Efficient Delivery of SARS-CoV-2 Plasmid DNA in HEK-293T Cells Using Chitosan Nanoparticles
Abstract
:1. Introduction
2. Results
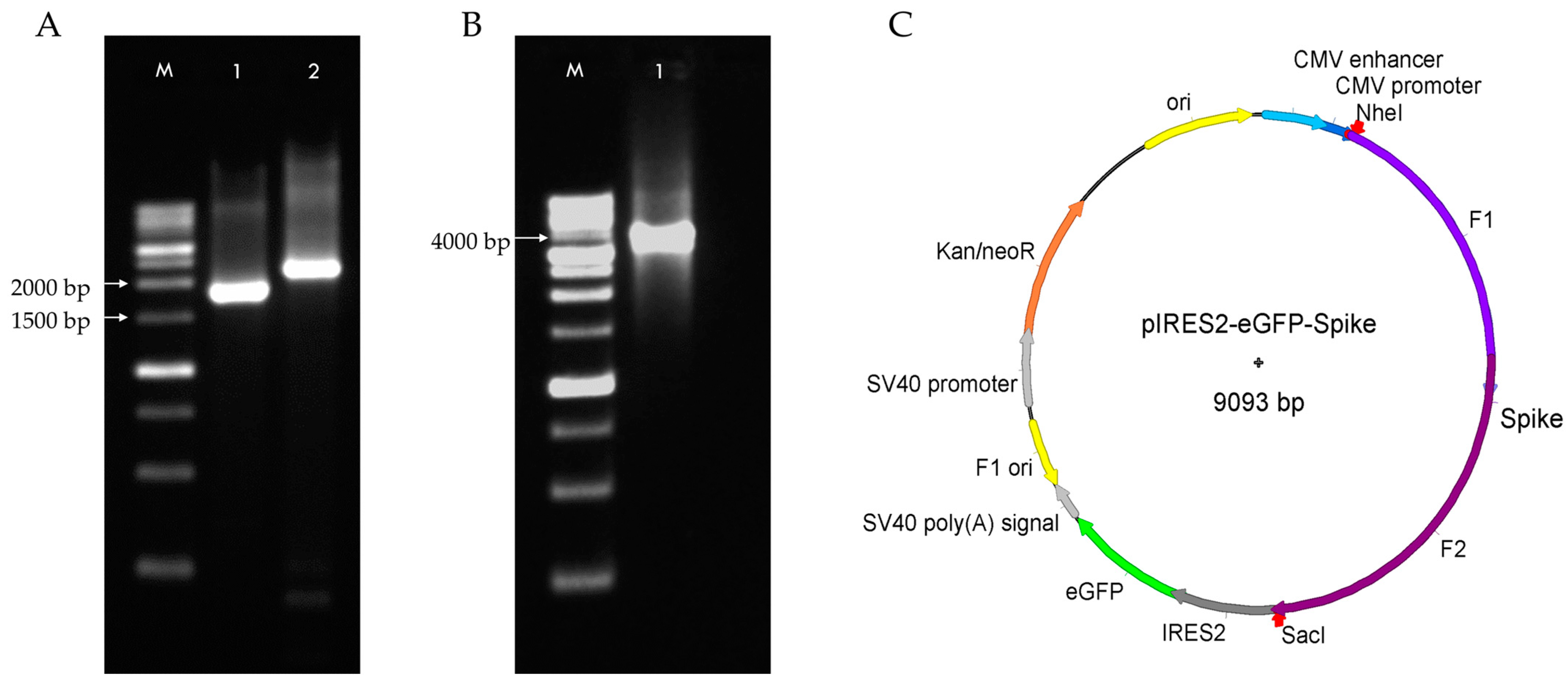
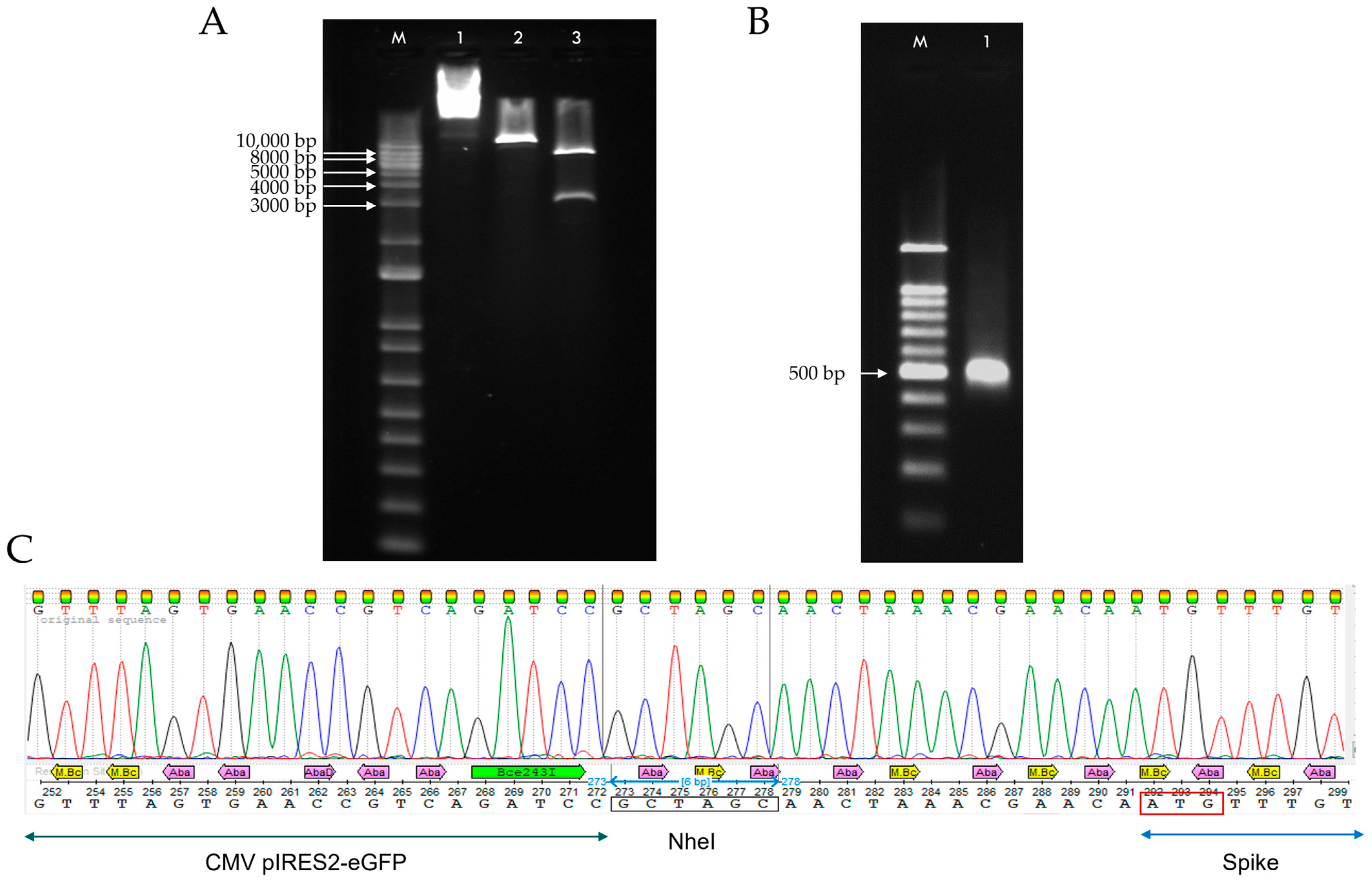
2.1. Construction of DNA Plasmid pIRES2-eGFP-Spike
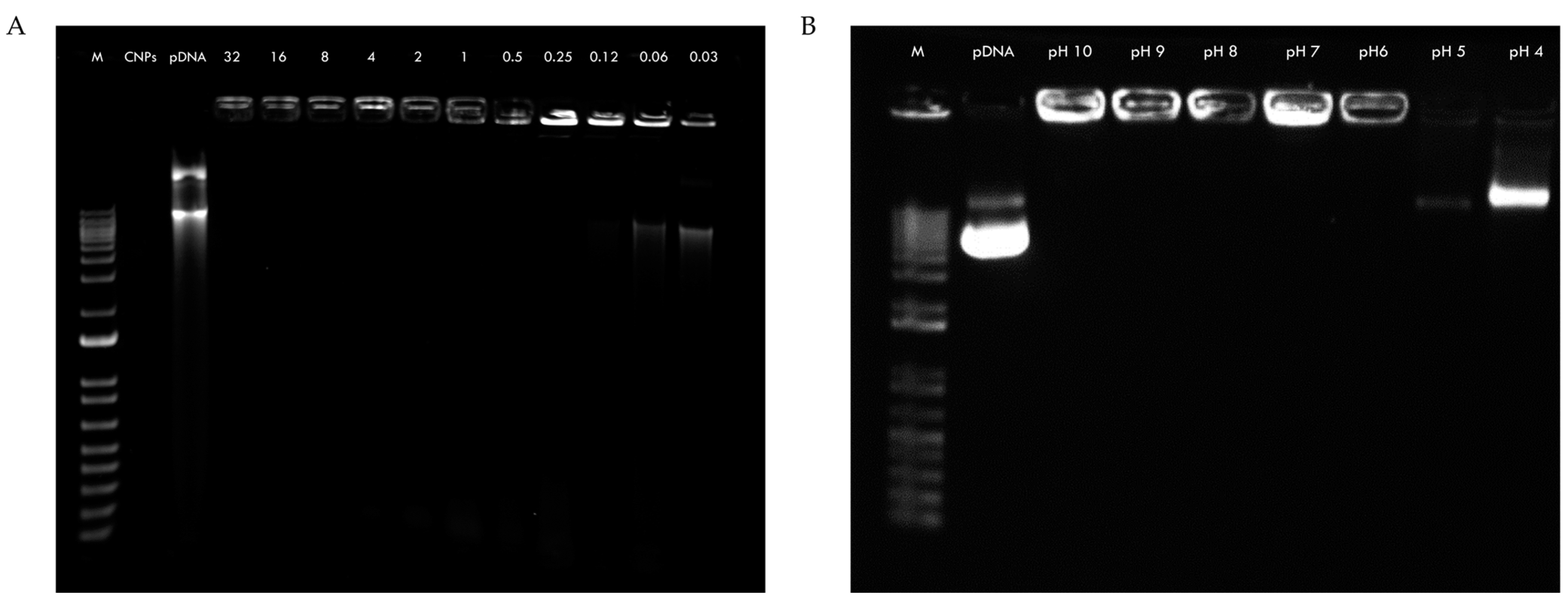
2.2. Retardation and Release Assay of CNPs-pDNA Polyplexes
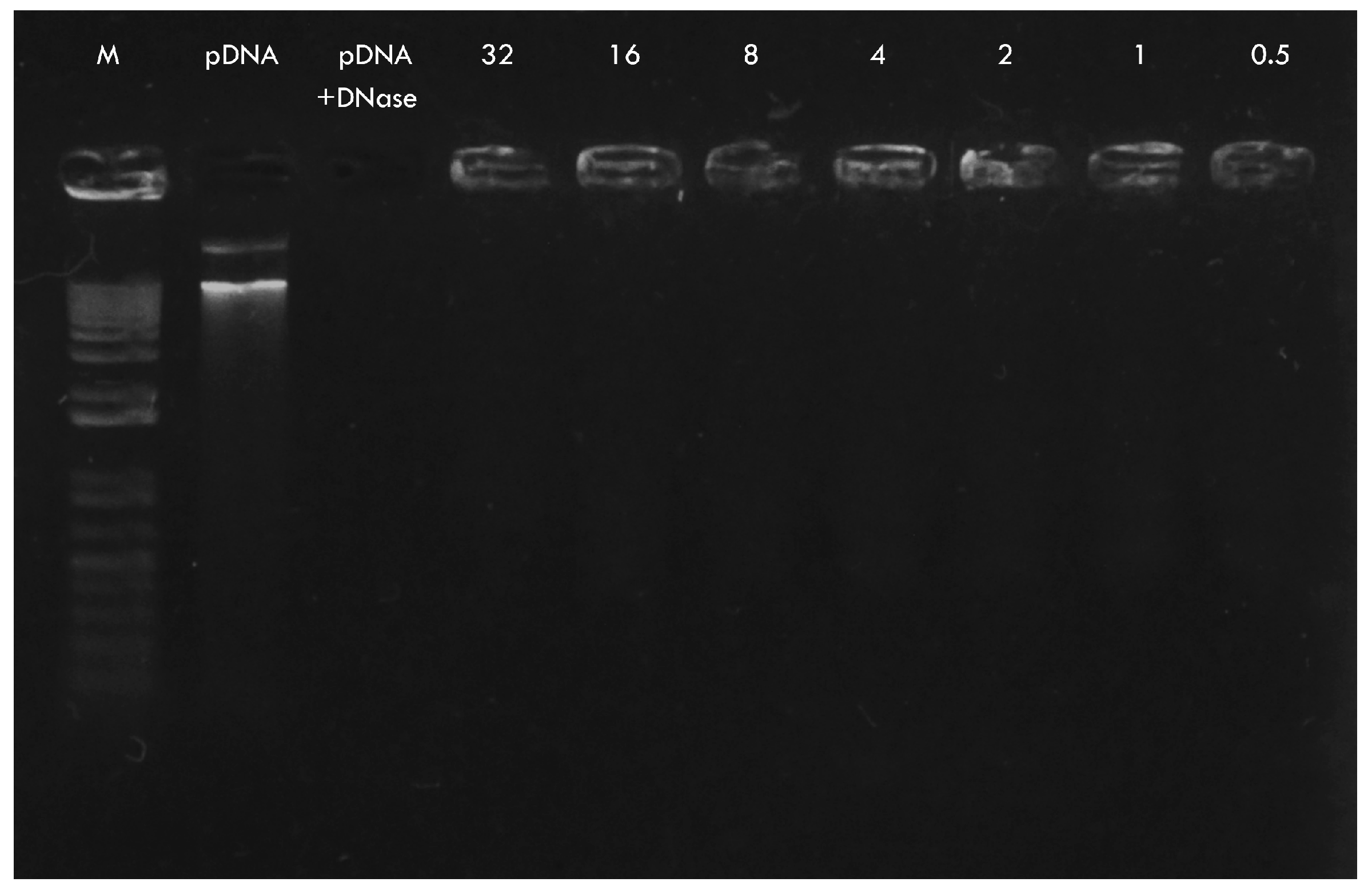
2.3. DNase I Protection Assay of CNPs-pDNA Polyplexes
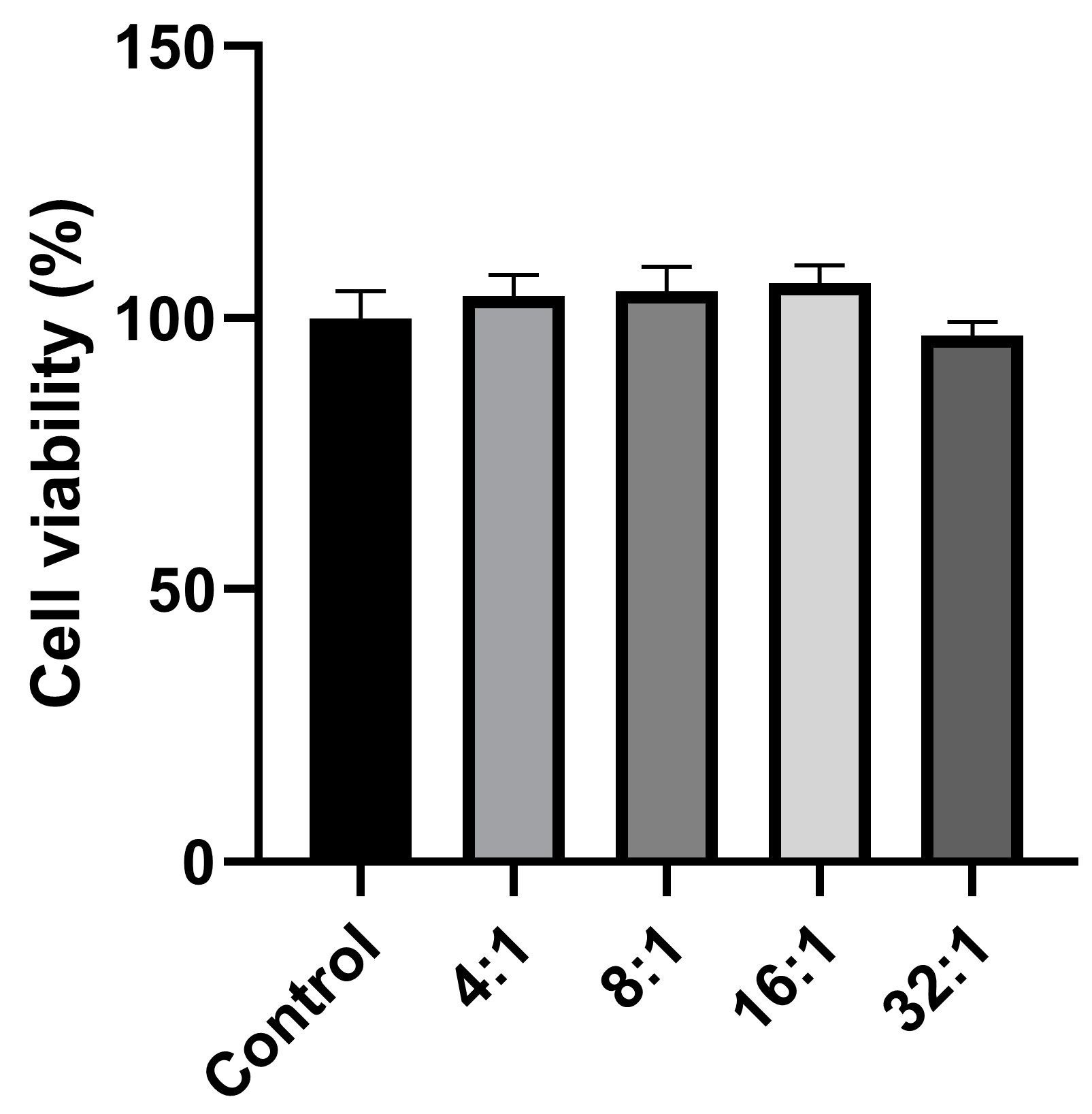
2.4. Cell Viability Assay by MTT
2.5. Characterization of CNPs-pDNA Polyplexes
2.6. Transfection of HEK-293T Cells
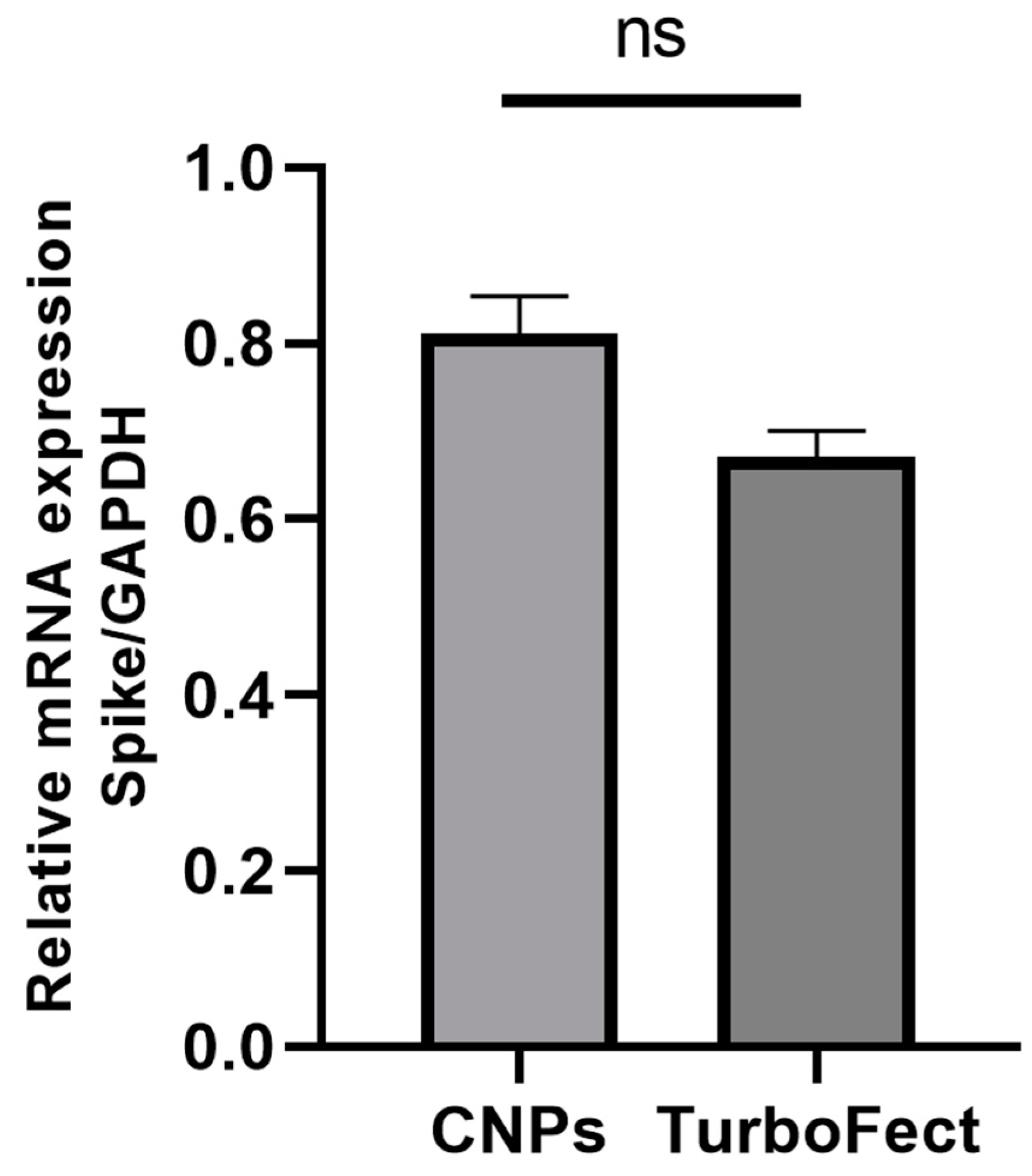
2.7. Spike mRNA Expression in HEK-293T Cells by RT-qPCR
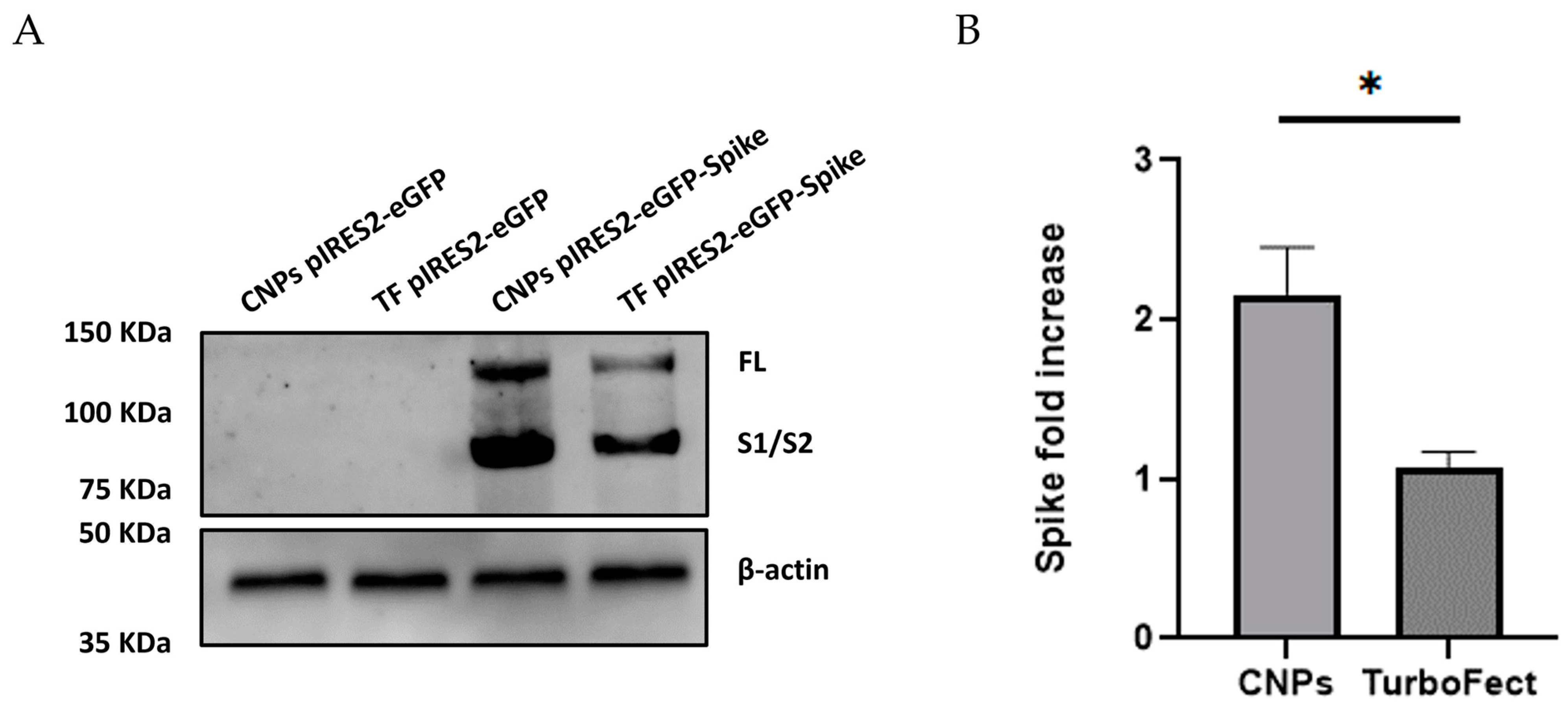
2.8. Verification of Spike Protein Expression in HEK-293T Cells by Western Blot
3. Discussion
4. Materials and Methods
4.1. Construction of DNA Plasmid pIRES2-eGFP-Spike
4.1.1. Synthesis of Spike cDNA by RT-PCR from Positive Samples
4.1.2. Amplification of the Spike Sequence
4.1.3. Cloning of the Spike Sequence into pIRES2-eGFP
4.2. Synthesis of Chitosan Nanoparticles and Preparation of pDNA Polyplexes
4.3. Retardation and Release Assay of pDNA Polyplexes
4.4. DNase I Protection Assay of CNPs-pDNA Polyplexes
4.5. Cell Viability Assay by MTT
4.6. Characterization of CNPs-pDNA Polyplexes
4.6.1. Spectroscopic Measurement by UV-Vis
4.6.2. Chemical Composition by Fourier-Transform Infrared Spectroscopy (FT-IR)
4.6.3. Size and Morphology by Transmission Electron Microscopy (TEM)
4.6.4. Size, PDI, and Zeta Potential by Dynamic Light Scattering (DLS)
4.7. Transfection of HEK-293T Cells
4.7.1. Spike mRNA Expression in HEK-293T Cells by RT-qPCR
4.7.2. Spike mRNA Expression in HEK-293T Cells by Western Blot
4.8. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ginn, S.L.; Amaya, A.K.; Alexander, I.E.; Edelstein, M.; Abedi, M.R. Gene therapy clinical trials worldwide to 2017: An update. J. Gene Med. 2018, 20, e3015. [Google Scholar] [CrossRef]
- Wang, D.; Tai, P.W.L.; Gao, G. Adeno-associated virus vector as a platform for gene therapy delivery. Nat. Rev. Drug Discov. 2019, 18, 358–378. [Google Scholar] [CrossRef] [PubMed]
- Nayerossadat, N.; Maedeh, T.; Ali, P.A. Viral and nonviral delivery systems for gene delivery. Adv. Biomed. Res. 2012, 1, 27. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Kanasty, R.L.; Eltoukhy, A.A.; Vegas, A.J.; Dorkin, J.R.; Anderson, D.G. Non-viral vectors for gene-based therapy. Nat. Rev. Genet. 2014, 15, 541–555. [Google Scholar] [CrossRef]
