RETRACTED: Oral Administration of Myelin Oligodendrocyte Glycoprotein Attenuates Experimental Autoimmune Encephalomyelitis through Induction of Th2/Treg Cells and Suppression of Th1/Th17 Immune Responses
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. EAE Induction and Treatment
2.3. Histopathology
2.4. BrdU Proliferation Assay
2.5. Cytokine Assay
2.6. Quantitative Real-Time PCR
2.7. Statistical Analysis
2.8. Ethics Statement
3. Results
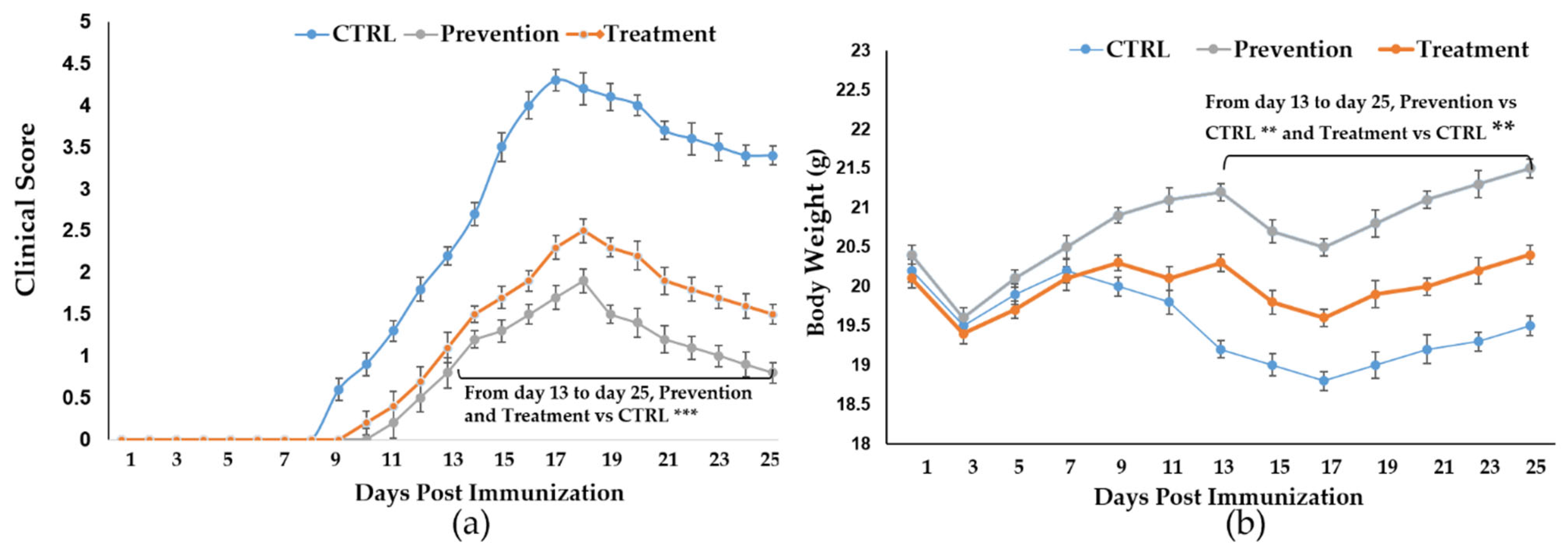
3.1. Oral Administration of MOG Inhibits the Development of EAE in C57BL/6 Mice
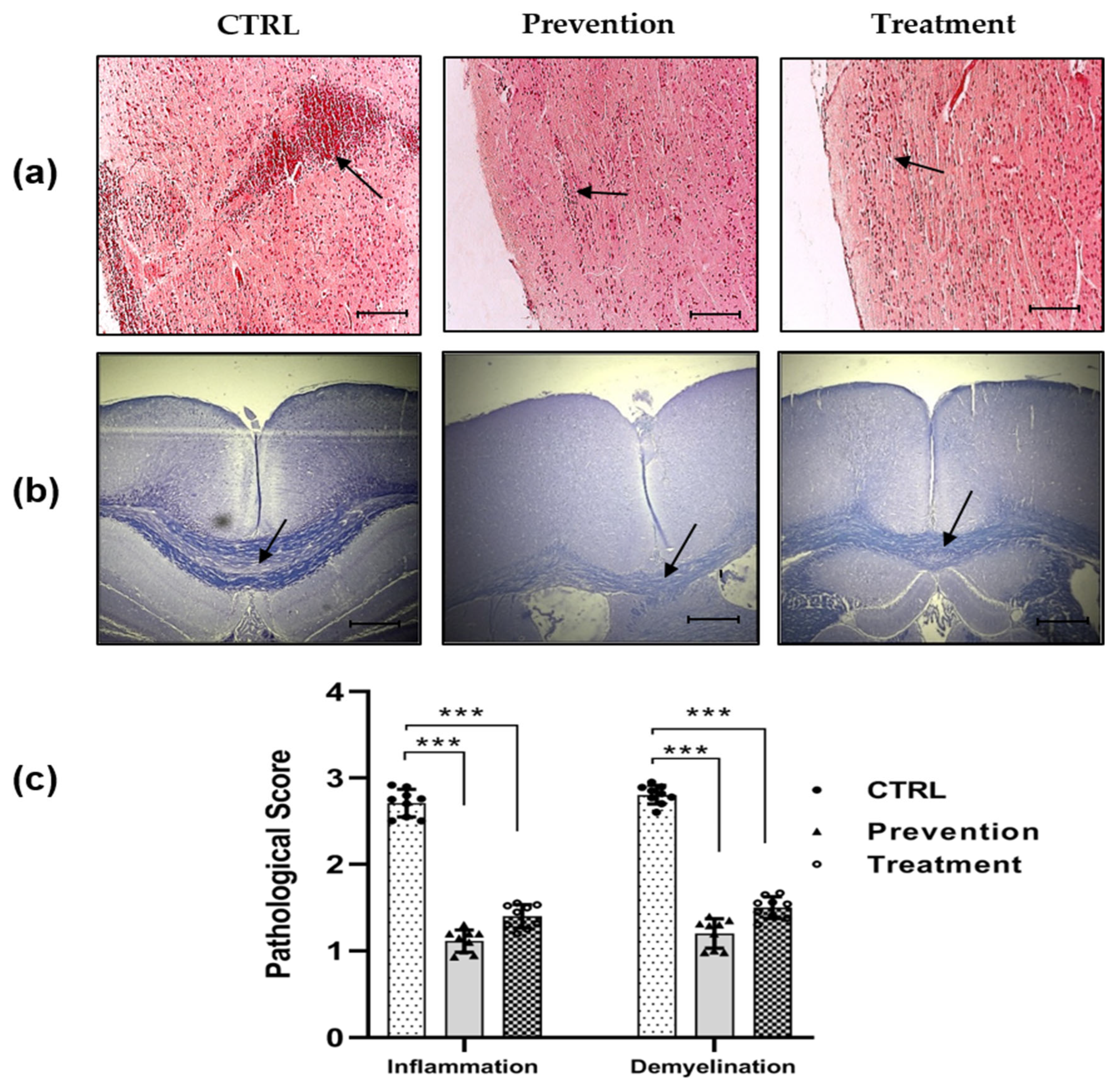
3.2. MOG Administration Ameliorates CNS Inflammation and Demyelination
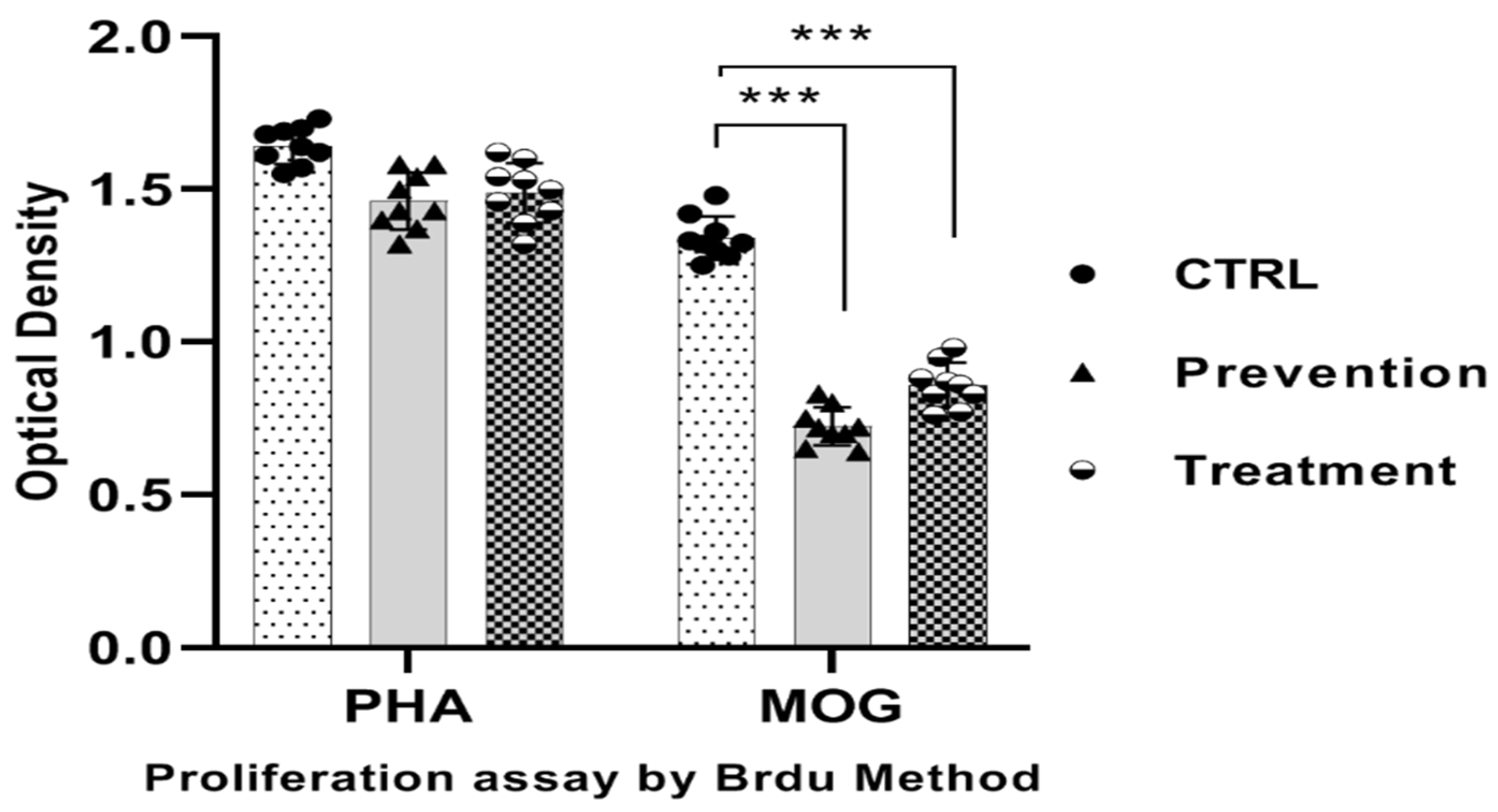
3.3. Oral Administration of MOG Suppresses T Cell Proliferation
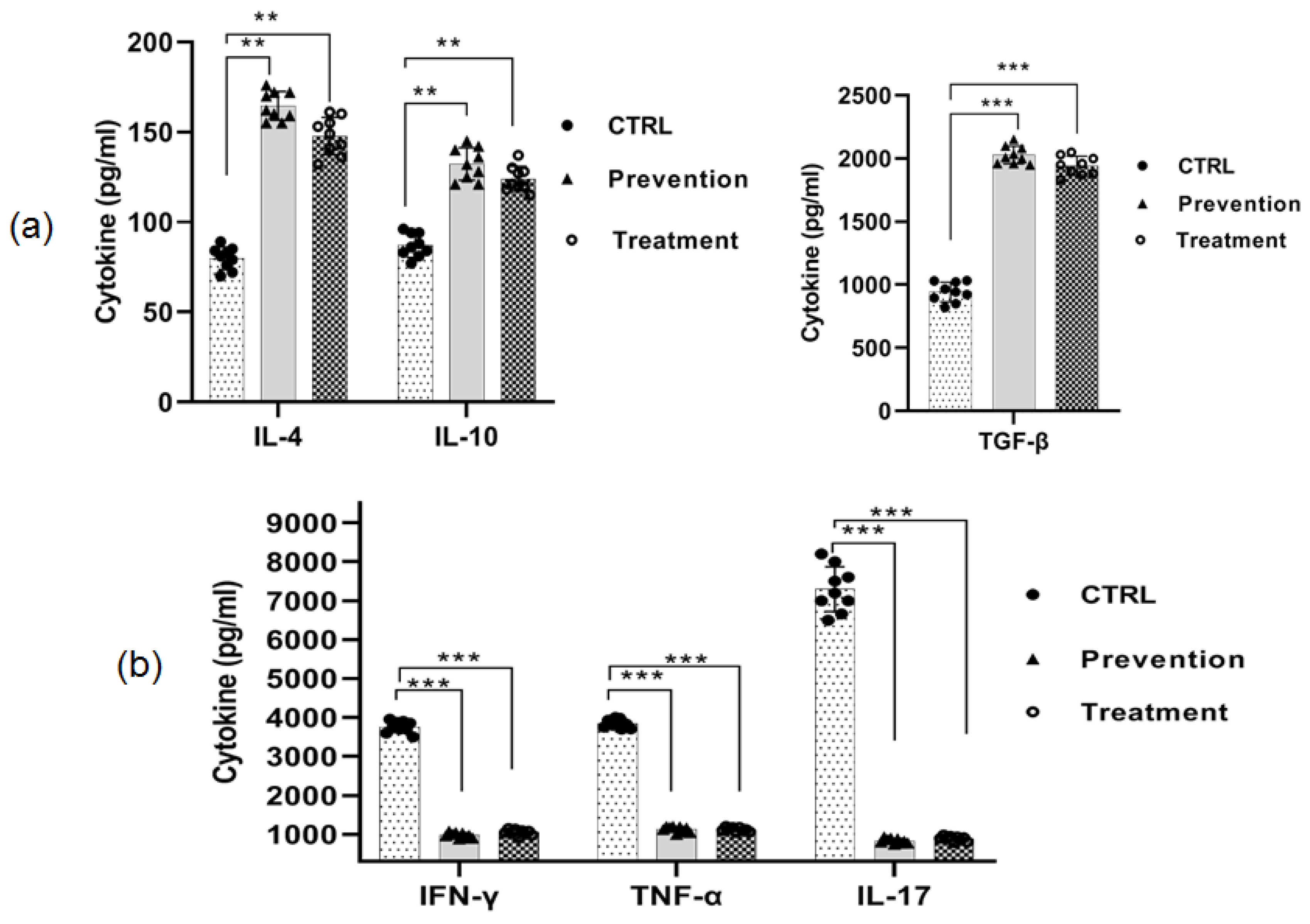
3.4. Administration of MOG Suppresses Pro-Inflammatory and Enhanced Anti-Inflammatory Cytokines
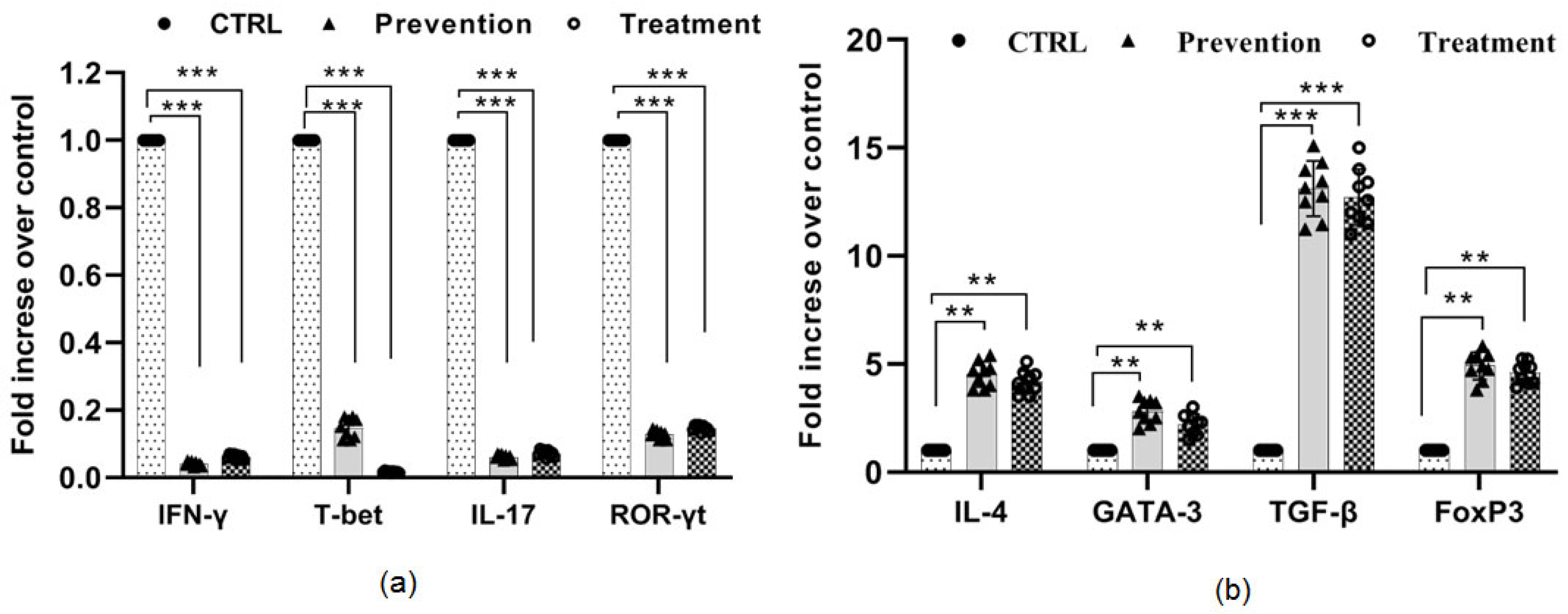
3.5. Administration of MOG Upregulated Expression of Cytokines and Transcription Factors in Th2 and Treg, and Downregulated in Th1 and Th17
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Walton, C.; King, R.; Rechtman, L.; Kaye, W.; Leray, E.; Marrie, R.A.; Robertson, N.; La Rocca, N.; Uitdehaag, B.; van der Mei, I. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS. Mult. Scler. J. 2020, 26, 1816–1821. [Google Scholar] [CrossRef] [PubMed]
- Azami, M.; YektaKooshali, M.H.; Shohani, M.; Khorshidi, A.; Mahmudi, L. Epidemiology of multiple sclerosis in Iran: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0214738. [Google Scholar]
