Abstract
Calendula officinalis Linn. (CO) is a popular medicinal plant from the plant kingdom’s Asteraceae family that has been used for millennia. This plant contains flavonoids, triterpenoids, glycosides, saponins, carotenoids, volatile oil, amino acids, steroids, sterols, and quinines. These chemical constituents confer multifaceted biological effects such as anti-inflammatory, anti-cancer, antihelminthic, antidiabetes, wound healing, hepatoprotective, and antioxidant activities. Additionally, it is employed in cases of certain burns and gastrointestinal, gynecological, ocular, and skin conditions. In this review, we have discussed recent research from the last five years on the therapeutic applications of CO and emphasized its myriad capabilities as a traditional medicine. We have also elucidated CO’s molecular mechanisms and recent clinical studies. Overall, this review intends to summarize, fill in the gaps in the existing research, and provide a wealth of possibilities for researchers working to validate traditional claims and advance the safe and effective use of CO in treating various ailments.
1. Introduction
The use of traditional medicine was found to be first implemented in Ancient Greece. According to Greek traditional knowledge, gods gave the knowledge of healing to man. Theophrastus (372–286 BC), a disciple of Aristotle, an ancient Greek philosopher, and a scientist, authored the first scientific system of plants [1]. Although not wholly aware of their exact physicochemical characteristics at the time, the human population has found additional health benefits from plants throughout history. The same components from plant sources that have a long medicinal history and are proven effective in the welfare of human health are indicated within traditional medicine. This traditional medicinal knowledge and colonial expansion through the progress of communication mediums have been transferred over the generations [1,2]. Currently, traditional medicines are becoming more popular for therapeutic use, specifically for self-treatment practices [3,4,5].
Calendula officinalis Linn. (CO), as an important plant within traditional medicine, has found application in the food industry [6] as well as the pharmaceutical industry [7] owing to the presence of secondary metabolites in the plant. The Calendula genus covers approximately 25 species, among which C. officinalis, C. arvensis, C. tripterocarpa, C. stellata, and C. suffruticose are the most common [8]. CO is the most studied species of Calendula. It has been used medicinally since the 12th century [9,10] and is known as English Marigold, Pot Marigold, Holigold, Mary Bud, Marybud, or Mary Gowles. The name Calendula originates from the Latin term “calends” denoting the first day of each month when the Calendula flower blooms. Along with this, Calendula has also been referred to as the “herb of the sun”, considering the efflorescence of Calendula flowers in the morning and their shriveling in the evening. For a long period, this traditional herb has been used to treat minor burns, wounds, and skin problems. Currently used CO medicines include pot marigold tincture and carophyllenic ointment, which both contain carotenoids derived from the flowers. It is one of the ingredients of the branded homeopathic drug Traumeel®, which is intended to relieve the pain and swelling brought on by sudden musculoskeletal injuries [11]. Moreover, many sources suggest using Calendula petal powder as an economical substitute for saffron because its coloring and flavoring aided in food products in early times [10].
CO is a self-seeding, annual plant species that grows to a height of 12–18 inches and is found near warm and humid atmospheric conditions [12]. A 5 to 7 cm composite flower head rests on the plant’s stem. The flower head consists of an epicalyx of multiple tapered lanceolate sepals, compactly overlayed on each of the two sides by glandular hairs and yellow-orange tubular florets on the interior side [9,13]. CO powder is a yellowish-brown powder with a distinctive aromatic smell and a mildly bitter taste. It contains normocytic stomata in the outer epidermis’ apical region, fragments of the corolla, covering and glandular trichomes, elongated sclerenchymatous cells, fragments of the walls of the ovaries containing brown pigment, pollen grains, fragments of stigma, and fibrous fragments. CO plants are abundantly seen in Central Europe and the Mediterranean regions [14,15]. It is also found in Middle Eastern countries, specifically Cyprus, Turkey, and Iran. In addition, Calendula cultivation has also been observed in India and China on a larger scale [16,17].
It is considered a safe medication when considering its therapeutic potential with a proper dose and other pharmacological indications [9,18]. Some toxicological studies have even proven the safety of acute and subacute administration of Calendula in terms of biochemistry and physical parameters. According to the European Medicines Agency, CO oil is classified as a herbal medical product and has a claimed LD 50 (lethal dose 50) value of 20 mL/kg of body weight [10,19].
This review congregates the hitherto scattered reports on the pharmacological activities of CO from the last five years. Nonetheless, we aim to highlight the importance of CO as a natural remedy for therapeutic purposes based on the positive data that has been documented in the literature. In summary, the objective of this review is to provide a summary, fill in the gaps in the existing research, and present a multitude of possibilities to researchers already working on the validation of traditional claims and the development of CO’s use in the safe and effective treatment of a variety of diseases.
2. Chemical Composition
Some of the important components in CO pharmacological activities belong to different classes of chemical compounds, terpenoids, flavonoids, triterpeneol esters, steroids, phenolic compounds, carotenes, triterpenoids, essential oils, quinones, fatty acids, minerals, saponins, carbohydrates, sterols, and tocopherols [20,21]. In various regions of CO, the compounds ubiquinone, tocopherol, phylloquinone, and proto-quinone were identified from quinones. From the petroleum ether extract of CO flowers, terpenoids were extracted [22,23]. Some other phytoconstituents present in CO are paraffins, calendin, and calendulin [12]. All these secondary metabolites increase the importance of CO as traditional medicine. Carotenoids and triterpene alcohols, in both free and esterified forms, are also present in CO [24]. Co-derived carotenoid pigments [25] and other polyunsaturated fatty acids produced from CO, such as Calendric acid [26], have been demonstrated to have anti-inflammatory activities in vitro and in vivo [27]. Nonetheless, triterpene oligoglycosides and calendasaponins A, B, C, and D from CO have proven to exhibit gastric-emptying-inhibitory, gastroprotective, and hypoglycemic properties [28]. CO leaf extract contains fatty acids, triterpenes, chloroform extracts, and sterols. In the aqueous extract, flavonoids and saponins were identified, and alkaloids were also found in the ethanolic extract. In various regions of CO, the compounds ubiquinone, tocopherol, phylloquinone, and proto-quinone were identified from quinones. From the petroleum ether extract of CO flowers, terpenoids were extracted [22,23]. CO was also used to extract flavonoids such as quercetin, isorhamnetin, and isoquercetin. Some other phytoconstituents present in CO are paraffins, calendin, and calendulin.
Table 1 represents the major constituents and percentages of various Calendula species, and Table 2 represents the various chemical constituents present in CO.

Table 1.
The major constituents and percentages of various Calendula species [29].

Table 2.
Various chemical constituents are present in Calendula officinalis Linn.
2.1. Carotenoids
The flower of CO, which is primarily orange, has high levels of carotenoids. The number of carotenoids in CO inflorescences increased significantly. Orange CO species include more hydrocarbons than yellow ones, which mainly contain oxygenated derivatives [25].
Carotenoids, which are pre-eminently found in plant flowers, majorly consist of lycopene, beta carotene, lutein, flavoxanthin, and zeaxanthin. Some of the other carotenoids found in petals and pollens of CO are luteoxanthin, neoxanthin, violaxanthin, 9Z-Violaxanthin, 9Z-Neoxanthin, auroxanthin, 9Z-Anthroxanthin, mutatoxanthin, 13/13′Z-Lutein, α-cryptoxanthin, z-cryptoxanthin, 9/9′Z-lutein, α-carotene, β-carotene, and β-cryptoxanthin. In addition to this, carotenoids found in the stem and leaves of CO include violaxanthin, 9Z-Violaxanthin, 9Z-Neoxanthin, antheraxanthin, neoxanthin, mutatoxanthin epimer 1 and 2, 9/9′Z-Lutein, β-carotene, α-cryptoxanthin, lutein, luteoxanthin, β-cryptoxanthin, and 13Z-Violaxanthin [51,52]. Carotenoids are predominantly known for their antioxidant activity through a radical scavenging mechanism, which makes them extremely useful in the pharmacotherapy of oxidative disorders. The same antioxidant potential and their ability to form artificial cross-linkage make them possess wound-healing action [25,53,54]. Zeaxanthin, a non-provitamin A carotenoid belonging to the xanthophyll family, is known to have a beneficiary therapeutic effect on age-related macular degeneration through its antioxidant and blue-filtering potential [55].
2.2. Terpenoids
Terpenoids, which are primarily present in flowers and roots of CO, are majorly known for their antioxidant activity. These sesquiterpenoids, entailing τ-cadinol, α-cadinol, and τ-muurolol, bring out antioxidant action through a radical scavenging mechanism. Thus, terpenoids have a significant role in the management of diseases and disorders involving oxidative reactions such as Alzheimer’s disease, skin hyperpigmentation, and diabetes-related complications. In addition to this, terpenoids have extensive anti-inflammatory action. This action is brought about by the inhibition of the COX-2 enzyme (Cyclo-oxygenase-2), pro-inflammatory cytokines including Interleukins 1 and 6, tissue necrosis factor, and synthesis of prostaglandins [22,23].
2.3. Flavonoids
Flavonoids present in CO, especially quercetin, have significant wound-healing activity. There are several proposed mechanisms for this action. The basic mechanism of action is the antioxidant activity brought about through radical scavenging action. Another mechanism explains the adhesion and augmentation of fibroblasts, which additionally cause an approbatory effect on the cellular activity in a given area [56,57]. Additionally, flavonoids are known to have anti-plaque and anti-gingivitis action [58,59]. Quite a few mechanisms are suggested for this action, including removal of plaque through inhibition of lysosomal hydrolase, reduction in collagen degradation through inhibition of recombinant human matrix metalloproteinases (MMPs), and subsequent increment in collagen concentration. Furthermore, other constituents of CO belonging to the flavonoid class such as rutin, apigenin, kaempferol, vitexin, and luteolin are known to have skin-protective action through the antioxidant mechanism. In addition to this, flavonoid compounds quercetin and rutin possess anti-depressant action. These compounds produce their action through the inhibition of Monoamine (MAO) oxidases and reduction in GABA levels [60,61,62]. Isorhamnetin with quercetin derivatives such as 3-O-(2″-rhamnosyl)-rhamnosides, 3-O-(2″-rhamnosyl)-glucosides, 3-O-(2″,6″-di-rhamnosyl)-glucosides, 3-O-(6″-rhamnosyl)-glucosides, 3-O-glucosides, and 3-O-(6″-acetyl)-glucosides are known to have anti-acetylcholinesterase activity. This activity is chemically attributed to the presence of acetyl and rhamnosyl groups in flavonoid structure [27]. Hyperoside, another flavonoid class compound, has a crucial effect on the management of osteosarcoma through restraining multiplication and stimulation of osteogenic differentiation of sarcoma cells [63].