- Anselmo, A.C.; Mitragotri, S. Nanoparticles in the clinic: An update. Bioeng. Transl. Med. 2019, 4, e10143. [Google Scholar] [CrossRef] [PubMed]
- Wilczewska, A.Z.; Niemirowicz, K.; Markiewicz, K.H.; Car, H. Nanoparticles as drug delivery systems. Pharmacol. Rep. 2012, 64, 1020–1037. [Google Scholar] [CrossRef]
- Blanco, E.; Shen, H.; Ferrari, M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat. Biotechnol. 2015, 33, 941–951. [Google Scholar] [CrossRef]
- Stewart, M.P.; Langer, R.; Jensen, K.F. Intracellular delivery by membrane disruption: Mechanisms, strategies, and concepts. Chem. Rev. 2018, 118, 7409–7531. [Google Scholar] [CrossRef]
- Pardi, N.; Hogan, M.J.; Porter, F.W.; Weissman, D. mRNA vaccines—A new era in vaccinology. Nat. Rev. Drug Discov. 2018, 17, 261–279. [Google Scholar] [CrossRef]
- Grewal, A.K.; Salar, R.K. Chitosan nanoparticle delivery systems: An effective approach to enhancing efficacy and safety of anticancer drugs. Nano TransMed. 2024, 3, 100040. [Google Scholar] [CrossRef]
- Dilnawaz, F.; Acharya, S.; Kanungo, A. A clinical perspective of chitosan nanoparticles for infectious disease management. Polym. Bull. 2024, 81, 1071–1095. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Wu, Y. Recent advances of chitosan-based nanoparticles for biomedical and biotechnological applications. Int. J. Biol. Macromol. 2022, 203, 379–388. [Google Scholar] [CrossRef] [PubMed]
- Kean, T.; Thanou, M. Biodegradation, biodistribution and toxicity of chitosan. Adv. Drug Deliv. Rev. 2010, 62, 3–11. [Google Scholar] [CrossRef]
- Rinaudo, M. Chitin and chitosan: Properties and applications. Prog. Polym. Sci. 2006, 31, 603–632. [Google Scholar] [CrossRef]
- Mao, S.; Sun, W.; Kissel, T. Chitosan-based formulations for delivery of DNA and siRNA. Adv. Drug Deliv. Rev. 2010, 62, 12–27. [Google Scholar] [CrossRef]
- Huang, M.; Khor, E.; Lim, L.Y. Uptake and cytotoxicity of chitosan molecules and nanoparticles: Effects of molecular weight and degree of deacetylation. Pharm. Res. 2004, 21, 344–353. [Google Scholar] [CrossRef]
- Amidi, M.; Romeijn, S.G.; Borchard, G.; Junginger, H.E.; Hennink, W.E.; Jiskoot, W. Preparation and characterization of protein-loaded N-trimethyl chitosan nanoparticles as nasal delivery system. J. Control. Release 2006, 111, 107–116. [Google Scholar] [CrossRef]
