Polytherapy and Multimorbidity Pattern of Users of Anti-VEGF Drugs and Dexamethasone for the Treatment of Age-Related Macular Degeneration and other Vascular Retinopathies in Clinical Practice
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Setting
4.3. Data Sources
- ▪
- Inhabitant Registry (IR) with demographic information (birthyear, gender, citizenship), start and end dates of presence in the region;
- ▪
- Hospital discharge records (HOSP): each hospital admission is described with dates of admission and discharge, and one main and five secondary diagnoses and 6 procedures coded using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD9CM);
- ▪
- Outpatient care records (OUTPAT): it is a list of outpatient activities dispensed by the healthcare system free of charge or upon co-payment, among which specialist encounters (with no diagnostic code), laboratory or instrumental or bio-imaging diagnostic tests (without results) and procedures in outpatient setting are recorded with a specific Italian coding system; the facility where the activity takes place is recorded as well;
- ▪
- Prescribed drugs intended for outpatient use. Prescription records include information on the dispensed drugs (e.g., active principle, ATC code) as well as the date of dispensation. Drugs are registered in two databases: one collects dispensing from hospital pharmacies (DDRUG), the other dispensing from community pharmacies (DRUGS);
- ▪
- Disease-specific exemptions from co-payment to health care coding using ICD9CM (EXE).
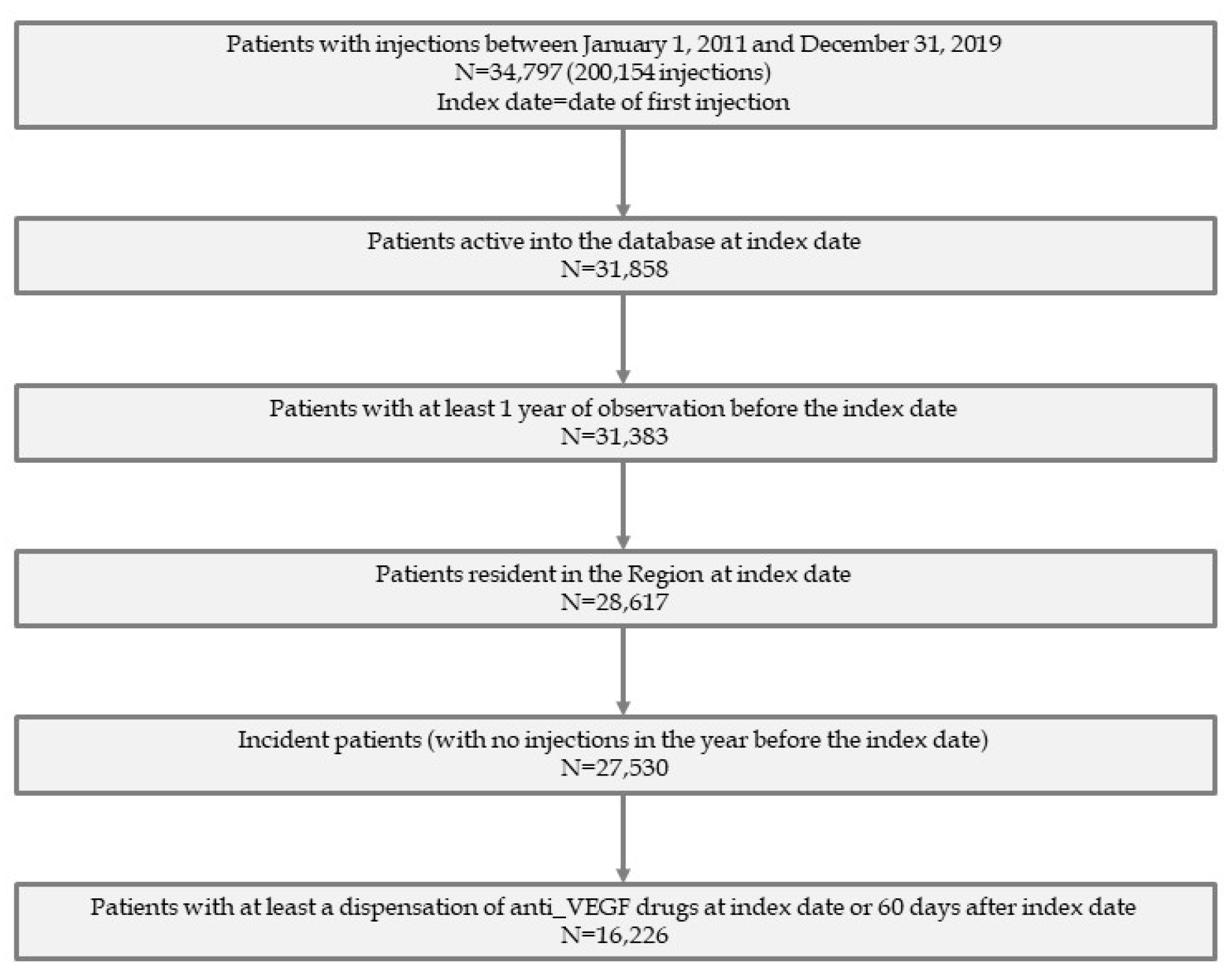
4.4. Study Population
4.5. Follow-Up
4.6. Cohort of Residents
4.7. Study Variables
4.8. Other Variables
4.9. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Resnikoff, S.; Pascolini, D.; Etya’Ale, D.; Kocur, I.; Pararajasegaram, R.; Pokharel, G.P.; Mariotti, S.P. Global data on visual impairment in the year 2002. Bull. World Health Organ. 2004, 82, 844–851. [Google Scholar]
- Frank, R.N. Diabetic Retinopathy. N. Engl. J. Med. 2004, 350, 48–58. [Google Scholar] [CrossRef]
- Campochiaro, P.A.; Heier, J.S.; Feiner, L.; Gray, S.; Saroj, N.; Rundle, A.C.; Murahashi, W.Y.; Rubio, R.G. Ranibizumab for Macular Edema following Branch Retinal Vein Occlusion: Six-Month Primary End Point Results of a Phase III Study. Ophthalmology 2010, 117, 1102–1112. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.; McIntosh, R.L.; Cheung, N.; Lim, L.; Wang, J.J.; Mitchell, P.; Kowalski, J.W.; Nguyen, H.; Wong, T.Y. The Prevalence of Retinal Vein Occlusion: Pooled Data from Population Studies from the United States, Europe, Asia, and Australia. Ophthalmology 2010, 117, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Servillo, A.; Zucchiatti, I.; Sacconi, R.; Parravano, M.; Querques, L.; La Rubia, P.; Prascina, F.; Bandello, F.; Querques, G. The state-of-the-art pharmacotherapeutic management of neovascular age-related macular degeneration. Expert Opin. Pharmacother. 2022, 24, 197–206. [Google Scholar] [CrossRef]
- Leal, J.R.; Laupland, K.B. Validity of ascertainment of co-morbid illness using administrative databases: A systematic review. Clin. Microbiol. Infect. 2010, 16, 715–721. [Google Scholar] [CrossRef] [PubMed]
- Ferner, R.E.; Aronson, J.K. Communicating information about drug safety. Br. Med. J. 2006, 333, 143–145. [Google Scholar] [CrossRef]
- Veehof, L.J.G.; Stewart, R.E.; Haaijer-Ruskamp, F.M.; Meyboom-de Jong, B. The development of polypharmacy. A longitudinal study. Fam. Pract. 2000, 17, 261–267. [Google Scholar] [CrossRef]
- Zheng, D.D.; Christ, S.L.; Lam, B.L.; Feaster, D.J.; McCollister, K.; Lee, D.J. Patterns of Chronic Conditions and Their Association With Visual Impairment and Health Care Use. JAMA Ophthalmol. 2020, 138, 387. [Google Scholar] [CrossRef]
- Boehmer, K.R.; Abu Dabrh, A.M.; Gionfriddo, M.R.; Erwin, P.; Montori, V.M. Does the chronic care model meet the emerging needs of people living with multimorbidity? A systematic review and thematic synthesis. PLoS ONE 2018, 13, e0190852. [Google Scholar] [CrossRef]
- Scondotto, G.; Sultana, J.; Ientile, V.; Ingrasciotta, Y.; Fontana, A.; Copetti, M.; Mirabelli, E.; Trombetta, C.J.; Rapisarda, C.; Reibaldi, M.; et al. How Have Intravitreal Anti-VEGF and Dexamethasone Implant Been Used in Italy? A Multiregional, Population-Based Study in the Years 2010–2016. BioMed Res. Int. 2020, 2020, 7582763 . [Google Scholar] [CrossRef]
- Virgili, G.; Tosi, G.M.; Figus, M.; Rizzo, S.; Murro, V.; Mucciolo, D.P.; Roberto, G.; Gini, R. Use of anti-vascular endothelial growth factor drugs for eye disease in Tuscany: Development and test of indicators of treatment intensity. Eur. J. Ophthalmol. 2019, 30, 1440–1447. [Google Scholar] [CrossRef]
- Velilla, S.; Garcia-Medina, J.J.; García-Layana, A.; Dolz-Marco, R.; Pons-Vázquez, S.; Pinazo-Duran, M.D.; Gómez-Ulla, F.; Arevalo, J.F.; Díaz-Llopis, M.; Gallego-Pinazo, R. Smoking and Age-Related Macular Degeneration: Review and Update. J. Ophthalmol. 2013, 2013, 895147 . [Google Scholar] [CrossRef]
