Critical Overview on the Benefits and Harms of Aspirin
Abstract
:1. Introduction
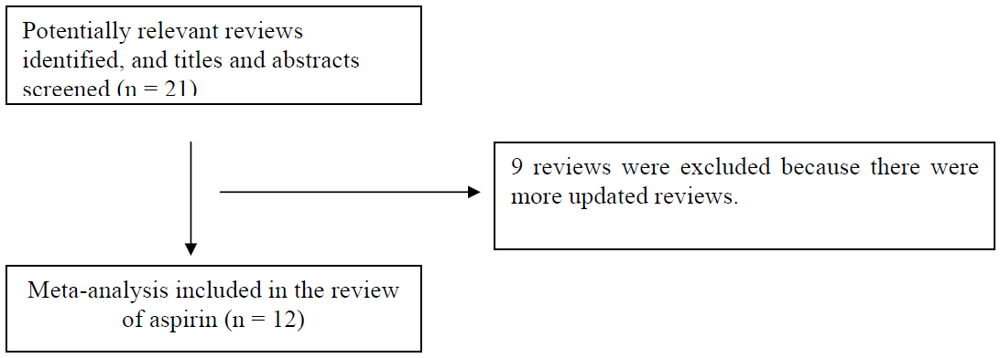
2. Experimental Methods
3. Results and Discussion
| Study | Trials and design | Participants | Outcomes | Findings | Quality |
|---|---|---|---|---|---|
| Alghamdi 2007 [62] | 10 studies; 5 trials, 5 cohort studies | 1,748 participants; 913 aspirin group, 835 control group | Risk of bleeding in coronary artery bypass graft patients | Aspirin use was associated with increase in blood loss, red cell and fresh frozen plasma transfusion, but not platelets or reexploration. | Results were limited because of heterogeneity and poor methodological quality |
| Askie 2007 [58] | 31 trials | 32,217 women and 32,819 babies | Risk of pre-eclampsia and pregnancy outcomes | Aspirin associated with reduced risk of pre-eclampsia, preterm delivery <34 weeks but no effect on maternal or fetal outcomes. | Trial quality was not discussed |
| ATC 2009 [3] | 22 trials, 6 primary prevention, 16 secondary prevention | 95,000 participants in primary prevention, 17,000 participants in secondary prevention trials | Risk of cardiovascular events, stroke, coronary events and death | Primary prevention with aspirin therapy results showed significant reduction in serious vascular events, non-fatal MI but not stroke or vascular mortality. Secondary prevention with aspirin significantly reduced serious vascular events, stroke and coronary events. | Trial quality was not discussed |
| Significant increase in major extracranial bleeds. | |||||
| Berger 2009 [57] | 18 trials | 5,269 participants; 2,823 aspirin group, 2,446 control group | Risk of cardiovascular events, stroke, coronary events, death and bleeding | Aspirin therapy significantly reduced incidence of non-fatal stroke but not all-cause mortality or MI. | Quality was assessed in 12 trials, high quality (Jadad 4–5) in 6 trials and low quality (Jadad 1–3) in 6 trials |
| Bujold 2009 [59] | 9 trials | 1,317 women | Risk of pre-eclampsia and pregnancy outcomes | Aspirin therapy before <16 weeks was associated with reduced pre-eclampsia, severe preeclampsia and gestational hypertension. | Mixed quality of trials as 5/9 were double-blind, 6/9 used ITT and most had <6% loss to follow up |
| Cole 2009 [60] | 4 trials | 2,967 participants; 1,289 control, 1,678 aspirin | Risk of adenomas and adverse events | Aspirin therapy significantly reduced both adenomas and advanced lesions compared to placebo. | One trial was small and had many drop outs and there was no formal quality assessment |
| De Berardis 2009 [56] | 6 trials | 10117 participants | Risk of cardiovascular events, death and adverse events | Aspirin therapy in diabetes patient was associated with no significant reduction in cardiovascular events, cardiovascular mortality or overall mortality. | Quality was suboptimal in some studies, 3/6 had adequate allocation concealment, all studies were adequately blinded and 5/6 used ITT principles |
| Kraspoulos 2008 [13] | 20 studies; 1 trial, 19 cohort studies | 2,930 participants | Risk of cardiovascular events, stroke, coronary events, death and vascular interventions | Among aspirin resistant patient there is significantly increased risk of cardiovascular event, death and acute coronary syndrome. | Quality of trials was high in 17/20 trials and remaining trials lacked information on quality |
