Safety of Inclisiran: A Disproportionality Analysis from the EudraVigilance Database
Abstract
1. Introduction
2. Results
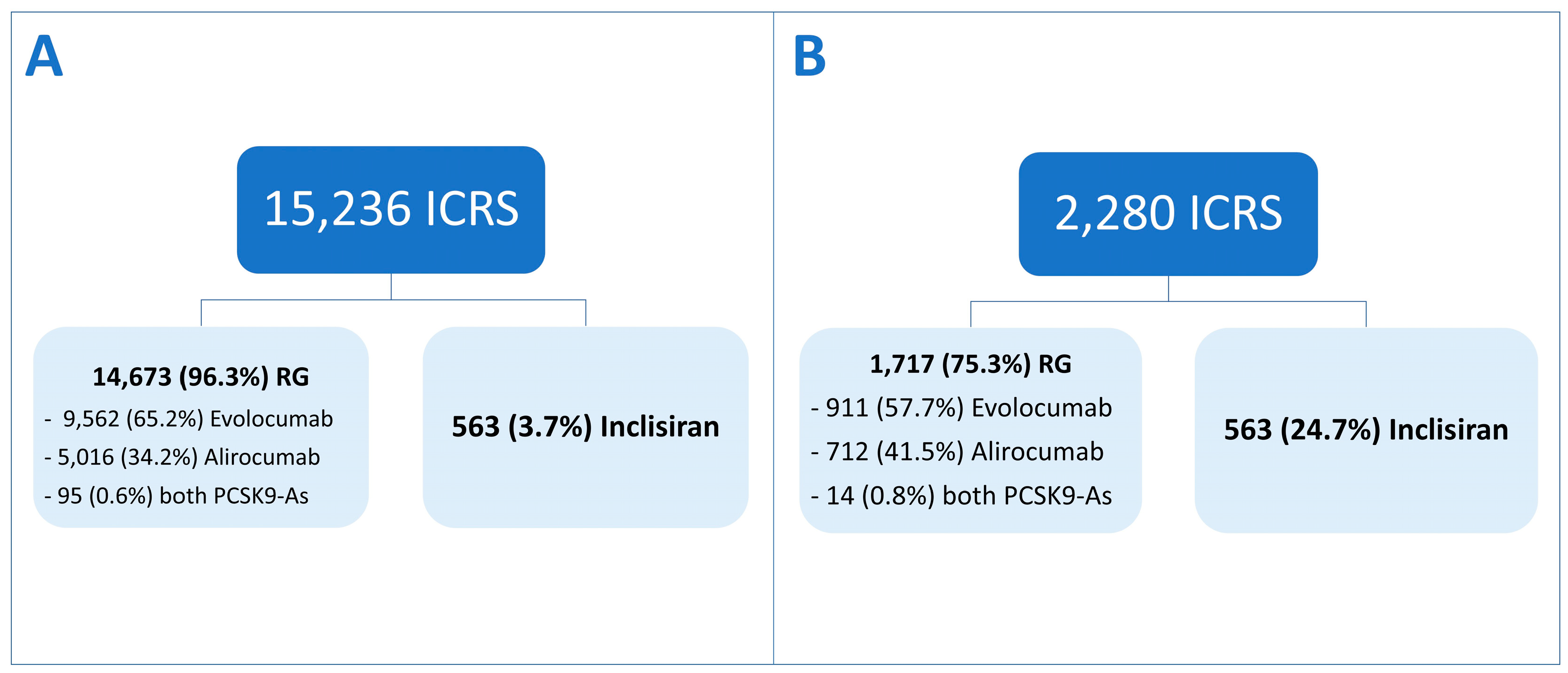
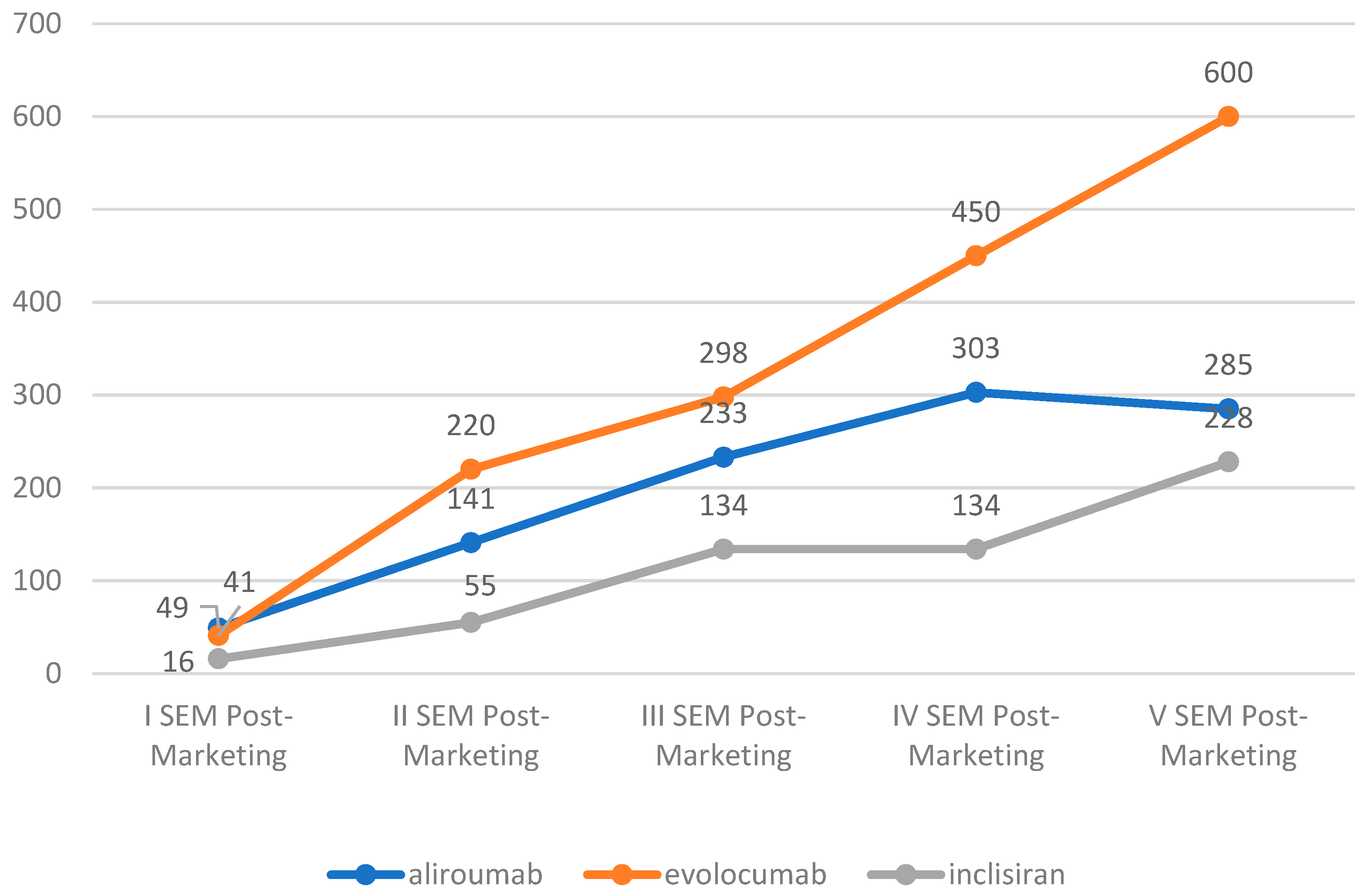
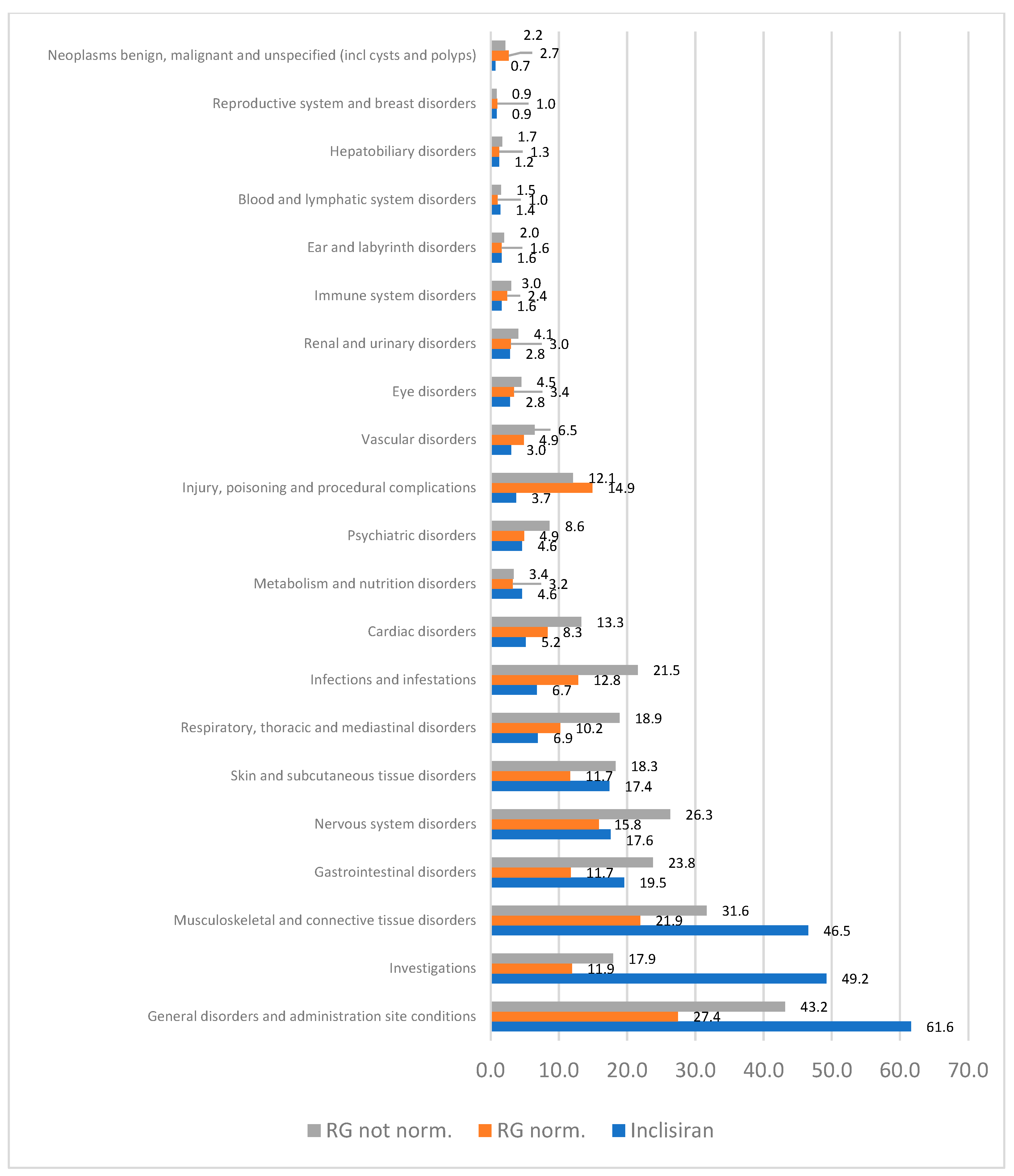
2.1. Descriptive Analysis
2.2. Disproportionality Analysis
3. Discussion
3.1. Descriptive Analysis
3.2. ADRs of Clinical Interest
3.2.1. Myalgia Related ADRs
3.2.2. Drug Ineffectiveness
3.2.3. Weight Gain
3.2.4. Injection-Site Reactions
3.2.5. Changes in Liver Functions
3.2.6. Strengths and Limitations
4. Materials and Methods
4.1. Data Source and Selection Process
4.2. Reports Selection
4.3. Data Characteristics
4.4. Data Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias: Lipid Modification to Reduce Cardiovascular Risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, 625. [Google Scholar] [CrossRef]
- Ridker, P.M.; Mora, S.; Rose, L. Percent Reduction in LDL Cholesterol Following High-Intensity Statin Therapy: Potential Implications for Guidelines and for the Prescription of Emerging Lipid-Lowering Agents. Eur. Heart J. 2016, 37, 1373–1379. [Google Scholar] [CrossRef]
- Byrne, P.; Demasi, M.; Jones, M.; Smith, S.M.; O’Brien, K.K.; DuBroff, R. Evaluating the Association Between Low-Density Lipoprotein Cholesterol Reduction and Relative and Absolute Effects of Statin Treatment. JAMA Intern. Med. 2022, 182, 474. [Google Scholar] [CrossRef]
- Bitto, A.; Pallio, G.; Messina, S.; Arcoraci, V.; Pizzino, G.; Russo, G.T.; Pallio, S.; Squadrito, F.; Altavilla, D. Genomic Variations Affecting Biological Effects of Statins. Curr. Drug Metab. 2016, 17, 566–572. [Google Scholar] [CrossRef]