- Adams, M.K.M.; Chong, E.W.; Williamson, E.; Aung, K.Z.; Makeyeva, G.A.; Giles, G.; English, D.; Hopper, J.; Guymer, R.; Baird, P.; et al. 20/20—Alcohol and Age-related Macular Degeneration: The Melbourne Collaborative Cohort Study. Am. J. Epidemiol. 2012, 176, 289–298. [Google Scholar] [CrossRef]
- Choi, D.; Choi, S.; Park, S.M. Effect of smoking cessation on the risk of dementia: A longitudinal study. Ann. Clin. Transl. Neurol. 2018, 5, 1192–1199. [Google Scholar] [CrossRef]
- Ngandu, T.; Lehtisalo, J.; Solomon, A.; Levälahti, E.; Ahtiluoto, S.; Antikainen, R.; Bäckman, L.; Hänninen, T.; Jula, A.; Laatikainen, T.; et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 2015, 385, 2255–2263. [Google Scholar] [CrossRef]
- Bettiol, S.S.; Rose, T.C.; Hughes, C.J.; Smith, L.A. Alcohol Consumption and Parkinson’s Disease Risk: A Review of Recent Findings. J. Park. Dis. 2015, 5, 425–442. [Google Scholar] [CrossRef]
- Carrière, I.; Delcourt, C.; Daien, V.; Pérès, K.; Féart, C.; Berr, C.; Ancelin, M.L.; Ritchie, K. A prospective study of the bi-directional association between vision loss and depression in the elderly. J. Affect. Disord. 2013, 151, 164–170. [Google Scholar] [CrossRef]
- Talks, S.J.; Stratton, I.; Peto, T.; Lotery, A.; Chakravarthy, U.; Eleftheriadis, H.; Izadi, S.; Dhingra, N.; Scanlon, P.; Talks, J.; et al. Aflibercept in clinical practice; visual acuity, injection numbers and adherence to treatment, for diabetic macular oedema in 21 UK hospitals over 3 years. Eye 2021, 36, 72–77. [Google Scholar] [CrossRef]
- Mehta, H.; Kim, L.N.; Mathis, T.; Zalmay, P.; Ghanchi, F.; Amoaku, W.M.; Kodjikian, L. Trends in Real-World Neovascular AMD Treatment Outcomes in the UK. Clin. Ophthalmol. 2020, 14, 3331–3342. [Google Scholar] [CrossRef]
- Ehlken, C.; Ziemssen, F.; Eter, N.; Lanzl, I.; Kaymak, H.; Lommatzsch, A.; Schuster, A.K. Systematic review: Non-adherence and non-persistence in intravitreal treatment. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 2077–2090. [Google Scholar] [CrossRef]

| Overall | Aflibercept | Bevacizumab | Dexamethasone | Ranibizumab | Pegaptanib | |
|---|---|---|---|---|---|---|
| TOTAL, N (%) | 16,226 | 4230 (26.1) | 593 (3.6) | 2500 (15.4) | 8731 (53.8) | 172 (1.1) |
| Gender | ||||||
| Female, N (%) | 8605 (53.0) | 2327 (55.0) | 311 (52.4) | 1116 (44.6) | 4766 (54.6) | 85 (49.4) |
| Age | ||||||
| mean (SD), years | 72.8 (11.5) | 74.5 (10.8) | 72.6 (12.0) | 69.7 (11.6) | 72.9 (11.7) | 74.6 (10.1) |
| groups, N (%) | ||||||
| <55 | 1310 (8.1) | 257 (6.0%) | 54 (9.1) | 267 (10.7) | 724 (8.3) | 8 (4.7) |
| 55-<65 | 2194 (13.5) | 459 (10.9) | 74 (12.5) | 476 (19.0) | 1170 (13.4) | 15 (8.7) |
