Preparation Strategies of the Anti-Mycobacterial Drug Bedaquiline for Intrapulmonary Routes of Administration
Abstract
1. Introduction
2. Results and Discussion
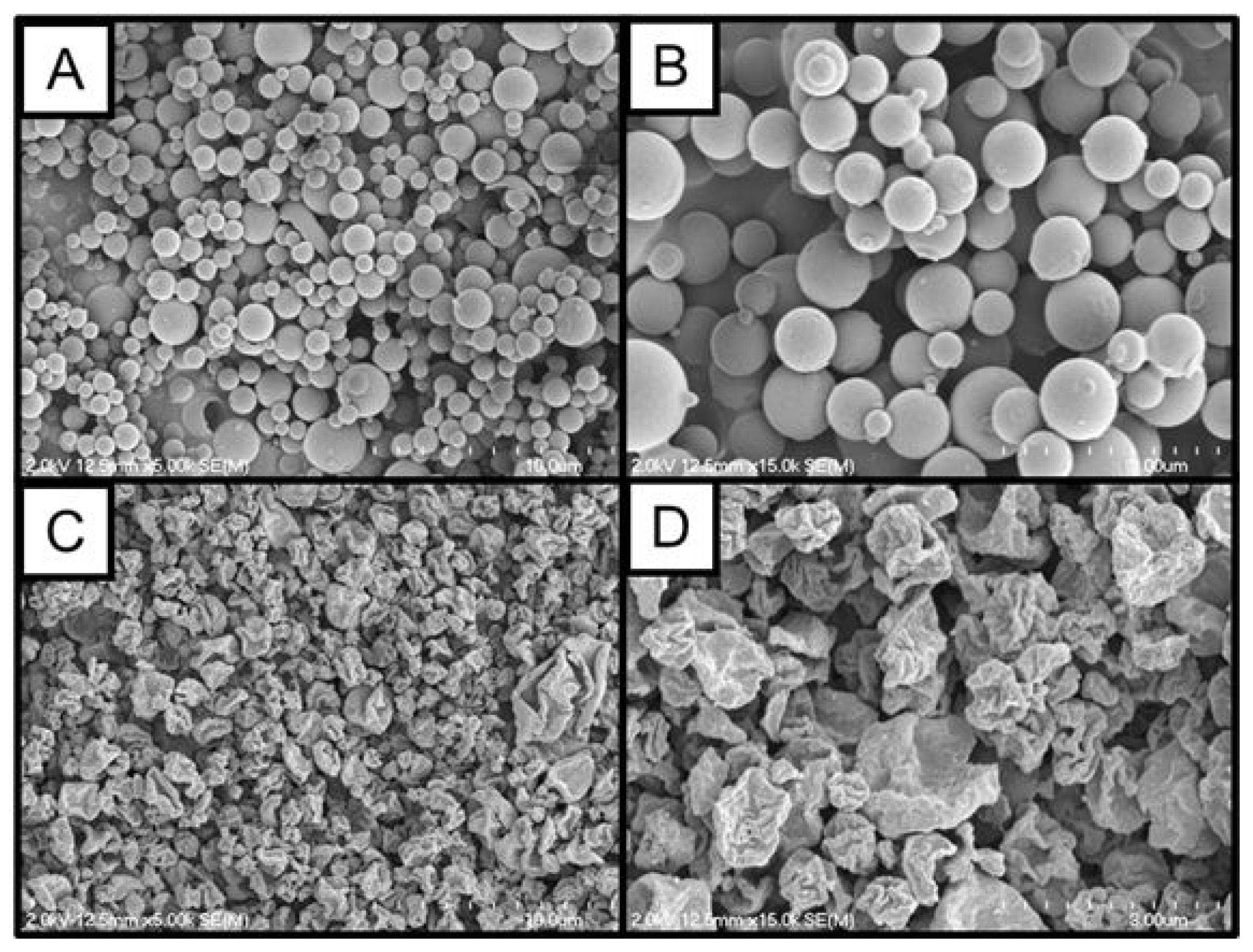
2.1. Powder Manufacture and Particle Morphology
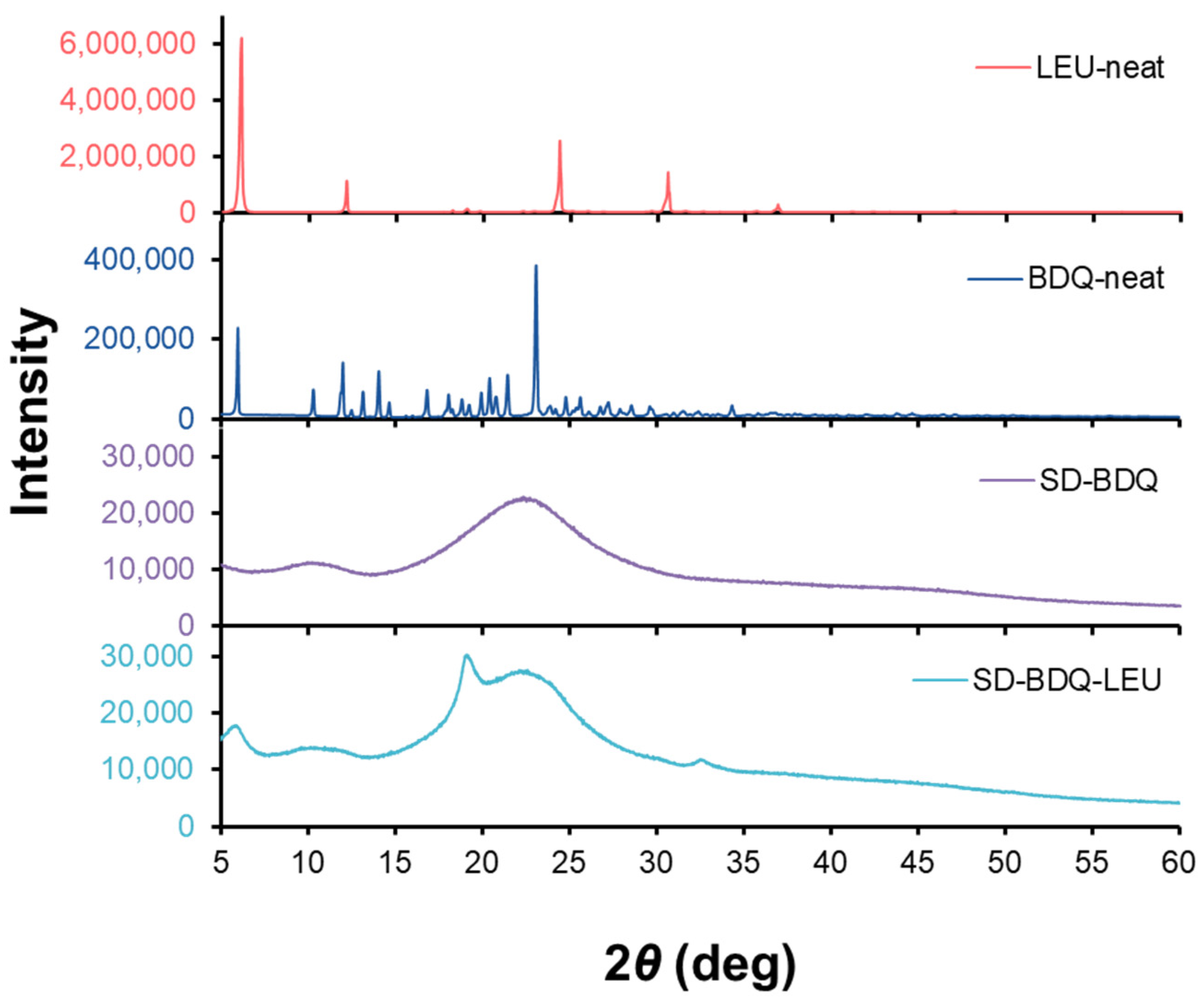
2.2. Physicochemical Characterization of Spray-Dried BDQ Powder
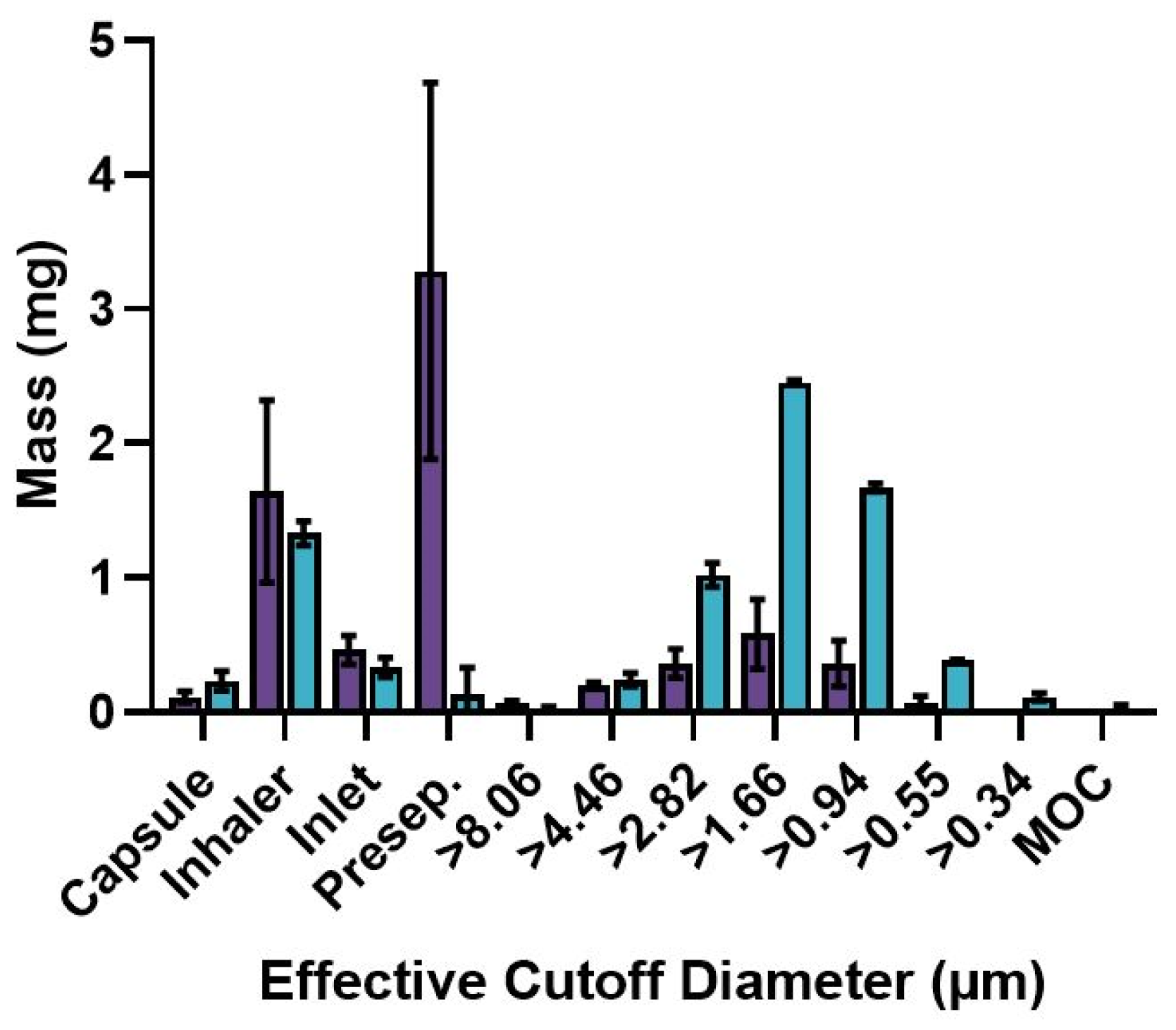
2.3. Aerodynamic Properties of Spray-Dried BDQ Powder
2.4. Preparation of Aqueous BDQ Solution
2.5. Stability of BDQ Formulations
2.6. In Vivo Pharmacokinetic Comparison of Liquid and Powder Delivery of BDQ
3. Materials and Methods
3.1. Materials
3.2. Preparation of BDQ Dry Powder Aerosol
3.3. Morphological Characterization
3.4. Thermal Analysis
3.5. Crystallinity
3.6. Aerodynamic Performance Characterization
3.7. Dosator Preparation
3.8. Preparation of Aqueous BDQ Solution
3.9. Stability Analysis
3.10. In Vivo Pharmacokinetic Study
3.11. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Tuberculosis Report 2022; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Chahine, E.B.; Karaoui, L.R.; Mansour, H. Bedaquiline: A novel diarylquinoline for multidrug-resistant tuberculosis. Ann. Pharmacother. 2014, 48, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Sun, F.; Zhang, W. Bedaquiline and delamanid in the treatment of multidrug-resistant tuberculosis: Promising but challenging. Drug Dev. Res. 2019, 80, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Momin, M.A.M.; Rangnekar, B.; Larson, I.; Sinha, S.; Das, S.C. Dry powder formulation combining bedaquiline with pyrazinamide for latent and drug-resistant tuberculosis. Adv. Powder Technol. 2019, 30, 2473–2482. [Google Scholar] [CrossRef]
- Diacon, A.H.; Pym, A.; Grobusch, M.; Patienta, R.; Rustomjee, R.; Page-Shipp, L.; Pistorius, C.; Krause, R.; Bogoshi, M.; Churchyard, G.; et al. The diarylquinoline TMC207 for multidrug-resistant tuberculosis. N. Engl. J. Med. 2009, 360, 2397–2405. [Google Scholar] [CrossRef] [PubMed]