- Ortiz, G.G.; Pacheco-Moisés, F.P.; Macías-Islas, M.Á.; Flores-Alvarado, L.J.; Mireles-Ramírez, M.A.; González-Renovato, E.D.; Hernández-Navarro, V.E.; Sánchez-López, A.L.; Alatorre-Jiménez, M.A. Role of the blood–brain barrier in multiple sclerosis. Arch. Med. Res. 2014, 45, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Frohman, E.M.; Racke, M.K.; Raine, C.S. Multiple sclerosis—The plaque and its pathogenesis. N. Engl. J. Med. 2006, 354, 942–955. [Google Scholar] [CrossRef]
- Hemmer, B.; Cepok, S.; Nessler, S.; Sommer, N. Pathogenesis of multiple sclerosis: An update on immunology. Curr. Opin. Neurol. 2002, 15, 227–231. [Google Scholar] [CrossRef]
- Kawachi, I.; Lassmann, H. Neurodegeneration in multiple sclerosis and neuromyelitis optica. J. Neurol. Neurosurg. Psychiatry 2017, 88, 137–145. [Google Scholar] [CrossRef]
- Baxter, A.G. The origin and application of experimental autoimmune encephalomyelitis. Nat. Rev. Immunol. 2007, 7, 904–912. [Google Scholar] [CrossRef]
- Bradl, M.; Lassmann, H. Oligodendrocytes: Biology and pathology. Acta Neuropathol. 2010, 119, 37–53. [Google Scholar] [CrossRef]
- Mosayebi, G.; Haghmorad, D.; Namaki, S.; Ghazavi, A.; Ekhtiari, P.; Mirshafiey, A. Therapeutic effect of EDTA in experimental model of multiple sclerosis. Immunopharmacol. Immunotoxicol. 2010, 32, 321–326. [Google Scholar] [CrossRef]
- Walczak, A.; Siger, M.; Ciach, A.; Szczepanik, M.; Selmaj, K. Transdermal application of myelin peptides in multiple sclerosis treatment. JAMA Neurol. 2013, 70, 1105–1109. [Google Scholar] [CrossRef]
- Sospedra, M.; Martin, R. Immunology of multiple sclerosis. Annu. Rev. Immunol. 2005, 23, 683–747. [Google Scholar] [CrossRef] [PubMed]
- Castro-Borrero, W.; Graves, D.; Frohman, T.C.; Flores, A.B.; Hardeman, P.; Logan, D.; Orchard, M.; Greenberg, B.; Frohman, E.M. Current and emerging therapies in multiple sclerosis: A systematic review. Ther. Adv. Neurol. Disord. 2012, 5, 205–220. [Google Scholar] [CrossRef] [PubMed]