| 65-<75 | 4844 (29.9) | 1183 (28.0) | 175 (29.5) | 856 (34.2) | 2565 (29.4) | 65 (37.8) |
| 75-<85 | 5938 (36.6) | 1742 (41.2) | 225 (37.9) | 747 (29.9) | 3166 (36.3) | 58 (33.7) |
| 85+ | 1940 (12.0) | 589 (13.9) | 65 (11.0) | 154 (6.2) | 1106 (12.7) | 26 (15.1) |
| Education | ||||||
| None | 507 (3.1) | 153 (3.6) | 19 (3.2) | 64 (2.6) | 268 (3.1) | 3 (1.7) |
| Middle school | 7782 (48.0) | 1932 (45.7) | 297 (50.1) | 1184 (47.4) | 4284 (49.1) | 85 (49.4) |
| High school | 3420 (21.1) | 937 (22.2) | 118 (19.9) | 580 (23.2) | 1743 (20.0) | 42 (24.4) |
| College | 1080 (6.7) | 332 (7.8) | 27 (4.6) | 154 (6.2) | 561 (6.4) | 6 (3.5) |
| Unknown | 3437 (21.2) | 876 (20.7) | 132 (22.3) | 518 (20.7) | 1875 (21.5) | 36 (20.9) |
| Overall | Aflibercept | Bevacizumab | Dexamethasone | Ranibizumab | Pegaptanib | |
|---|---|---|---|---|---|---|
| TOTAL, N (%) | 16,226 | 4230 (26.1) | 593 (3.6) | 2500 (15.4) | 8731 (53.8) | 172 (1.1) |
| Adherence | ||||||
| Number of injections in the follow-up periods, mean (standard deviation) | ||||||
| First year | 3.7 (2.2) | 4.5 (2.3) | 3.5 (2.2) | 2.0 (1.4) | 3.8 (2.0) | 3.6 (1.7) |
| Second year | 1.3 (2.0) | 1.6 (2.1) | 1.3 (2.1) | 0.9 (1.6) | 1.3 (2.0) | 1.0 (1.6) |
| Third year | 1.0 (1.8) | 1.3 (2.0) | 0.8 (1.6) | 0.6 (1.3) | 1.0 (1.8) | 0.6 (1.3) |
| Number of specialist examinations in the follow-up period, mean (standard deviation) | ||||||
| First year | 8.9 (6.5) | 9.1 (6.3) | 6.5 (4.7) | 6.7 (4.7) | 9.5 (6.9) | 12.7 (8.0) |
| Second year | 3.7 (4.9) | 3.6 (4.7) | 2.7 (3.7) | 3.2 (4.2) | 3.8 (5.3) | 5.3 (6.8) |
| Third year | 2.8 (4.4) | 2.9 (4.4) | 1.8 (2.9) | 2.2 (3.4) | 2.9 (4.6) | 3.4 (4.8) |
| Number of subjects with at least 3 doses in the first 90 days of follow-up | 6569 (40.5) | 2229 (52.7) | 172 (29.0) | 35 (1.4) | 4097 (46.9) | 36 (20.9) |
| Discontinuation, N (%) | ||||||
| At least 60 days without contact in the first year of follow-up and at least 90 days in the second | 10,706 (66.0) | 3219 (76.1) | 349 (58.9) | 1424 (57.0) | 5601 (64.2) | 113 (65.7) |
| At least 90 days without contact in the first year of follow-up and at least 180 days in the second | 8384 (51.7) | 2225 (52.6) | 262 (44.2) | 1393 (55.7) | 4421 (50.6) | 83 (48.3) |
| Overall | Aflibercept | Bevacizumab | Dexamethasone | Ranibizumab | Pegaptanib | |
|---|---|---|---|---|---|---|
| TOTAL, N (%) | 16,226 | 4230 (26.1) | 593 (3.6) | 2500 (15.4) | 8731 (53.8) | 172 (1.1) |
| Charlson Comorbidity Index | ||||||
| Mean (standard deviation) | 0.5 (1.2) | 0.4 (1.1) | 0.4 (1.1) | 0.6 (1.4) | 0.4 (1.2) | 0.4 (1.0) |
