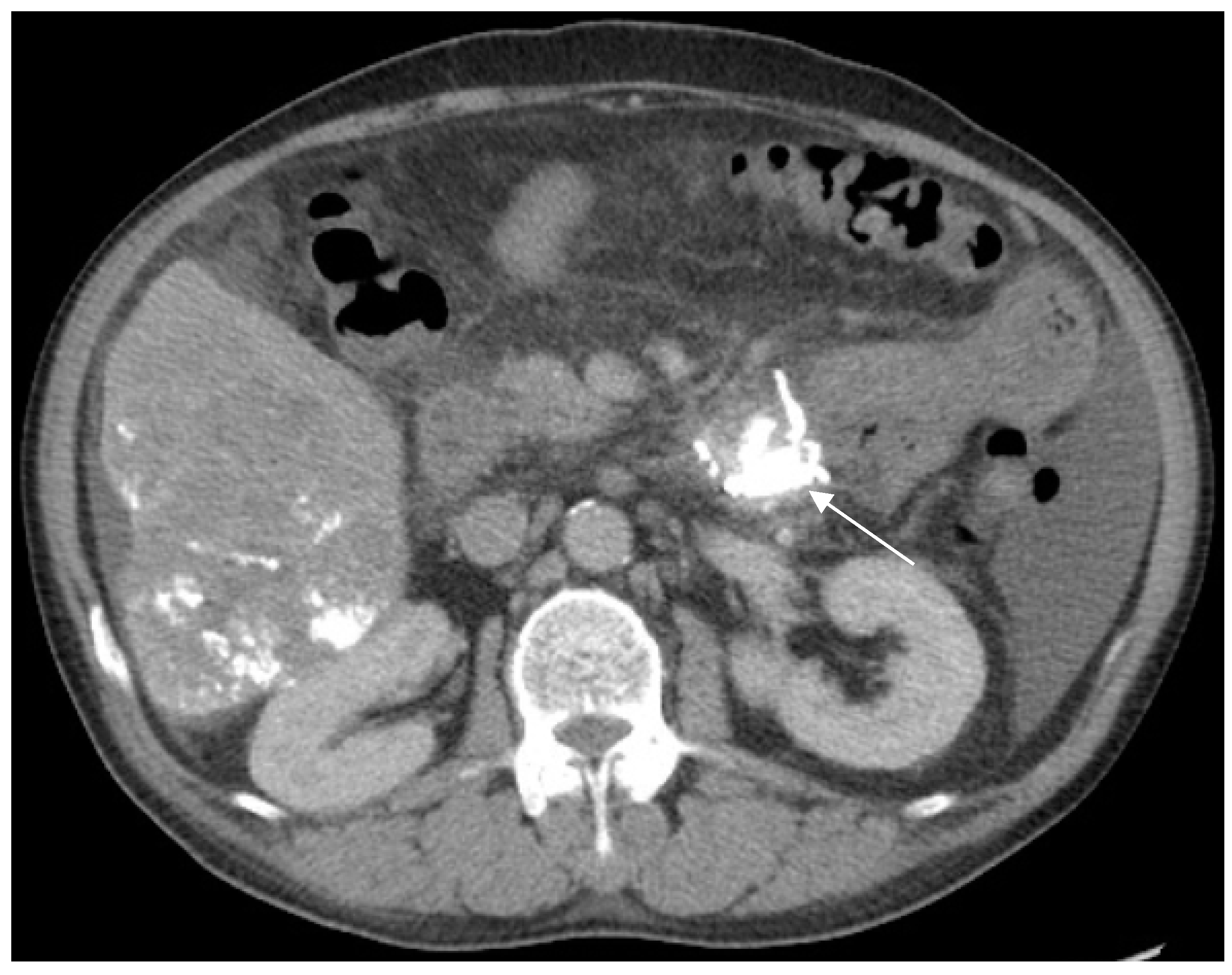
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lebrec, D.; Benhamou, J.P. Ectopic varices in portal hypertension. Clin. Gastroenterol. 1985, 14, 105–121. [Google Scholar] [PubMed]
- Watanabe, N.; Toyonaga, A.; Kojima, S.; Takashimizu, S.; Oho, K.; Kokubu, S.; Nakamura, K.; Hasumi, A.; Murashima, N.; Tajiri, T. Current status of ectopic varices in Japan: Results of a survey by the Japan Society for Portal Hypertension. Hepatol. Res. 2010, 40, 763–776. [Google Scholar] [CrossRef] [PubMed]
- Saad, W.E.; Lippert, A.; Saad, N.E.; Caldwell, S. Ectopic varices: Anatomical classification, hemodynamic classification, and hemodynamic-based management. Tech. Vasc. Interv. Radiol. 2013, 16, 158–175. [Google Scholar] [CrossRef] [PubMed]
- Norton, I.D.; Andrews, J.C.; Kamath, P.S. Management of ectopic varices. Hepatology 1998, 28, 1154–1158. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, S.; Sato, T.; Kimura, M. Endoscopic sclerotherapy with a high concentration of n-butyl-2-cyanoacrylate for anastomotic varices after choledochojejunostomy. Endoscopy 2015, 47 (Suppl. 1), E321–E322. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.B.; Choi, Y.H.; So, Y.H.; Ahn, D.W.; Jeong, J.B. Balloon-occluded retrograde transvenous obliteration of jejunal varices: A case report, therapeutic approach. Dig. Dis. Sci. 2016, 61, 948–951. [Google Scholar] [CrossRef] [PubMed]
- Mansoor, E.; Singh, A.; Nizialek, G.; Veloso, H.M.; Katz, J.; Cooper, G.S.; Isenberg, G. Massive gastrointestinal bleeding due to isolated jejunal varices in a patient with extrahepatic portal hypertension: A case report. Am. J. Gastroenterol. 2016, 111, 1209–1211. [Google Scholar] [CrossRef] [PubMed]
- Kastanakis, M.; Anyfantakis, D.; Katsougris, N.; Bobolakis, E. Massive gastrointestinal bleeding due to isolated jejunal varices in a patient without portal hypertension. Int. J. Surg. Case Rep. 2013, 4, 439–441. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.S.; Chen, K.C.; Chou, Y.H.; Chen, K.H. Emergent single-balloon enteroscopy for overt bleeding of small intestinal vascular malformation. World J. Gastroenterol. 2018, 24, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Park, C.W.; Kim, S.H.; Yang, H.W.; Lee, Y.J.; Jung, S.H.; Song, H.S.; Lee, S.O.; Kim, A.; Cha, S.W. A case of variceal bleeding from the jejunum in liver cirrhosis. Clin. Mol. Hepatol. 2013, 19, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.J.; Zanati, S.; Dubcenco, E.; Cirocco, M.; Christodoulou, D.; Kandel, G.; Haber, G.B.; Kortan, P.; Marcon, N.E. Diagnosis of small-bowel varices by capsule endoscopy. Gastrointest. Endosc. 2004, 60, 129–135. [Google Scholar] [CrossRef]
- Lin, M.C.; Chen, P.J.; Shih, Y.L.; Huang, H.H.; Chang, W.K.; Hsieh, T.Y.; Huang, T.Y. Outcome and safety of anterograde and retrograde single-balloon enteroscopy: Clinical experience at a tertiary medical center in Taiwan. PLoS ONE 2016, 11, e0161188. [Google Scholar] [CrossRef] [PubMed]