- Ferrajolo, C.; Arcoraci, V.; Sullo, M.G.; Rafaniello, C.; Sportiello, L.; Ferrara, R.; Cannata, A.; Pagliaro, C.; Tari, M.G.; Caputi, A.P.; et al. Pattern of Statin Use in Southern Italian Primary Care: Can Prescription Databases Be Used for Monitoring Long-Term Adherence to the Treatment? PLoS ONE 2014, 9, e102146. [Google Scholar] [CrossRef]
- Piacentini, N.; Trifiró, G.; Tari, M.; Moretti, S.; Arcoraci, V. Statin-Macrolide Interaction Risk: A Population-Based Study throughout a General Practice Database. Eur. J. Clin. Pharmacol. 2005, 61, 615–620. [Google Scholar] [CrossRef]
- Zhang, H.; Plutzky, J.; Skentzos, S.; Morrison, F.; Mar, P.; Shubina, M.; Turchin, A. Discontinuation of Statins in Routine Care Settings. Ann. Intern. Med. 2013, 158, 526. [Google Scholar] [CrossRef]
- Rottura, M.; Scondotto, G.; Barbieri, M.A.; Sorbara, E.E.; Nasso, C.; Marino, S.; Scoglio, R.; Mandraffino, G.; Pallio, G.; Irrera, N.; et al. Management of High Cardiovascular Risk in Diabetic Patients: Focus on Low Density Lipoprotein Cholesterol and Appropriate Drug Use in General Practice. Front. Cardiovasc. Med. 2021, 8, 749686. [Google Scholar] [CrossRef]
- Rottura, M.; Molonia, A.; Giorgi, D.A.; Marino, S.; Scoglio, R.; Pallio, G.; Irrera, N.; Imbalzano, E.; Altavilla, D.; Squadrito, G.; et al. Pharmacological Treatment of Diabetic and Non-Diabetic Patients with Coronary Artery Disease in the Real World of General Practice. Front. Pharmacol. 2022, 13, 858385. [Google Scholar] [CrossRef]
- Boekholdt, S.M.; Hovingh, G.K.; Mora, S.; Arsenault, B.J.; Amarenco, P.; Pedersen, T.R.; LaRosa, J.C.; Waters, D.D.; DeMicco, D.A.; Simes, R.J.; et al. Very Low Levels of Atherogenic Lipoproteins and the Risk for Cardiovascular Events. J. Am. Coll. Cardiol. 2014, 64, 485–494. [Google Scholar] [CrossRef]