- Fox, G.J.; Menzies, D. A review of the evidence for using bedaquiline (TMC207) to treat multi-drug resistant tuberculosis. Infect. Dis. Ther. 2013, 2, 123–144. [Google Scholar] [CrossRef]
- Field, S.K. Bedaquiline for the treatment of multidrug-resistant tuberculosis: Great promise or disappointment. Ther. Adv. Chronic Dis. 2015, 6, 170–184. [Google Scholar] [CrossRef]
- Diacon, A.H.; Pym, A.; Grobusch, M.P.; de los Rios, J.M.; Gotuzzo, E.; Vasilyeva, I.; Leimane, V.; Andries, K.; Bakare, N.; De Marez, T.; et al. Multidrug-resistant tuberculosis and culture conversion with bedaquiline. N. Engl. J. Med. 2014, 371, 723–732. [Google Scholar] [CrossRef]
- Chesov, D.; Heyckendorf, J.; Alexandru, S.; Donica, A.; Chesov, E.; Reiman, M.; Crudu, V.; Botnaru, V.; Lange, C. Impact of bedaquiline on treatment outcomes of multidrug-resistant tuberculosis in a high-burden country. Eur. Respir. J. 2020, 57, 2002544. [Google Scholar] [CrossRef]
- Pontali, E.; Sotgiu, G.; D’Ambrosio, L.; Centis, R.; Battista Migliori, G. Bedaquiline and multidrug-resistant tuberculosis: A systematic and critical analysis of the evidence. Eur. Respir. J. 2016, 47, 394–402. [Google Scholar] [CrossRef]
- Zhao, Y.; Li, F.; Liu, Y.; Shi, Y.; Li, Z.; Cao, G.; Zhu, W. Comparison of efficacy of inhaled and intravenous corticosteroid on pregnant women with COPD and the effects on the expression of PCT and hs-CRP. Exp. Ther. Med. 2018, 15, 4717–4722. [Google Scholar]
- Borghardt, J.M.; Kloft, C.; Sharma, A. Inhaled therapy in respiratory diseases: The complex interplay of pulmonary kinetic processes. Can. Respir. J. 2018, 2018, 2732017. [Google Scholar] [CrossRef]