- Pei, Y.; Yeo, Y. Drug delivery to macrophages: Challenges and opportunities. J. Control. Release 2016, 240, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.L.; Islam, M.A.; Xing, L.; Firdous, J.; Cao, W.; He, Y.J.; Zhu, Y.; Cho, K.H.; Li, H.S.; Cho, C.S. Degradable Polyethylenimine-Based Gene Carriers for Cancer Therapy. Top. Curr. Chem. 2017, 375, 34. [Google Scholar] [CrossRef]
- He, H.; Lu, Y.; Qi, J.; Zhu, Q.; Chen, Z.; Wu, W. Adapting liposomes for oral drug delivery. Acta Pharm. Sin. B 2019, 9, 36–48. [Google Scholar] [CrossRef]
- Gaglio, S.C.; Perduca, M.; Zipeto, D.; Bardi, G. Efficiency of Chitosan Nanocarriers in Vaccinology for Mucosal Immunization. Vaccines 2023, 11, 1333. [Google Scholar] [CrossRef]
- Richard, I.; Thibault, M.; De Crescenzo, G.; Buschmann, M.D.; Lavertu, M. Ionization behavior of chitosan and chitosan-DNA polyplexes indicate that chitosan has a similar capability to induce a proton-sponge effect as PEI. Biomacromolecules 2013, 14, 1732–1740. [Google Scholar] [CrossRef] [PubMed]
- Carroll, E.C.; Jin, L.; Mori, A.; Muñoz-Wolf, N.; Oleszycka, E.; Moran, H.B.T.; Mansouri, S.; McEntee, C.P.; Lambe, E.; Agger, E.M.; et al. The vaccine adjuvant chitosan promotes cellular immunity via DNA sensor cGAS-STING-dependent induction of type I interferons. Immunity 2016, 44, 597–608. [Google Scholar] [CrossRef] [PubMed]
- Sharma, D.; Arora, S.; Singh, J.; Layek, B. A review of the tortuous path of nonviral gene delivery and recent progress. Int. J. Biol. Macromol. 2021, 183, 2055–2073. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Antoniou, V.; Mourelatou, E.A.; Galatou, E.; Avgoustakis, K.; Hatziantoniou, S. Gene therapy with chitosan nanoparticles: Modern formulation strategies for enhancing cancer cell transfection. Pharmaceutics 2024, 16, 868. [Google Scholar] [CrossRef] [PubMed]
- Aibani, N.; Rai, R.; Patel, P.; Cuddihy, G.; Wasan, E.K. Chitosan nanoparticles at the biological interface: Implications for drug delivery. Pharmaceutics 2021, 13, 1686. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Herdiana, Y.; Husni, P.; Nurhasanah, S.; Shamsuddin, S.; Wathoni, N. Chitosan-based nano systems for natural antioxidants in breast cancer therapy. Polymers 2023, 15, 2953. [Google Scholar] [CrossRef]
- Duceppe, N.; Tabrizian, M. Advances in using chitosan-based nanoparticles for in vitro and in vivo drug and gene delivery. Expert Opin. Drug Deliv. 2010, 7, 1191–1207. [Google Scholar] [CrossRef] [PubMed]