| Lewis 2007 [63] | 6 cohorts studies, 4 included aspirin | 1,373 participants | Risk of complications in surgery | Aspirin therapy was associated with statistically significant increase in complications. | All studies had limitations and potential biases due to observational designs |
| Mangiapane 2008 [61] | 10 cohort studies | 236,655 participants | Risk of breast cancer | Aspirin therapy was associated with statistically significant reduction in breast cancer. | Quality was not discussed |
| Application of aspirin | Risk of event (95% confidence interval) | Treated event rate | Control event rate | Number needed to treat |
|---|---|---|---|---|
| Primary and secondary prevention of cardiovascular disease | ||||
| Primary prevention of non-fatal MI | RR 0.77 (0.67–0.89) | 0.18% per year | 0.23% per year | 1891 (NNTB 1318– 3953) per year |
| Secondary prevention of non-fatal MI | RR 0.69 (0.60–0.80) | 6.7% per year | 8.2% per year | 40 (NNTB 31– 61) per year |
| Primary prevention of stroke | RR 0.95 (0.85–1.06) | 0.20% per year | 0.21% per year | No significant benefit |
| Secondary prevention of stroke | RR 0.81 (0.71–0.92) | 2.08% per year | 2.54% per year | 208 (NNTB 136– 493) per year |
| Major GI and extracranial bleeds in primary prevention | RR 1.54 (1.30–1.82) | 0.10% per year | 0.08% per year | 2315 (NNTH 1525–4167) per year |
| Major GI and extracranial bleeds in secondary prevention | RR 2.69 (1.25– 5.76) | 0.17% per year | 0.07% per year | 846 (NNTH 301–5715) per year |
| Patients with peripheral vascular disease | ||||
| Major cardiovacular events | RR 0.88 (0.76– 1.04) | 8.9% (from 10 days to 6.7 years) | 11.0% (from 10 days to 6.7 years) | No significant benefit |
| Nonfatal stroke | RR 0.66 (0.47–0.94) | 2.1% (from 10 days to 6.7 years) | 3.1% (from 10 days to 6.7 years) | 95 (NNTB 61–538) (from 10 days to 6.7 years) |
| Patients with diabetes | ||||
| Major cardiovascular events | RR 0.90 (0.81– 1.00) | 12.5% (from 3– 10 years) | 13.7% (from 3–10 years) | No significant benefit |
| Patients with pre-eclampsia | ||||
| Risk of pre-eclampsia | RR 0.90 (0.84–0.97) | 7.9% during course of pregnancy | 8.7% during course of pregnancy | 115 (NNTB 72–384) during course of pregnancy |
| Patients with colorectal adenoma | ||||
| Prevention of any adenoma | RR 0.83 (0.72– 0.96) | 32.9% over 33 months | 36.7% over 33 months | 17 (NNTB 10–69) over 33 months |
| Prevention of advanced adenomas | RR 0.72 (0.57– 0.90) | 8.7% over 33 months | 11.9% over 33 months | 31 (NNTB 20–85) over 33 months |
3.1. Aspirin in cardiovascular disease
3.2. Aspirin in obstetrics
3.3. Aspirin in neoplastic conditions
3.4. Adverse effects of aspirin in patients having surgical procedures
3.5. Aspirin and Gastrointestinal Harm
4. Conclusions
Acknowledgements
References and Notes
- Antiplatelet Trialists’ Collaboration. Collaborative overview of randomised trials of antiplatelet therapy I: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ 1994, 308, 81–106. [PubMed]