2.4. Coumarins
Coumarins, which are significantly found in flowers of CO, may prevent oxidative damage to cells [54]. Some of the important coumarins present in CO are Umbelliferone, Scopoletin, and Esculetin. Umbelliferone, using the antioxidant mechanism of action, acts as a skin-protective agent, especially in sunscreen products. Scopoletin has spasmolytic action: it acts by constraining the spastic contraction of muscles of the urogenital system and gastrointestinal system. Esculetin, which is from the same class of coumarins, acts as a phlebotonic and inflammatory agent by decreasing the permeability of capillaries and rejuvenating venous tone. In addition to this, it is also known to have anti-thrombotic action owing to its revelatory effect in the augmentation of the occlusion period for thrombotic platelet plug formation [64,65].
2.5. Phenolic Acids
Phenolic acids found in CO such as caffeic acid, vanillic acid, chlorogenic acid, and coumaric acid have proven scavenging activity because of their hydrogen-donating tendency, which makes them useful in the treatment of oxidative disorders [66]. The same mechanism of action explains the role of phenolic compounds from CO in the reduction in exercise-instigated oxidative stress [67,68,69]. CO contains various fatty acids such as calendic acid, linoleic acid, oleic acid, palmitic acids, and dimorphecolic acid. Among all fatty acids with a crucial role in human bodily functions, calendic acid, a major fatty acid found in CO, has additional predominant cytotoxic action. The mechanism of this action is lipid peroxidation and downregulation of the gene lcf1, which is involved in the encoding of long-chain fatty acyl-CoA synthetase [70,71,72].
Some of the fatty acid derivatives from CO are 28-O-β-D-glucopyranosyl ole-anolic acid 3-O-β-D-galactopyranosyl (1→3)-β-D-glucuronopyranoside (calendulaglycoside C) [73], 28-O-β-D-glucopyranosyl oleanolic acid 3-O-β-D-glucuronopyranoside (chikusetsusaponin or glycoside F) [74], oleanolic acid 3-O-β-D-galactopyranosyl (1→3)-β-D-glucuronopyranoside (calenduloside G) [75], 28-O-β-D-glucopyranosyl oleanolic acid 3-O-β-D-glucopyranosyl-(1→2)-[β-D-galactopyranosyl-(1→3)]-β-D-glucuronopyranoside (calendulaglycoside A) [42], 28-O-β-D-glucopyranosyl oleanolic acid 3-O-β-D-galactopyranosyl (1→3)-β-D-glucopyranoside (calenduloside B) [73], oleanolic acid 3-O-β-D-glucopyranoside (Glucoside I) [76], 3-O-β-D-glucopyranosyl-(1→2)-[β-D-galactopyranosyl-(1→3)]-β-D-glucopyranosyl olea-nolic acid (osteosaponin-I) [77], oleanolic acid, 3-O-β-D-galacto-pyranosyl-(1→3)-β-D-glucopyranosyl oleanolic acid (arvensoside B) [78], stigmasterol and machaerinic acid 3-O-β-D-glucuronopyranoside [79].
2.6. Quinones
Quinones that are majorly found in the leaves of CO consist of phylloquinone, α-tocopherol, ubiquinone, and plastoquinone. They have anti-cancer potential, and their mechanism of action is alkylation and cleavage of DNA through DNA topoisomerase I and II [80,81].
Other minor components of CO such as phenolics and tannins are known to have antioxidant action as well as anti-ulcer action, which is rendered through maintenance as well as regeneration of gastric mucosa [82].
2.7. Amino Acids
Threonine, glutamic asparagine, leucine, proline, acid, serine, histidine, phenylalanine, tyrosine, arginine, lysine, aspartic alanine, methionine, and valine are some of the amino acids that are present in CO that have been detected in its stems, leaves, and flowers. Around 5% of amino acids were found to be present in the leaves, 3.5% in the stems, and 4.5% in the flowers [83].
The chemical structures of some of the important chemical constituents present in CO are shown in Figure 1.
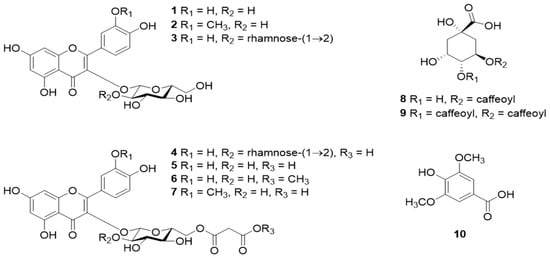
Figure 1.
Chemical structures of constituents of CO. (1), isorhamnetin 3-O-β-glucoside (2), quercetin 3-O-β-neohesperidoside (3), quercetin 3-O-(2″-O-α-rhamnosyl-6″-O-malonyl)-β-glucoside (4), quercetin 3-O-(6″-O-malonyl)-β-glucoside (5), quercetin 3-O-6″-O-methyl malonyl)-β-glucoside (6), isorhamnetin 3-O-(6″-O-malonyl)-β-glucoside (7), chlorogenic acid (8), 3,4-dicaffeoylquinic acid (9), and syringic acid (10). Adapted from [84] under Creative Commons CC BY license (CC BY 4.0).
For the extraction of CO, numerous conventional and novel techniques are available. Conventional techniques used in past decades are hydrodistillation, solvent extraction, steam distillation, acid-catalyzed extraction, maceration, expression, and soxhlet extraction [85,86,87,88,89]. The most common solvents used in these processes are methanol, ethanol, acetone, and hexane. Here, due to the presence of high phenolic content, solvents with high polarity are employed; for example, 80% methanol, when used in the extraction process, leads to higher output in terms of the components yield [15,23,90]. Nevertheless, these conventional techniques are challenging because of prolonged extraction time, temperature, and pressure conditions. Here novel techniques such as ultrasound-assisted extraction, microwave-assisted hydrodistillation, microwave distillation, headspace solid-phase microextraction, and headspace–cold finger extraction come into the picture, which support numerous aspects such as enhanced extraction, in terms of yield and quality of extracts, and economical as well as ecological advantages [86,91,92,93,94].
3. Therapeutic Applications of Calendula officinalis
Many ailments have been treated with CO; a plant frequently used in homeopathic medicine. Additionally, it can be cytotoxic and inhibit tumor growth [95]. It functions as an antimicrobial [56,96], antioxidant [97], anti-inflammatory [89,98], antiseptic [99], anti-viral [89], hepatoprotective [56], and antidiabetic medicine [100]. It is also applied to the skin to treat various conditions, including inflammation of the skin, open wounds, and laceration wounds that bleed. Additionally, it is used to heal minor ailments such as razor burns and wind burns. The major parts of the CO plant and their therapeutic applications discussed in this review are represented in Figure 2 and Table 3.
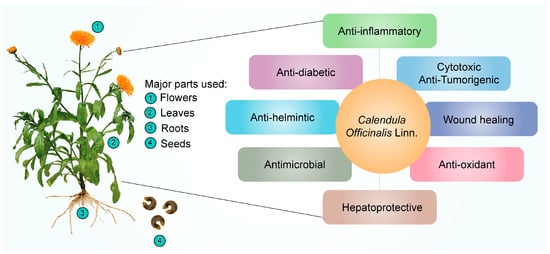
Figure 2.
Pharmacological effects of Calendula officinalis Linn.

Table 3.
Summary of clinical studies of the use of Calendula officinalis.
3.1. Anti-Inflammatory
CO is currently being investigated, as it exhibits excellent anti-inflammatory activity. Alkaloids, tannins, flavonoids, essential oils, sterols, saponins, carotenoids, triterpene alcohols, mucilage, polysaccharides, and resin are only a few of the categories of secondary metabolites that the plant has that are correlated with the anti-inflammatory characteristics [110]. Dried flower heads or dried ligulate flowers are plant components that are utilized in medicine and cosmetics. The ligulate flowers are rich in triterpene alcohols, triterpene saponins, fatty acid esters, flavonoids, carotenoids, coumarins, hydrocarbons, essential oils, and fatty acids [111]. Using in vivo pharmacological testing, it has been determined that the triterpenoid fatty acid esters are responsible for the anti-inflammatory effects of Calendula flowers. The lauryl, myristoyl, and palmitoyl esters of faradiol are the most prevalent of these [112], demonstrating that flower extract of CO was much more effective for treating both acute (caused by dextran and carrageenan) and chronic (caused by formalin) swelling in mice. They hypothesized that it may be attributed to the inhibition of the production of proinflammatory cytokines (IL-6, interleukin 6; IL-1β; TNF-α, tumor necrosis factor α; and IFN-γ, interferon γ) and COX-2 (cyclooxygenase 2), and subsequently, Refs. [112,113] demonstrated the anti-inflammatory activity of CO extract and investigated its effects on nitric oxide production. The results revealed that the CO extract inhibited nitric oxide production in a dose-dependent manner, with cytotoxicity only observed at 147 μL/mL concentrations or above.
Garrido-Suárez [98] studied the antinociceptive effects of CO cream on inflammatory hyper-nociception. Rats were subjected to several tests, and it was reported that CO cream (20% or 30% w/w), when applied topically, led to a significant decrease in TNF-α and suppression of COX-2. Pharmaceutical formulations such as nanoemulsion [114] have also been developed to achieve the anti-inflammatory effects of CO. Furthermore, the scientists discovered that all three samples of Calendula extract (3, 5, and 7%) had beneficial effects on healing and soothing wounds when applied to albino rats. The Calendula extract nanoemulsion has an anti-inflammatory impact on skin cells, according to the findings. The schematic representation of the anti-inflammatory effects of CO is shown in Figure 3. The aforementioned information reveals the potential uses of CO as an anti-inflammatory and analgesic agent. Considering this characteristic of CO, it was able to minimize dermatitis in newborns caused by diaper friction when compared to Aloe vera [101]. In the oral cavity, mouth rinsing with CO tincture reduced gingival inflammation [58].