- Costa, E.M.; Silva, S.; Pintado, M. Chitosan nanoparticles production: Optimization of physical parameters, biochemical characterization, and stability upon storage. Appl. Sci. 2023, 13, 1900. [Google Scholar] [CrossRef]
- Lu, B.; Lim, J.M.; Yu, B.; Song, S.; Neeli, P.; Sobhani, N.; K, P.; Bonam, S.R.; Kurapati, R.; Zheng, J.; et al. The next-generation DNA vaccine platforms and delivery systems: Advances, challenges and prospects. Front. Immunol. 2024, 15, 1332939. [Google Scholar] [CrossRef]
- Zhang, C.; Maruggi, G.; Shan, H.; Li, J. Advances in mRNA vaccines for infectious diseases. Front. Immunol. 2019, 10, 594. [Google Scholar] [CrossRef]
- Li, L.; Petrovsky, N. Molecular mechanisms for enhanced DNA vaccine immunogenicity. Expert Rev. Vaccines 2016, 15, 313–329. [Google Scholar] [CrossRef] [PubMed]
- Khalid, K.; Poh, C.L. The development of DNA vaccines against SARS-CoV-2. Adv. Med. Sci. 2023, 68, 213–226. [Google Scholar] [CrossRef] [PubMed]
- Karayianni, M.; Sentoukas, T.; Skandalis, A.; Pippa, N.; Pispas, S.; Khalid, K.; Poh, C.L. Chitosan-based nanoparticles for nucleic acid delivery: Technological aspects, applications, and future perspectives. Pharmaceutics 2023, 15, 1849. [Google Scholar] [CrossRef]
- Al-Dosari, M.S.; Gao, X. Nonviral gene delivery: Principle, limitations, and recent progress. AAPS J. 2009, 11, 671–681. [Google Scholar] [CrossRef]
- Kumar, U.S.; Afjei, R.; Ferrara, K.; Massoud, T.F.; Paulmurugan, R. Gold-Nanostar-Chitosan-Mediated Delivery of SARS-CoV-2 DNA Vaccine for Respiratory Mucosal Immunization: Development and Proof-of-Principle. ACS Nano 2021, 15, 17582–17601. [Google Scholar] [CrossRef]
- Safer, A.M.; Leporatti, S. Chitosan Nanoparticles for Antiviral Drug Delivery: A Novel Route for COVID-19 Treatment. Int. J. Nanomed. 2021, 16, 8141–8158. [Google Scholar] [CrossRef]
- Raghunath, I.; Koland, M.; Sarathchandran, C.; Saoji, S.; Rarokar, N. Design and optimization of chitosan-coated solid lipid nanoparticles containing insulin for improved intestinal permeability using piperine. Int. J. Biol. Macromol. 2024, 280 Pt 2, 135849. [Google Scholar] [CrossRef] [PubMed]
- Nunes, R.; Serra, A.S.; Simaite, A.; Sousa, Â. Modulation of Chitosan-TPP Nanoparticle Properties for Plasmid DNA Vaccines Delivery. Polymers 2022, 14, 1443. [Google Scholar] [CrossRef]
- Halarnekar, D.; Ayyanar, M.; Gangapriya, P.; Kalaskar, M.; Redasani, V.; Gurav, N.; Nadaf, S.; Saoji, S.; Rarokar, N.; Gurav, S. Eco synthesized chitosan/zinc oxide nanocomposites as the next generation of nano-delivery for antibacterial, antioxidant, antidiabetic potential, and chronic wound repair. Int. J. Biol. Macromol. 2023, 242, 124764. [Google Scholar] [CrossRef]