- Videira, M.A.; Llop, J.; Sousa, C.; Kreutzer, B.; Cossio, U.; Forbes, B.; Vieira, I.; Gil, N.; Silva-Lima, B. Pulmonary administration: Strengthening the value of therapeutic proximity. Front. Med. 2020, 7, 50. [Google Scholar] [CrossRef] [PubMed]
- Rawal, T.; Patel, S.; Butani, S. Chitosan nanoparticles as a promising approach for pulmonary delivery of bedaquiline. Eur. J. Pharm. Sci. 2018, 124, 273–287. [Google Scholar] [CrossRef] [PubMed]
- Maloney, S.E.; Mecham, J.B.; Hickey, A.J. Performance Testing for Dry Powder Inhaler Products: Towards Clinical Relevance. KONA Powder Part. J. 2023, 40, 172–185. [Google Scholar] [CrossRef]
- Momin, M.A.M.; Rangnekar, B.; Sinha, S.; Cheung, C.-Y.; Cook, G.M.; Das, S.C. Inhalable dry powder of bedaquiline for pulmonary tuberculosis: In vitro physicochemical characterization, antimicrobial activity and safety studies. Pharmaceutics 2019, 11, 502. [Google Scholar] [CrossRef]
- Rangnekar, B.; Momin, M.A.M.; Eedara, B.B.; Sinha, S.; Das, S.C. Bedaquiline containing triple combination powder for inhalation to treat drug-resistant tuberculosis. Int. J. Pharm. 2019, 570, 118689. [Google Scholar] [CrossRef] [PubMed]
- Okezue, M.A.; Byrn, S.J.; Clase, K.L. Determining the solubilities for benzoate, nicotinate, hydrochloride, and malonate salts of bedaquiline. Int. J. Pharm. 2022, 627, 122229. [Google Scholar] [CrossRef]
- BUCHI Labortechnik AG. B-290 Mini Spray Dryer Operation Manual; BUCHI Labortechnik AG: Flawil, Switzerland, 2020. [Google Scholar]
- Alhajj, N.; O’Reilly, N.J.; Cathcart, H. Leucine as an excipient in spray dried powder for inhalation. Drug Discov. Today 2021, 26, 2384–2396. [Google Scholar] [CrossRef]
- Seville, P.C.; Learoyd, T.P.; Li, H.Y.; Williamson, I.J.; Birchall, J.C. Amino acid-modified spray-dried powders with enhanced aerosolization properties for pulmonary drug delivery. Powder Technol. 2007, 178, 40–50. [Google Scholar] [CrossRef]