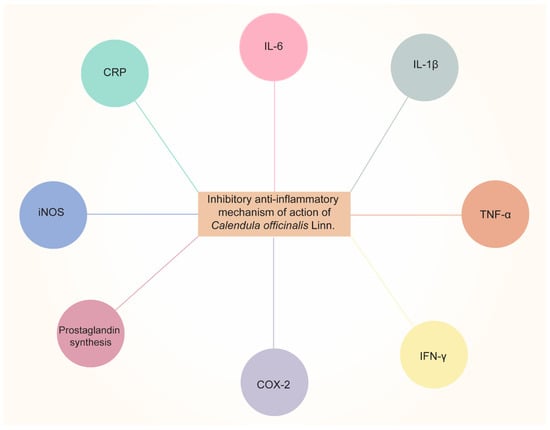
Figure 3.
Anti-inflammatory effects of Calendula officinalis Linn by inhibiting pro-inflammatory cytokines (IL-6, IL-1β, TNF-α, and IFN-γ, etc.), COX-2, prostaglandin synthesis, iNOS (inducible nitric oxide synthase), and CRP (C-Reactive Protein).
3.2. Antioxidant Activity
Plant polyphenols such as flavonoids are among the most significant natural compounds with active antioxidant properties. The radical scavenging or chelating flavonoids are caused by their hydroxyl group content [115,116]. The family of antioxidants [115] as phenolic chemicals, on the other hand, operate as free radical terminators [117]. Hence, CO’s high flavonoid and phenolic phytochemical content contribute to its antioxidant activity, which can further promote its strong radical-scavenging capacity and confer protective effects [104]. The leaves and petals of the CO plant contain natural sources of antioxidants [56]. As a result of riboflavin’s photoreduction, it has been claimed that CO extract scavenges hydroxyl and superoxide radicals. Pandey et al. [118] examined the antioxidant properties of the leaves and flowers of CO by using TBA (thiobarbituric acid) and FTC (ferric thiocyanate) techniques. The FTC technique calculated the amount of peroxide produced during the initial stage of linoleic acid peroxidation. The results revealed that the antioxidant concentration decreases with decreasing absorbance value. When compared to regular Vitamins C and E, the aqueous extract of leaves and petals exhibited a high level of antioxidant effect based on absorption rates. The fact that the aqueous extract of the petals displayed lower absorbance with both the FTC and TBA techniques suggests that the petals possessed more antioxidant activity than the leaves.
Based on the evidence, it can be concluded that CO extracts may be extremely beneficial in treating several ailments such as AIDS (acquired immunodeficiency syndrome), heart disease, malaria, diabetes, stroke, cancer, and arteriosclerosis due to their potent antioxidant activity.
3.3. Cytotoxic and Anti-Tumor Activity
Saponin, one of the separated active compounds of CO, has been shown to exhibit antimutagenic action [119]. The interest in the purported anti-tumor activity of CO extracts and components has grown with the rise of complementary and alternative medicine based on herbs as cancer treatment. Cruceriu et al. [120] demonstrated the anti-tumor activity of methanolic extracts of CO using a cell line study. The authors reported that CO extracts could exert anti-cancer activity by inducing apoptosis, activating caspase 3 and caspase 7 at a protein level, and downregulating cyclin D1, D3, A, E, and several cyclin-dependent kinases. Furthermore, BAX (Bcl2 associated X protein) and BBC3 (Bcl2 binding component), two proapoptotic genes, were upregulated and NF-κB (nuclear factor kappa-light-chain enhancer of activated B cells) and STAT3 (signal transducer and activator of transcription factor 3) were downregulated after the treatment with CO extracts. Similarly, Hernández-Rosas et al. [121] demonstrated the in vitro cytotoxic effects of hydro-alcoholic extract of CO on human cancer cell lines. The authors found that the biological activities of high free-radical scavenging capacity (ABTS; 2,2-azino-bis (3-ethylbenzothiazoline-6sulfonic acid, DPPH; 2,2-diphenylpicrylhydrazyl), moderate ability to neutralize hydroxyl radicals, effective metal chelation, and strong reducing capacity are responsible for the anti-cancer effect.
Clinical studies have shown the use of CO in different presentations. At the beginning of the 20th century, the clinical study conducted by Pommier et al. [102] showed the efficacy of Calendula ointment as adjuvant therapy when compared to trolamine for acute dermatitis during irradiation in the treatment of breast cancer. In another study, promising results showed the use of CO gel on oral leukoplakia when compared to lycopene gel [103]. In oral mucositis, the 2% CO mouthwash was able to decrease oral mucositis when compared to the placebo group [104].
In conclusion, there are encouraging findings about CO’s prospective usage in cancer management, particularly in cancer prevention, treatment of cancer, and palliative care for cancer patients. However, progress to pertinent preclinical studies is impeded without understanding the bioactive components responsible for the in vitro and in vivo selective cytotoxicity and for preventing radiotherapy-induced adverse effects. As a result, further study is required to find novel components of CO that have the potential to become useful bioactive components in the treatment of cancer.
3.4. Wound-Healing Activity
Chronic wounds and delayed wound healing are major medical issues that provide difficult clinical challenges for doctors and have profound socioeconomic consequences. Since ancient times, herbs and their preparations have been utilized in addition to traditional medicines to expedite the healing of wounds. In this context, preparations (alcoholic and lipophilic) made from the flowers of CO have received stellar reviews for treating mild skin inflammations and slow-healing wounds. This is accomplished by enhancing the amount of blood and oxygen delivered to the wound site, which encourages the body to produce new tissue. CO plants’ dried petals are used to make tinctures, ointments, and washes to cure mild infections, scrapes, bruises, and burns. CO also contributes to maintaining calmed, hydrated skin by encouraging the development of collagen, a necessary protein for radiant skin.
Deka et al. [99] stated that CO could dramatically increase wound angiogenesis and collagen metabolism, which results in scar softening and emollient characteristics. The floral extract of CO, when applied topically and orally, has therapeutic properties for burns and wounds. An increase in collagen-hydroxyproline and hexosamine shows that the person or animal being treated is mending their wounds. Gunasekaran et al. [122] demonstrated the wound-healing activity of CO in the winter strain of albino rats. The results revealed that a herbal ointment containing CO could inhibit the activation of macrophages and speed up the migration and proliferation of keratinocytes and fibroblasts, which were responsible for wound healing. This was accomplished by preventing the release of proinflammatory cytokines and reducing oxidative stress at the wound site. The mechanism of action of CO for wound healing is shown in Figure 4.
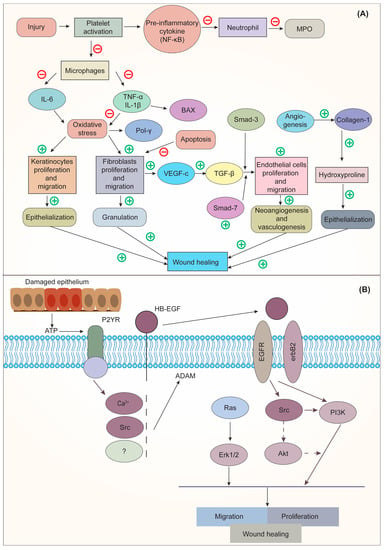
Figure 4.
(A). Mechanism of action of CO on Interleukin 6 (IL-6); (B) Mechanism of action of epidermal growth factor (EGF) on wound healing. Adapted from [122] under Creative Commons CC BY license (CC BY 4.0). NF-κB, nuclear factor kappa-light-chain-enhancer of activated B cells; MPO, myeloperoxidase; IL-6, interleukin-6; TNF-α, tumor necrosis factor alpha; IL-1β, interleukin-1-beta; BAX, BCL-2 associated x protein; Pol γ, DNA polymerase γ; SMAD, suppressor of mothers against decapentaplegic; VEGF-c, vascular endothelial growth factor C; TGF-β, transforming growth factor-beta; ATP, adenosine triphosphate; P2YR, purinergic G protein-coupled receptors; HB-EGF, heparin-binding EGF-like growth factor; EGFR, epidermal growth factor receptor; RAS, rat sarcoma; ERK1/2, extracellular signal-regulated kinase; Src, steroid receptor coactivator; Akt, protein kinase B; PI3K, phosphoinositide 3-kinase.
Similarly, Rathod and co-workers [123] investigated the wound-healing efficacy of CO-loaded collagen films on wounds induced in Wistar rats. On day 21, the rate of wound contraction in the developed CO film was considerably higher than in the control group, the placebo-treated group, and the marketed-product-treated group. In a randomized controlled trial, the CO-containing ointment was studied on 72 qualified primiparous females for cesarean wound healing. According to the findings, applying CO ointment to the wound after a cesarean significantly boosted the rate of wound healing. It can be successfully employed to speed up the cesarean healing process [124].
It is important to note that clinical studies have already been conducted in order to evaluate the efficacy of the use of CO in the healing of hand and finger wounds by secondary intention. In this perspective, there is evidence showing that CO extract is favorable for the treatment of these wounds by reducing the epithelialization time and increasing the healing speed [105]. In chronic wounds, such as venous ulcers, the use of CO also obtained positive results, showing that the treatment with topical CO reduces the surface area of the lesion, achieves greater epithelialization in less time, and accelerates healing time [106]. In addition, this type of healing is advantageous because it reduces medical interventions and treatment costs [125]. Another important finding is that the use of CO ointment after episiotomy reduces pain, redness, and swelling and helps healing [107].
3.5. Hepatoprotective Activity
Most substances that enter the body are processed by the liver, which is also in charge of detoxification. Up to 83% of all pathological cases worldwide are hepatotoxic, making it the most prevalent disease. The main causes of liver toxicity include hepatitis, viral infections, dietary additives, alcohol, toxic industrial chemicals, air pollution, and water pollution. Researchers have shown that CO extracts can protect the liver from the cytotoxicity and oxidative stress caused by carbon tetrachloride. This results in a rise in the amount of total hemoglobin. Similarly, in vitro and in vivo models of the flowers’ hydro-alcoholic extract show decreased hepato-cytolysis and liver biomarkers. The treatment with ethanolic extract brought back normal levels of hepatic blood markers, increased the level of total thiols, decreased levels of total antioxidant status, decreased levels of antioxidant enzymes (CAT, catalase; SOD, superoxide dismutase; GPx, glutathione peroxidase; and GST, glutathione s-transferases) and decreased the levels of malondialdehyde and total oxidant status in both the blood and the hepatocytes. Furthermore, restoration of cellular antioxidant levels, specifically enhanced levels of reduced glutathione enzymatic components and total thiols of the antioxidant system, was also observed, which may be due to the polyphenolic chemicals in CO that protect the cells from chemically induced cellular damage. Moreover, in a dose-dependent manner, CO extract improved the histological picture of the liver, as well as the biochemical parameters and inflammatory cytokines [126].