- Gong, X.; Gao, Y.; Shu, J.; Zhang, C.; Zhao, K. Chitosan-Based Nanomaterial as Immune Adjuvant and Delivery Carrier for Vaccines. Vaccines 2022, 10, 1906. [Google Scholar] [CrossRef] [PubMed]
- Kumar, G.; Virmani, T.; Misra, S.K.; Sharma, A.; Pathak, K. Exploration of chitosan and its modified derivatives as vaccine adjuvant: A review. Carbohydr. Polym. Technol. Appl. 2024, 8, 100537. [Google Scholar] [CrossRef]
- Cao, Y.; Tan, Y.F.; Wong, Y.S.; Liew, M.W.J.; Venkatraman, S. Recent advances in chitosan-based carriers for gene delivery. Mar. Drugs 2019, 17, 381. [Google Scholar] [CrossRef]
- Trejo-Santillan, I.; Mendoza-Guevara, C.C.; Ramos-Godinez, M.D.P.; Ramon-Gallegos, E. Biosecurity Test of Conjugated Nanoparticles of Chitosan-Protoporphyrin IX-Vitamin B9 for Their Use in Photodynamic Therapy. IEEE Trans. Nanobiosci. 2022, 21, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Vaezifar, S.; Razavi, S.; Golozar, M.A.; Karbasi, S.; Morshed, M.; Kamali, M. Effects of some parameters on particle size distribution of chitosan nanoparticles prepared by ionic gelation method. J. Clust. Sci. 2013, 24, 891–903. [Google Scholar] [CrossRef]
- Mendoza-Guevara, C.C.; Ramon-Gallegos, E.; Martinez-Escobar, A.; Alonso-Morales, R.; Ramos-Godinez, M.D.P.; Ortega, J. Attachment and in vitro transfection efficiency of an anti-rabies chitosan-DNA nanoparticle vaccine. IEEE Trans. Nanobiosci. 2022, 21, 105–116. [Google Scholar] [CrossRef]
- Banerjee, T.; Mitra, S.; Kumar Singh, A.; Kumar Sharma, R.; Maitra, A. Preparation, characterization, and biodistribution of ultrafine chitosan nanoparticles. Int. J. Pharm. 2002, 243, 93–105. [Google Scholar] [CrossRef]
- Han, Y.; Han, L.; Yao, Y.; Li, Y.; Liu, X. Key factors in FTIR spectroscopic analysis of DNA: The sampling technique, pretreatment temperature, and sample concentration. Anal. Methods 2018, 10, 2430–2437. [Google Scholar] [CrossRef]
- Liu, W.; Sun, S.; Cao, Z.; Zhang, X.; Yao, K.; Lu, W.W.; Luk, K.D. An investigation on the physicochemical properties of chitosan/DNA polyelectrolyte complexes. Biomaterials 2005, 26, 2705–2711. [Google Scholar] [CrossRef]
- Köping-Höggård, M.; Mel’nikova, Y.S.; Vårum, K.M.; Lindman, B.; Artursson, P. Relationship between the physical shape and the efficiency of oligomeric chitosan as a gene delivery system in vitro and in vivo. J. Gene Med. 2003, 5, 130–141. [Google Scholar] [CrossRef]