- Zadeh, A.R.; Ghadimi, K.; Ataei, A.; Askari, M.; Sheikhinia, N.; Tavoosi, N.; Falahatian, M. Mechanism and adverse effects of multiple sclerosis drugs: A review article. Part 2. Int. J. Physiol. Pathophysiol. Pharmacol. 2019, 11, 105. [Google Scholar]
- Peron, J.P.S.; Yang, K.; Chen, M.-L.; Brandao, W.N.; Basso, A.S.; Commodaro, A.G.; Weiner, H.L.; Rizzo, L.V. Oral tolerance reduces Th17 cells as well as the overall inflammation in the central nervous system of EAE mice. J. Neuroimmunol. 2010, 227, 10–17. [Google Scholar] [CrossRef]
- Bynoe, M.S.; Evans, J.T.; Viret, C.; Janeway, C.A., Jr. Epicutaneous immunization with autoantigenic peptides induces T suppressor cells that prevent experimental allergic encephalomyelitis. Immunity 2003, 19, 317–328. [Google Scholar] [CrossRef]
- Peschl, P.; Bradl, M.; Höftberger, R.; Berger, T.; Reindl, M. Myelin oligodendrocyte glycoprotein: Deciphering a target in inflammatory demyelinating diseases. Front. Immunol. 2017, 8, 529. [Google Scholar] [CrossRef]
- Shimizu, K.; Agata, K.; Takasugi, S.; Goto, S.; Narita, Y.; Asai, T.; Magata, Y.; Oku, N. New strategy for MS treatment with autoantigen-modified liposomes and their therapeutic effect. J. Control. Release 2021, 335, 389–397. [Google Scholar] [CrossRef]
- Zorzella-Pezavento, S.F.G.; Mimura, L.A.N.; Fraga-Silva, T.F.C.; Ishikawa, L.L.W.; França, T.G.D.; Sartori, A. Experimental autoimmune encephalomyelitis is successfully controlled by epicutaneous administration of MOG plus vitamin D analog. Front. Immunol. 2017, 8, 1198. [Google Scholar] [CrossRef]