- Wolfenden, R.; Andersson, L.; Cullis, P.M.; Southgate, C.C.B. Affinities of amino acid side chains for solvent water. Biochemistry 1981, 20, 849–855. [Google Scholar] [CrossRef]
- Glinski, J.; Chavepeyer, G.; Platten, J.K. Surface properties of aqeuous solutions of L-leucine. Biophys. Chem. 2000, 84, 99–103. [Google Scholar] [CrossRef]
- Chew, N.Y.; Chan, H.K. Use of solid corrugated particles to enhance powder aerosol performance. Pharm. Res. 2001, 18, 1570–1577. [Google Scholar] [CrossRef]
- Peng, T.; Lin, S.; Niu, B.; Wang, X.; Huang, Y.; Zhang, X.; Li, G.; Pan, X.; Wu, C. Influence of physical properties of carrier on the performance of dry powder inhalers. Acta Pharm. Sin. B 2016, 6, 308–318. [Google Scholar] [CrossRef]
- Weiler, C.; Egen, M.; Trunk, M.; Langguth, P. Force control and powder dispersibility of spray dried particles for inhalation. J. Pharm. Sci. 2010, 99, 303–316. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Li, X.; Mansour, H.M. Surface analytical techniques in solid-state particle characterization for predicting performance in dry powder inhalers. KONA Powder Part. J. 2010, 28, 3–18. [Google Scholar] [CrossRef]
- Chaurasiya, B.; Zhao, Y.-Y. Dry powder for pulmonary delivery: A comprehensive review. Pharmaceutics 2021, 13, 31. [Google Scholar] [CrossRef]
- Stewart, I.E.; Lukka, P.B.; Liu, J.; Meibohm, B.; Gonzalez-Juarrero, M.; Braunstein, M.S.; Lee, R.E.; Hickey, A.J. Development and characterization of a dry powder formulation for anti-tuberculosis drug spectinamide 1599. Pharm. Res. 2019, 36, 136. [Google Scholar] [CrossRef] [PubMed]
- Maloney, S.E.; Alshiraihi, I.M.; Singh, A.; Stewart, I.E.; Mariner Gonzalez, J.; Gonzalez-Juarrero, M.; Meibohm, B.; Hickey, A.J. Spray dried tigecycline dry powder aerosols for the treatment of nontuberculous mycobacterial pulmonary infections. Tuberculosis 2023, 139, 102306. [Google Scholar] [CrossRef] [PubMed]