- Warden, B.A.; Fazio, S.; Shapiro, M.D. The PCSK9 Revolution: Current Status, Controversies, and Future Directions. Trends Cardiovasc. Med. 2020, 30, 179–185. [Google Scholar] [CrossRef]
- Cupido, A.J.; Kastelein, J.J.P. Inclisiran for the Treatment of Hypercholesterolaemia: Implications and Unanswered Questions from the ORION Trials. Cardiovasc. Res. 2020, 116, e136–e139. [Google Scholar] [CrossRef]
- Cohen, J.C.; Boerwinkle, E.; Mosley, T.H.; Hobbs, H.H. Sequence Variations in PCSK9, Low LDL, and Protection against Coronary Heart Disease. N. Engl. J. Med. 2006, 354, 1264–1272. [Google Scholar] [CrossRef]
- Bao, X.; Liang, Y.; Chang, H.; Cai, T.; Feng, B.; Gordon, K.; Zhu, Y.; Shi, H.; He, Y.; Xie, L. Targeting Proprotein Convertase Subtilisin/Kexin Type 9 (PCSK9): From Bench to Bedside. Signal Transduct. Target. Ther. 2024, 9, 13. [Google Scholar] [CrossRef]
- Reyes-Soffer, G.; Pavlyha, M.; Ngai, C.; Thomas, T.; Holleran, S.; Ramakrishnan, R.; Karmally, W.; Nandakumar, R.; Fontanez, N.; Obunike, J.; et al. Effects of PCSK9 Inhibition with Alirocumab on Lipoprotein Metabolism in Healthy Humans. Circulation 2017, 135, 352–362. [Google Scholar] [CrossRef]
- Watts, G.F.; Chan, D.C.; Dent, R.; Somaratne, R.; Wasserman, S.M.; Scott, R.; Burrows, S.; Barrett, P.H.R. Factorial Effects of Evolocumab and Atorvastatin on Lipoprotein Metabolism. Circulation 2017, 135, 338–351. [Google Scholar] [CrossRef]