- Bodnar, M.; Hartmann, J.F.; Borbely, J. Preparation and characterization of chitosan-based nanoparticles. Biomacromolecules 2005, 6, 2521–2527. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Liu, N.; Wang, Z.; Gao, J.; Zhang, H.; Li, M.; Du, Y.; Gao, X.; Zheng, A. Development and optimization of chitosan nanoparticle-based intranasal vaccine carrier. Molecules 2021, 27, 204. [Google Scholar] [CrossRef]
- Dong, L.; Li, Y.; Cong, H.; Yu, B.; Shen, Y. A review of chitosan in gene therapy: Developments and challenges. Carbohydr. Polym. 2024, 324, 121562. [Google Scholar] [CrossRef]
- Alameh, M.; Lavertu, M.; Tran-Khanh, N.; Chang, C.Y.; Lesage, F.; Bail, M.; Darras, V.; Chevrier, A.; Buschmann, M.D. siRNA delivery with chitosan: Influence of chitosan molecular weight, degree of deacetylation, and amine to phosphate ratio on in vitro silencing efficiency, hemocompatibility, biodistribution, and in vivo efficacy. Biomacromolecules 2018, 19, 112–131. [Google Scholar] [CrossRef]
- Nimesh, S. 9-Chitosan nanoparticles. In Gene Therapy; Nimesh, S., Ed.; Woodhead Publishing: Cambridge, UK, 2013; pp. 163–196. [Google Scholar] [CrossRef]
- Nimesh, S.; Thibault, M.M.; Lavertu, M.; Buschmann, M.D. Enhanced gene delivery mediated by low molecular weight chitosan/DNA complexes: Effect of pH and serum. Mol. Biotechnol. 2010, 46, 182–196. [Google Scholar] [CrossRef] [PubMed]
- Aranda-Barradas, M.; Trejo-López, S.; Real, A.; Álvarez-Almazán, S.; Méndez-Albores, A.; García-Tovar, C.G.; González-Díaz, F.R.; Miranda-Castro, S.P. Effect of molecular weight of chitosan on the physicochemical, morphological, and biological properties of polyplex nanoparticles intended for gene delivery. Carbohydr. Polym. Technol. Appl. 2022, 4, 100228. [Google Scholar] [CrossRef]
- Mao, H.Q.; Roy, K.; Troung-Le, V.L.; Janes, K.A.; Lin, K.Y.; Wang, Y.; August, J.T.; Leong, K.W. Chitosan-DNA nanoparticles as gene carriers: Synthesis, characterization, and transfection efficiency. J. Control. Release 2001, 70, 399–421. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Yin, L.; Ding, J.; Tang, C.; Gu, S.; Yin, C.; Mao, Y. Thiolated trimethyl chitosan nanocomplexes as gene carriers with high in vitro and in vivo transfection efficiency. J. Control. Release 2010, 144, 46–54. [Google Scholar] [CrossRef]
