Neophobia—A Natural Developmental Stage or Feeding Difficulties for Children?
Abstract
1. Introduction
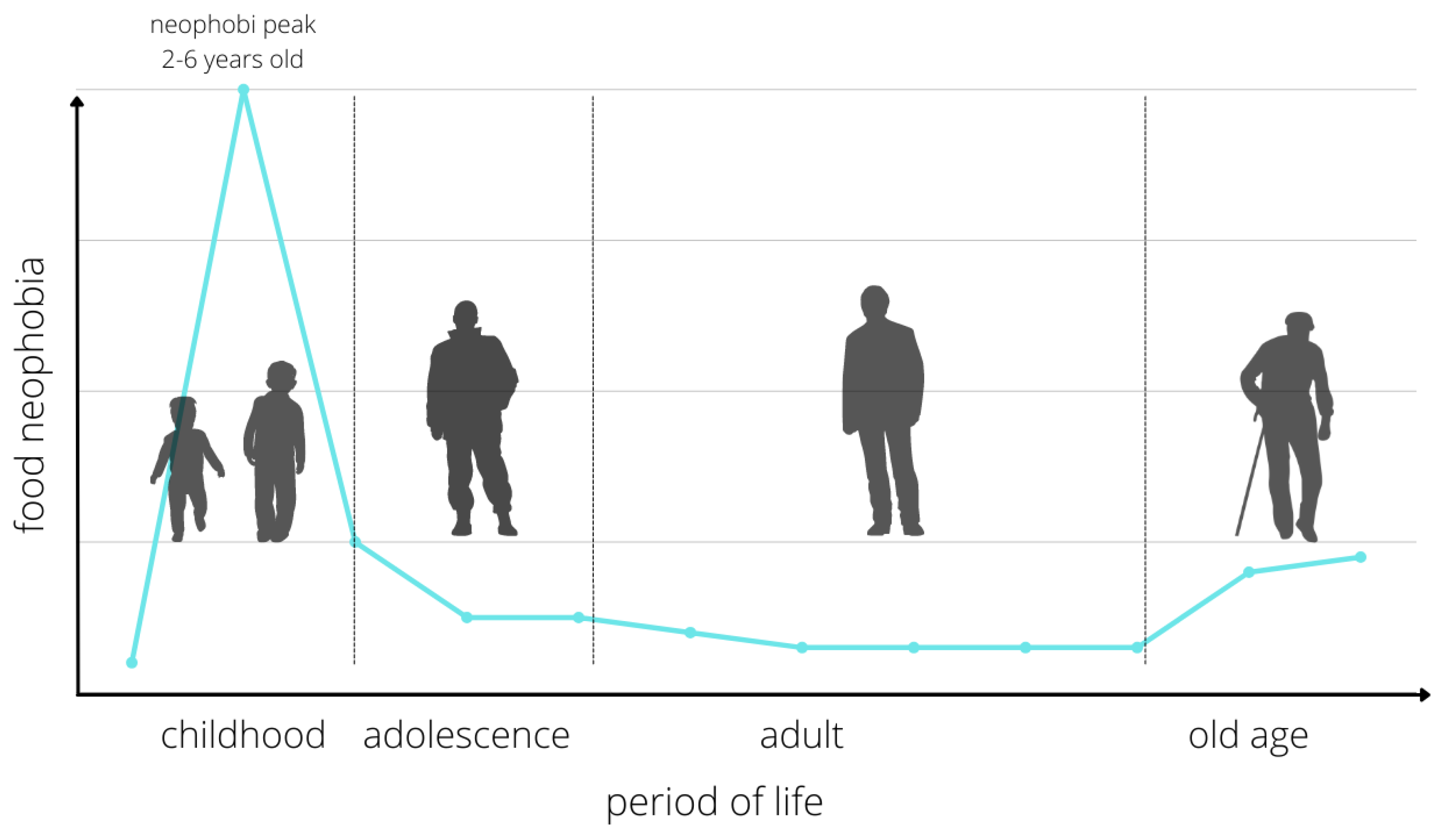
2. Epidemiology of Food Neophobia
3. Food Neophobia
4. Causes of Food Neophobia
5. Differential Diagnosis of Feeding Difficulties
6. Impact of Neophobia on Child Health
7. Management of Children with Nutritional Neophobia
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ramsay, M.; Martel, C.; Porporino, M.; Zygmuntowicz, C. The Montreal Children’s Hospital Feeding Scale: A brief bilingual screening tool for identifying feeding problems. Paediatr. Child Health 2011, 16, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Maiz, E.; Urkia-Susin, I.; Urdaneta, E.; Allirot, X. Child Involvement in Choosing a Recipe, Purchasing Ingredients, and Cooking at School Increases Willingness to Try New Foods and Reduces Food Neophobia. J. Nutr. Educ. Behav. 2021, 53, 279–289. [Google Scholar] [CrossRef] [PubMed]
- Marlow, C.S.; Forestell, C.A. The effect of parental food neophobia on children’s fruit and vegetable consumption: A serial mediation model. Appetite 2022, 172, 105942. [Google Scholar] [CrossRef] [PubMed]
- Goday, P.S.; Huh, S.Y.; Alan Silverman, A.; Lukens, C.T.; Dodrill, P.; Cohen, S.S.; Delaney, A.L.; Feuling, M.B.; Noel, R.J.; Gisel, E.; et al. Pediatric Feeding Disorder-Consensus Definition and Conceptual Framework. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Rommel, N.; De Meyer, A.-M.; Feenstra, L.; Veereman-Wauters, G. The Complexity of Feeding Problems in 700 Infants and Young Children Presenting to a Tertiary Care Institution. J. Pediatr. Gastroenterol. Nutr. 2003, 37, 75–84. [Google Scholar] [CrossRef]
- Anliker, J.A.; Bartoshuk, L.; Ferris, A.M.; Hooks, L.D. Children’s food preferences and genetic sensitivity to the bitter taste of 6-n propylthiouracil (PROP). Am. J. Clin. Nutr. 1991, 54, 316–320. [Google Scholar] [CrossRef]
- Field, D.; Garland, M.; Williams, K. Correlates of specific childhood feeding problems. J. Paediatr. Child Health 2003, 39, 299–304. [Google Scholar] [CrossRef]
- Palmer, M.M.; Heyman, M.B. Assessment and treatment of sensory- versus motor-based feeding problems in very young children. Infants Young Child. 1993, 6, 67–73. [Google Scholar] [CrossRef]
- Ramsay, M.; Gisel, E.G.; Boutry, M. Non-organic failure to thrive: Growth failure secondary to feeding-skills disorder. Dev. Med. Child Neurol. 1993, 35, 285–297. [Google Scholar] [CrossRef]
- Tannenbaum, G.S.; Ramsay, M.; Martel, C.; Samia, M.; Zygmuntowicz, C.; Porporino, M.; Ghosh, S. Elevated Circulating Acylated and Total Ghrelin Concentrations Along With Reduced Appetite Scores in Infants With Failure to Thrive. Pediatr. Res. 2009, 65, 569–573. [Google Scholar] [CrossRef]
- Wright, C.M.; Parkinson, K.N.; Drewett, R.F. How Does Maternal and Child Feeding Behavior Relate to Weight Gain and Failure to Thrive? Data from a Prospective Birth Cohort. Pediatrics 2006, 117, 1262–1269. [Google Scholar] [CrossRef] [PubMed]