3.6. Anthelmintic Activity
In addition to being a major cause of illness in humans and animals, parasitic infections also negatively impact the economy. Due to increased resistance to conventional antihelminthic treatments, there has been a quantum leap toward investigating herbal medicines. Herbs such as CO have been used for centuries to combat parasitic illnesses, and they are still utilized for that purpose in many countries. In a study, Khursheed et al. [89] investigated the anthelmintic activity in adult Indian earthworms (Pheretima posthuma). It was observed that the ethanolic extracts of CO exhibited anthelmintic activity (paralysis of the worms followed by death) at 10 mg/mL concentration compared with the standard drug, albendazole. CO was also proven to show anthelminthic activity against Ascaris suum [127] and 50% efficacy on L1-2 larvae of Strongiloides papillosus [128].
3.7. Antimicrobial Activity
Although antibiotics have played a significant part in the treatment of infectious diseases caused by bacteria and fungi for the past 60 years, it has been observed that the occurrence of dangerous bacteria that are resistant to antibiotics has increased in frequency over the course of the past several decades [129]. Because there are a number of different mechanisms by which drug resistance can be manifested, finding a solution to this issue is not likely to be an easy challenge. Because of the growing prevalence of drug-resistant pathogens, there is an immediate and pressing requirement to discover and isolate new bioactive compounds derived from medicinal plants using standardized and contemporary analytical methods. Compounds obtained from medicinal plants might provide unique and relatively simple techniques to treat pathogenic microbes. CO extracts have also proven to be effective as antimicrobial agents [36].
3.7.1. Antibacterial Activity
It is of the utmost significance to discover novel antibacterial medicines in view of the research that shows the rapid global spread of clinical isolates that are resistant to antibiotic treatment. A large variety of medicinal plants have been identified as useful sources of natural antibacterial agents as alternative choices that have the potential to be successful in the treatment of several bacterial diseases [130]. The antibacterial properties of a variety of plants, which are caused by the production of phytochemicals during the secondary metabolism of the plant, have led to their adoption in a wide range of fields. Tannins, alkaloids, phenolic compounds, and flavonoids are just examples of the large range of secondary metabolites that are abundant in plants. These metabolites have been shown to exhibit antibacterial effects when tested in vitro [131,132,133].
CO has also been shown to possess potent antibacterial properties. Recently, Karnwal [134] studied the antibacterial potential of CO. It was observed that the minimum inhibitory concentration (MIC) with CO aqueous extracts was 3.75 % for Clostridium perfringens, Staphylococcus aureus, Pseudomonas aeruginosa, and Listeria monocytogenes. For Listeria monocytogenes, Clostridium perfringens, and Staphylococcus aureus, however, the lowest MBC (1.87%) was observed. Ethanolic extract of CO showed the lowest MIC and MBC for just one bacterial pathogen, and that was Pseudomonas aeruginosa, with 3.75% and 1.87%, respectively. The antibacterial property of CO was also compared to sodium hypochlorite against Streptococcus mutans as a root-canal-irrigating solution by Yalgi et al. [135]. It was observed that CO showed a significant CFU reduction in S. mutans, i.e., from 15.85 CFU to 1.20 CFU. The results were comparable to those of the group treated with sodium hypochlorite. The authors reported that the antibacterial effect may be attributed to the presence of terpene alcohols and terpene lactones in CO. Darekar et al. [136] also investigated the antibacterial potential of CO against Bacillus subtilis, Klebsiella pneumonia, Staphylococcus aureus, and Enterococcus faecalis using the disc diffusion method at a concentration of 10 mg/mL. The results revealed strong antibacterial activity of CO against the tested strains as indicated by their significant inhibition zones. Shahen and coworkers [137] studied chemical compounds with bioactive properties from CO flowers and their antibacterial activity. The authors studied paper-disc agar diffusion and tube-dilution techniques to test growth inhibition and to calculate the minimum inhibitory concentration. Variable levels of antibacterial activity were shown by the leaf extract against various microorganisms. The largest inhibitory zone was generated by E. coli and K. pneumonia around the CO leaves, whereas B. subtilis and S. lutea were shown to be more resistant bacteria. E. coli had the least inhibitory effects. Calendula extracts in petroleum ether and chloroform showed antibacterial efficacy against B. subtilis and E. coli. This finding shows that several pathogens are strongly inhibited by leaf extracts of CO that were made using petroleum ether and chloroform.
3.7.2. Antiprotozoal Activity
An important global cause of death and morbidity is protozoal disease. Every year, malaria infects between 200 and 500 million people, killing 2 million of them, mostly young children under the age of 5 [138]. Future therapeutic agents must be found immediately, and understanding traditional medicine can help to pave the path for future developments in this area. However, due to the restricted availability and high cost of pharmaceutical treatments, it is estimated that two-thirds of the global population relies on traditional medicines. Additionally, it was discovered through global biological screens that many natural compounds had antiparasitic activities, often with a surprising potency and high selectivity. Samra et al. [139] studied the antiprotozoal activity of CO. The methanol extract of CO included a novel phytoconstituent called (6Z,9Z)-heptadeca-6,9-diene-5,11-dione (I). The structure of I was discovered by examining NMR spectra and HRESIMS data. For both antibacterial and antiprotozoal properties, tests were conducted. Compound I demonstrated mild antitrypanosomal activity with an IC50 of 37.6136 µM, leishmanicidal activity against L. donovani amastigote with an IC50 of 16.4394 µM and IC90 of 28.9015 µM, and leishmanicidal activity against L. donovani ecdysone. Standard experimental techniques were used to test compound I cytotoxicity against THP1 cells; however, no cytotoxicity was seen, demonstrating its selectivity and safety.
3.7.3. Antifungal Activity
According to the findings of the epidemiological studies, the incidence and prevalence of major fungal infections are likely to continue to be a concern for public health. Antifungal treatments have been used more often, which has resulted in the emergence of fungal strains that are resistant to these medications. It is vital to identify new classes of antifungals from natural products such as medicinal plants because of the rapid growth of drug-resistant strains of fungus that are resistant to several treatments. CO has been found to possess antifungal properties [140]. Vinola et al. [97] compared the antifungal activity of CO with 2% chlorhexidine against C. albicans. It was observed that compared to CO, chlorhexidine exhibits much higher antifungal activity against C. albicans. CO does, however, have some antifungal efficacy against C. albican. Nevertheless, CO also displayed volume-dependent antifungal activity against C. albican to a considerable extent.
Recent findings shed light on the antifungal characteristics of CO that are utilized in the treatment of infectious disorders. The bioactive chemicals from CO extracts will need to be identified in further detail, as well as their pharmacological target or mechanism of action. It is now essential to conduct more clinical trials to thoroughly investigate the antimicrobial principles of CO and their numerous potential uses. It also has the potential to be employed for the preservation of processed foods. Various other therapeutic applications of CO are represented in Table 4.

Table 4.
Various therapeutic applications of CO.
4. Future Perspectives
For many centuries, CO has been utilized by humanity for diverse therapeutic applications. CO herb consist of terpenoids, steroids, phenolic compounds, carotenes, triterpenoids, essential oils, quinones, fatty acids, minerals, saponins, carbohydrates, and tocopherols, with α-cadinol (sesquiterpenoid) as a major component. Being rich in these secondary metabolites, CO has been proven to have anti-inflammatory, antidiabetic, antioxidant, anti-cancer, antibacterial, anti-ulcer, antifungal, anti-viral, anti-thrombogenic, neuroprotective, antiprotozoal, skin-protective, and antifatigue activities. Considering that CO has these multiple applications, it is crucial that extensive research on nonfloral components of the plant, such as seeds, roots, leaves, and stems, be conducted in the future. In addition to this, there is a vital need to focus on genus chemistry. Because of the limited amount of literature available, other species of CO including C. arvensis, C. tripterocarpa, C. stellata, and C. suffruticose should be explored further regarding their biochemical profiles and pharmacological properties. In the same fashion, relative studies should be conducted to understand variations in terms of the age of the plant, method of extraction, or processing method. It is anticipated that as extraction methods become more advanced, previously unidentified phytochemicals and an expansion of this plant’s pharmacological range of activity will likely be found, posing fascinating research challenges. Moreover, the research on developing novel drug delivery systems containing CO is still nascent; we anticipate that research in this area will continue. Molecular docking and molecular dynamics are two modern computational drug design techniques that hold great promise for developing novel therapeutic candidates for various ailments.
Additionally, bioinformatics technologies have opened up new avenues for finding the essential critical amino acids under almost comparable physiological settings, considerably validating the outcomes of computational methods. However, based on the chemical makeup of the medication and its target receptor, the therapeutic potential of several bioactive compounds can be investigated, saving time and money [150]. In the foreseeable future, CO-containing micro- and nano-formulations have excellent potential for treating several ailments, and the future developments and applications are assured to be astounding. Moreover, activity enhancement, combined with other available agents, offers a promising strategy that may ultimately enhance pharmacological outcomes [3].
5. Conclusions
CO species have shown tremendous health advantages from prehistoric times to the present. The present state-of-the-art CO in the health sciences realm has been rigorously examined and briefly explained in this study with insights into their molecular processes. Additionally, many CO-containing drug delivery methods and patents have been developed to improve solubility, targeting, and stability, and their active components have been considered in this analysis. As a result, it is envisioned that this review will act as a foundation for scientists, agronomists, and even small-scale herbal industries to integrate the information that is currently available on CO and realize the full pharmacological, agricultural, and industrial potential of this fascinating medicinal plant.