- European Medicnes Agency Summary of Product Characteristics—Praluent. Available online: https://www.ema.europa.eu/en/documents/product-information/praluent-epar-product-information_en.pdf (accessed on 27 March 2024).
- European Medicines Agency Summary of Product Characteristics—Repatha. Available online: https://www.ema.europa.eu/en/documents/product-information/repatha-epar-product-information_en.pdf (accessed on 27 March 2024).
- Roth, E.M.; Davidson, M.H. PCSK9 Inhibitors: Mechanism of Action, Efficacy, and Safety. Rev. Cardiovasc. Med. 2018, 19, 31–46. [Google Scholar] [CrossRef]
- Moriarty, P.M.; Jacobson, T.A.; Bruckert, E.; Thompson, P.D.; Guyton, J.R.; Baccara-Dinet, M.T.; Gipe, D. Efficacy and Safety of Alirocumab, a Monoclonal Antibody to PCSK9, in Statin-Intolerant Patients: Design and Rationale of ODYSSEY ALTERNATIVE, a Randomized Phase 3 Trial. J. Clin. Lipidol. 2014, 8, 554–561. [Google Scholar] [CrossRef]
- Raal, F.J.; Honarpour, N.; Blom, D.J.; Hovingh, G.K.; Xu, F.; Scott, R.; Wasserman, S.M.; Stein, E.A. Inhibition of PCSK9 with Evolocumab in Homozygous Familial Hypercholesterolaemia (TESLA Part B): A Randomised, Double-Blind, Placebo-Controlled Trial. Lancet 2015, 385, 341–350. [Google Scholar] [CrossRef]
- Blom, D.J.; Hala, T.; Bolognese, M.; Lillestol, M.J.; Toth, P.D.; Burgess, L.; Ceska, R.; Roth, E.; Koren, M.J.; Ballantyne, C.M.; et al. A 52-Week Placebo-Controlled Trial of Evolocumab in Hyperlipidemia. N. Engl. J. Med. 2014, 370, 1809–1819. [Google Scholar] [CrossRef]
- European Medicines Agency Summary of Product Characteristics—Leqvio. Available online: https://www.ema.europa.eu/en/documents/product-information/leqvio-epar-product-information_en.pdf (accessed on 27 March 2024).
