SUMOtherapeutics for Ischemic Stroke
Abstract
1. Introduction
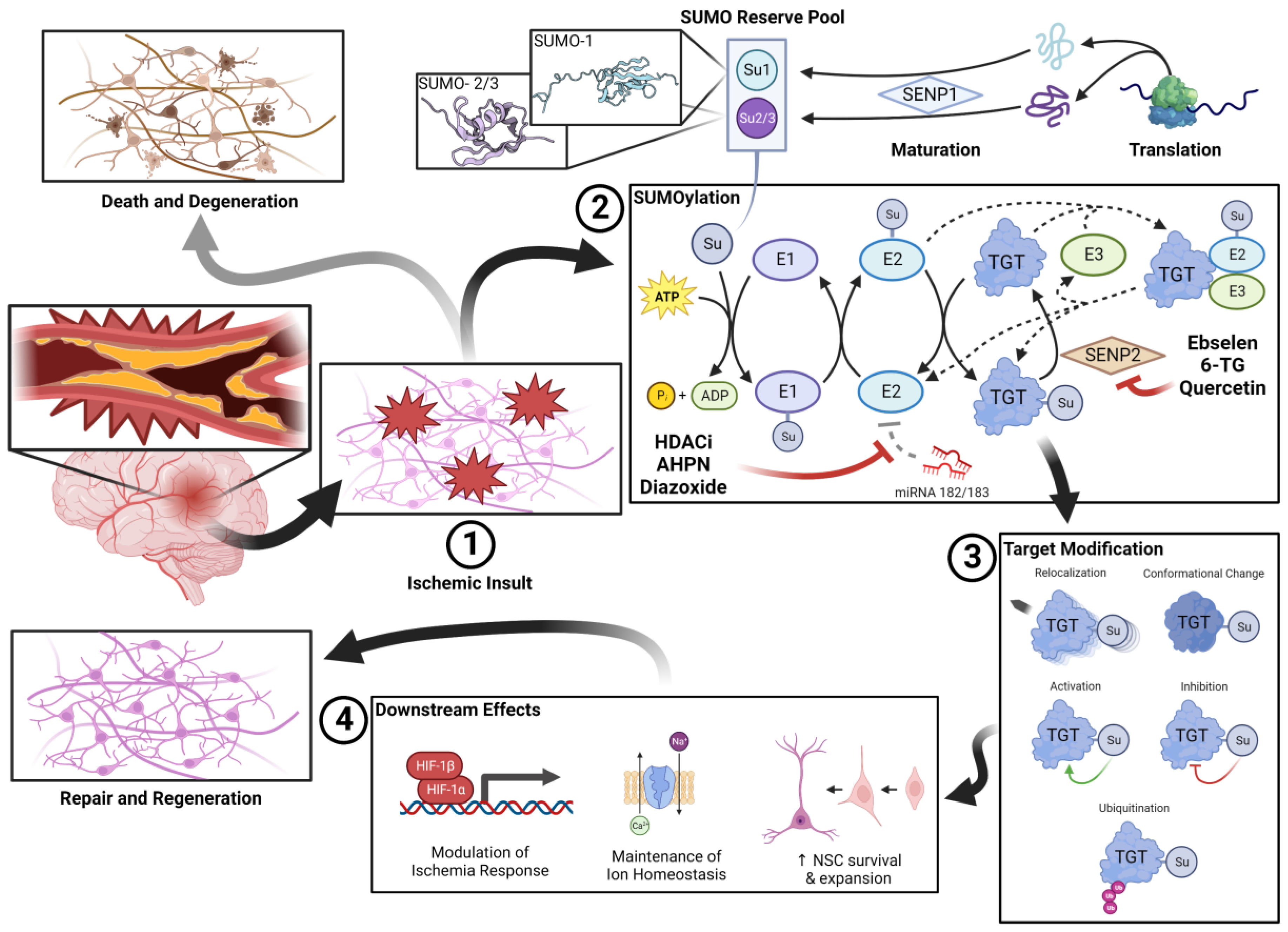
1.1. Biological Significance of the SUMO Pathway
1.2. Role of SUMO in Neuroprotection
1.2.1. SUMO and the Ischemia Response
1.2.2. Maintenance of Ion Homeostasis
1.2.3. Preservation of Neural Stem Cell Populations
2. SUMOtherapeutics for Cerebral Ischemia
2.1. miRNA-182/183 Inhibitors
| Drug | Tissue/ Animal | Ischemia Model | Intervention | Measured Outcome | Results Summary | Study |
|---|---|---|---|---|---|---|
| Orotic Acid | SHSY5Y, E18 PCN | SHSY5Y: 15 h OGD + 6 h recoveryE18 PCN: 5 h OGD + 16 h recovery | Drug co-treatment | Cell survival, SUMO concentration | SUMO upregulation *, OGD protection * | Bernstock et al., 2016 [75] |
| AHPN | ||||||
| Telmisartan | ||||||
| TW-37 | ||||||
| Dianiline | ||||||
| Diazoxide | ||||||
| NCGC00185916 | SUMO upregulation * | |||||
| Romidepsin | ||||||
| VX-702 | ||||||
| Lenalidomide | ||||||
| Belinostat | ||||||
| Pracinostat | ||||||
| Licofelone | ||||||
| Fosmidomycin | ||||||
| JWH-015 | ||||||
| Motesanib | ||||||
| Vatalanib | ||||||
| Entinostat | ||||||
| Panobinostat | ||||||
| Entinostat | CD-1 mice | Photothrombotic stroke at PMCA | Drug post-treatment (post stroke day 5–15) | Motor recovery, infarct volumes | No difference vs. negative control for both measures | Al Shoyaib et al., 2016 [80] |
| Collagenase-induced ICH | Drug post-treatment (1 h post stroke, 10 mg/kg IP in PBS) | Sensorimotor deficit score, CD16/32 expression, neurodegeneration (via TUNEL staining neurons), infarct volume | Reduction in day 1 and day 3 post-ICH sensorimotor deficit *. Reduction in CD16/32 expression *, neurodegeneration, and infarct volume * | Bonsack and Sukumari-Ramesh, 2021 [81] | ||
| Diazoxide | Wistar rats | 1.5 h MCAO | Drug pretreatment (15 min prior to stroke, 30 μL 0.4 mM or 2 mM ICV bolus) | 24 h post-stroke neurological score, infarct volume | Increase in neurological score *; reduction in infarct volume * | Shimizu et al., 2002 [82] |
| SD rats | 1 h RCCA ligation + hemorrhagic shock | Drug pre- and post-treatment: 5 mg/kg IP bolus 24 h pre-stroke; 2.3 mg/kg/10 min IV infusion 10 min or 60 min posttreatment | HSP25 and 70 concentrations | Pretreatment: upregulation of HSP25 and 70 *; 60 min posttreatment: upregulation of HSP25 and 70 * | O’Sullivan et al., 2007 [83] |
2.2. SENP Inhibitors
| Drug | Tissue/ Animal | Ischemia Model | Intervention | Measured Outcome | Results Summary | Study |
|---|---|---|---|---|---|---|
| Quercetin | SHSY5Y, B35, E18 PCN | SHSY5Y, B35: 16 h OGD + 5 h recovery E18 PCN: 5 h OGD + 16 h recovery | Drug treatment ± pre-treatment | SENP activity, SUMOylation, cell survival, LDH release | Decrease in SENP expression *; increase in SUMOylation *; increase in cell survival (in SHSY5Y and E18 PCN) *; decrease in LDH release with co-treatment alone and with pre-treatment * | Lee et al., 2016 [86] |
| Isoprenaline HCl | B35 | 20 h OGD | 4 h pretreatment + treatment | SUMO-1 expression, cell survival | Increase in SUMO-2/3 conjugation *, no significant OGD protection | Bernstock et al., 2018 [84] |
| Ethyl protocatechuate | SUMO-1 upregulation *, OGD protection * | |||||
| 6-thioguanine | C57BL6 mice | N/A | 12 mg/kg IP bolus treatment | SUMOylation 1 h after bolus | Increases in SUMO-1 and SUMO-2/3 conjugation * | |
| Ebselen | SHRSP, WKY rat PDN | 24 h OGD + 3 h recovery | treatment + 3 h posttreatment | Cell survival, LDH activity | OGD protection *, no significant difference in LDH activity | Yamagata et al., 2008 [98] |
| SHRSP, WKY rat | 0.5 h BCCO | 30 mg/kg/day pretreatment for 7 days, then 30 mg/kg/day posttreatment for 3 days | Apoptotic neurons in CA1 subfield of hippocampus | Almost complete inhibition of apoptosis † | ||
| N/A | 60 mg/kg/day treatment for 6 weeks | Oxidative stress (via cortical NO and MDA concentrations); iNOS expression | Reduction in NO and MDA concentrations *; reduction in iNOS expression * | Sui et al., 2005 [99] | ||