- Stewart, I.E.; Durham, P.G.; Sittenauer, J.M.; Barreda, A.P.; Stowell, G.W.; Moody, C.; Mecham, J.B.; Simpson, C.; Daily, S.; Maloney, S.E.; et al. Optimization and scale up of spray dried CPZEN-45 aerosol powders for inhaled tuberculosis treatment. Pharm. Res. 2022, 39, 3359–3370. [Google Scholar] [CrossRef]
- Maa, Y.-F.; Nguyen, P.-A.; Andya, J.D.; Dasovich, N.; Sweeney, T.D.; Shire, S.J.; Hsu, C.C. Effect of spray drying and subsequent processing conditions on residual mositure content and physical/biochemical stability of protein inhalation powders. Pharm. Res. 1998, 15, 768–775. [Google Scholar] [CrossRef]
- Okezue, M.; Bogdanowich-Knipp, S.; Smith, D.; Zeller, M.; Byrn, S.; Smith, P.; Purcell, D.K.; Clase, K. Salts and Polymorph Screens for Bedaquiline. AAPS PharmSciTech 2021, 22, 228. [Google Scholar] [CrossRef]
- Shetty, N.; Cipolla, D.; Park, H.; Zhou, Q.T. Physical stability of dry powder inhaler formulations. Expert Opin. Drug Deliv. 2020, 17, 77–96. [Google Scholar] [CrossRef]
- Chen, L.; Okuda, T.; Lu, X.-Y.; Chan, H.-K. Amorphous powders for inhalation drug delivery. Adv. Drug Deliv. Rev. 2016, 100, 102–115. [Google Scholar] [CrossRef] [PubMed]
- Chang, R.Y.K.; Chen, L.; Chen, D.; Chan, H.-K. Overcoming challenges for development of amorphous powders for inhalation. Expert Opin. Drug Deliv. 2020, 17, 1583–1595. [Google Scholar] [CrossRef] [PubMed]
- Andries, K.; Verhasselt, P.; Guillemont, J.; Gohlmann, H.W.H.; Neefs, J.-M.; Winkler, H.; Van Gestel, J.; Timmerman, P.; Zhu, M.; Lee, E.; et al. A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science 2005, 307, 223–227. [Google Scholar] [CrossRef]
- Hirayama, F.; Uekama, K. Cyclodextrin-based controlled drug release system. Adv. Drug Deliv. Rev. 1999, 36, 125–141. [Google Scholar] [CrossRef]
- Vyas, A.; Saraf, S.; Saraf, S. Cyclodextrin based novel drug delivery systems. J. Incl. Phenom. Macrocycl. Chem. 2008, 62, 23–42. [Google Scholar] [CrossRef]