- Lamb, Y.N. Inclisiran: First Approval. Drugs 2021, 81, 389–395. [Google Scholar] [CrossRef]
- German, C.A.; Shapiro, M.D. Small Interfering RNA Therapeutic Inclisiran: A New Approach to Targeting PCSK9. BioDrugs 2020, 34, 1–9. [Google Scholar] [CrossRef]
- Nair, J.K.; Willoughby, J.L.S.; Chan, A.; Charisse, K.; Alam, M.R.; Wang, Q.; Hoekstra, M.; Kandasamy, P.; Kel’in, A.V.; Milstein, S.; et al. Multivalent N. -Acetylgalactosamine-Conjugated SiRNA Localizes in Hepatocytes and Elicits Robust RNAi-Mediated Gene Silencing. J. Am. Chem. Soc. 2014, 136, 16958–16961. [Google Scholar] [CrossRef]
- Dyrbuś, K.; Gąsior, M.; Penson, P.; Ray, K.K.; Banach, M. Inclisiran—New Hope in the Management of Lipid Disorders? J. Clin. Lipidol. 2020, 14, 16–27. [Google Scholar] [CrossRef]
- Raal, F.J.; Kallend, D.; Ray, K.K.; Turner, T.; Koenig, W.; Wright, R.S.; Wijngaard, P.L.J.; Curcio, D.; Jaros, M.J.; Leiter, L.A.; et al. Inclisiran for the Treatment of Heterozygous Familial Hypercholesterolemia. N. Engl. J. Med. 2020, 382, 1520–1530. [Google Scholar] [CrossRef]
- Ray, K.K.; Landmesser, U.; Leiter, L.A.; Kallend, D.; Dufour, R.; Karakas, M.; Hall, T.; Troquay, R.P.T.; Turner, T.; Visseren, F.L.J.; et al. Inclisiran in Patients at High Cardiovascular Risk with Elevated LDL Cholesterol. N. Engl. J. Med. 2017, 376, 1430–1440. [Google Scholar] [CrossRef]
- Luo, M.; Liu, Y.; Xu, X.; Liu, K.; Shen, C.; Hu, H.; He, Z.; Wu, F. Efficacy and Safety of Inclisiran in Stroke or Cerebrovascular Disease Prevention: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Pharmacol. 2023, 14, 1158274. [Google Scholar] [CrossRef]
- Khan, S.A.; Naz, A.; Qamar Masood, M.; Shah, R. Meta-Analysis of Inclisiran for the Treatment of Hypercholesterolemia. Am. J. Cardiol. 2020, 134, 69–73. [Google Scholar] [CrossRef]
- Hovingh, G.K.; Lepor, N.E.; Kallend, D.; Stoekenbroek, R.M.; Wijngaard, P.L.J.; Raal, F.J. Inclisiran Durably Lowers Low-Density Lipoprotein Cholesterol and Proprotein Convertase Subtilisin/Kexin Type 9 Expression in Homozygous Familial Hypercholesterolemia. Circulation 2020, 141, 1829–1831. [Google Scholar] [CrossRef]
- Fitzgerald, K.; White, S.; Borodovsky, A.; Bettencourt, B.R.; Strahs, A.; Clausen, V.; Wijngaard, P.; Horton, J.D.; Taubel, J.; Brooks, A.; et al. A Highly Durable RNAi Therapeutic Inhibitor of PCSK9. N. Engl. J. Med. 2017, 376, 41–51. [Google Scholar] [CrossRef]
- Ray, K.K.; Wright, R.S.; Kallend, D.; Koenig, W.; Leiter, L.A.; Raal, F.J.; Bisch, J.A.; Richardson, T.; Jaros, M.; Wijngaard, P.L.J.; et al. Two Phase 3 Trials of Inclisiran in Patients with Elevated LDL Cholesterol. N. Engl. J. Med. 2020, 382, 1507–1519. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, J.; Wang, S. Comparative Effectiveness of Inclisiran 100, 300, and 500 Mg in a Population with Hyperlipidemia: A Network Meta-Analysis of Randomized Controlled Trials. Am. J. Cardiovasc. Drugs 2018, 18, 271–282. [Google Scholar] [CrossRef]
- di Mauro, G.; Zinzi, A.; Scavone, C.; Mascolo, A.; Gaio, M.; Sportiello, L.; Ferrajolo, C.; Rafaniello, C.; Rossi, F.; Capuano, A. PCSK9 Inhibitors and Neurocognitive Adverse Drug Reactions: Analysis of Individual Case Safety Reports from the Eudravigilance Database. Drug Saf. 2021, 44, 337–349. [Google Scholar] [CrossRef]
- Hoffman, K.B.; Dimbil, M.; Erdman, C.B.; Tatonetti, N.P.; Overstreet, B.M. The Weber Effect and the United States Food and Drug Administration’s Adverse Event Reporting System (FAERS): Analysis of Sixty-Two Drugs Approved from 2006 to 2010. Drug Saf 2014, 37, 283–294. [Google Scholar] [CrossRef]
- Chamberlain, A.M.; Gong, Y.; Shaw, K.M.; Bian, J.; Song, W.; Linton, M.F.; Fonseca, V.; Price-Haywood, E.; Guhl, E.; King, J.B.; et al. PCSK9 Inhibitor Use in the Real World: Data from the National Patient-Centered Research Network. J. Am. Heart Assoc. 2019, 8, 11246. [Google Scholar] [CrossRef]
- Piccinni, C.; Antonazzo, I.C.; Maggioni, A.P.; Pedrini, A.; Calabria, S.; Ronconi, G.; Dondi, L.; Martini, N.; Roberto, G.; Sampietro, T.; et al. PCSK9 Inhibitors’ New Users: Analysis of Prescription Patterns and Patients’ Characteristics from an Italian Real-World Study. Clin. Drug Investig. 2020, 40, 173–181. [Google Scholar] [CrossRef]
- Sabatine, M.S.; Giugliano, R.P.; Wiviott, S.D.; Raal, F.J.; Blom, D.J.; Robinson, J.; Ballantyne, C.M.; Somaratne, R.; Legg, J.; Wasserman, S.M.; et al. Efficacy and Safety of Evolocumab in Reducing Lipids and Cardiovascular Events. N. Engl. J. Med. 2015, 372, 1500–1509. [Google Scholar] [CrossRef]
- Raschi, E.; Moretti, U.; Salvo, F.; Pariente, A.; Cosimo Antonazzo, I.; De Ponti, F.; Poluzzi, E. Evolving Roles of Spontaneous Reporting Systems to Assess and Monitor Drug Safety. In Pharmacovigilance; IntechOpen: London, UK, 2019. [Google Scholar]
- Osservatorio Nazionale sull’impiego dei Medicinali L’uso Dei Farmaci in Italia: Rapporto Nazionale Anno 2022. Available online: https://www.aifa.gov.it/documents/20142/1967301/Rapporto-OsMed-2022.pdf (accessed on 27 March 2024).