| Human | MCAO | 150 mg PO BID post-treatment within 12 h of onset for 2 weeks. Placebo controlled, double blind trial. | Infarct volume 1 mo post stroke, GOS 3 mo post stroke | Reduction in infarct volume *; superior GOS if administered within 6 h *; no significant difference in GOS vs. negative control overall | Ogawa et al., 1999 [91] | |
| AIS | 150 mg PO BID posttreatment within 48 h of onset for 2 weeks. Placebo controlled, double blind trial. | GOS (1- and 3-month), neurological status (2 weeks, modified Mathew Scale), functional status (2 weeks, Barthel Index) | Improvement in 1-month GOS * but no significant difference in 3-month GOS; superior GOS if administered ≤24 h *; reduction in both impairment (Mathew) * and disability (Barthel) * | Yamaguchi et al., 1998 [92] | ||
| SD rats | Permanent MCAO | 1 mg/kg/h pretreatment 45 min pre-stroke to 4 h post-stroke | Extent of ischemic damage, oxidative stress (via IHC) | 28% reduction in cortical ischemic damage vs. control †; reduction in oxidative stress markers vs. control † | Imai et al., 2003 [100] | |
| 2 h FCI | 1 mg/kg IV bolus + 1 mg/kg/h IV post-treatment for 24 h | 24 h neurological deficit, gray matter damage, Axonal damage, and oxidative stress (via IHC) | 40.7% reduced neurological deficit at 24 h vs. control *; 53.6% reduction in gray matter damage *; 46.8% reduction in axonal damage IHC markers * | Imai et al., 2001 [101] | ||
| Wistar rats | 45 min BCCO | 30 mg/kg PO bolus pretreatment 2 h prior to stroke | cortical EAA and NO concentrations, 24 h hippocampal CA1 subfield integrity | Increase in intact CA1 neurons *; no difference in EAA or NO concentrations vs. control. | Koizumi et al., 2011 [89] | |
| 2 h FCI | 10 mg/kg and 100 mg/kg PO bolus pretreatment 1 h prior to FCI | Reduced glutathione concentration; plasma Selenium; 1 week post stroke infarct size | Increase in perfusion with 100 mg/kg *; increase in plasma Selenium * | Salom et al., 2004 [102] | ||
| Wistar rat cerebellar neurons | Glutamate exposure | 25 min treatment ± posttreatment; posttreatment | 24 h cell survival, 48 h cell survival | Increase in survival with treatment * and posttreatment * comparable to negative control | Porciúncula et al., 2001 [95] | |
| Wistar rat hippocampal neurons | 45 min OGD | Pretreatment and posttreatment | 3 h cell survival | Increase in survival with treatment * and post-treatment * comparable to negative control | Porciúncula et al., 2003 [96] |
2.3. Direct SUMO Upregulators
3. Near Future Innovation in SUMOtherapeutics
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef] [PubMed]
- Albers, G.W.; Marks, M.P.; Kemp, S.; Christensen, S.; Tsai, J.P.; Ortega-Gutierrez, S.; McTaggart, R.A.; Torbey, M.T.; Kim-Tenser, M.; Leslie-Mazwi, T.; et al. Thrombectomy for stroke at 6 to 16 h with selection by perfusion imaging. N. Engl. J. Med. 2018, 378, 708–718. [Google Scholar] [CrossRef]
- Nogueira, R.G.; Jadhav, A.P.; Haussen, D.C.; Bonafe, A.; Budzik, R.F.; Bhuva, P.; Yavagal, D.R.; Ribo, M.; Cognard, C.; Hanel, R.A.; et al. Thrombectomy 6 to 24 h after stroke with a mismatch between deficit and infarct. N. Engl. J. Med. 2018, 378, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Berkhemer, O.A.; Fransen, P.S.S.; Beumer, D.; van den Berg, L.A.; Lingsma, H.F.; Yoo, A.J.; Schonewille, W.J.; Vos, J.A.; Nederkoorn, P.J.; Wermer, M.J.H.; et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N. Engl. J. Med. 2015, 372, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Campbell, B.C.V.; Parsons, M.W.; Churilov, L.; Levi, C.R.; Hsu, C.; Kleinig, T.J.; Wijeratne, T.; Curtze, S.; Dewey, H.M.; et al. Thrombolysis guided by perfusion imaging up to 9 h after onset of stroke. N. Engl. J. Med. 2019, 380, 1795–1803. [Google Scholar] [CrossRef] [PubMed]
- Anand, S.K.; Benjamin, W.J.; Adapa, A.R.; Park, J.V.; Wilkinson, D.A.; Daou, B.J.; Burke, J.F.; Pandey, A.S. Trends in acute ischemic stroke treatments and mortality in the united states from 2012 to 2018. Neurosurg. Focus 2021, 51, E2. [Google Scholar] [CrossRef]
- Goyal, M.; Menon, B.K.; van Zwam, W.H.; Dippel, D.W.J.; Mitchell, P.J.; Demchuk, A.M.; Davalos, A.; Majoie, C.B.L.M.; van der Lugt, A.; de Miquel, M.A.; et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 2016, 387, 1723–1731. [Google Scholar] [CrossRef]