- Antithromboic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002, 324, 71–86. [CrossRef] [PubMed]
- Antithromboic Trialists’ Collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009, 373, 1849–1860. [CrossRef] [PubMed]
- US Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: US Preventive Service Task Force Recommendation Statement. Ann. Intern. Med. 2009, 150, 396–404. [PubMed]
- Pearson, T.A.; Blair, S.N.; Daniels, S.R.; Eckel, R.H.; Fair, J.M.; Fortmann, S.P.; Franklin, B.A.; Goldstein, L.B.; Greenland, P.; Grundy, S.M.; et al. AHA Guidelines for primary prevention of cardiovascular disease and stroke 2002 update. Circulation 2002, 106, 388–391. [Google Scholar] [PubMed]
- JBS 2: Joint British Societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart 2005, 91 (Suppl. 5), v1–v52. [CrossRef] [PubMed]
- Kuliczkowski, W.; Halawa, B.; Korolko, B.; Mazurek, W. Aspirin resistance in ischemic heart disease. Kariol. Pol. 2005, 62, 14–19. [Google Scholar]
- Angiolillo, D.J.; Fernandez-Ortiz, A.; Bernardo, E.; Ramirez, D.; Sabate, M.; Jimenez-Quevedo, P.; Hernandez, R.; Moreno, R.; Escaned, J.; Alfonso, F.; Bañuelos, C.; Costa, M.A.; Bass, T.A.; Macaya, C. Influence of aspirin resistance on platelet function profiles in patients on long-term aspirin and clopidogrel after percutaneous coronary intervention. Am. J. Cardiol. 2006, 97, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Hegason, C.M.; Bolin, K.M.; Hoff, J.A.; Winkler, S.R.; Manget, A.; Tortorice, K.L.; Brace, L.D. Development of aspirin resistance in persons with previous ischaemic stroke. Stroke 1994, 25, 2331–2336. [Google Scholar]
- Kawasaki, T.; Ozeki, Y.; Igawa, T.; Kambayashi, J.-I. Increased platelet sensitivity to collagen in individuals resistant to low dose aspirin. Stroke 2000, 31, 591–596. [Google Scholar]
- Macchi, L.; Christianes, L.; Brabant, S.; Sorel, N.; Allal, J.; Mauco, G.; Brizard, A. Resistance to aspirin is associated with platelet sensitivity to adenosine diphosphate. Thromb. Res. 2002, 107, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, N.; Wenk, A.; Kim, U.; Kienzel, P.; Weber, A.A.; Gams, E.; Schror, K.; Hohlfeld, T. Functional and biochemical evaluation of platelet aspirin resistance after coronary artery bypass surgery. Circulation 2003, 108, 542–547. [Google Scholar]
- Krasopoulos, G.; Brister, S.J.; Beattie, W.S.; Elliot, R.F.; Buchanan, M.R. Aspirin “resistance” and risk of cardiovascular morbidity: systematic review and meta-analysis. BMJ 2008, 336, 195–198. [Google Scholar]
- Patrono, C.; Garcia Rodriguez, L.A.; Landolfi, R.; Baigent, C. Low-dose aspirin for the prevention of atherothrombosis. N. Engl. J. Med. 2005, 353, 2373–2383. [Google Scholar]
- Buchanan, M.R. Biological basis and clinical implications of acetylsalicylic acid resistance. Can. J. Cardiol. 2006, 22, 149–151. [Google Scholar]
- Eikelboon, J.W.; Hirsh, J.; Weitz, J.I.; Johnson, M.; Yi, Q.; Yusef, S. Aspirin-resistant thromboxane biosynthesis and risk of myocardial infarction, stroke or cardiovascular death in patients at high risk for cardiovascular events. Circulation 2002, 105, 1650–1655. [Google Scholar] [CrossRef] [PubMed]