- Haghmorad, D.; Amini, A.A.; Mahmoudi, M.B.; Rastin, M.; Hosseini, M.; Mahmoudi, M. Pregnancy level of estrogen attenuates experimental autoimmune encephalomyelitis in both ovariectomized and pregnant C57BL/6 mice through expansion of Treg and Th2 cells. J. Neuroimmunol. 2014, 277, 85–95. [Google Scholar] [CrossRef]
- Soltanmohammadi, A.; Tavaf, M.J.; Zargarani, S.; Yazdanpanah, E.; Sadighi-Moghaddam, B.; Yousefi, B.; Sameni, H.R.; Haghmorad, D. Daphnetin alleviates experimental autoimmune encephalomyelitis by suppressing Th1 and Th17 cells and upregulating Th2 and regulatory T cells. Acta Neurobiol. Exp. 2022, 82, 273–283. [Google Scholar] [CrossRef]
- Haghmorad, D.; Yazdanpanah, E.; Jadid Tavaf, M.; Zargarani, S.; Soltanmohammadi, A.; Mahmoudi, M.B.; Mahmoudi, M. Prevention and treatment of experimental autoimmune encephalomyelitis induced mice with 1, 25-dihydroxyvitamin D3. Neurol. Res. 2019, 41, 943–957. [Google Scholar] [CrossRef] [PubMed]
- Haghmorad, D.; Yazdanpanah, E.; Sadighimoghaddam, B.; Yousefi, B.; Sahafi, P.; Ghorbani, N.; Rashidy-Pour, A.; Kokhaei, P. Kombucha ameliorates experimental autoimmune encephalomyelitis through activation of Treg and Th2 cells. Acta Neurol. Belg. 2021, 121, 1685–1692. [Google Scholar] [CrossRef] [PubMed]
- Berard, J.L.; Wolak, K.; Fournier, S.; David, S. Characterization of relapsing-remitting and chronic forms of experimental autoimmune encephalomyelitis in C57BL/6 mice. Glia 2010, 58, 434–445. [Google Scholar] [CrossRef] [PubMed]
- Toft-Hansen, H.; Fuchtbauer, L.; Owens, T. Inhibition of reactive astrocytosis in established experimental autoimmune encephalomyelitis favors infiltration by myeloid cells over T cells and enhances severity of disease. Glia 2011, 59, 166–176. [Google Scholar] [CrossRef]