- Yoshimura, S.; Sakai, N.; Yamagami, H.; Uchida, K.; Beppu, M.; Toyoda, K.; Matsumaru, Y.; Matsumoto, Y.; Kimura, K.; Takeuchi, M.; et al. Endovascular therapy for acute stroke with a large ischemic region. N. Engl. J. Med. 2022, 386, 1303–1313. [Google Scholar] [CrossRef] [PubMed]
- Sarraj, A.; Hassan, A.E.; Abraham, M.G.; Ortega-Gutierrez, S.; Kasner, S.E.; Hussain, M.S.; Chen, M.; Blackburn, S.; Sitton, C.W.; Churilov, L.; et al. Trial of endovascular thrombectomy for large ischemic strokes. N. Engl. J. Med. 2023, 388, 1259–1271. [Google Scholar] [CrossRef] [PubMed]
- Huo, X.; Ma, G.; Tong, X.; Zhang, X.; Pan, Y.; Nguyen, T.N.; Yuan, G.; Han, H.; Chen, W.; Wei, M.; et al. Trial of endovascular therapy for acute ischemic stroke with large infarct. N. Engl. J. Med. 2023, 388, 1272–1283. [Google Scholar] [CrossRef] [PubMed]
- Filippopoulou, C.; Simos, G.; Chachami, G. The role of sumoylation in the response to hypoxia: An overview. Cells 2020, 9, 2359. [Google Scholar] [CrossRef]
- Lee, Y.-J.; Miyake, S.-I.; Wakita, H.; McMullen, D.C.; Azuma, Y.; Auh, S.; Hallenbeck, J.M. Protein sumoylation is massively increased in hibernation torpor and is critical for the cytoprotection provided by ischemic preconditioning and hypothermia in shsy5y cells. J. Cereb. Blood Flow Metab. 2007, 27, 950–962. [Google Scholar] [CrossRef]
- Lee, Y.J.; Castri, P.; Bembry, J.; Maric, D.; Auh, S.; Hallenbeck, J.M. Sumoylation participates in induction of ischemic tolerance. J. Neurochem. 2009, 109, 257–267. [Google Scholar] [CrossRef]
- Oliveira, F.R.M.B.; Soares, E.S.; Harms, C.; Cimarosti, H.I.; Sordi, R. Sumoylation in peripheral tissues under low perfusion-related pathological states. J. Cell. Biochem. 2022, 123, 1133–1147. [Google Scholar] [CrossRef]
- Bernstock, J.D.; Ye, D.G.; Griffin, A.; Lee, Y.-J.; Lynch, J.; Latour, L.L.; Friedman, G.K.; Marić, D.; Hallenbeck, J.M. Cerebral ischemia increases small ubiquitin-like modifier conjugation within human penumbral tissue: Radiological-pathological correlation. Front. Neurol. 2018, 8, 738. [Google Scholar] [CrossRef]
- Hendriks, I.A.; Lyon, D.; Su, D.; Skotte, N.H.; Daniel, J.A.; Jensen, L.J.; Nielsen, M.L. Site-specific characterization of endogenous sumoylation across species and organs. Nat. Commun. 2018, 9, 2456. [Google Scholar] [CrossRef]
- Sahin, U.; de Thé, H.; Lallemand-Breitenbach, V. Sumoylation in physiology, pathology and therapy. Cells 2022, 11, 814. [Google Scholar] [CrossRef]
- Flotho, A.; Melchior, F. Sumoylation: A regulatory protein modification in health and disease. Annu. Rev. Biochem. 2013, 82, 357–385. [Google Scholar] [CrossRef]
- Yang, W.; Sheng, H.; Wang, H. Targeting the sumo pathway for neuroprotection in brain ischaemia. Stroke Vasc. Neurol. 2016, 1, 101–107. [Google Scholar] [CrossRef]
- Droescher, M.; Chaugule, V.K.; Pichler, A. Sumo rules: Regulatory concepts and their implication in neurologic functions. Neuromol. Med. 2013, 15, 639–660. [Google Scholar] [CrossRef]
- Zhang, L.; Liu, X.; Sheng, H.; Liu, S.; Li, Y.; Zhao, J.Q.; Warner, D.S.; Paschen, W.; Yang, W. Neuron-specific sumo knockdown suppresses global gene expression response and worsens functional outcome after transient forebrain ischemia in mice. Neuroscience 2017, 343, 190–212. [Google Scholar] [CrossRef]
- Bernstock, J.D.; Ye, D.; Gessler, F.A.; Lee, Y.J.; Peruzzotti-Jametti, L.; Baumgarten, P.; Johnson, K.R.; Maric, D.; Yang, W.; Kögel, D.; et al. Topotecan is a potent inhibitor of sumoylation in glioblastoma multiforme and alters both cellular replication and metabolic programming. Sci. Rep. 2017, 7, 7425. [Google Scholar] [CrossRef]
- Yang, W.; Ma, Q.; Mackensen, G.B.; Paschen, W. Deep hypothermia markedly activates the small ubiquitin-like modifier conjugation pathway; implications for the fate of cells exposed to transient deep hypothermic cardiopulmonary bypass. J. Cereb. Blood Flow Metab. 2009, 29, 886–890. [Google Scholar] [CrossRef]
- Yang, W.; Sheng, H.; Thompson, J.W.; Zhao, S.; Wang, L.; Miao, P.; Liu, X.; Moseley, M.A.; Paschen, W. Small ubiquitin-like modifier 3-modified proteome regulated by brain ischemia in novel small ubiquitin-like modifier transgenic mice: Putative protective proteins/pathways. Stroke 2014, 45, 1115–1122. [Google Scholar] [CrossRef]