| Number of comorbidities (one of those present in Table) | ||||||
| Mean (standard deviation) | 0.9 (1.1) | 0.8 (1.0) | 0.8 (1.0) | 1.0 (1.1) | 0.9 (1.0) | 0.9 (1.1) |
| Median (interquartile range) | 1.0 (0.0–1.0) | 1.0 (0.0–1.0) | 1.0 (0.0–1.0) | 1.0 (0.0–2.0) | 1.0 (0.0–1.0) | 0.0 (0.0–2.0) |
| Group, N (%) | ||||||
| 0 | 7471 (46.0) | 2049 (48.4) | 284 (47.9) | 974 (39.0) | 4076 (46.7) | 88 (51.2) |
| 1–2 | 7468 (46.0) | 1866 (44.1) | 270 (45.5) | 1271 (50.8) | 3992 (45.7) | 69 (40.1) |
| 3–5 | 1253 (7.7) | 307 (7.3) | 39 (6.6) | 249 (10.0) | 643 (7.4) | 15 (8.7) |
| 6+ | 34 (0.2) | 8 (0.2) | - | 6 (0.2) | 20 (0.2) | - |
| Psychiatric or mental health conditions, N (%) | ||||||
| Anxiety | 132 (0.8) | 25(0.6) | 4 (0.7) | 20 (0.8) | 83 (1.0) | - |
| Bipolar disease | 27 (0.2) | 8 (0.2) | 1 (0.2) | 3 (0.1) | 15 (0.2) | - |
| Delirium | 15 (0.1) | 1 (0.0) | - | 4 (0.2) | 10 (0.1) | - |
| Dementia | 28 (0.2) | 7 (0.2) | 1 (0.2) | 6 (0.2) | 13 (0.1) | 1 (0.6) |
| Depression | 46 (0.3) | 7 (0.2) | - | 9 (0.4) | 30 (0.3) | - |
| Non-schizophrenic psychosis | 29 (0.2) | 7 (0.2) | - | 2 (0.1) | 20 (0.2) | - |
| Schizophrenia | 17 (0.1) | 2 (0.0) | - | 3 (0.1) | 12 (0.1) | - |
| Cardio/cerebrovascular diseases, N (%) | ||||||
| Arrhythmia | 251 (1.5) | 81 (1.9) | 2 (0.3) | 44 (1.8) | 123 (1.4) | 1 (0.6) |
| Congestive heart failure | 323 (2.0) | 80 (1.9) | 13 (2.2) | 49 (2.0) | 178 (2.0) | 3 (1.7) |
| Ischemic heart disease | 1166 (7.2) | 302 (7.1) | 29 (4.9) | 204 (8.2) | 608 (7.0) | 23 (13.4) |
| Stroke | 224 (1.4) | 60 (1.4) | 7 (1.2) | 46 (1.8) | 108 (1.2) | 3 (1.7) |
| Hypertension | 4961 (30.6) | 1262 (29.8) | 185 (31.2) | 875 (35.0) | 2583 (29.6) | 56 (32.6) |
| Peripheral arterial disease | 28 (0.2) | 11 (0.3) | - | 7 (0.3) | 10 (0.1) | - |
| Valve disorders | 224 (1.4) | 54 (1.3) | 5 (0.8) | 36 (1.4) | 127 (1.5) | 2 (1.2) |
| Venous thrombosis embolism | 75 (0.5) | 12 (0.3) | 1 (0.2) | 28 (1.1) | 33 (0.4) | 1 (0.6) |
| Other conditions, N (%) | ||||||
| Diabetes | 5561 (34.3) | 1287 (30.4) | 215 (36.3) | 1072 (42.9) | 2941 (33.7) | 46 (26.7) |
| COPD | 373 (2.3) | 102 (2.4) | 10 (1.7) | 52 (2.1) | 204 (2.3) | 5 (2.9) |
| Osteoporosis | 106 (0.7) | 34 (0.8) | 5 (0.8) | 10 (0.4) | 56 (0.6) | 1 (0.6) |
| Parkinson’s disease | 38 (0.2) | 7 (0.2) | - | 11 (0.4) | 19 (0.2) | 1 (0.6) |
| Epilepsy | 67 (0.4) | 23 (0.5) | 2 (0.3) | 14 (0.6) | 26 (0.3) | 2 (1.2) |
| Hip fracture | 35 (0.2) | 10 (0.2) | 1 (0.2) | 4 (0.2) | 20 (0.2) | - |
| Pneumonia | 316 (1.9) | 81 (1.9) | 6 (1.0) | 51 (2.0) | 176 (2.0) | 2 (1.2) |