- Patrono, C. Aspirin resistance: definition, mechanisms and clinical read-outs. J. Thrombo. Haemost. 2003, 1, 1710–1713. [Google Scholar]
- Hennekens, C.H.; Schor, K.; Weisman, S.; Fitzgerald, G.A. Semantic complexity and aspirin resistance. Circulation 2004, 110, 1706–1708. [Google Scholar]
- Cattaneo, M. Aspirin and clopidogrel: efficacy, safety, and the issues of drug resistance. Arterioscler. Throm. Vasc. Biol. 2004, 24, 1980–1987. [Google Scholar] [CrossRef]
- Duley, L.; Hendeson-Smart, D.J.; Knight, M.; King, J. Antiplatelet agents for preventing pre-eclampsia and its complications. Cochrane Database Syst. Rev. 2003, 1, CD004659. [Google Scholar]
- Sibai, B.M.; Cartis, S.; Thom, E.; Klebanoff, M.; McNellis, D.; Rocco, L.; Paul, R.H.; Romero, R.; Witter, F.; Rosen, M.; et al. Prevention of preeclampsia with low-dose aspirin in healthy, nulliparous pregnant women. N. Engl. J. Med. 1993, 329, 1213–1218. [Google Scholar]
- CLASP (Collaborative Low-dose Aspirin Study in Pregnancy) Collaborative Group. CLASP: a randomised trial of low-dose aspirin for the prevention and treatment of pre-eclampsia among 9364 pregnant women. Lancet 1994, 343, 619–629. [PubMed]
- Golding, J. A randomised trial of low dose aspirin for primipara in pregnancy. Br. J. Obstet. Gynaecol. 1998, 105, 293–299. [Google Scholar]
- Rotchell, Y.E.; Cruikshank, J.K.; Gay, M.P.; Griffiths, J.; Stewart, A.; Farrell, B.; Ayers, S.; Hennis, A.; Grant, A.; Duley, L.; Collins, R. Barbados Low Dose Aspirin Study in Pregnancy (BLASP): a randomised trial for the prevention of pre-eclampsia and its complications. Br. J. Obstet. Gynaecol. 1998, 105, 286–292. [Google Scholar]
- Cartitis, S.; Sibai, B.M.; Hauth, J.; Lindheimer, M.D.; Klebanoff, M.; Thom, E.; van Dorsten, P.; Landon, M.; Paul, R.; Miodovnik, M.; Meis, P.; Thurnau, G. Low-dose aspirin to prevent preeclampsia in women at high risk. N. Engl. J. Med. 1998, 338, 701–705. [Google Scholar]
- Lindheimer, M.D. Unraveling the mysteries of preeclampsia. Am. J. Obstet. Gynecol. 2005, 193, 3–4. [Google Scholar]
- Baron, J.A. Epidemiology of non-steroidal anti-inflammatory drugs and cancer. Prog. Exp. Tumor Res. 2003, 37, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Flossman, E.; Rothwell, P.M. Effect of aspirin on long-term risk of colorectal cancer: consistent evidence from randomised and observational studies. Lancet 2007, 369, 1603–1613. [Google Scholar]
- Chan, A.T.; Giovannuci, E.L.; Meyerhardt, J.A.; Schernhammer, E.S.; Curhan, G.C.; Wu, K.; Fuches, C.S. Aspirin dose and duration of use and risk of colorectal cancer in mean. Gastroenterology 2008, 134, 21–28. [Google Scholar]
- Chan, A.T.; Giovannuci, E.L.; Meyerhardt, J.A.; Schernhammer, E.S.; Curhan, G.C.; Fuches, C.S. Long-term use of aspirin and nonsteroidal anti-inflammatory drugs and risk of colorectal cancer. JAMA 2005, 294, 914–923. [Google Scholar]
- Sandler, R.S.; Halabi, S.; Baron, J.A.; Budinger, S.; Paskett, E.; Keresztes, R.; Petrelli, N.; Pipas, J.M.; Karp, D.D.; Loprinzi, C.L.; Steinbach, G.; Schilsky, R. A randomized trial of aspirin to prevent colorectal adenomas in patients with previous colorectal cancer. New Engl. J. Med. 2003, 348, 883–890. [Google Scholar]