- Yang, W.; Sheng, H.; Warner, D.S.; Paschen, W. Transient global cerebral ischemia induces a massive increase in protein sumoylation. J. Cereb. Blood Flow Metab. 2008, 28, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Sheng, H.; Warner, D.S.; Paschen, W. Transient focal cerebral ischemia induces a dramatic activation of small ubiquitin-like modifier conjugation. J. Cereb. Blood Flow Metab. 2008, 28, 892–896. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Ashikaga, E.; Rubin, P.P.; Heimann, M.J.; Hildick, K.L.; Bishop, P.; Girach, F.; Josa-Prado, F.; Tang, L.T.H.; Carmichael, R.E.; et al. Receptor trafficking and the regulation of synaptic plasticity by sumo. Neuromol. Med. 2013, 15, 692–706. [Google Scholar] [CrossRef] [PubMed]
- Feligioni, M.; Mattson, M.P.; Nisticò, R. Sumoylation in neuroplasticity and neurological disorders. Neuromol. Med. 2013, 15, 637–638. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhang, Y.; Wang, Q.; Qin, Y.; Yang, X.; Xing, Z.; Shen, Y.; Wu, H.; Qi, Y. The function of sumoylation and its crucial roles in the development of neurological diseases. FASEB J. 2021, 35, e21510. [Google Scholar] [CrossRef]
- Mendler, L.; Braun, T.; Müller, S. The ubiquitin-like sumo system and heart function: From development to disease. Circ. Res. 2016, 118, 132–144. [Google Scholar] [CrossRef]
- Kho, C.; Lee, A.; Jeong, D.; Oh, J.G.; Chaanine, A.H.; Kizana, E.; Park, W.J.; Hajjar, R.J. Sumo1-dependent modulation of serca2a in heart failure. Nature 2011, 477, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Wei, Q.; Su, Y.; Dong, Z. Sumoylation occurs in acute kidney injury and plays a cytoprotective role. Biochim. Biophys. Acta 2015, 1852, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zhang, X.; Rong, J. Sumoylation as a therapeutic target for myocardial infarction. Front. Cardiovasc. Med. 2021, 8, 701583. [Google Scholar] [CrossRef] [PubMed]
- Datwyler, A.L.; Lättig-Tünnemann, G.; Yang, W.; Paschen, W.; Lee, S.L.L.; Dirnagl, U.; Endres, M.; Harms, C. Sumo2/3 conjugation is an endogenous neuroprotective mechanism. J. Cereb. Blood Flow Metab. 2011, 31, 2152–2159. [Google Scholar] [CrossRef]
- Bernstock, J.D.; Ye, D.G.; Lee, Y.-J.; Gessler, F.; Friedman, G.K.; Zheng, W.; Hallenbeck, J.M. Drugging sumoylation for neuroprotection and oncotherapy. Neural Regen. Res. 2018, 13, 415–416. [Google Scholar] [CrossRef]
- Cuomo, O.; Pignataro, G.; Sirabella, R.; Molinaro, P.; Anzilotti, S.; Scorziello, A.; Sisalli, M.J.; Di Renzo, G.; Annunziato, L. Sumoylation of lys590 of ncx3 f-loop by sumo1 participates in brain neuroprotection induced by ischemic preconditioning. Stroke 2016, 47, 1085–1093. [Google Scholar] [CrossRef]
- Kunz, K.; Wagner, K.; Mendler, L.; Hölper, S.; Dehne, N.; Müller, S. Sumo signaling by hypoxic inactivation of sumo-specific isopeptidases. Cell Rep. 2016, 16, 3075–3086. [Google Scholar] [CrossRef]
- Bernstock, J.D.; Ye, D.G.; Estevez, D.; Chagoya, G.; Wang, Y.-C.; Gessler, F.; Hallenbeck, J.M.; Yang, W. The role of sumoylation and ubiquitination in brain ischaemia: Critical concepts and clinical implications. Curr. Issues Mol. Biol. 2020, 35, 127–144. [Google Scholar] [CrossRef]
- Dong, P.; Li, Q.; Han, H. Hif-1α in cerebral ischemia (review). Mol. Med. Rep. 2022, 25, 41. [Google Scholar] [CrossRef]
- Mabb, A.M.; Miyamoto, S. SUMO and NF-κB ties. Cell. Mol. Life Sci. 2007, 64, 1979–1996. [Google Scholar] [CrossRef]
- Li, J.; Xu, Y.; Long, X.-D.; Wang, W.; Jiao, H.-K.; Mei, Z.; Yin, Q.-Q.; Ma, L.-N.; Zhou, A.-W.; Wang, L.-S.; et al. Cbx4 governs hif-1α to potentiate angiogenesis of hepatocellular carcinoma by its sumo e3 ligase activity. Cancer Cell 2014, 25, 118–131. [Google Scholar] [CrossRef]
- Pan, Y.; Li, Q.; Cao, Z.; Zhao, S. The sumo e3 ligase cbx4 is identified as a poor prognostic marker of gastric cancer through multipronged omic analyses. Genes Dis. 2021, 8, 827–837. [Google Scholar] [CrossRef]