Author Contributions
Conceptualization, P.A. and S.T.; methodology, K.S., M.K., S.T., D.J. and S.R.; data curation, K.S., M.K., S.T., D.J. and S.R.; writing—original draft preparation, K.S., M.K., S.T., D.J. and S.R.; writing—review and editing, R.R.L., M.K.M.F., K.S., M.K., S.T., D.J., S.R., S.M., P.A., P.P.S. and J.C.; visualization, R.R.L., M.K.M.F., P.A. and S.T.; supervision, P.A., P.P.S. and J.C.; project administration, J.C.; funding acquisition, R.R.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the CNPq (grant number 312275/2021-8).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Knoess, W.; Wiesner, J. The Globalization of Traditional Medicines: Perspectives Related to the European Union Regulatory Environment. Engineering 2019, 5, 22–31. [Google Scholar] [CrossRef]
- Galucio, N.C.d.R.; Moysés, D.d.A.; Pina, J.R.S.; Marinho, P.S.B.; Gomes Júnior, P.C.; Cruz, J.N.; Vale, V.V.; Khayat, A.S.; Marinho, A.M.d.R. Antiproliferative, Genotoxic Activities and Quantification of Extracts and Cucurbitacin B Obtained from Luffa operculata (L.) Cogn. Arab. J. Chem. 2022, 15, 103589. [Google Scholar] [CrossRef]
- Chandorkar, N.; Tambe, S.; Amin, P.; Madankar, C. A Systematic and Comprehensive Review on Current Understanding of the Pharmacological Actions, Molecular Mechanisms, and Clinical Implications of the Genus Eucalyptus. Phytomed. Plus 2021, 1, 100089. [Google Scholar] [CrossRef]
- Rout, S.; Tambe, S.; Deshmukh, R.K.; Mali, S.; Cruz, J.; Srivastav, P.P.; Amin, P.D.; Gaikwad, K.K.; Andrade, E.H.D.A.; de Oliveira, M.S. Recent Trends in the Application of Essential Oils: The next Generation of Food Preservation and Food Packaging. Trends Food Sci. Technol. 2022, 129, 421–439. [Google Scholar] [CrossRef]
- Muzammil, S.; Neves Cruz, J.; Mumtaz, R.; Rasul, I.; Hayat, S.; Khan, M.A.; Khan, A.M.; Ijaz, M.U.; Lima, R.R.; Zubair, M. Effects of Drying Temperature and Solvents on In Vitro Diabetic Wound Healing Potential of Moringa Oleifera Leaf Extracts. Molecules 2023, 28, 710. [Google Scholar] [CrossRef]
- Savic Gajic, I.M.; Savic, I.M.; Skrba, M.; Dosić, A.; Vujadinovic, D. Food Additive Based on the Encapsulated Pot Marigold (Calendula officinalis L.) Flowers Extract in Calcium Alginate Microparticles. J. Food Process. Preserv. 2022, 46, e15792. [Google Scholar] [CrossRef]
- Pedram Rad, Z.; Mokhtari, J.; Abbasi, M. Preparation and Characterization of Calendula officinalis-Loaded PCL/Gum Arabic Nanocomposite Scaffolds for Wound Healing Applications. Iran. Polym. J. 2019, 28, 51–63. [Google Scholar] [CrossRef]
- Fallahi, M.; Mohammadi, A.; Miri, S.M. The Natural Variation in Six Populations of Calendula officinalis L.: A Karyotype Study. J. Genet. 2020, 6, 34–40. [Google Scholar] [CrossRef]
- Basch, E.; Bent, S.; Foppa, I.; Haskmi, S.; Kroll, D.; Mele, M.; Szapary, P.; Ulbricht, C.; Vora, M.; Yong, S. Marigold (Calendula officinalis L.): An Evidence-Based Systematic Review by the Natural Standard Research Collaboration. J. Herb. Pharm. 2006, 6, 135–159. [Google Scholar] [CrossRef]
- Gu, J.; Aidy, A.; Goorani, S. Anti-Human Lung Adenocarcinoma, Cytotoxicity, and Antioxidant Potentials of Copper Nanoparticles Green-Synthesized by Calendula officinalis. J. Exp. Nanosci. 2022, 17, 285–296. [Google Scholar] [CrossRef]
- Schneider, C. Traumeel – an Emerging Option to Nonsteroidal Anti-Inflammatory Drugs in the Management of Acute Musculoskeletal Injuries. Int. J. Gen. Med. 2011, 4, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Ashwlayan, V.D.; Kumar, A.; Verma, M.; Garg, V.K.; Gupta, S. Therapeutic Potential of Calendula officinalis. Pharm. Pharmacol. Int. J. 2018, 6, 1. [Google Scholar] [CrossRef]
- Almeida, V.M.; Dias, Ê.R.; Souza, B.C.; Cruz, J.N.; Santos, C.B.R.; Leite, F.H.A.; Queiroz, R.F.; Branco, A. Methoxylated Flavonols from Vellozia Dasypus Seub Ethyl Acetate Active Myeloperoxidase Extract: In Vitro and in Silico Assays. J. Biomol. Struct. Dyn 2022, 40, 7574–7583. [Google Scholar] [CrossRef] [PubMed]
- Arora, D.; Rani, A.; Sharma, A. A Review on Phytochemistry and Ethnopharmacological Aspects of Genus Calendula. Pharmacogn. Rev. 2013, 7, 179–187. [Google Scholar] [CrossRef]
- Rego, C.M.A.; Francisco, A.F.; Boeno, C.N.; Paloschi, M.V.; Lopes, J.A.; Silva, M.D.S.; Santana, H.M.; Serrath, S.N.; Rodrigues, J.E.; Lemos, C.T.L.; et al. Inflammasome NLRP3 Activation Induced by Convulxin, a C-Type Lectin-like Isolated from Crotalus Durissus Terrificus Snake Venom. Sci. Rep. 2022, 12, 1428. [Google Scholar] [CrossRef] [PubMed]
- Ercetin, T.; Senol, F.S.; Erdogan Orhan, I.; Toker, G. Comparative Assessment of Antioxidant and Cholinesterase Inhibitory Properties of the Marigold Extracts from Calendula arvensis L. and Calendula officinalis L. Ind. Crop. Prod. 2012, 36, 203–208. [Google Scholar] [CrossRef]
- Gonçalves, A.C.; Castro, S.; Paiva, J.; Santos, C.; Silveira, P. Taxonomic Revision of the Genus Calendula (Asteraceae) in the Iberian Peninsula and the Balearic Islands. Phytotaxa 2018, 352, 1–91. [Google Scholar] [CrossRef]
- Medical Economics Company. PDR for Herbal Medicines; Medical Economics Co.: Montvale, NJ, USA, 2000; ISBN 1563633612. [Google Scholar]
- R Silva, E.J.; Gonçalves, E.S.; Aguiar, F.; Evêncio, L.B.; A Lyra, M.M.; Cristina C Coelho, M.O.; do Carmo A Fraga, M.C.; Wanderley, A.G.; Gonçalves Wanderley, A.; Rego, M. Toxicological Studies on Hydroalcohol Extract of Calendula officinalis L. Phytother. Res. 2007, 21, 332–336. [Google Scholar] [CrossRef]
- Pedram Rad, Z.; Mokhtari, J.; Abbasi, M. Calendula officinalis Extract/PCL/Zein/Gum Arabic Nanofibrous Bio-Composite Scaffolds via Suspension, Two-Nozzle and Multilayer Electrospinning for Skin Tissue Engineering. Int. J. Biol. Macromol. 2019, 135, 530–543. [Google Scholar] [CrossRef]
- Lima, A.D.M.; Siqueira, A.S.; Möller, M.L.S.; de Souza, R.C.; Cruz, J.N.; Lima, A.R.J.; da Silva, R.C.; Aguiar, D.C.F.; Junior, J.L.D.S.G.V.; Gonçalves, E.C. In Silico Improvement of the Cyanobacterial Lectin Microvirin and Mannose Interaction. J. Biomol. Struct. Dyn. 2022, 40, 1064–1073. [Google Scholar] [CrossRef]
- Chamansara, R.; Rashidfarokhi, R.; Sakallı, E.A.; Öztinen, N.; Koşar, M. Comparison of Commercial Calendula officinalis L. Samples with Pharmacopeial Drug: Antiradical Activities and Chemical Profiles. J. Res. Pharm. 2022, 26, 809–819. [Google Scholar] [CrossRef]
- Janarny, G.; Ranaweera, K.K.D.S.; Gunathilake, K.D.P.P. Antioxidant Activities of Hydro-Methanolic Extracts of Sri Lankan Edible Flowers. Biocatal. Agric. Biotechnol. 2021, 35, 102081. [Google Scholar] [CrossRef]
- Neukirch, H.; D’Ambrosio, M.; Dalla Via, J.; Guerriero, A. Simultaneous Quantitative Determination of Eight Triterpenoid Monoesters from Flowers of 10 Varieties of Calendula officinalis L. and Characterisation of a New Triterpenoid Monoester. Phytochem. Anal. 2004, 15, 30–35. [Google Scholar] [CrossRef]
- Kishimoto, S.; Maoka, T.; Sumitomo, K.; Ohmiya, A. Analysis of Carotenoid Composition in Petals of Calendula (Calendula officinalis L.). Biosci. Biotechnol. Biochem. 2005, 69, 2122–2128. [Google Scholar] [CrossRef]
- Muley, B.P.; Khadabadi, S.S.; Banarase, N.B. Phytochemical Constituents and Pharmacological Activities of Calendula officinalis Linn (Asteraceae): A Review. Trop. J. Pharm. Res. 2009, 8, 455–465. [Google Scholar] [CrossRef]
- Olennikov, D.N.; Kashchenko, N.I.; Chirikova, N.K.; Akobirshoeva, A.; Zilfikarov, I.N.; Vennos, C. Isorhamnetin and Quercetin Derivatives as Anti-Acetylcholinesterase Principles of Marigold (Calendula officinalis) Flowers and Preparations. Int. J. Mol. Sci. 2017, 18, 1685. [Google Scholar] [CrossRef]
- Yoshikawa, M.; Murakami, T.; Kishi, A.; Kageura, T.; Matsuda, H. Medicinal Flowers. III. Marigold. (1): Hypoglycemic, Gastric Emptying Inhibitory, and Gastroprotective Principles and New Oleanane-Type Triterpene Oligoglycosides, Calendasaponins A, B, C, and D, from Egyptian Calendula officinalis. Chem. Pharm. Bull. 2001, 49, 863–870. [Google Scholar] [CrossRef]