| Overall | Aflibercept | Bevacizumab | Dexamethasone | Ranibizumab | Pegaptanib | |
|---|---|---|---|---|---|---|
| TOTAL, N (%) | 16,226 | 4230 (26.1) | 593 (3.6) | 2500 (15.4) | 8731 (53.8) | 172 (1.1) |
| Number of concomitant drugs | ||||||
| Mean (standard deviation) | 8.6 (5.3) | 8.4 (5.0) | 8.5 (5.1) | 9.3 (5.4) | 8.6 (5.3) | 9.2 (5.8) |
| Median (interquartile range | 8.0 (5.0–12.0) | 8.0 (5.0–11.0) | 8.0 (5.0–11.0) | 9.0 (5.0–12.0) | 8.0 (5.0–12.0) | 8.5 (5.0–12.0) |
| Group, N (%) | ||||||
| 0 | 447 (2.8) | 122 (2.9) | 20 (3.4) | 39 (1.6) | 260 (3.0) | 6 (3.5) |
| 1–2 | 1249 (7.7) | 336 (7.9) | 49 (8.3) | 148 (5.9) | 711 (8.1) | 5 (2.9) |
| 3–5 | 3202 (19.7) | 835 (19.7) | 102 (17.2) | 484 (19.4) | 1746 (20.0) | 35 (20.3) |
| 6–9 | 4992 (30.8) | 1369 (32.4) | 205 (34.6) | 745 (29.8) | 2622 (30.0) | 51 (29.7) |
| 10+ | 6336 (39.0) | 1568 (37.1) | 217 (36.6) | 1084 (43.4) | 3392 (38.9) | 75 (43.6) |
| Type of concomitant drug (ATC code), N (%) | ||||||
| Digoxin (C01AA05) | 300 (1.8) | 63 (1.5) | 14 (2.4) | 32 (1.3) | 187 (2.1) | 4 (2.3) |
| NSAIDs (M01) | 7137 (44.0) | 1791 (42.3) | 268 (45.2) | 1049 (42.0) | 3942 (45.1) | 87 (50.6) |
| Low-dose aspirin (B01AC06; B01AC30 | 5760 (35.5) | 1467 (34.7) | 205 (34.6) | 1069 (42.8) | 2951 (33.8) | 68 (39.5) |
| Antibacterial (J01) | 10,207 (62.9) | 2573 (60.8) | 387 (65.3) | 1584 (63.4) | 5536 (63.4) | 127 (73.8) |
| Anti-thrombotic (B01) | 8486 (52.3) | 2170 (51.3) | 294 (49.6) | 1628 (65.1) | 4296 (49.2) | 98 (57.0) |
| Drugs for peptic ulcers (A02) | 9209 (56.8) | 2349 (55.5) | 323 (54.5) | 1451 (58.0) | 4987 (57.1) | 99 (57.6) |
| Organic nitrates (C01DA) | 815 (5.0) | 176 (4.2) | 40 (6.7) | 106 (4.2) | 474 (5.4) | 19 (11.0) |
| Corticosteroids (H02) | 2846 (17.5) | 749 (17.7) | 84 (14.2) | 562 (22.5) | 1425 (16.3) | 26 (15.1) |
| Antihypertensives (C02) | 1059 (6.5) | 244 (5.8) | 41 (6.9) | 192 (7.7) | 572 (6.6) | 10 (5.8) |
| Anti-dyslipidaemic agents (C10) | 6863 (42.3) | 1779 (42.1) | 239 (40.3) | 1100 (44.0) | 3660 (41.9) | 85 (49.4) |
| Overall | Aflibercept | Bevacizumab | Dexamethasone | Ranibizumab | Pegaptanib | |
|---|---|---|---|---|---|---|
| TOTAL, N (%) | 16,226 | 4230 (26.1) | 593 (3.6) | 2500 (15.4) | 8731 (53.8) | 172 (1.1) |
| History of proxy of diabetes-related eye disease, N (%) | ||||||
| Diabetes | 5545 (34.2) | 1283 (30.3) | 214 (36.1) | 1071 (42.8) | 2931 (33.6) | 46 (26.7) |
| Argon-laser retina (and laser photocoagulation) | 1205 (7.4) | 164 (3.9) | 61 (10.3) | 345 (13.8) | 622 (7.1) | 13 (7.6) |