- Nakagawa, K.; Kohara, T.; Uehata, Y.; Miyakawa, Y.; Sato-Ueshima, M.; Okubo, N.; Asaka, M.; Takeda, H.; Kobayashi, M. Pias3 enhances the transcriptional activity of hif-1α by increasing its protein stability. Biochem. Biophys. Res. Commun. 2016, 469, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Tojo, M.; Matsuzaki, K.; Minami, T.; Honda, Y.; Yasuda, H.; Chiba, T.; Saya, H.; Fujii-Kuriyama, Y.; Nakao, M. The aryl hydrocarbon receptor nuclear transporter is modulated by the sumo-1 conjugation system. J. Biol. Chem. 2002, 277, 46576–46585. [Google Scholar] [CrossRef] [PubMed]
- Cai, Q.; Verma, S.C.; Kumar, P.; Ma, M.; Robertson, E.S. Hypoxia inactivates the vhl tumor suppressor through piasy-mediated sumo modification. PLoS ONE 2010, 5, e9720. [Google Scholar] [CrossRef] [PubMed]
- Kang, X.; Li, J.; Zou, Y.; Yi, J.; Zhang, H.; Cao, M.; Yeh, E.T.H.; Cheng, J. Piasy stimulates hif1α sumoylation and negatively regulates hif1α activity in response to hypoxia. Oncogene 2010, 29, 5568–5578. [Google Scholar] [CrossRef]
- Núñez-O’Mara, A.; Gerpe-Pita, A.; Pozo, S.; Carlevaris, O.; Urzelai, B.; Lopitz-Otsoa, F.; Rodríguez, M.S.; Berra, E. PHD3-SUMO conjugation represses HIF1 transcriptional activity independently of PHD3 catalytic activity. J. Cell Sci. 2015, 128, 40–49. [Google Scholar] [CrossRef]
- Sallais, J.; Alahari, S.; Tagliaferro, A.; Bhattacharjee, J.; Post, M.; Caniggia, I. Factor inhibiting hif1-a novel target of sumoylation in the human placenta. Oncotarget 2017, 8, 114002–114018. [Google Scholar] [CrossRef]
- Chachami, G.; Stankovic-Valentin, N.; Karagiota, A.; Basagianni, A.; Plessmann, U.; Urlaub, H.; Melchior, F.; Simos, G. Hypoxia-induced changes in sumo conjugation affect transcriptional regulation under low oxygen. Mol. Cell. Proteom. 2019, 18, 1197–1209. [Google Scholar] [CrossRef]
- Zhang, W.; Potrovita, I.; Tarabin, V.; Herrmann, O.; Beer, V.; Weih, F.; Schneider, A.; Schwaninger, M. Neuronal activation of NF-κB contributes to cell death in cerebral ischemia. J. Cereb. Blood Flow Metab. 2005, 25, 30–40. [Google Scholar] [CrossRef]
- Tashiro, K.; Pando, M.P.; Kanegae, Y.; Wamsley, P.M.; Inoue, S.; Verma, I.M. Direct involvement of the ubiquitin-conjugating enzyme ubc9/hus5 in the degradation of IκBα. Proc. Natl. Acad. Sci. USA 1997, 94, 7862–7867. [Google Scholar] [CrossRef] [PubMed]
- Desterro, J.M.; Rodriguez, M.S.; Hay, R.T. Sumo-1 modification of IκBα inhibits NF-κB activation. Mol. Cell 1998, 2, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xia, Q.; Mao, M.; Zhou, H.; Zheng, L.; Wang, Y.; Zeng, Z.; Yan, L.; Zhao, Y.; Shi, J. Annexin-a1 sumoylation regulates microglial polarization after cerebral ischemia by modulating IKκ stability via selective autophagy. Sci. Adv. 2021, 7, eabc5539. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.T.; Wuerzberger-Davis, S.M.; Wu, Z.-H.; Miyamoto, S. Sequential modification of NEMO/IKKγ by sumo-1 and ubiquitin mediates NF-κB activation by genotoxic stress. Cell 2003, 115, 565–576. [Google Scholar] [CrossRef]
- Yang, T.; Sun, J.; Wei, B.; Liu, S. Senp1-mediated nemo de-sumoylation inhibits intermittent hypoxia induced inflammatory response of microglia in vitro. J. Cell. Physiol. 2020, 235, 3529–3538. [Google Scholar] [CrossRef]
- Lee, J.H.; Park, S.M.; Kim, O.S.; Lee, C.S.; Woo, J.H.; Park, S.J.; Joe, E.H.; Jou, I. Differential sumoylation of LXRα and LXRβ mediates transrepression of stat1 inflammatory signaling in IFN-γ-stimulated brain astrocytes. Mol. Cell 2009, 35, 806–817. [Google Scholar] [CrossRef]
- Cimarosti, H.; Lindberg, C.; Bomholt, S.F.; Rønn, L.C.; Henley, J.M. Increased protein sumoylation following focal cerebral ischemia. Neuropharmacology 2008, 54, 280–289. [Google Scholar] [CrossRef]
- Guo, C.; Henley, J.M. Wrestling with stress: Roles of protein sumoylation and desumoylation in cell stress response. IUBMB Life 2014, 66, 71–77. [Google Scholar] [CrossRef]
- Henley, J.M.; Craig, T.J.; Wilkinson, K.A. Neuronal sumoylation: Mechanisms, physiology, and roles in neuronal dysfunction. Physiol. Rev. 2014, 94, 1249–1285. [Google Scholar] [CrossRef]
- Guo, C.; Hildick, K.L.; Luo, J.; Dearden, L.; Wilkinson, K.A.; Henley, J.M. Senp3-mediated desumoylation of dynamin-related protein 1 promotes cell death following ischaemia. EMBO J. 2013, 32, 1514–1528. [Google Scholar] [CrossRef]