- Green, R.J.; Samy, G.; Saleh Miqdady, M.; Salah, M.; Sleiman, R.; Abdelrahman, H.M.A.; Al Haddad, F.; Reda, M.M.; Lewis, H.; Ekanem, E.E. How to Improve Eating Behaviour during Early Childhood. Pediatr. Gastroenterol. Hepatol. Nutr. 2015, 18, 1–9. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Faith, M.S.; Heo, M.; Keller, K.L.; Pietrobelli, A. Child food neophobia is heritable, associated with less compliant eating, and moderates familial resemblance for BMI. Obesity 2013, 21, 1650–1655. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, E.E.; Roefs, A.; Kremers, S.P.J.; Jansen, A.; Gubbels, J.S.; Sleddens, E.F.C.; Thijs, C. Picky eating and child weight status development: A longitudinal study. J. Hum. Nutr. Diet. 2015, 29, 298–307. [Google Scholar] [CrossRef]
- Johnson, S.L.; Davies, P.L.; Boles, R.E.; Gavin, W.J.; Bellows, L.L. Young children’s food neophobia characteristics and sensory behaviors are related to their food intake. J. Nutr. 2015, 145, 2610–2616. [Google Scholar] [CrossRef]
- Kozioł-Kozakowska, A.; Jagielski, P.; Schlegel-Zawadzka, M. Nutritional neophobia and nutritional status in preschool children. Endokrynol. Otył. Zab. Przem. Mat. 2011, 2, 89. [Google Scholar]
- Kozioł-Kozakowska, A.; Piórecka, B. Food neophobia its determinants and health consequences. Stand. Med. Pediatr. 2013, 1–6. [Google Scholar]
- Cooke, L.J.; Haworth, C.M.A.; Wardle, J. Genetic and environmental influences on children’s food neophobia. Am. J. Clin. Nutr. 2007, 86, 428–433. [Google Scholar] [CrossRef]
- Emmett, P.M.; Hays, N.; Taylor, C.M. Antecedents of picky eating behaviour in young children. Appetite 2018, 130, 163–173. [Google Scholar] [CrossRef]
- Guzek, D.; Nguyen, D.; Głąbska, D. Food Neophobia and Consumer Choices within Vietnamese Menu in a Polish Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 2925. [Google Scholar] [CrossRef]
- Patel, M.D.; Donovan, S.M.; Lee, S.-Y. Considering Nature and Nurture in the Etiology and Prevention of Picky Eating: A Narrative Review. Nutrients 2020, 12, 3409. [Google Scholar] [CrossRef] [PubMed]
- Kerzner, B.; Milano, K.; MacLean, W.C.; Berall, G.; Stuart, S.; Chatoor, I. A Practical Approach to Classifying and Managing Feeding Difficulties. Pediatrics 2015, 135, 344–353. [Google Scholar] [CrossRef] [PubMed]
- Chatoor, I. Eating Disorders in Infancy and Early Childhood. The Oxford Handbook of Child and Adolescent Eating Disorders: Developmental Perspectives. Available online: https://www.oxfordhandbooks.com/view/10.1093/oxfordhb/9780199744459.001.0001/oxfordhb-9780199744459-e-012 (accessed on 1 March 2022).
- Demattè, M.L.; Endrizzi, I.; Biasioli, F.; Corollaro, M.L.; Pojer, N.; Zampini, M.; Aprea, E.; Gasperi, F. Food neophobia and its relation with olfactory ability in common odour identification. Appetite 2013, 68, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Cooke, L. Genetic and environmental determinants of children’s food preferences. Br. J. Nutr. 2008, 99, S15–S21. [Google Scholar] [CrossRef] [PubMed]