- Horstmann, L.; Schmid, H.; Heinen, A.P.; Kurschus, F.C.; Dick, H.B.; Joachim, S.C. Inflammatory demyelination induces glia alterations and ganglion cell loss in the retina of an experimental autoimmune encephalomyelitis model. J. Neuroinflamm. 2013, 10, 120. [Google Scholar] [CrossRef]
- Metaxakis, A.; Petratou, D.; Tavernarakis, N. Molecular interventions towards multiple sclerosis treatment. Brain Sci. 2020, 10, 299. [Google Scholar] [CrossRef]
- Derdelinckx, J.; Cras, P.; Berneman, Z.N.; Cools, N. Antigen-specific treatment modalities in MS: The past, the present and the future. Front. Immunol. 2021, 12, 10. [Google Scholar] [CrossRef]
- Yamout, B.; Hourani, R.; Salti, H.; Barada, W.; El-Hajj, T.; Al-Kutoubi, A.; Herlopian, A.; Baz, E.K.; Mahfouz, R.; Khalil-Hamdan, R. Bone marrow mesenchymal stem cell transplantation in patients with multiple sclerosis: A pilot study. J. Neuroimmunol. 2010, 227, 185–189. [Google Scholar] [CrossRef]
- Faria, A.; Weiner, H.L. Oral tolerance: Therapeutic implications for autoimmune diseases. Clin. Dev. Immunol. 2006, 13, 143–157. [Google Scholar] [CrossRef]
- Jiang, Z.; Li, H.; Fitzgerald, D.C.; Zhang, G.X.; Rostami, A. MOG35–55 iv suppresses experimental autoimmune encephalomyelitis partially through modulation of Th17 and JAK/STAT pathways. Eur. J. Immunol. 2009, 39, 789–799. [Google Scholar] [CrossRef]
- Duraes, F.V.; Lippens, C.; Steinbach, K.; Dubrot, J.; Brighouse, D.; Bendriss-Vermare, N.; Issazadeh-Navikas, S.; Merkler, D.; Hugues, S. pDC therapy induces recovery from EAE by recruiting endogenous pDC to sites of CNS inflammation. J. Autoimmun. 2016, 67, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Langrish, C.L.; Chen, Y.; Blumenschein, W.M.; Mattson, J.; Basham, B.; Sedgwick, J.D.; McClanahan, T.; Kastelein, R.A.; Cua, D.J. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J. Exp. Med. 2005, 201, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Cua, D.J.; Sherlock, J.; Chen, Y.; Murphy, C.A.; Joyce, B.; Seymour, B.; Lucian, L.; To, W.; Kwan, S.; Churakova, T. Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature 2003, 421, 744–748. [Google Scholar] [CrossRef] [PubMed]
- Voorthuis, J.; Uitdehaag, B.; De Groot, C.; Goede, P.; Van Der Meide, P.H.; Dijkstra, C. Suppression of experimental allergic encephalomyelitis by intraventricular administration of interferon-gamma in Lewis rats. Clin. Exp. Immunol. 1990, 81, 183–188. [Google Scholar] [CrossRef]
- Sabatino, J.J.; Shires, J.; Altman, J.D.; Ford, M.L.; Evavold, B.D. Loss of IFN-γ enables the expansion of autoreactive CD4+ T cells to induce experimental autoimmune encephalomyelitis by a nonencephalitogenic myelin variant antigen. J. Immunol. 2008, 180, 4451–4457. [Google Scholar] [CrossRef] [PubMed]
- Arellano, G.; Ottum, P.A.; Reyes, L.I.; Burgos, P.I.; Naves, R. Stage-specific role of interferon-gamma in experimental autoimmune encephalomyelitis and multiple sclerosis. Front. Immunol. 2015, 6, 492. [Google Scholar] [CrossRef]
- Guo, B. IL-10 modulates Th17 pathogenicity during autoimmune diseases. J. Clin. Cell. Immunol. 2016, 7, 400. [Google Scholar] [CrossRef]
- Iwakura, Y.; Ishigame, H. The IL-23/IL-17 axis in inflammation. J. Clin. Investig. 2006, 116, 1218–1222. [Google Scholar] [CrossRef]
- McGeachy, M.J.; Stephens, L.A.; Anderton, S.M. Natural recovery and protection from autoimmune encephalomyelitis: Contribution of CD4+ CD25+ regulatory cells within the central nervous system. J. Immunol. 2005, 175, 3025–3032. [Google Scholar] [CrossRef]