- Neumar, R.W. Molecular mechanisms of ischemic neuronal injury. Ann. Emerg. Med. 2000, 36, 483–506. [Google Scholar] [CrossRef] [PubMed]
- Feligioni, M.; Nishimune, A.; Henley, J.M. Protein sumoylation modulates calcium influx and glutamate release from presynaptic terminals. Eur. J. Neurosci. 2009, 29, 1348–1356. [Google Scholar] [CrossRef] [PubMed]
- Dustrude, E.T.; Wilson, S.M.; Ju, W.; Xiao, Y.; Khanna, R. Crmp2 protein sumoylation modulates nav1.7 channel trafficking. J. Biol. Chem. 2013, 288, 24316–24331. [Google Scholar] [CrossRef]
- Martin, S.; Nishimune, A.; Mellor, J.R.; Henley, J.M. Sumoylation regulates kainate-receptor-mediated synaptic transmission. Nature 2007, 447, 321–325. [Google Scholar] [CrossRef]
- Coelho-Silva, L.; Stephens, G.J.; Cimarosti, H. Sumoylation and calcium signalling: Potential roles in the brain and beyond. Neuronal Signal. 2017, 1, NS20160010. [Google Scholar] [CrossRef] [PubMed]
- Bernstock, J.D.; Peruzzotti-Jametti, L.; Ye, D.; Gessler, F.A.; Maric, D.; Vicario, N.; Lee, Y.-J.; Pluchino, S.; Hallenbeck, J.M. Neural stem cell transplantation in ischemic stroke: A role for preconditioning and cellular engineering. J. Cereb. Blood Flow Metab. 2017, 37, 2314–2319. [Google Scholar] [CrossRef]
- Ding, D.-C.; Lin, C.-H.; Shyu, W.-C.; Lin, S.-Z. Neural stem cells and stroke. Cell Transplant. 2013, 22, 619–630. [Google Scholar] [CrossRef]
- Baker, E.W.; Kinder, H.A.; West, F.D. Neural stem cell therapy for stroke: A multimechanistic approach to restoring neurological function. Brain Behav. 2019, 9, e01214. [Google Scholar] [CrossRef]
- Tahmasebi, S.; Ghorbani, M.; Savage, P.; Gocevski, G.; Yang, X.-J. The sumo conjugating enzyme ubc9 is required for inducing and maintaining stem cell pluripotency. Stem Cells 2014, 32, 1012–1020. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Sharma, P.; Athanasiou, M.; Kumar, A.; Yamada, S.; Kuehn, M.R. Mutation of senp1/supr-2 reveals an essential role for desumoylation in mouse development. Mol. Cell. Biol. 2005, 25, 5171–5182. [Google Scholar] [CrossRef]
- Bernstock, J.D.; Peruzzotti-Jametti, L.; Leonardi, T.; Vicario, N.; Ye, D.; Lee, Y.-J.; Maric, D.; Johnson, K.R.; Mou, Y.; Van Den Bosch, A.; et al. Sumoylation promotes survival and integration of neural stem cell grafts in ischemic stroke. EBioMedicine 2019, 42, 214–224. [Google Scholar] [CrossRef]
- Lee, Y.-J.; Johnson, K.R.; Hallenbeck, J.M. Global protein conjugation by ubiquitin-like-modifiers during ischemic stress is regulated by micrornas and confers robust tolerance to ischemia. PLoS ONE 2012, 7, e47787. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-J.; Hallenbeck, J.M. Sumo and ischemic tolerance. Neuromol. Med. 2013, 15, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Tokarz, P.; Woźniak, K. Senp proteases as potential targets for cancer therapy. Cancers 2021, 13, 2059. [Google Scholar] [CrossRef]
- Bernstock, J.D.; Lee, Y.-J.; Peruzzotti-Jametti, L.; Southall, N.; Johnson, K.R.; Maric, D.; Volpe, G.; Kouznetsova, J.; Zheng, W.; Pluchino, S.; et al. A novel quantitative high-throughput screen identifies drugs that both activate sumo conjugation via the inhibition of micrornas 182 and 183 and facilitate neuroprotection in a model of oxygen and glucose deprivation. J. Cereb. Blood Flow Metab. 2016, 36, 426–441. [Google Scholar] [CrossRef]
- Nadareishvili, Z.; Kelley, D.; Luby, M.; Simpkins, A.N.; Leigh, R.; Lynch, J.K.; Hsia, A.W.; Benson, R.T.; Johnson, K.R.; Hallenbeck, J.M.; et al. Molecular signature of penumbra in acute ischemic stroke: A pilot transcriptomics study. Ann. Clin. Transl. Neurol. 2019, 6, 817–820. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Rowe, M.; Ren, M.; Hong, J.-S.; Chen, P.-S.; Chuang, D.-M. Histone deacetylase inhibitors exhibit anti-inflammatory and neuroprotective effects in a rat permanent ischemic model of stroke: Multiple mechanisms of action. J. Pharmacol. Exp. Ther. 2007, 321, 892–901. [Google Scholar] [CrossRef]