- Traina, M.; Tarantino, I.; Barresi, L.; Mocciaro, F. Variceal bleeding from ileum identified and treated by single balloon enteroscopy. World J. Gastroenterol. 2009, 15, 1904–1905. [Google Scholar] [CrossRef] [PubMed]
- Satapathy, S.K.; Sanyal, A.J. Nonendoscopic management strategies for acute esophagogastric variceal bleeding. Gastroenterol. Clin. N. Am. 2014, 43, 819–833. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.W.; Sohn, J.H.; Kim, T.Y.; Kim, J.Y.; Yhi, J.; Kwak, D.S.; Kim, H.S.; Song, S.Y. Long-term successful treatment of massive distal duodenal variceal bleeding with balloon-occluded retrograde transvenous obliteration. Korean J. Gastroenterol. 2014, 63, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Nakata, M.; Nakata, W.; Isoda, N.; Yoshizawa, M.; Sugimoto, H. Percutaneous retrograde sclerotherapy for refractory bleeding of jejunal varices: Direct injection via superficial epigastric vein. Cardiovasc. Interv. Radiol. 2012, 35, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.Y.; Lee, W.K.; Kim, Y.H.; Kwon, B.W.; Kang, M.S.; Kim, S.B.; Song, I.H. Ruptured duodenal varices arising from the main portal vein successfully treated with endoscopic injection sclerotherapy: A case report. Korean. J. Hepatol. 2011, 17, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.S.; Kim, H.H.; Park, S.H.; Kim, S.E.; Jung, J.I.; Ahn, B.Y.; Kim, S.H.; Chung, S.K.; Park, Y.H.; Choi, K.H. N-butyl-2-cyanoacrylate pulmonary embolism after endoscopic injection sclerotherapy for gastric variceal bleeding. J. Comput. Assist. Tomogr. 2001, 25, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Akahoshi, T.; Tanoue, K.; Tomikawa, M.; Hashizume, M.; Sugimachi, K. Rupture of jejunal varices treated by percutaneous transhepatic obliteration and endoscopic injection sclerotherapy with N-butyl-2-cyanoacrylate. Endoscopy 2001, 33, 998. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-H.; Wu, C.-S.; Huang, J.-H. Endoscopic Sclerotherapy with a Large Volume of High Concentration of Cyanoacrylate for Jejunal Variceal Bleeding bys Single-Balloon Enteroscopy. Medicina 2018, 54, 68. https://doi.org/10.3390/medicina54050068
Lee J-H, Wu C-S, Huang J-H. Endoscopic Sclerotherapy with a Large Volume of High Concentration of Cyanoacrylate for Jejunal Variceal Bleeding bys Single-Balloon Enteroscopy. Medicina. 2018; 54(5):68. https://doi.org/10.3390/medicina54050068
Chicago/Turabian StyleLee, Jyong-Hong, Chih-Sheng Wu, and Jen-Hsuan Huang. 2018. "Endoscopic Sclerotherapy with a Large Volume of High Concentration of Cyanoacrylate for Jejunal Variceal Bleeding bys Single-Balloon Enteroscopy" Medicina 54, no. 5: 68. https://doi.org/10.3390/medicina54050068
APA StyleLee, J.-H., Wu, C.-S., & Huang, J.-H. (2018). Endoscopic Sclerotherapy with a Large Volume of High Concentration of Cyanoacrylate for Jejunal Variceal Bleeding bys Single-Balloon Enteroscopy. Medicina, 54(5), 68. https://doi.org/10.3390/medicina54050068