- Lenaerts, A.J.; Hoff, D.; Aly, S.; Ehlers, S.; Andries, K.; Cantarero, L.; Orme, I.M.; Basaraba, R.J. Location of persisting mycobacteria in a guinea pig model of tuberculosis revealed by R207910. Antimicrob. Agents Chemother. 2007, 51, 3338–3345. [Google Scholar] [CrossRef] [PubMed]
- Durham, P.G.; Hanif, S.N.; Contreras, L.G.; Young, E.F.; Braunstein, M.S.; Hickey, A.J. Disposable dosators for pulmonary insufflation of therapeutic agents to small animals. JoVE 2017, 121, e55356. [Google Scholar]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maloney, S.E.; Stewart, I.E.; Podell, B.K.; Gary, H.E.; Mecham, J.B.; Berube, B.J.; Baldwin, S.L.; Coler, R.N.; Hickey, A.J. Preparation Strategies of the Anti-Mycobacterial Drug Bedaquiline for Intrapulmonary Routes of Administration. Pharmaceuticals 2023, 16, 729. https://doi.org/10.3390/ph16050729
Maloney SE, Stewart IE, Podell BK, Gary HE, Mecham JB, Berube BJ, Baldwin SL, Coler RN, Hickey AJ. Preparation Strategies of the Anti-Mycobacterial Drug Bedaquiline for Intrapulmonary Routes of Administration. Pharmaceuticals. 2023; 16(5):729. https://doi.org/10.3390/ph16050729
Chicago/Turabian StyleMaloney, Sara E., Ian E. Stewart, Brendan K. Podell, Hadley E. Gary, Jeffrey B. Mecham, Bryan J. Berube, Susan L. Baldwin, Rhea N. Coler, and Anthony J. Hickey. 2023. "Preparation Strategies of the Anti-Mycobacterial Drug Bedaquiline for Intrapulmonary Routes of Administration" Pharmaceuticals 16, no. 5: 729. https://doi.org/10.3390/ph16050729
APA StyleMaloney, S. E., Stewart, I. E., Podell, B. K., Gary, H. E., Mecham, J. B., Berube, B. J., Baldwin, S. L., Coler, R. N., & Hickey, A. J. (2023). Preparation Strategies of the Anti-Mycobacterial Drug Bedaquiline for Intrapulmonary Routes of Administration. Pharmaceuticals, 16(5), 729. https://doi.org/10.3390/ph16050729