- Malakooty Poor, E.; Baghaban Eslaminejad, M.; Gheibi, N.; Bagheri, F.; Atyabi, F. Chitosan–pDNA nanoparticle characteristics determine the transfection efficacy of gene delivery to human mesenchymal stem cells. Artif. Cells Nanomed. Biotechnol. 2014, 42, 376–384. [Google Scholar] [CrossRef]
- Karimzadeh, S.; Jafarizadeh-Malmiri, H.; Mokhtarzadeh, A. Chitosan nanoparticles synthesis and surface modification using histidine/polyethylenimine and evaluation of their gene transfection efficiency in breast cancer cells. Biologia 2022, 77, 841–849. [Google Scholar] [CrossRef]
- Çelik, S.; Gök, M.K.; Demir, K.; Pabuccuoğlu, S.; Özgümüş, S. Relationship between phosphorylamine-modification and molecular weight on transfection efficiency of chitosan. Carbohydr. Polym. 2022, 277, 118870. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Dong, D.; Zhang, C.; Deng, Y.; Ding, J.; Niu, S.; Tan, S.; Sun, L. Chitosan-functionalized poly(β-amino ester) hybrid system for gene delivery in vaginal mucosal epithelial cells. Pharmaceutics 2024, 16, 154. [Google Scholar] [CrossRef] [PubMed]
- Jha, R.; Mayanovic, R.A. A review of the preparation, characterization, and applications of chitosan nanoparticles in nanomedicine. Nanomaterials 2023, 13, 1302. [Google Scholar] [CrossRef]
- Seferian, P.G.; Martinez, M.L. Immune stimulating activity of two new chitosan containing adjuvant formulations. Vaccine 2000, 19, 661–668. [Google Scholar] [CrossRef]
- Kumar, M.; Behera, A.K.; Lockey, R.F.; Zhang, J.; Bhullar, G.; De La Cruz, C.P.; Chen, L.C.; Leong, K.W.; Huang, S.K.; Mohapatra, S.S. Intranasal gene transfer by chitosan-DNA nanospheres protects BALB/c mice against acute respiratory syncytial virus infection. Hum. Gene Ther. 2002, 13, 1415–1425. [Google Scholar] [CrossRef] [PubMed]
- Farris, E.; Brown, D.M.; Ramer-Tait, A.E.; Pannier, A.K. Micro- and nanoparticulates for DNA vaccine delivery. Exp. Biol. Med. 2016, 241, 919–929. [Google Scholar] [CrossRef]
- Lim, M.; Badruddoza, A.Z.M.; Firdous, J.; Azad, M.; Mannan, A.; Al-Hilal, T.A.; Cho, C.S.; Islam, M.A. Engineered nanodelivery systems to improve DNA vaccine technologies. Pharmaceutics 2020, 12, 30. [Google Scholar] [CrossRef]
- Demidenko, R.; Razanauskas, D.; Daniunaite, K.; Lazutka, J.R.; Jankevicius, F.; Jarmalaite, S. Frequent down-regulation of ABC transporter genes in prostate cancer. BMC Cancer 2015, 15, 683. [Google Scholar] [CrossRef]
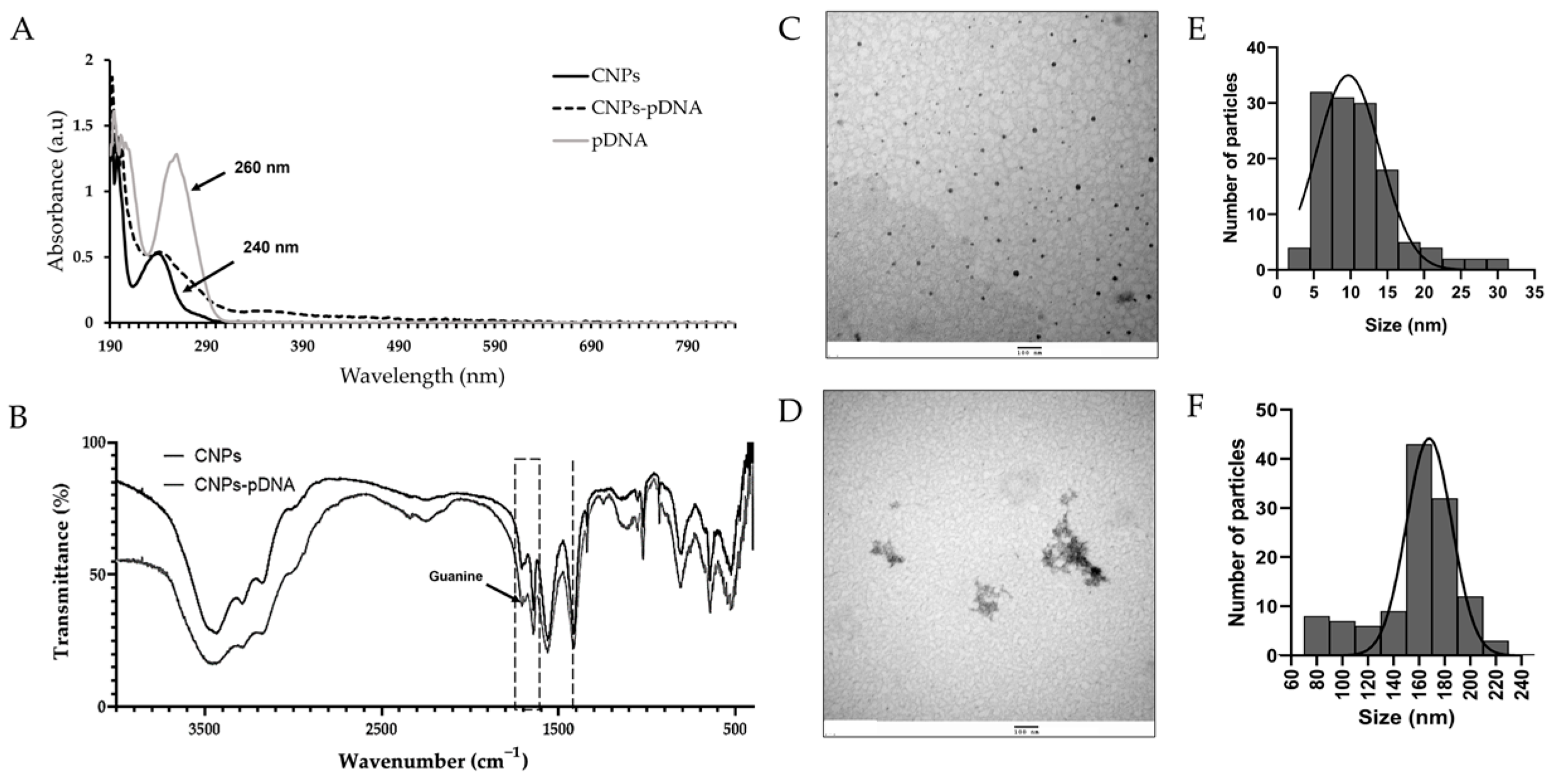

| Characterization | CNPs | CNPs-pDNA |
|---|---|---|
| TEM diameter (nm) | 11.1 ± 5.2 | 159.0 ± 33.1 |