- Brookes, R.L.; Crichton, S.; Wolfe, C.D.A.; Yi, Q.; Li, L.; Hankey, G.J.; Rothwell, P.M.; Markus, H.S. Sodium valproate, a histone deacetylase inhibitor, is associated with reduced stroke risk after previous ischemic stroke or transient ischemic attack. Stroke 2018, 49, 54–61. [Google Scholar] [CrossRef]
- Park, M.J.; Sohrabji, F. The histone deacetylase inhibitor, sodium butyrate, exhibits neuroprotective effects for ischemic stroke in middle-aged female rats. J. Neuroinflamm. 2016, 13, 300. [Google Scholar] [CrossRef]
- Al Shoyaib, A.; Alamri, F.F.; Syeara, N.; Jayaraman, S.; Karamyan, S.T.; Arumugam, T.V.; Karamyan, V.T. The effect of histone deacetylase inhibitors panobinostat or entinostat on motor recovery in mice after ischemic stroke. Neuromol. Med. 2021, 23, 471–484. [Google Scholar] [CrossRef]
- Bonsack, F.; Sukumari-Ramesh, S. Entinostat improves acute neurological outcomes and attenuates hematoma volume after intracerebral hemorrhage. Brain Res. 2021, 1752, 147222. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, K.; Lacza, Z.; Rajapakse, N.; Horiguchi, T.; Snipes, J.; Busija, D.W. Mitok(atp) opener, diazoxide, reduces neuronal damage after middle cerebral artery occlusion in the rat. Am. J. Physiol. Heart Circ. Physiol. 2002, 283, H1005–H1011. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, J.C.; Yao, X.-L.; Alam, H.; McCabe, J.T. Diazoxide, as a postconditioning and delayed preconditioning trigger, increases hsp25 and hsp70 in the central nervous system following combined cerebral stroke and hemorrhagic shock. J. Neurotrauma 2007, 24, 532–546. [Google Scholar] [CrossRef]
- Bernstock, J.D.; Ye, D.; Smith, J.A.; Lee, Y.-J.; Gessler, F.A.; Yasgar, A.; Kouznetsova, J.; Jadhav, A.; Wang, Z.; Pluchino, S.; et al. Quantitative high-throughput screening identifies cytoprotective molecules that enhance sumo conjugation via the inhibition of sumo-specific protease (senp)2. FASEB J. 2018, 32, 1677–1691. [Google Scholar] [CrossRef]
- Chojnowski, K.; Opielka, M.; Nazar, W.; Kowianski, P.; Smolenski, R.T. Neuroprotective effects of guanosine in ischemic stroke—Small steps towards effective therapy. Int. J. Mol. Sci. 2021, 22, 6898. [Google Scholar] [CrossRef]
- Lee, Y.-J.; Bernstock, J.D.; Nagaraja, N.; Ko, B.; Hallenbeck, J.M. Global sumoylation facilitates the multimodal neuroprotection afforded by quercetin against the deleterious effects of oxygen/glucose deprivation and the restoration of oxygen/glucose. J. Neurochem. 2016, 138, 101–116. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Ma, J.; Yang, F.; Li, S.; Ma, W.; Chang, X.; Yang, L. Neuroprotective effects of quercetin on ischemic stroke: A literature review. Front. Pharmacol. 2022, 13, 854249. [Google Scholar] [CrossRef]
- Guo, C.; Wang, W.-J.; Liao, Y.-C.; Zhao, C.; Yin, Y.; Yao, M.-N.; Ding, Y.; Wang, J.-W. Effect and mechanisms of quercetin for experimental focal cerebral ischemia: A systematic review and meta-analysis. Oxidative Med. Cell. Longev. 2022, 2022, 9749461. [Google Scholar] [CrossRef]
- Koizumi, H.; Fujisawa, H.; Suehiro, E.; Shirao, S.; Suzuki, M. Neuroprotective effects of ebselen following forebrain ischemia: Involvement of glutamate and nitric oxide. Neurol. Med. Chir. 2011, 51, 337–343. [Google Scholar] [CrossRef]
- Park, S.; Kang, S.; Kim, D.S.; Shin, B.K.; Moon, N.R.; Daily, J.W., 3rd. Ebselen pretreatment attenuates ischemia/reperfusion injury and prevents hyperglycemia by improving hepatic insulin signaling and β-cell survival in gerbils. Free Radic. Res. 2014, 48, 864–874. [Google Scholar] [CrossRef]
- Ogawa, A.; Yoshimoto, T.; Kikuchi, H.; Sano, K.; Saito, I.; Yamaguchi, T.; Yasuhara, H. Ebselen in acute middle cerebral artery occlusion: A placebo-controlled, double-blind clinical trial. Cerebrovasc. Dis. 1999, 9, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, T.; Sano, K.; Takakura, K.; Saito, I.; Shinohara, Y.; Asano, T.; Yasuhara, H. Ebselen in acute ischemic stroke: A placebo-controlled, double-blind clinical trial. Ebselen study group. Stroke 1998, 29, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Mulder, I.A.; van Bavel, E.T.; de Vries, H.E.; Coutinho, J.M. Adjunctive cytoprotective therapies in acute ischemic stroke: A systematic review. Fluids Barriers CNS 2021, 18, 46. [Google Scholar] [CrossRef]