- Etesam, Z.; Nemati, M.; Ebrahimizadeh, M.-A.; Ebrahimi, H.-A.; Hajghani, H.; Khalili, T.; Jafarzadeh, A. Different expressions of specific transcription factors of Th1 (T-bet) and Th2 cells (GATA-3) by peripheral blood mononuclear cells from patients with multiple sclerosis. Basic Clin. Neurosci. 2018, 9, 458. [Google Scholar] [CrossRef]
- Xu, J.; Wang, Y.; Jiang, H.; Sun, M.; Gao, J.; Xie, A. TGF-β in mice ameliorates experimental autoimmune encephalomyelitis in regulating NK cell activity. Cell Transplant. 2019, 28, 1155–1160. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.W.; Severin, M.E.; Lovett-Racke, A.E. TGF-β regulation of encephalitogenic and regulatory T cells in multiple sclerosis. Eur. J. Immunol. 2017, 47, 446–453. [Google Scholar] [CrossRef] [PubMed]
| Genes | Forward | Reverse |
|---|---|---|
| IFN-γ | CCAAGTTTGAGGTCAACA | CTGGCAGAATTATTCTTATTGG |
| T-bet | TGTGGTCCAAGTTCAACC | CATCCTGTAATGGCTTGTG |
| IL-17 | CCTCAGACTACCTCAACC | CCAGATCACAGAGGGATA |
| ROR-γt | GGATGAGATTGCCCTCTA | CCTTGTCGATGAGTCTTG |
| IL-4 | CTGGATTCATCGATAAGC | GATGCTCTTTAGGCTTTC |
| GATA3 | CTGCGGACTCTACCATAA | GTGGTGGTCTGACAGTTC |
| TGF-β | CGGACTACTATGCTAAAGA | CTGTGTGAGATGTCTTTG |
| Foxp3 | CAGAGTTCTTCCACAACA | CATGCGAGTAAACCAATG |
| B2m | CCTGTATGCTATCCAGAA | GTAGCAGTTCAGTATGTTC |
| Group | Day of Onset | Maximal Score (Score at Peak) | Mean Score (Last Day) | Cumulative Disease Index (CDI) |
|---|---|---|---|---|
| CTRL 1 | 9.5 ± 0.4 | 4.3 ± 0.13 | 3.4 ± 0.11 | 51.2 ± 1.27 |
| Prevention 2 | 11.2 ± 0.3 ** | 1.9 ± 0.14 *** | 0.8 ± 0.12 | 17 ± 0.61 *** |