- Feeney, E.; O’Brien, S.; Scannell, A.; Markey, A.; Gibney, E.R. Genetic variation in taste perception: Does it have a role in healthy eating? Proc. Nutr. Soc. 2011, 70, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Knaapila, A.; Silventoinen, K.; Broms, U.; Rose, R.J.; Perola, M.; Kaprio, J.; Tuorila, H.M. Food Neophobia in Young Adults: Genetic Architecture and Relation to Personality, Pleasantness and Use Frequency of Foods, and Body Mass Index—A Twin Study. Behav. Genet. 2010, 41, 512–521. [Google Scholar] [CrossRef]
- Scaglioni, S.; De Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors Influencing Children’s Eating Behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef]
- Tuorila, H.; Hartmann, C. Consumer responses to novel and unfamiliar foods. Curr. Opin. Food Sci. 2019, 33, 1–8. [Google Scholar] [CrossRef]
- Jezewska-Zychowicz, M.; Plichta, M.; Drywień, M.; Hamulka, J. Food Neophobia among Adults: Differences in Dietary Patterns, Food Choice Motives, and Food Labels Reading in Poles. Nutrients 2021, 13, 1590. [Google Scholar] [CrossRef]
- Spahn, J.M.; Callahan, E.H.; Spill, M.K.; Wong, Y.P.; Benjamin-Neelon, S.E.; Birch, L.; Black, M.M.; Cook, J.T.; Faith, M.S.; Mennella, J.A.; et al. Influence of maternal diet on flavor transfer to amniotic fluid and breast milk and children’s responses: A systematic review. Am. J. Clin. Nutr. 2019, 109, 1003S–1026S. [Google Scholar] [CrossRef]
- Drewnowski, A. Taste preferences and food intake. Annu. Rev. Nutr. 1997, 17, 237–253. [Google Scholar] [CrossRef]
- Nicklaus, S.; Issanchou, S. Understanding Consumers of Food Products. In Children and Food Choice; Elsevier: Amsterdam, The Netherlands, 2007; pp. 329–358. [Google Scholar]
- Werthmann, J.; Jansen, A.; Havermans, R.; Nederkoorn, C.; Kremers, S.; Roefs, A. Bits and pieces. Food texture influences food acceptance in young children. Appetite 2015, 84, 181–187. [Google Scholar] [CrossRef]
- Cappellotto, M.; Olsen, A. Food Texture Acceptance, Sensory Sensitivity, and Food Neophobia in Children and Their Parents. Foods 2021, 10, 2327. [Google Scholar] [CrossRef] [PubMed]
- Frank, R.A.; Raudenbush, B. Individual differences in approach to novelty: The case of human food neophobia. In Viewing Psychology as a Whole: The Integrative Science of William N. Dember; American Psychological Association: Washington, DC, USA, 2004; pp. 227–245. [Google Scholar] [CrossRef]
- Benton, D. Role of parents in the determination of the food preferences of children and the development of obesity. Int. J. Obes. 2004, 28, 858–869. [Google Scholar] [CrossRef] [PubMed]
- Howard, A.J.; Mallan, K.; Byrne, R.; Magarey, A.; Daniels, L. Toddlers’ food preferences. The impact of novel food exposure, maternal preferences and food neophobia. Appetite 2012, 59, 818–825. [Google Scholar] [CrossRef] [PubMed]
- Capiola, A.; Raudenbush, B. The Effects of Food Neophobia and Food Neophilia on Diet and Metabolic Processing. Food Nutr. Sci. 2012, 3, 1397–1403. [Google Scholar] [CrossRef]