- Parnham, M.J.; Sies, H. The early research and development of ebselen. Biochem. Pharmacol. 2013, 86, 1248–1253. [Google Scholar] [CrossRef]
- Porciúncula, L.O.; Rocha, J.B.; Boeck, C.R.; Vendite, D.; Souza, D.O. Ebselen prevents excitotoxicity provoked by glutamate in rat cerebellar granule neurons. Neurosci. Lett. 2001, 299, 217–220. [Google Scholar] [CrossRef]
- Porciúncula, L.O.; Rocha, J.B.T.; Cimarosti, H.; Vinade, L.; Ghisleni, G.; Salbego, C.G.; Souza, D.O. Neuroprotective effect of ebselen on rat hippocampal slices submitted to oxygen-glucose deprivation: Correlation with immunocontent of inducible nitric oxide synthase. Neurosci. Lett. 2003, 346, 101–104. [Google Scholar] [CrossRef]
- Chen, S.; Dong, D.; Xin, W.; Zhou, H. Progress in the discovery of small molecule modulators of desumoylation. Curr. Issues Mol. Biol. 2020, 35, 17–34. [Google Scholar] [CrossRef] [PubMed]
- Yamagata, K.; Ichinose, S.; Miyashita, A.; Tagami, M. Protective effects of ebselen, a seleno-organic antioxidant on neurodegeneration induced by hypoxia and reperfusion in stroke-prone spontaneously hypertensive rat. Neuroscience 2008, 153, 428–435. [Google Scholar] [CrossRef]
- Sui, H.; Wang, W.; Wang, P.H.; Liu, L.S. Protective effect of antioxidant ebselen (pz51) on the cerebral cortex of stroke-prone spontaneously hypertensive rats. Hypertens. Res. 2005, 28, 249–254. [Google Scholar] [CrossRef]
- Imai, H.; Graham, D.I.; Masayasu, H.; Macrae, I.M. Antioxidant ebselen reduces oxidative damage in focal cerebral ischemia. Free Radic. Biol. Med. 2003, 34, 56–63. [Google Scholar] [CrossRef]
- Imai, H.; Masayasu, H.; Dewar, D.; Graham, D.I.; Macrae, I.M. Ebselen protects both gray and white matter in a rodent model of focal cerebral ischemia. Stroke 2001, 32, 2149–2154. [Google Scholar] [CrossRef] [PubMed]
- Salom, J.B.; Pérez-Asensio, F.J.; Burguete, M.C.; Marín, N.; Pitarch, C.; Torregrosa, G.; Romero, F.J.; Alborch, E. Single-dose ebselen does not afford sustained neuroprotection to rats subjected to severe focal cerebral ischemia. Eur. J. Pharmacol. 2004, 495, 55–62. [Google Scholar] [CrossRef]
- Krajnak, K.; Dahl, R. Small molecule sumoylation activators are novel neuroprotective agents. Bioorg. Med. Chem. Lett. 2018, 28, 405–409. [Google Scholar] [CrossRef]
- Chang, H.M.; Yeh, E.T.H. Sumo: From bench to bedside. Physiol. Rev. 2020, 100, 1599–1619. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, O.; Vicogne, J. Total chemical synthesis of sumo proteins. Tetrahedron Lett. 2016, 57, 4319–4324. [Google Scholar] [CrossRef]
- Langston, S.P.; Grossman, S.; England, D.; Afroze, R.; Bence, N.; Bowman, D.; Bump, N.; Chau, R.; Chuang, B.-C.; Claiborne, C.; et al. Discovery of tak-981, a first-in-class inhibitor of sumo-activating enzyme for the treatment of cancer. J. Med. Chem. 2021, 64, 2501–2520. [Google Scholar] [CrossRef]
- Tymianski, M. Combining neuroprotection with endovascular treatment of acute stroke: Is there hope? Stroke 2017, 48, 1700–1705. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karandikar, P.; Gerstl, J.V.E.; Kappel, A.D.; Won, S.-Y.; Dubinski, D.; Garcia-Segura, M.E.; Gessler, F.A.; See, A.P.; Peruzzotti-Jametti, L.; Bernstock, J.D. SUMOtherapeutics for Ischemic Stroke. Pharmaceuticals 2023, 16, 673. https://doi.org/10.3390/ph16050673
Karandikar P, Gerstl JVE, Kappel AD, Won S-Y, Dubinski D, Garcia-Segura ME, Gessler FA, See AP, Peruzzotti-Jametti L, Bernstock JD. SUMOtherapeutics for Ischemic Stroke. Pharmaceuticals. 2023; 16(5):673. https://doi.org/10.3390/ph16050673
Chicago/Turabian StyleKarandikar, Paramesh, Jakob V. E. Gerstl, Ari D. Kappel, Sae-Yeon Won, Daniel Dubinski, Monica Emili Garcia-Segura, Florian A. Gessler, Alfred Pokmeng See, Luca Peruzzotti-Jametti, and Joshua D. Bernstock. 2023. "SUMOtherapeutics for Ischemic Stroke" Pharmaceuticals 16, no. 5: 673. https://doi.org/10.3390/ph16050673
APA StyleKarandikar, P., Gerstl, J. V. E., Kappel, A. D., Won, S.-Y., Dubinski, D., Garcia-Segura, M. E., Gessler, F. A., See, A. P., Peruzzotti-Jametti, L., & Bernstock, J. D. (2023). SUMOtherapeutics for Ischemic Stroke. Pharmaceuticals, 16(5), 673. https://doi.org/10.3390/ph16050673