- John, R.; Jan, N. Calendula officinalis—An Important Medicinal Plant with Potential Biological Properties. Proc. Indian Natl. Sci. Acad. 2017, 83, 769–787. [Google Scholar] [CrossRef]
- Khalil, M.Y.; Naguib, N.Y.; Sherbeny, S.E. A Comparative Study on the Productivity and Chemical Constituents of Various Sources and Species of Calendula Plants as Affected by Two Foliar Fertilizers Cultivation and Production of Medicinal and Aromatic Plants Department. J. Appl. Sci. Res. 2005, 1, 176–189. [Google Scholar]
- Paolini, J.; Barboni, T.; Desjobert, J.M.; Djabou, N.; Muselli, A.; Costa, J. Chemical Composition, Intraspecies Variation and Seasonal Variation in Essential Oils of Calendula arvensis L. Biochem. Syst. Ecol. 2010, 38, 865–874. [Google Scholar] [CrossRef]
- Bisset, N.G.; Wichtl, M. Herbal Drugs and Phytopharmaceuticals; Medpharm GmbH Scientific Publishers: Stuttgart, Germany; CRC Press: Boca Raton, FL, USA, 1994; pp. 91–95. [Google Scholar]
- Raal, A.; Orav, A.; Nesterovitsch, J.; Maidla, K. Analysis of Carotenoids, Flavonoids and Essential Oil of Calendula officinalis Cultivars Growing in Estonia. Nat. Prod. Commun. 2016, 11, 1934578X1601100831. [Google Scholar] [CrossRef]
- Sahingil, D. GC/MS-Olfactometric Characterization of the Volatile Compounds, Determination Antimicrobial and Antioxidant Activity of Essential Oil from Flowers of Calendula (Calendula officinalis L.). J. Essent. Oil Bear. Plants 2019, 22, 1571–1580. [Google Scholar] [CrossRef]
- Afolayan, A.J. Variation in the Essential Oil Composition of Calendula officinalis L. by Omobola Okoh Dissertation Submitted in Satisfaction of the Requirements for the Degree of Master of Science (Chemistry) in the Faculty of Science and Agriculture University of Fort Hare Supervisors. Ph.D. Thesis, University of Fort Hare, Alice, South Africa, 2008. [Google Scholar]
- Khalid, K.A.; EL-Ghorab, A.H. The Effect of Presowing Low Temperature on Essential Oil Content and Chemical Composition of Calendula officinalis. J. Essent. Oil Bear. Plants 2013, 9, 32–41. [Google Scholar] [CrossRef]
- Al-Rifai, A. Identification and Evaluation of In-Vitro Antioxidant Phenolic Compounds from the Calendula Tripterocarpa Rupr. S. Afr. J. Bot. 2018, 116, 238–244. [Google Scholar] [CrossRef]
- Al-Saleem, M.S.; Awaad, A.S.; Alothman, M.R.; Alqasoumi, S.I. Phytochemical Standardization and Biological Activities of Certain Desert Plants Growing in Saudi Arabia. Saudi Pharm. J. 2017, 26, 198–204. [Google Scholar] [CrossRef]
- Zitterl-Eglseer, K.; Sosa, S.; Jurenitsch, J.; Schubert-Zsilavecz, M.; della Loggia, R.; Tubaro, A.; Bertoldi, M.; Franz, C. Anti-Oedematous Activities of the Main Triterpendiol Esters of Marigold (Calendula officinalis L.). J. Ethnopharmacol. 1997, 57, 139–144. [Google Scholar] [CrossRef]
- Wojciechowski, Z.; Jelonkiewicz-Konador, A.; Tomaszewski, M.; Jankowski, J.; Kasprzyk, Z. The Structure of Glycosides of Oleanolic Acid Isolated from the Roots of Calendula officinalis. Phytochemistry 1971, 10, 1121–1124. [Google Scholar] [CrossRef]
- Vecherko, L.P.; Sviridov, A.F.; Zinkevich, E.P.; Kogan, L.M. The Structure of Calendulosides C and D from the Roots of Calendula officinalis. Chem. Nat. Compd. 1975, 11, 379–384. [Google Scholar] [CrossRef]
- Ukiya, M.; Akihisa, T.; Yasukawa, K.; Tokuda, H.; Suzuki, T.; Kimura, Y. Anti-Inflammatory, Anti-Tumor-Promoting, and Cytotoxic Activities of Constituents of Marigold (Calendula officinalis) Flowers. J. Nat. Prod. 2006, 69, 1692–1696. [Google Scholar] [CrossRef]
- Naved, T.; Ansari, S.H.; Mukhtar, H.M.; Ali, M. New Triterpenic Esters of Oleanene-Series from the Flowers of Calendula officinalis Linn. ChemInform 2005, 36, 1088–1091. [Google Scholar] [CrossRef]
- Kurkin, V.A.; Sharova, O.v. Flavonoids from Calendula officinalis Flowers. Chem. Nat. Compd. 2007, 43, 216–217. [Google Scholar] [CrossRef]
- Vidal-ollivier, E.; Balansard, G.; Faure, R.; Babadjamian, A. Revised Structures of Triterpenoid Saponins from the Flowers of Calendula officinalis. J. Nat. Prod. 1989, 52, 1156–1159. [Google Scholar] [CrossRef]
- Derkach, A.I.; Komissarenko, N.F.; Chernobai, V.T. Coumarins of the Inflorescences of Calendula officinalis and Helichrysum Arenarium. Chem. Nat. Compd. 1987, 22, 722–723. [Google Scholar] [CrossRef]
- Crabas, N.; Marongiu, B.; Piras, A.; Pivetta, T.; Porcedda, S. Extraction, Separation and Isolation of Volatiles and Dyes from Calendula officinalis L. and Aloysia triphylla (L’Her.) Britton by Supercritical CO2. J. Essent. Oil Res. 2011, 15, 272–277. [Google Scholar] [CrossRef]
- Khalid, K.; SILVA, D.A.; Teixeira, J.A. Biology of Calendula officinalis Linn.: Focus on Pharmacology, Biological Activities and Agronomic Practices. Med. Aromat. Plant Sci. Biotechnol. 2012, 6, 12–27. [Google Scholar]
- Janiszowska, W.; Michalski, W.; Kasprzyk, Z. Polyprenyl Quinones and α-Tocopherol in Calendula officinalis. Phytochemistry 1976, 15, 125–127. [Google Scholar] [CrossRef]
- Iatsyno, A.I.; Belova, L.F.; Lipkina, G.S.; Sokolov, S.I.; Trutneva, E.A. Pharmacology of Calenduloside B, a New Triterpene Glycoside from the Roots of Calendula officinalis. Farm. Toksikol. 1978, 41, 556–560. [Google Scholar]
- Goodwin, T.W. Studies in Carotenogenesis. 13. The Carotenoids of the Flower Petals of Calendula officinalis. Biochem. J. 1954, 58, 90. [Google Scholar] [CrossRef] [PubMed]
- Bakó, E.; Deli, J.; Tóth, G. HPLC Study on the Carotenoid Composition of Calendula Products. J. Biochem. Biophys. Methods 2002, 53, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Preethi, K.; Kuttan, R. Hepato and Reno Protective Action of Calendula officinalis L. Flower Extract. Indian J. Exp. Biol. 2009, 47, 163–180. [Google Scholar] [PubMed]
- Preethi, K.C.; Kuttan, G.; Kuttan, R. Antioxidant Potential of an Extract of Calendula officinalis. Flowers in Vitro. and in Vivo. Pharm. Biol. 2008, 44, 691–697. [Google Scholar] [CrossRef]
- Murillo, A.G.; Hu, S.; Fernandez, M.L. Zeaxanthin: Metabolism, Properties, and Antioxidant Protection of Eyes, Heart, Liver, and Skin. Antioxidants 2019, 8, 390. [Google Scholar] [CrossRef]
- Patil, K.; Sanjay, C.; Doggalli, N.; Devi, K.R.; Harshitha, N. A Review of Calendula officinalis Magic in Science. J. Clin. Diagn. Res. 2022, 16, ZE23–ZE27. [Google Scholar] [CrossRef]
- Selvaraj, S.; Fathima, N.N. Fenugreek Incorporated Silk Fibroin Nanofibers—A Potential Antioxidant Scaffold for Enhanced Wound Healing. ACS Appl. Mater. Interfaces 2017, 9, 5916–5926. [Google Scholar] [CrossRef] [PubMed]
- Khairnar, M.S.; Pawar, B.; Marawar, P.P.; Mani, A. Evaluation of Calendula officinalis as an Anti-Plaque and Anti-Gingivitis Agent. J. Indian Soc. Periodontol. 2013, 17, 741. [Google Scholar] [CrossRef] [PubMed]
- Saini, P.; Al-Shibani, N.; Sun, J.; Zhang, W.; Song, F.; Gregson, K.S.; Windsor, L.J. Effects of Calendula officinalis on Human Gingival Fibroblasts. Homeopathy 2012, 101, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Kumari, K. An overview on Calendula officinalis L.: (pot marigold). J. Adv. Sci. Res. 2021, 12, 13–18. [Google Scholar] [CrossRef]
- Lohani, A.; Mishra, A.K.; Verma, A. Cosmeceutical Potential of Geranium and Calendula Essential Oil: Determination of Antioxidant Activity and in Vitro Sun Protection Factor. J. Cosmet. Dermatol. 2019, 18, 550–557. [Google Scholar] [CrossRef]
- Rajwinder, K.; Singh, R.; Lalit; Jaswinder, K. Rajat Evaluation of the Antidepressant Like Activity of Ethanolic Extract of Calendula officinalis Using Rodent Models (Wistar Rat) of Depression. Curr. Psychopharmacol. 2020, 9, 58–67. [Google Scholar] [CrossRef]
- Zhang, N.; Ying, M.D.; Wu, Y.P.; Zhou, Z.H.; Ye, Z.M.; Li, H.; Lin, D.S. Hyperoside, a Flavonoid Compound, Inhibits Proliferation and Stimulates Osteogenic Differentiation of Human Osteosarcoma Cells. PLoS ONE 2014, 9, e98973. [Google Scholar] [CrossRef]
- Hsia, C.W.; Lin, K.C.; Lee, T.Y.; Hsia, C.H.; Chou, D.S.; Jayakumar, T.; Velusamy, M.; Chang, C.C.; Sheu, J.R. Esculetin, a Coumarin Derivative, Prevents Thrombosis: Inhibitory Signaling on PLCγ2–PKC–AKT Activation in Human Platelets. Int. J. Mol. Sci. 2019, 20, 2731. [Google Scholar] [CrossRef] [PubMed]