- Ray, K.K.; Troquay, R.P.T.; Visseren, F.L.J.; Leiter, L.A.; Scott Wright, R.; Vikarunnessa, S.; Talloczy, Z.; Zang, X.; Maheux, P.; Lesogor, A.; et al. Long-Term Efficacy and Safety of Inclisiran in Patients with High Cardiovascular Risk and Elevated LDL Cholesterol (ORION-3): Results from the 4-Year Open-Label Extension of the ORION-1 Trial. Lancet Diabetes Endocrinol. 2023, 11, 109–119. [Google Scholar] [CrossRef]
- He, Y.; Guan, X.; Zhang, Y.; Zhu, Z.; Zhang, Y.; Feng, Y.; Li, X. Analysis of Inclisiran in the US FDA Adverse Event Reporting System (FAERS): A Focus on Overall Patient Population and Sex-Specific Subgroups. Expert. Opin. Drug Saf. 2024, 1–9. [Google Scholar] [CrossRef]
- Ji, C.; Bai, J.; Zhou, J.; Zou, Y.; Yu, M. Adverse Event Profiles of PCSK9 Inhibitors Alirocumab and Evolocumab: Data Mining of the FDA Adverse Event Reporting System. Br. J. Clin. Pharmacol. 2022, 88, 5317–5325. [Google Scholar] [CrossRef]
- Mulder, J.W.C.M.; Galema-Boers, A.M.H.; Roeters van Lennep, J.E. First Clinical Experiences with Inclisiran in a Real-World Setting. J. Clin. Lipidol. 2023, 17, 818–827. [Google Scholar] [CrossRef]
- Karatasakis, A.; Danek, B.A.; Karacsonyi, J.; Rangan, B.V.; Roesle, M.K.; Knickelbine, T.; Miedema, M.D.; Khalili, H.; Ahmad, Z.; Abdullah, S.; et al. Effect of PCSK9 Inhibitors on Clinical Outcomes in Patients with Hypercholesterolemia: A Meta-Analysis of 35 Randomized Controlled Trials. J. Am. Heart Assoc. 2017, 6, 6910. [Google Scholar] [CrossRef]
- Li, W.; Sun, L.; Yan, S. PCSK9 Inhibitors and Inclisiran with or without Statin Therapy on Incident Muscle Symptoms and Creatine Kinase: A Systematic Review and Network Meta-Analysis. Front. Cardiovasc. Med. 2024, 11, 1375040. [Google Scholar] [CrossRef]
- Makhmudova, U.; Schatz, U.; Perakakis, N.; Kassner, U.; Schumann, F.; Axthelm, C.; Stürzebecher, P.; Sinning, D.L.; Doevelaar, A.; Rohn, B.; et al. High Interindividual Variability in LDL-Cholesterol Reductions after Inclisiran Administration in a Real-World Multicenter Setting in Germany. Clin. Res. Cardiol. 2023, 112, 1639–1649. [Google Scholar] [CrossRef]
- Altschmiedová, T.; Todorovová, V.; Šnejdrlová, M.; Šatný, M.; Češka, R. PCSK9 Inhibitors in Real-World Practice: Analysis of Data from 314 Patients and 2 Years of Experience in a Center of Preventive Cardiology. Curr. Atheroscler. Rep. 2022, 24, 357–363. [Google Scholar] [CrossRef]
- Zafrir, B.; Jubran, A. Lipid-lowering Therapy with PCSK 9-inhibitors in the Real-world Setting: Two-year Experience of a Regional Lipid Clinic. Cardiovasc. Ther. 2018, 36, 12439. [Google Scholar] [CrossRef]
- Figarska, S.M.; Rigdon, J.; Ganna, A.; Elmståhl, S.; Lind, L.; Gardner, C.D.; Ingelsson, E. Proteomic Profiles before and during Weight Loss: Results from Randomized Trial of Dietary Intervention. Sci. Rep. 2020, 10, 7913. [Google Scholar] [CrossRef]
- Filippatos, T.D.; Liberopoulos, E.; Georgoula, M.; Tellis, C.; Tselepis, A.D.; Elisaf, M. Effects of Increased Body Weight and Short-Term Weight Loss on Serum PCSK9 Levels—A Prospective Pilot Study. Arch. Med. Sci.—Atheroscler. Dis. 2017, 2, 46–51. [Google Scholar] [CrossRef]
- Tóth, Š.; Fedačko, J.; Pekárová, T.; Hertelyová, Z.; Katz, M.; Mughees, A.; Kuzma, J.; Štefanič, P.; Kopolovets, I.; Pella, D. Elevated Circulating PCSK9 Concentrations Predict Subclinical Atherosclerotic Changes in Low Risk Obese and Non-Obese Patients. Cardiol. Ther. 2017, 6, 281–289. [Google Scholar] [CrossRef]
- Li, J.; Lei, X.; Li, Z.; Yang, X. Effectiveness and Safety of Inclisiran in Hyperlipidemia Treatment: An Overview of Systematic Reviews. Medicine 2023, 102, e32728. [Google Scholar] [CrossRef]
- Padda, I.S.; Mahtani, A.U.; Patel, P.; Parmar, M. Small Interfering RNA (SiRNA) Therapy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK580472/ (accessed on 27 March 2024).