- An, M.; Zhou, Q.; Younger, K.M.; Liu, X.; Kearney, J.M. Are Maternal Feeding Practices and Mealtime Emotions Associated with Toddlers’ Food Neophobia? A Follow-Up to the DIT-Coombe Hospital Birth Cohort in Ireland. Int. J. Environ. Res. Public Health 2020, 17, 8401. [Google Scholar] [CrossRef]
- De Oliveira Torresa, T.; Gomes, D.R.; Mattosa, M.P. Factors associated with food neophobia in children: Systematic review. Rev. Paul Pediatr. 2021, 39, e2020089. [Google Scholar] [CrossRef]
- Bąbik, K.; Dziechciarz, P.; Horvath, A.; Ostaszewski, P. The Polish version of the Montreal Children’s Hospital Feeding Scale (MCH-FS): Translation, cross-cultural adaptation, and validation. Pediatr. Pol. 2019, 94, 299–305. [Google Scholar] [CrossRef]
- Pliner, P.; Hobden, K.L. Development of a scale to measure the trait of food neophobia in humans. Appetite 1992, 19, 105–120. [Google Scholar] [CrossRef]
- Loewen, R.; Pliner, P. The food situations questionnaire: A measure of children’s willingness to try novel foods in stimulating and non-stimulating situations. Appetite 2000, 35, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Damsbo-Svendsen, M.; Frøst, M.; Olsen, A. Development of novel tools to measure food neophobia in children. Appetite 2017, 113, 255–263. [Google Scholar] [CrossRef]
- Cooke, L.; Wardle, J.; Gibson, L. Relationship between parental report of food neophobia and everyday food consumption in 2–6-year-old children. Appetite 2003, 41, 205–206. [Google Scholar] [CrossRef]
- Falciglia, G.A.; Couch, S.C.; Gribble, L.S.; Pabst, S.M.; Frank, R. Food Neophobia in Childhood Affects Dietary Variety. J. Am. Diet. Assoc. 2000, 100, 1474–1481. [Google Scholar] [CrossRef]
- Pliner, P. Development of Measures of Food Neophobia in Children. Appetite 1994, 23, 147–163. [Google Scholar] [CrossRef] [PubMed]
- Flight, I.; Leppard, P.; Cox, D.N. Food neophobia and associations with cultural diversity and socio-economic status amongst rural and urban Australian adolescents. Appetite 2003, 41, 51–59. [Google Scholar] [CrossRef]
- Fraker, C.; Fishbein, M.; Walbert, L.; Cox, S. Food Chaining: The Proven 6-Step Plan to Stop Picky Eating, Solve Feeding Problems, and Expand Your Child’s Diet; Da Capo Press: Boston, MA, USA, 2007; 1p. [Google Scholar]
- Zucker, N.L.; LaVia, M.C.; Craske, M.G.; Foukal, M.; Harris, A.A.; Datta, N.; Savereide, E.; Maslow, G.R. Feeling and body investigators (FBI): ARFID division-Anacceptance-based interoceptive exposure treatment for children with ARFID. Int. J. Eat. Disord. 2018, 52, 466–472. [Google Scholar] [CrossRef]
- Białek-Dratwa, A.; Soczewka, M.; Grochowska-Niedworok, E. Introduction of complementary foods to infant diet using baby-led weaning. Pediatr. Med. Rodz. 2020, 16, 362–367. [Google Scholar] [CrossRef]
- Cunningham-Sabo, L.; Lohse, B. Cooking with KidsPositively Affects Fourth Graders’ Vegetable Preferences and Attitudes and Self-Efficacy for Food and Cooking. Child. Obes. 2013, 9, 549–556. [Google Scholar] [CrossRef]