- Logan, R.F.A.; Grainge, M.J.; Shepherd, V.C.; Armitage, N.C.; Muir, K.R. Aspirin and folic acid for the prevention of recurrent colorectal adenomas. Gastroenterology 2008, 134, 29–38. [Google Scholar]
- Benamouzig, R.; Deyra, J.; Martin, A.; Girard, B.; Jullian, E.; Piednoir, B.; Couturier, D.; Coste, T.; Little, J.; Chaussade, S. Daily soluble aspirin and prevention of colorectal adenomas recurrence: one-year results of the APACC trial. Gastroenterology 2003, 125, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Khuder, S.A.; Mutgi, A.B. Breast cancer and NSAID use: A meta-analysis. Br. J. Cancer 2001, 84, 1188–1192. [Google Scholar]
- Gonzalez-Perez, A.; Garcia Rodriguez, L.A.; Lopez-Ridaura, R. Effects of non-steroidal anti-inflammatory drugs on cancer sites other than the colon and rectum: a meta-analysis. BMC Cancer 2003, 3, 28. [Google Scholar]
- Coogan, P.F.; Rao, S.R.; Rosenberg, L.; Palmer, J.R.; Strom, B.L.; Zauber, A.G.; Stolley, P.D.; Shapiro, S. The relationship of nonsteroidal anti-inflammatory drug use to the risk of breast cancer. Prev. Med. 1999, 24, 107–109. [Google Scholar]
- Egan, K.M.; Stampfer, M.J.; Giovannucci, E.; Rosner, B.A.; Colditz, G.A. Prospective study of regular aspirin use and the risk of breast cancer. J. Natl. Cancer Inst. 1996, 88, 988–933. [Google Scholar]
- Harris, R.E.; Namboodiri, K.K.; Farrar, W.B. Nonsteroidal anti-inflammatory drugs and breast cancer. Epidemiology 1996, 7, 203–205. [Google Scholar]
- Neugut, A.I.; Rosenberg, D.J.; Ahsan, H.; Jacobson, J.S.; Wahid, N.; Hagan, M.; Rahman, M.I.; Khan, Z.R.; Chen, L.; Pablos-Mendez, A.; Shea, S. Association between coronary heart disease and cancers of the breast, prostate and colon. Cancer Epidemiol. Biomarkers Prev. 1998, 7, 869–873. [Google Scholar]
- Harris, R.E.; Kasbari, S.; Farrar, W.B. Prospective study of non-steroidal anti-inflammatory drugs and breast cancer. Oncol. Rep. 1999, 6, 71–73. [Google Scholar]
- Sharpe, C.R.; Collet, J.P.; McNutt, M.; Belzile, E.; Boivin, J.F.; Hanley, J.A. Nested case-control study of the effects of non-steroidal anti-inflammatory drugs on breast cancer risk and stage. Br. J. Cancer 2000, 83, 112–120. [Google Scholar]
- Langman, M.J.; Cheng, K.K.; Gilman, E.A.; Lancashire, R.J. Effect of anti-inflammatory drugs on overall risk of common cancer: Case-control study in general practice research database. Br. Med. J. 2000, 320, 1642–1646. [Google Scholar]
- Meier, C.R.; Schmitz, S.; Jick, H. Association between acetaminophen or nonsteroidal anti-inflammatory drugs and risk of developing ovarian, breast, or colon cancer. Pharmacotherapy 2002, 22, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Cotterchio, M.; Kreiger, N.; Sloan, M.; Steingart, A. Nonsteroidal anti-inflammatory drug use and breast cancer risk. Cancer Epidemiol. Biomarkers Prev. 2001, 10, 1213–1217. [Google Scholar]
- Johnson, T.W.; Anderson, K.E.; Lazovich, D.; Folsom, A.R. Association of aspirin and non-steroidal anti-inflammatory drugs use with breast cancer. Cancer Epidemiol. Biomarkers Prev. 2002, 11, 1586–1591. [Google Scholar] [PubMed]
- He, J.; Whelton, P.K.; Vu, B.; Klag, M.J. Aspirin and risk of hemorrhagic stroke: a meta-analysis of randomized controlled trials. JAMA 1998, 280, 1930–1935. [Google Scholar]