- Sharifi-Rad, J.; Cruz-Martins, N.; López-Jornet, P.; Lopez, E.P.F.; Harun, N.; Yeskaliyeva, B.; Beyatli, A.; Sytar, O.; Shaheen, S.; Sharopov, F.; et al. Natural Coumarins: Exploring the Pharmacological Complexity and Underlying Molecular Mechanisms. Oxidative Med. Cell. Longev. 2021, 2021, 6492346. [Google Scholar] [CrossRef] [PubMed]
- Butnariu, M.; Coradini, C.Z. Evaluation of Biologically Active Compounds from Calendula officinalis Flowers Using Spectrophotometry. Chem. Cent. J. 2012, 6, 35. [Google Scholar] [CrossRef]
- Naveed, M.; Hejazi, V.; Abbas, M.; Kamboh, A.A.; Khan, G.J.; Shumzaid, M.; Ahmad, F.; Babazadeh, D.; FangFang, X.; Modarresi-Ghazani, F.; et al. Chlorogenic Acid (CGA): A Pharmacological Review and Call for Further Research. Biomed. Pharmacother. 2018, 97, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Y.; Ye, Y.; Cai, T.; Li, S.; Liu, X. Anti-Fatigue Activity of the Polysaccharides Isolated from Ribes Stenocarpum Maxim. J. Funct. Foods 2022, 89, 104947. [Google Scholar] [CrossRef]
- Cetkovic, G.; Djilas, S.; Canadanovic-Brunet, J.; Tumbas, V. Thin-Layer Chromatography Analysis and Scavenging Activity of Marigold (Calendula officinalis L.) Extracts. Acta Period. Technol. 2003, 34, 93–102. [Google Scholar] [CrossRef]
- Garaiova, M.; Hua, Q.; Holic, R. Heterologous Production of Calendic Acid Naturally Found in Calendula officinalis by Recombinant Fission Yeast. J. Agric. Food Chem. 2022, 71, 8. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, R.; Noguchi, R.; Ota, T.; Abe, M.; Miyashita, K.; Kawada, T. Cytotoxic Effect of Conjugated Trienoic Fatty Acids on Mouse Tumor and Human Monocytic Leukemia Cells. Lipids 2001, 36, 477–482. [Google Scholar] [CrossRef]
- Dulf, F.V.; Pamfil, D.; Baciu, A.D.; Pintea, A. Fatty Acid Composition of Lipids in Pot Marigold (Calendula officinalis L.) Seed Genotypes. Chem. Cent. J. 2013, 7, 8. [Google Scholar] [CrossRef]
- Pizza, C.; Zhong-Liang, Z.; Tommasi, N. Plant Metabolites Triterpenoid Saponins from Calendula Arvensis. J. Nat. Prod. 1987, 50, 927–931. [Google Scholar] [CrossRef]
- Tagousop, C.N.; Tamokou, J.D.D.; Feugap, L.D.T.; Harakat, D.; Voutquenne-Nazabadioko, L.; Ngnokam, D.; Tagousop, C.N.; Tamokou, J.-D.-D.; Feugap, L.D.T.; Harakat, D.; et al. New Hemisynthetic Oleanane Saponin with Antimicrobial Activities. Adv. Biol. Chem. 2021, 11, 1–11. [Google Scholar] [CrossRef]
- Vecherko, L.P.; Sviridov, A.F.; Zinkevich, E.P.; Kogan, L.M. Structures of Calendulosides G and H from the Roots of Calendula officinalis. Chem. Nat. Compd. 1974, 10, 548–549. [Google Scholar] [CrossRef]
- Szakiel, A.; Ruszkowski, D.; Grudniak, A.; Kurek, A.; Wolska, K.I.; Doligalska, M.; Janiszowska, W. Antibacterial and Antiparasitic Activity of Oleanolic Acid and Its Glycosides Isolated from Marigold (Calendula officinalis). Planta Med. 2008, 74, 1709–1715. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, B.; Khan, R.A.; Al-Howiriny, T.A.; Al-Rehaily, A.J. Osteosaponins 1 and 2: Two New Saponin Glycosides from Osteospermum vaillantii. Nat. Prod. Res. 2010, 24, 1258–1267. [Google Scholar] [CrossRef] [PubMed]
- Vidal-Ollivier, E.; Balansard, G.; Babadjamian, A.; Faure, R.; Vincent, E.J.; Chemli, R.; Boukef, K. Two-Dimensional NMR Studies of Triterpenoid Glycosides. II)-1H NMR Assignment of Arvensoside A and B, Calenduloside C and D. Spectrosc. Lett. 1989, 22, 579–584. [Google Scholar] [CrossRef]
- Zaki, A.A.; Qiu, L. Machaerinic Acid 3-O-β-D-Glucuronopyranoside from Calendula officinalis. Nat. Prod. Res. 2019, 34, 2938–2944. [Google Scholar] [CrossRef]
- El-Najjar, N.; Gali-Muhtasib, H.; Ketola, R.A.; Vuorela, P.; Urtti, A.; Vuorela, H. The Chemical and Biological Activities of Quinones: Overview and Implications in Analytical Detection. Phytochem. Rev. 2011, 10, 353–370. [Google Scholar] [CrossRef]
- Baskaran Kaviena Pharmacological Activities of Calendula officinalis. Int. J. Sci. Res. 2017, 6, 43–47.
- Chandra, P.; Kishore, K.; Ghosh, A.K. Evaluation of Antacid Capacity and Antiulcer Activity of Calendula officinalis L. in Experimental Rats. Orient. Pharm. Exp. Med. 2015, 15, 277–285. [Google Scholar] [CrossRef]
- Abasova, R.L.; Aslanov, S.M.; Mamedova, M.É. Amino Acids of Calendula officinalis. Chem. Nat. Compd. 1995, 30, 641. [Google Scholar] [CrossRef]
- Kadowaki, W.; Miyata, R.; Fujinami, M.; Sato, Y.; Kumazawa, S. Catechol-O-Methyltransferase Inhibitors from Calendula officinalis Leaf. Molecules 2023, 28, 1333. [Google Scholar] [CrossRef] [PubMed]
- Ak, G.; Zengin, G.; Ceylan, R.; Fawzi Mahomoodally, M.; Jugreet, S.; Mollica, A.; Stefanucci, A. Chemical Composition and Biological Activities of Essential Oils from Calendula officinalis L. Flowers and Leaves. Flavour. Fragr. J. 2021, 36, 554–563. [Google Scholar] [CrossRef]
- Ak, G.; Zengin, G.; Sinan, K.I.; Mahomoodally, M.F.; Picot-Allain, M.C.N.; Cakir, O.; Bensari, S.; Yilmaz, M.A.; Gallo, M.; Montesano, D. A Comparative Bio-Evaluation and Chemical Profiles of Calendula officinalis L. Extracts Prepared via Different Extraction Techniques. Appl. Sci. 2020, 10, 5920. [Google Scholar] [CrossRef]
- Mishra, A.K.; Mishra, A.; Pragya; Chattopadhyay, P. Screening of Acute and Sub-Chronic Dermal Toxicity of Calendula officinalis L Essential Oil. Regul. Toxicol. Pharmacol. 2018, 98, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Nicolaus, C.; Junghanns, S.; Hartmann, A.; Murillo, R.; Ganzera, M.; Merfort, I. In Vitro Studies to Evaluate the Wound Healing Properties of Calendula officinalis Extracts. J. Ethnopharmacol. 2017, 196, 94–103. [Google Scholar] [CrossRef]
- Khursheed, A.; Devender, P.; Shahid, A.; Vandana Arora, S.; Alok, B.; Alam Professor, K. Evaluation of Anthelmintic Activity of Calendula officinalis Flowers Extract. J. Drug Deliv. Ther. 2021, 11, 48–50. [Google Scholar] [CrossRef]
- Slavov, A.; Ognyanov, M.; Vasileva, I. Pectic Polysaccharides Extracted from Pot Marigold (Calendula officinalis) Industrial Waste. Food Hydrocoll. 2020, 101, 105545. [Google Scholar] [CrossRef]
- Bedoya, L.C.R.; López, K.G.; Pareja, N.M. Extraction of Metabolites from Calendula officinalis and Evaluation of Their Colorant and Antibacterial Capacity. Rev. Colomb. Biotecnol. 2020, 22, 60–69. [Google Scholar] [CrossRef]
- Gazim, Z.C.; Rezende, C.M.; Fraga, S.R.; Dias Filho, B.P.; Nakamura, C.V.; Cortez, D.A.G. Analysis of the Essential Oils from Calendula officinalis Growing in Brazil Using Three Different Extraction Procedures. Rev. Bras. Ciênc. Farm. 2008, 44, 391–395. [Google Scholar] [CrossRef]
- García-Risco, M.R.; Mouhid, L.; Salas-Pérez, L.; López-Padilla, A.; Santoyo, S.; Jaime, L.; Ramírez de Molina, A.; Reglero, G.; Fornari, T. Biological Activities of Asteraceae (Achillea millefolium and Calendula officinalis) and Lamiaceae (Melissa officinalis and Origanum majorana) Plant Extracts. Plant Foods Hum. Nutr. 2017, 72, 96–102. [Google Scholar] [CrossRef]
- López-Padilla, A.; Ruiz-Rodriguez, A.; Reglero, G.; Fornari, T. Supercritical Carbon Dioxide Extraction of Calendula officinalis: Kinetic Modeling and Scaling up Study. J. Supercrit. Fluids 2017, 130, 292–300. [Google Scholar] [CrossRef]
- Jiménez-Medina, E.; Garcia-Lora, A.; Paco, L.; Algarra, I.; Collado, A.; Garrido, F. A New Extract of the Plant Calendula officinalis Produces a Dual in Vitro Effect: Cytotoxic Anti-Tumor Activity and Lymphocyte Activation. BMC Cancer 2006, 6, 119. [Google Scholar] [CrossRef] [PubMed]
- Balciunaitiene, A.; Puzeryte, V.; Radenkovs, V.; Krasnova, I.; Memvanga, P.B.; Viskelis, P.; Streimikyte, P.; Viskelis, J. Sustainabl–Green Synthesis of Silver Nanoparticles Using Aqueous Hyssopus Officinalis and Calendula officinalis Extracts and Their Antioxidant and Antibacterial Activities. Molecules 2022, 27, 7700. [Google Scholar] [CrossRef]
- Vinola, S.M.J.; Sekar, M.; Renganathan, S.K.; Dhiraviam, S. Comparative Evaluation of Calendula officinalis and 2% Chlorhexidine against Enterococcus Faecalis and Candida Albicans. J. Interdiscip. Dent. 2022, 11, 119. [Google Scholar] [CrossRef]