- Ehrenberg, B.; Leone, L.A.; Sharpe, B.; Reardon, K.; Anzman-Frasca, S. Using repeated exposure through hands-on cooking to increase children’s preferences for fruits and vegetables. Appetite 2019, 142, 104347. [Google Scholar] [CrossRef]
- Cunningham-Sabo, L.; Lohse, B. Impact of a School-Based Cooking Curriculum for Fourth-Grade Students on Attitudes and Behaviors Is Influenced by Gender and Prior Cooking Experience. J. Nutr. Educ. Behav. 2014, 46, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Nicklaus, S.; Boggio, V.; Chabanet, C.; Issanchou, S. A prospective study of food variety seeking in childhood, adolescence and early adult life. Appetite 2005, 44, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Nixon, C.A.; Moore, H.J.; Douthwaite, W.; Gibson, E.L.; Vogele, C.; Kreichauf, S.; Wildgruber, A.; Manios, Y.; Summerbell, C.D.; ToyBox-study group. Identifying effective behavioural models and behaviour change strategies underpinning preschool- and school-based obesity prevention interventions aimed at 4-6-year-olds: A systematic review. Obes. Rev. 2012, 13, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Birch, L.L.; Fisher, J.O. Development of Eating Behaviors among Children and Adolescents. Pediatrics 1998, 101, 539–549. [Google Scholar] [CrossRef]
| Limited Appetite | Food Selectivity |
|---|---|
A misperceived problem:
| A misperceived problem:
|
Temperament:
| Mild food selectivity:
|
Organic causes
| Organic causes:
|
| Fear of Food/Feeding |
|---|
| Children with fear of feeding are usually those with food aversions or who have experienced unpleasant (e.g., choking) or painful (e.g., tube feeding) feeding situations. Anxiety may also accompany the first attempts to feed solids and is caused by inexperience, undeveloped psychomotor skills, and an unfamiliar situation. |
A misperceived problem:
|
Fear of feeding in infants:
|
Fear of feeding in older children:
|
Organic causes:
|
Feeding styles:
The most desirable feeding style is the responsive style. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Białek-Dratwa, A.; Szczepańska, E.; Szymańska, D.; Grajek, M.; Krupa-Kotara, K.; Kowalski, O. Neophobia—A Natural Developmental Stage or Feeding Difficulties for Children? Nutrients 2022, 14, 1521. https://doi.org/10.3390/nu14071521
Białek-Dratwa A, Szczepańska E, Szymańska D, Grajek M, Krupa-Kotara K, Kowalski O. Neophobia—A Natural Developmental Stage or Feeding Difficulties for Children? Nutrients. 2022; 14(7):1521. https://doi.org/10.3390/nu14071521
Chicago/Turabian StyleBiałek-Dratwa, Agnieszka, Elżbieta Szczepańska, Dorota Szymańska, Mateusz Grajek, Karolina Krupa-Kotara, and Oskar Kowalski. 2022. "Neophobia—A Natural Developmental Stage or Feeding Difficulties for Children?" Nutrients 14, no. 7: 1521. https://doi.org/10.3390/nu14071521
APA StyleBiałek-Dratwa, A., Szczepańska, E., Szymańska, D., Grajek, M., Krupa-Kotara, K., & Kowalski, O. (2022). Neophobia—A Natural Developmental Stage or Feeding Difficulties for Children? Nutrients, 14(7), 1521. https://doi.org/10.3390/nu14071521