- Derry, S.; Loke, Y.K. Risk of gastrointestinal haemorrhage with long term use of aspirin: a meta-analysis. BMJ 2000, 321, 1183–1187. [Google Scholar]
- Bojar, R.M. Manual of Perioperative Care in Adult Cardiac Surgery; Blackwell: Malden, Oxford, UK, 2005. [Google Scholar]
- Kallis, P.; Tooze, J.A.; Talbot, S.; Cowans, D.; Bevan, D.H.; Treasure, T. Pre-operative aspirin decreases platelet aggregation and increase post-operative blood loss-a prospective randomised, placebo controlled, double-blind clinical trial in 1000 patients with chronic stable angina. Eur. J. Cardio-Thorac. Surg. 1994, 8, 404–409. [Google Scholar] [CrossRef]
- Morawski, W.; Sanak, M.; Cisowski, M.; Szczeklik, M.; Szczeklik, W.; Dropinski, J.; Waclawczyk, T.; Ulczok, R.; Bochenek, A. Prediction of the excess perioperative bleeding in patients undergoing coronary artery bypass grafting: role of aspirin and platelet glycoprotein IIa polymorphism. J. Thorac. Cardiovasc. Surg. 2005, 130, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Sethi, G.K.; Copeland, J.G.; Goldman, S.; Moritz, T.; Zadina, K.; Henderson, W.G. Implications of preoperative administration of aspirin in patients undergoing coronary artery bypass grating. Department of Veterans Affairs Cooperative Study on Antiplatelet Therapy. J. Am. Coll. Cardiol. 1990, 15, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Reich, D.L.; Patel, G.C.; Vela-Cantos, F.; Bodian, C.; Lansman, S. Aspirin dose not increase homologous blood requirements in elective coronary bypass surgery. Anesth. Analg. 1994, 79, 4–8. [Google Scholar]
- Veylsteke, A.; Oduro, A.; Cardan, E.; Latimer, R.D. Effect of aspirin in coronary artery bypass grafting. J. Cardiothorac. Vasc. Anaesth. 1997, 11, 831–834. [Google Scholar]
- Dacey, L.J.; Munoz, J.J.; Johnson, E.R.; Leavitt, B.J.; Maloney, C.T.; Morton, J.R.; Olmstead, E.M.; Birkmeyer, J.D.; O’Connor, G.T. Effect of preoperative aspirin use on mortality in coronary artery bypass grafting patients. Ann. Thorac. Surg. 2000, 70, 1986–1990. [Google Scholar]
- Bybee, K.A.; Powell, B.D.; Valeti, U.; Rosales, A.G.; Kopecky, S.L.; Mullany, C.; Wright, R.S. Preoperative aspirin therapy is associated with improved postoperative outcomesin patients undergoing coronary artery bypass grafting. Circulation 2005, 112, 1286–1292. [Google Scholar]
- De Berardis, G.; Sacco, M.; Strippoli, G.F.M.; Pellegrini, F.; Graziano, G.; Tognoni, G.; Nicolucci, A. Aspirin for the primary prevention of cardiovascular events in people with diabetes: meta-analysis of randomised controlled trials. BMJ 2009, 339, b4531. [Google Scholar] [PubMed]
- Berger, J.S.; Krantz, M.J.; Kittelson, J.M.; Hiatt, W.R. Aspirin for the prevention of cardiovascular events in patients with peripheral artery disease: a meta-analysis or randomized trials. JAMA 2009, 301, 1909–1919. [Google Scholar]
- Askie, L.M.; Duley, L.; Henderson-Smart, D.J.; Stewart, L.A. of the PAIRS Collaborative Group. Antiplatelet agents for prevention of pre-eclampsia: meta-analysis of individual patient data. Lancet 2007, 369, 1791–1798. [Google Scholar] [PubMed]