- Guedeney, P.; Giustino, G.; Sorrentino, S.; Claessen, B.E.; Camaj, A.; Kalkman, D.N.; Vogel, B.; Sartori, S.; De Rosa, S.; Baber, U.; et al. Efficacy and Safety of Alirocumab and Evolocumab: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Eur. Heart J. 2022, 43, e17–e25. [Google Scholar] [CrossRef]
- Cicala, G.; de Filippis, R.; Barbieri, M.A.; Cutroneo, P.M.; De Fazio, P.; Schoretsanitis, G.; Spina, E. Tolerability Profile of Paliperidone Palmitate Formulations: A Pharmacovigilance Analysis of the EUDRAVigilance Database. Front. Psychiatry 2023, 14, 1130636. [Google Scholar] [CrossRef]
- Pal, S.N.; Duncombe, C.; Falzon, D.; Olsson, S. WHO Strategy for Collecting Safety Data in Public Health Programmes: Complementing Spontaneous Reporting Systems. Drug Saf. 2013, 36, 75–81. [Google Scholar] [CrossRef]
- Moore, N.; Berdaï, D.; Blin, P.; Droz, C. Pharmacovigilance—The next Chapter. Therapies 2019, 74, 557–567. [Google Scholar] [CrossRef]
- Coste, J. Diverging Approaches of Pharmacovigilance and Pharmacoepidemiology to Assessing Drug Safety: Epistemological and Ethical Implications. Pharmacoepidemiol. Drug Saf. 2017, 26, 600–602. [Google Scholar] [CrossRef]
- Cicala, G.; Barbieri, M.A.; Santoro, V.; Tata, C.; Colucci, P.V.; Vanadia, F.; Drago, F.; Russo, C.; Cutroneo, P.M.; Gagliano, A.; et al. Safety and Tolerability of Antipsychotic Drugs in Pediatric Patients: Data From a 1-Year Naturalistic Study. Front. Psychiatry 2020, 11, 1–9. [Google Scholar] [CrossRef]
- Monaco, L.; Biagi, C.; Conti, V.; Melis, M.; Donati, M.; Venegoni, M.; Vaccheri, A.; Motola, D. Safety Profile of the Direct Oral Anticoagulants: An Analysis of the WHO Database of Adverse Drug Reactions. Br. J. Clin. Pharmacol. 2017, 83, 1532–1543. [Google Scholar] [CrossRef]
- Barbieri, M.A.; Sorbara, E.E.; Russo, G.; Cicala, G.; Franchina, T.; Santarpia, M.; Silvestris, N.; Spina, E. Neuropsychiatric Adverse Drug Reactions with Tyrosine Kinase Inhibitors in Gastrointestinal Stromal Tumors: An Analysis from the European Spontaneous Adverse Event Reporting System. Cancers 2023, 15, 1851. [Google Scholar] [CrossRef]
- Zhang, X.; Feng, Y.; Li, F.; Ding, J.; Tahseen, D.; Hinojosa, E.; Chen, Y.; Tao, C. Evaluating MedDRA-to-ICD Terminology Mappings. BMC Med. Inform. Decis. Mak. 2024, 23, 299. [Google Scholar] [CrossRef]
- Mascolo, A.; Scavone, C.; Ferrajolo, C.; Rafaniello, C.; Danesi, R.; Del Re, M.; Russo, A.; Coscioni, E.; Rossi, F.; Alfano, R.; et al. Immune Checkpoint Inhibitors and Cardiotoxicity: An Analysis of Spontaneous Reports in Eudravigilance. Drug Saf. 2021, 44, 957–971. [Google Scholar] [CrossRef]
| Characteristics | Inclisiran ICSRs N 563 (%) | RG Norm N (%) | p-Value Inclisiran vs. RG Norm | RG No-Norm N (%) | p-Value Inclisiran vs. RG No-Norm |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 264 (48.3) | 779 (47.2) | 0.653 | 6475 (46.1) | 0.313 |
| Female | 283 (51.7) | 873 (52.8) | 0.653 | 7579 (53.9) | 0.313 |
| Age categories (years) | |||||
| <65 | 112 (52.8) | 520 (42.9) | 0.014 | 3877 (42.8) | 0.003 |
| ≥65 | 100 (47.2) | 670 (57.1) | 0.014 | 5204 (57.2) | 0.003 |
| Unknown | 351 (62.3) | 505 (29.4) | - | 5599 (38.1) | - |
| Seriousness | |||||
| Serious | 141 (25.0) | 1406 (81.9) | <0.001 | 8634 (58.8) | <0.001 |
| Non-serious | 422 (75.0) | 311 (18.1) | <0.001 | 6039 (41.2) | <0.001 |
| Outcome | |||||
| Fatal | 4 (1.3) | 62 (6.7) | <0.001 | 305 (4.4) | 0.009 |
| Not Recovered/Not Resolved | 123 (40.6) | 320 (34.7) | 0.064 | 2522 (36.7) | 0.171 |