| Treatment 3 | 10.6 ± 0.4 * | 2.5 ± 0.14 *** | 1.5 ± 0.12 *** | 25.3 ± 0.78 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haghmorad, D.; Yousefi, B.; Eslami, M.; Rashidy-Pour, A.; Tarahomi, M.; Tavaf, M.J.; Soltanmohammadi, A.; Zargarani, S.; Kamyshnyi, A.; Oksenych, V. RETRACTED: Oral Administration of Myelin Oligodendrocyte Glycoprotein Attenuates Experimental Autoimmune Encephalomyelitis through Induction of Th2/Treg Cells and Suppression of Th1/Th17 Immune Responses. Curr. Issues Mol. Biol. 2022, 44, 5728-5740. https://doi.org/10.3390/cimb44110388
Haghmorad D, Yousefi B, Eslami M, Rashidy-Pour A, Tarahomi M, Tavaf MJ, Soltanmohammadi A, Zargarani S, Kamyshnyi A, Oksenych V. RETRACTED: Oral Administration of Myelin Oligodendrocyte Glycoprotein Attenuates Experimental Autoimmune Encephalomyelitis through Induction of Th2/Treg Cells and Suppression of Th1/Th17 Immune Responses. Current Issues in Molecular Biology. 2022; 44(11):5728-5740. https://doi.org/10.3390/cimb44110388
Chicago/Turabian StyleHaghmorad, Dariush, Bahman Yousefi, Majid Eslami, Ali Rashidy-Pour, Mahdieh Tarahomi, Maryam Jadid Tavaf, Azita Soltanmohammadi, Simin Zargarani, Aleksandr Kamyshnyi, and Valentyn Oksenych. 2022. "RETRACTED: Oral Administration of Myelin Oligodendrocyte Glycoprotein Attenuates Experimental Autoimmune Encephalomyelitis through Induction of Th2/Treg Cells and Suppression of Th1/Th17 Immune Responses" Current Issues in Molecular Biology 44, no. 11: 5728-5740. https://doi.org/10.3390/cimb44110388
APA StyleHaghmorad, D., Yousefi, B., Eslami, M., Rashidy-Pour, A., Tarahomi, M., Tavaf, M. J., Soltanmohammadi, A., Zargarani, S., Kamyshnyi, A., & Oksenych, V. (2022). RETRACTED: Oral Administration of Myelin Oligodendrocyte Glycoprotein Attenuates Experimental Autoimmune Encephalomyelitis through Induction of Th2/Treg Cells and Suppression of Th1/Th17 Immune Responses. Current Issues in Molecular Biology, 44(11), 5728-5740. https://doi.org/10.3390/cimb44110388