- Bujold, E.; Morency, A.-M.; Roberge, S.; Lacasse, Y.; Forest, J.-C.; Giguere, Y. Acetylsalicylic acid for the prevention of preeclampsia and intra-uterine growth restriction in women with abnormal uterine artery Doppler: a systematic review and meta-analysis. J. Obstet. Gynaecol. Can. 2009, 31, 818–826. [Google Scholar]
- Cole, B.F.; Logan, R.F.; Halabi, S.; Benamouzig, R.; Sandler, R.S.; Grainge, M.J.; Chaussade, S.; Baron, J.A. Aspirin for the chemoprevention of colorectal adenomas: a meta-analysis of the randomized trials. J. Natl. Cancer. Inst. 2009, 101, 256–266. [Google Scholar]
- Mangiapane, S.; Blettner, M.; Schlattmann, P. Aspirin use and breast cancer risk: a meta-analysis and meta-regression of observational studies from 2001 to 2005. Pharmacoepidemiol. Drug Saf. 2008, 17, 115–124. [Google Scholar]
- Alghamdi, A.A.; Moussa, F.; Fremes, S.E. Does the use of preoperative aspirin increase the risk of bleeding in patients undergoing coronary artery bypass grafting surgery? Systematic review and meta-analysis. J. Card. Surg. 2007, 22, 247–256. [Google Scholar]
- Lewis, K.G.; Dufresne, R.G., Jr. A meta-analysis of complications attributed to anticoagulation among patients following cutaneous surgery. Dermatol. Surg. 2008, 34, 160–165. [Google Scholar] [PubMed]
- Syed, S.; Adams, B.B.; Liao, W.; Pipitone, M.; Gloster, H. A prospective assessment of bleeding and international normalized ratio in warfarin-anticoagulated patients having cutaneous surgery. J. Am. Acad. Dermtol. 2004, 51, 955–957. [Google Scholar]
- Kargi, E.; Babuccu, O.; Hosnuter, M.; Babuccu, B.; Altinyazar, C. Complications of minor cutaneous surgery in patients under anticoagulant treatment. Aesthet. Plast. Surg. 2002, 26, 483–485. [Google Scholar]
- Alcalay, J. Cutaneous surgery in patients receiving warfarin therapy. Dermatol. Surg. 2001, 27, 756–758. [Google Scholar]
- Alam, M.; Goldberg, L.H. Serious adverse vascular events associated with perioperative interruptions of antiplatelet and anticoagulant therapy. Dermatol. Surg. 2002, 28, 992–998, discussion 998. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.; Robinson, J.; Stewart, J.; Jacob, S. Does enteric-coated aspirin result in a lower incidence of gastrointestinal complications compared to normal aspirin? Interact Cardiovasc Thorac Surg. 2007, 6, 519–522. [Google Scholar] [CrossRef] [PubMed]
- Straube, S.; Tramèr, M.R.; Moore, R.A.; Derry, S.; McQuay, H.J. Mortality with upper gastrointestinal bleeding and perforation: effects of time and NSAID use. BMC Gastroenterol. 2009, 5, 9–41. [Google Scholar]
© 2010 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Kwok, C.S.; Loke, Y.K. Critical Overview on the Benefits and Harms of Aspirin. Pharmaceuticals 2010, 3, 1491-1506. https://doi.org/10.3390/ph3051491
Kwok CS, Loke YK. Critical Overview on the Benefits and Harms of Aspirin. Pharmaceuticals. 2010; 3(5):1491-1506. https://doi.org/10.3390/ph3051491
Chicago/Turabian StyleKwok, Chun Shing, and Yoon K. Loke. 2010. "Critical Overview on the Benefits and Harms of Aspirin" Pharmaceuticals 3, no. 5: 1491-1506. https://doi.org/10.3390/ph3051491
APA StyleKwok, C. S., & Loke, Y. K. (2010). Critical Overview on the Benefits and Harms of Aspirin. Pharmaceuticals, 3(5), 1491-1506. https://doi.org/10.3390/ph3051491