| Recovered with Sequelae | 5 (1.7) | 2 (0.2) | 0.004 | 39 (0.6) | 0.018 |
| Recovering/Resolving | 55 (18.2) | 135 (14.6) | 0.143 | 1165 (16.9) | 0.585 |
| Recovered/Resolved | 116 (38.3) | 403 (43.7) | 0.097 | 2838 (41.3) | 0.293 |
| Unknown | 260 (46.2) | 795 (46.3) | - | 3677 (25.1) | - |
| Primary Source Qualification | |||||
| Healthcare Professional | 486 (86.3) | 1336 (77.8) | <0.001 | 10967 (74.7) | <0.001 |
| Non-Healthcare Professional | 77 (13.7) | 381 (22.2) | <0.001 | 3706 (25.3) | <0.001 |
| Country | |||||
| European Economic Area | 495 (87.9) | 484 (28.2) | <0.001 | 7012 (47.7) | <0.001 |
| Non-European Economic Area | 68 (12.1) | 1233 (71.8) | <0.001 | 7685 (52.3) | <0.001 |
| Preferred Terms | N | Inclisiran vs. RG Norm. ROR [95%CI] | Inclisiran vs. RG No-Norm. ROR [95%CI] | Exp. |
|---|---|---|---|---|
| Drug intolerance | 13 | 13.50 [3.83, 47.56] | 5.30 [2.95, 9.85] | No |
| Low-density lipoprotein increased | 89 | 13.25 [8.34, 21.03] | 11.95 [9.10, 15.52] | No |
| Injection-site erythema | 35 | 8.06 [4.31, 15.10] | 5.19 [3.58, 7.53] | Yes |
| Drug ineffective | 51 | 6.74 [4.14, 10.99] | 6.37 [4.64, 8.74] | No |
| Liver function test increased | 13 | 5.05 [2.08, 12.25] | 13.85 [7.05, 27.22] | No |
| Injection-site pruritus | 17 | 4.83 [2.25, 10.37] | 4.01 [2.39, 6.73] | No |
| Injection-site reaction | 15 | 4.25 [1.94, 9.20] | 5.71 [3.25, 10.04] | Yes |
| Weight increased | 13 | 4.03 [1.76, 9.25] | 2.40 [1.35, 4.26] | No |
| Injection-site pain | 27 | 3.88 [2.19, 6.87] | 1.55 [1.04, 2.30] | Yes |
| Blood cholesterol increased | 19 | 3.71 [1.89, 7.27] | 3.94 [2.41, 6.42] | No |
| Drug effect less than expected | 8 | 3.52 [1.27, 9.75] | 3.14 [1.50, 6.57] | No |
| Transaminases increased | 7 | 3.59 [1.20, 10.73] | 4.98 [2.21, 11.22] | No |
| Inappropriate schedule of product administration | 7 | 3.59 [1.20, 10.73] | 2.66 [1.22, 5.83] | No |
| Blood triglycerides increased | 13 | 3.36 [1.52, 7.40] | 5.00 [2.75, 9.10] | No |
| Myalgia | 99 | 2.42 [1.83, 3.10] | 2.43 [1.94, 3.04] | No |
| Pain in extremity | 24 | 1.69 [1.02, 2.81] | 1.55 [1.02, 2.36] | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cicala, G.; Rottura, M.; Gianguzzo, V.M.; Cristiano, F.; Drago, S.F.A.; Pallio, G.; Irrera, N.; Imbalzano, E.; Spina, E.; Arcoraci, V. Safety of Inclisiran: A Disproportionality Analysis from the EudraVigilance Database. Pharmaceuticals 2024, 17, 1365. https://doi.org/10.3390/ph17101365
Cicala G, Rottura M, Gianguzzo VM, Cristiano F, Drago SFA, Pallio G, Irrera N, Imbalzano E, Spina E, Arcoraci V. Safety of Inclisiran: A Disproportionality Analysis from the EudraVigilance Database. Pharmaceuticals. 2024; 17(10):1365. https://doi.org/10.3390/ph17101365
Chicago/Turabian StyleCicala, Giuseppe, Michelangelo Rottura, Viviana Maria Gianguzzo, Federica Cristiano, Selene Francesca Anna Drago, Giovanni Pallio, Natasha Irrera, Egidio Imbalzano, Edoardo Spina, and Vincenzo Arcoraci. 2024. "Safety of Inclisiran: A Disproportionality Analysis from the EudraVigilance Database" Pharmaceuticals 17, no. 10: 1365. https://doi.org/10.3390/ph17101365
APA StyleCicala, G., Rottura, M., Gianguzzo, V. M., Cristiano, F., Drago, S. F. A., Pallio, G., Irrera, N., Imbalzano, E., Spina, E., & Arcoraci, V. (2024). Safety of Inclisiran: A Disproportionality Analysis from the EudraVigilance Database. Pharmaceuticals, 17(10), 1365. https://doi.org/10.3390/ph17101365