| Hydrodynamic diameter (nm) | 397.6 ± 51.6 | 422.1 ± 12.4 |
| PDI | 0.6 ± 0.1 | 0.6 ± 0.1 |
| Zeta potential (mV) | 20.4 ± 0.6 | 19.7 ± 0.3 |
| Target Sequence (pb) | Primer | Sequence 5′-3′ | Cycling Conditions (40 Cycles) |
|---|---|---|---|
| Spike F1 (1974 bp) | Forward F1 | AGGGGTACTGCTGTTATGTC | 98 °C—15 s 56 °C—15 s 72 °C—120 s |
| Reverse F1 | ACACCCTGATAAAGAACAGC | ||
| Spike F2 (2208 bp) | Forward F2 | TCCAACAATTTGGCAGAGAC | 98 °C—15 s 57 °C—15 s 72 °C—120 s |
| Reverse F2 | TTGATTTCACCTTGCTTCAAAGTTAC | ||
| Spike F1 with NheI site (1850 bp) (a) | Forward S-RE | TGTTCTTGCTAGCAACTAAACGAAC | 98 °C—15 s 58 °C—20 s 72 °C—120 s |
| Reverse F1 | ACACCCTGATAAAGAACAGC | ||
| Spike F2 with SacI site (2153 bp) (b) | Forward F2 | TCCAACAATTTGGCAGAGAC | 98 °C—15 s 58 °C—20 s 72 °C—120 s |
| Reverse S-ER | ATCCATGAGCTCGTTTATGTGTAATG | ||
| Sequencing (397 bp) | Forward CMV | GCCCAGTACATGACCTTATGGG | 98 °C—15 s 60 °C—15 s 72 °C—20 s |
| Reverse CMV | GCCCAGTACATGACCTTATGGG | ||
| qPCR Spike (160 bp) | Forward qPCR-Spike | TAGGGCGTGATCTCCCTCAG | 98 °C—15 s 63 °C—17 s 72 °C—15 s |
| Reverse qPCR-Spike | TAAGCTGCAGCACCAGCTGT | ||
| qPCR GAPDH (146 bp) | Forward qPCR-GAPDH | AGGTCGGAGTCAACGGATTT | 98 °C—15 s 63 °C—17 s 72 °C—15 s |
| Reverse qPCR-GAPDH | ATGGGTGGAATCATATTGGAAC |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendoza-Guevara, C.C.; Martinez-Escobar, A.; Ramos-Godínez, M.d.P.; Muñoz-Medina, J.E.; Ramon-Gallegos, E. Efficient Delivery of SARS-CoV-2 Plasmid DNA in HEK-293T Cells Using Chitosan Nanoparticles. Pharmaceuticals 2025, 18, 683. https://doi.org/10.3390/ph18050683
Mendoza-Guevara CC, Martinez-Escobar A, Ramos-Godínez MdP, Muñoz-Medina JE, Ramon-Gallegos E. Efficient Delivery of SARS-CoV-2 Plasmid DNA in HEK-293T Cells Using Chitosan Nanoparticles. Pharmaceuticals. 2025; 18(5):683. https://doi.org/10.3390/ph18050683
Chicago/Turabian StyleMendoza-Guevara, Citlali Cecilia, Alejandro Martinez-Escobar, María del Pilar Ramos-Godínez, José Esteban Muñoz-Medina, and Eva Ramon-Gallegos. 2025. "Efficient Delivery of SARS-CoV-2 Plasmid DNA in HEK-293T Cells Using Chitosan Nanoparticles" Pharmaceuticals 18, no. 5: 683. https://doi.org/10.3390/ph18050683
APA StyleMendoza-Guevara, C. C., Martinez-Escobar, A., Ramos-Godínez, M. d. P., Muñoz-Medina, J. E., & Ramon-Gallegos, E. (2025). Efficient Delivery of SARS-CoV-2 Plasmid DNA in HEK-293T Cells Using Chitosan Nanoparticles. Pharmaceuticals, 18(5), 683. https://doi.org/10.3390/ph18050683