| Younger than 55 at first injection | 1310 (8.1) | 257 (6.1) | 54 (9.1) | 267 (10.7) | 724 (8.3) | 8 (4.7) |
| Any proxy among the previous | 6679 (41.2) | 1478 (34.9) | 267 (45.0) | 1378 (55.1) | 3501 (40.1) | 55 (32.0) |
| History of glaucoma, N (%) | 617 (3.8) | 146 (3.5) | 26 (4.4) | 79 (3.2) | 360 (4.1) | 6 (3.5) |
| History of use of ophthalmic services, Mean (SD) | ||||||
| Specialist encounter | 2.0 (2.1) | 1.6 (1.8) | 1.5 (1.8) | 2.3 (2.3) | 2.1 (2.1) | 3.2 (2.8) |
| OCT | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) |
| Fluorescence imaging | 0.7 (0.9) | 0.5 (0.8) | 0.6 (0.7) | 0.6 (0.8) | 0.7 (0.9) | 1.0 (1.0) |
| Fluorescence imaging with indocyanine | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) |
| Fundus photography | 0.0 (0.2) | 0.0 (0.2) | 0.0 (0.1) | 0.0 (0.2) | 0.0 (0.1) | 0.0 (0.2) |
| Possible binocularity during the first year of follow-up period, N (%) | 1612 (9.9) | 531 (12.6) | 76 (12.8) | 167 (6.7) | 828 (9.5) | 10 (5.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucenteforte, E.; Finocchietti, M.; Addis, A.; Tettamanti, M.; Varano, M.; Parravano, M.; Virgili, G. Polytherapy and Multimorbidity Pattern of Users of Anti-VEGF Drugs and Dexamethasone for the Treatment of Age-Related Macular Degeneration and other Vascular Retinopathies in Clinical Practice. Pharmaceuticals 2023, 16, 646. https://doi.org/10.3390/ph16050646
Lucenteforte E, Finocchietti M, Addis A, Tettamanti M, Varano M, Parravano M, Virgili G. Polytherapy and Multimorbidity Pattern of Users of Anti-VEGF Drugs and Dexamethasone for the Treatment of Age-Related Macular Degeneration and other Vascular Retinopathies in Clinical Practice. Pharmaceuticals. 2023; 16(5):646. https://doi.org/10.3390/ph16050646
Chicago/Turabian StyleLucenteforte, Ersilia, Marco Finocchietti, Antonio Addis, Mauro Tettamanti, Monica Varano, Mariacristina Parravano, and Gianni Virgili. 2023. "Polytherapy and Multimorbidity Pattern of Users of Anti-VEGF Drugs and Dexamethasone for the Treatment of Age-Related Macular Degeneration and other Vascular Retinopathies in Clinical Practice" Pharmaceuticals 16, no. 5: 646. https://doi.org/10.3390/ph16050646
APA StyleLucenteforte, E., Finocchietti, M., Addis, A., Tettamanti, M., Varano, M., Parravano, M., & Virgili, G. (2023). Polytherapy and Multimorbidity Pattern of Users of Anti-VEGF Drugs and Dexamethasone for the Treatment of Age-Related Macular Degeneration and other Vascular Retinopathies in Clinical Practice. Pharmaceuticals, 16(5), 646. https://doi.org/10.3390/ph16050646