- Garrido-Suárez, B.B.; Garrido, G.; Menéndez, A.B.; Merino, N.; Valdés, O.; de la Paz, N.; Romero, A.; Delgado, L.; Fernández, M.D.; Piñeros, O.; et al. Topical Calendula officinalis L. Inhibits Inflammatory Pain through Antioxidant, Anti-Inflammatory and Peripheral Opioid Mechanisms. J. Integr. Med. 2022, 21, 34–46. [Google Scholar] [CrossRef]
- Deka, B.; Bhattacharjee, B.; Shakya, A.; Ikbal, A.M.A.; Goswami, C.; Sarma, S. Mechanism of Action of Wound Healing Activity of Calendula officinalis: A Comprehensive Review. Pharm. Biosci. J. 2021, 9, 28–44. [Google Scholar] [CrossRef]
- Hao, W.; Jia, Y.; Wang, C.; Wang, X. Preparation, Chemical Characterization and Determination of the Antioxidant, Cytotoxicity and Therapeutic Effects of Gold Nanoparticles Green-Synthesized by Calendula officinalis Flower Extract in Diabetes-Induced Cardiac Dysfunction in Rat. Inorg. Chem. Commun. 2022, 144, 109931. [Google Scholar] [CrossRef]
- Panahi, Y.; Sharif, M.R.; Sharif, A.; Beiraghdar, F.; Zahiri, Z.; Amirchoopani, G.; Marzony, E.T.; Sahebkar, A. A Randomized Comparative Trial on the Therapeutic Efficacy of Topical Aloe Vera and Calendula officinalis on Diaper Dermatitis in Children. Sci. World J. 2012, 2012, 810234. [Google Scholar] [CrossRef]
- Pommier, P.; Gomez, F.; Sunyach, M.P.; D’Hombres, A.; Carrie, C.; Montbarbon, X. Phase III Randomized Trial of Calendula officinalis Compared with Trolamine for the Prevention of Acute Dermatitis during Irradiation for Breast Cancer. J. Clin. Oncol. 2004, 22, 1447–1453. [Google Scholar] [CrossRef]
- Singh, M.; Bagewadi, A. Comparison of Effectiveness of Calendula officinalis Extract Gel with Lycopene Gel for Treatment of Tobacco-Induced Homogeneous Leukoplakia: A Randomized Clinical Trial. Int. J. Pharm. Investig. 2017, 7, 88. [Google Scholar] [CrossRef]
- Babaee, N.; Moslemi, D.; Khalilpour, M.; Vejdani, F.; Moghadamnia, Y.; Bijani, A.; Baradaran, M.; Kazemi, M.T.; Khalilpour, A.; Pouramir, M.; et al. Antioxidant Capacity of Calendula officinalis Flowers Extract and Prevention of Radiation Induced Oropharyngeal Mucositis in Patients with Head and Neck Cancers: A Randomized Controlled Clinical Study. DARU J. Pharm. Sci. 2013, 21, 18. [Google Scholar] [CrossRef] [PubMed]
- Giostri, G.S.; Novak, E.M.; Buzzi, M.; Guarita-Souza, L.C. Treatment of Acute Wounds in Hand with Calendula officinalis L.: A Randomized Trial. Tissue Barriers 2021, 10, 1994822. [Google Scholar] [CrossRef]
- Buzzi, M.; De Freitas, F.; De Barros Winter, M. Therapeutic Effectiveness of a Calendula officinalis Extract in Venous Leg Ulcer Healing. J. Wound Care 2016, 25, 732–739. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, C.; Di Stadio, A.; Vitale, S.; Saccone, G.; De Angelis, M.C.; Zizolfi, B.; Di Spiezio Sardo, A. Use of Calendula Ointment after Episiotomy: A Randomized Clinical Trial. J. Matern. Fetal Neonatal Med. 2020, 35, 1860–1864. [Google Scholar] [CrossRef] [PubMed]
- Saffari, E.; Mohammad-Alizadeh-Charandabi, S.; Adibpour, M.; Mirghafourvand, M.; Javadzadeh, Y. Comparing the Effects of Calendula officinalis and Clotrimazole on Vaginal Candidiasis: A Randomized Controlled Trial. Women Health 2016, 57, 1145–1160. [Google Scholar] [CrossRef]
- Pazhohideh, Z.; Mohammadi, S.; Bahrami, N.; Mojab, F.; Abedi, P.; Maraghi, E. The Effect of Calendula officinalis versus Metronidazole on Bacterial Vaginosis in Women: A Double-Blind Randomized Controlled Trial. J. Adv. Pharm. Technol. Res. 2018, 9, 19. [Google Scholar] [CrossRef]
- Fonseca, Y.M.; Catini, C.D.; Vicentini, F.T.M.C.; Nomizo, A.; Gerlach, R.F.; Fonseca, M.J.V. Protective Effect of Calendula officinalis Extract against UVB-Induced Oxidative Stress in Skin: Evaluation of Reduced Glutathione Levels and Matrix Metalloproteinase Secretion. J. Ethnopharmacol. 2010, 127, 596–601. [Google Scholar] [CrossRef]
- Hamburger, M.; Adler, S.; Baumann, D.; Förg, A.; Weinreich, B. Preparative Purification of the Major Anti-Inflammatory Triterpenoid Esters from Marigold (Calendula officinalis). Fitoterapia 2003, 74, 328–338. [Google Scholar] [CrossRef]
- Silva, D.; Ferreira, M.S.; Sousa-Lobo, J.M.; Cruz, M.T.; Almeida, I.F. Anti-Inflammatory Activity of Calendula officinalis L. Flower Extract. Cosmetics 2021, 8, 31. [Google Scholar] [CrossRef]
- Dennis Bilavendran, J.; Manikandan, A.; Thangarasu, P.; Sivakumar, K. Synthesis and Discovery of Pyrazolo-Pyridine Analogs as Inflammation Medications through pro- and Anti-Inflammatory Cytokine and COX-2 Inhibition Assessments. Bioorg. Chem. 2020, 94, 103484. [Google Scholar] [CrossRef]
- Kiaei, N.; Hajimohammadi, R.; Hosseini, M. Investigation of the Anti-Inflammatory Properties of Calendula Nanoemulsion on Skin Cells. Bioinspired Biomim. Nanobiomater. 2018, 7, 228–237. [Google Scholar] [CrossRef]
- Cook, N.C.; Samman, S. Flavonoids--Chemistry, Metabolism, Cardioprotective Effects, and Dietary Sources. J. Nutr. Biochem. 1996, 7, 66–76. [Google Scholar] [CrossRef]
- Younes, M.; Siegers, C.P. Inhibitory Action of Some Flavonoids on Enhanced Spontaneous Lipid Peroxidation Following Glutathione Depletion. Planta Med. 1981, 43, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Jacobo-Velázquez, D.A.; Cisneros-Zevallos, L. Correlations of Antioxidant Activity against Phenolic Content Revisited: A New Approach in Data Analysis for Food and Medicinal Plants. J. Food Sci. 2009, 74, R107–R113. [Google Scholar] [CrossRef] [PubMed]
- Pandey, P.; Despande, B. Antioxidant Activity in the Leaves and Petals of Calendula officinalis Linn. Asian Pac. J. Health Sci. 2022, 9, 130–132. [Google Scholar] [CrossRef]
- Elias, R.; De Méo, M.; Vidal-Ollivier, E.; Laget, M.; Balansard, G.; Dumenil, G. Antimutagenic Activity of Some Saponins Isolated from Calendula officinalis L., C. arvensis L. and Hedera helix L. Mutagenesis 1990, 5, 327–332. [Google Scholar] [CrossRef]
- Cruceriu, D.; Balacescu, O.; Rakosy, E. Calendula officinalis: Potential Roles in Cancer Treatment and Palliative Care. Integr. Cancer Ther. 2018, 17, 1068–1078. [Google Scholar] [CrossRef]
- Hernández-Rosas, N.A.; García-Zebadúa, J.C.; Hernández-Delgado, N.; Torres-Castillo, S.; Figueroa-Arredondo, P.; Mora-Escobedo, R.; Hernández-Rosas, N.A.; García-Zebadúa, J.C.; Hernández-Delgado, N.; Torres-Castillo, S.; et al. Polyphenols Profile, Antioxidant Capacity, and in Vitro Cytotoxic Effect on Human Cancer Cell Lines of a Hydro-Alcoholic Extract from Calendula officinalis L. Petals. TIP Rev. Espec. Cienc. Quím.-Biol. 2018, 21, 54–64. [Google Scholar] [CrossRef]
- Gunasekaran, S.; Arul, A.; Nayagam, J.; Natarajan, R. Wound Healing Potentials of Herbal Ointment Containing Calendula officinalis Linn. on the Alteration of Immunological Markers and Biochemical Parameters in Excision Wounded Animals. Clin. Phytosci. 2020, 6, 77. [Google Scholar] [CrossRef]
- Rathod, L.; Bhowmick, S.; Patel, P.; Sawant, K. Calendula Flower Extract Loaded Collagen Film Exhibits Superior Wound Healing Potential: Preparation, Evaluation, in-Vitro & in-Vivo Wound Healing Study. J. Drug Deliv. Sci. Technol. 2022, 72, 103363. [Google Scholar] [CrossRef]
- Jahdi, F.; Khabbaz, A.H.; Kashian, M.; Taghizadeh, M.; Haghani, H. The Impact of Calendula Ointment on Cesarean Wound Healing: A Randomized Controlled Clinical Trial. J. Fam. Med. Prim. Care 2018, 7, 893. [Google Scholar] [CrossRef]
- Bosley, R.; Leithauser, L.; Turner, M.; Gloster, H.M. The Efficacy of Second-Intention Healing in the Management of Defects on the Dorsal Surface of the Hands and Fingers after Mohs Micrographic Surgery. Dermatol. Surg. 2012, 38, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Pawan, V.; Rajinder, R.; Maninder, S.; Wazir, V.S. Kumar Pawan Attenuating Potential of Calendula officinalis on Biochemical and Antioxidant Parameters in Hepatotoxic Rats. Indian J Physiol. Pharmacol. 2017, 61, 398–410. [Google Scholar]
- Băieş, M.H.; Gherman, C.; Boros, Z.; Olah, D.; Vlase, A.M.; Cozma-Petruț, A.; Györke, A.; Miere, D.; Vlase, L.; Crișan, G.; et al. The Effects of Allium sativum L., Artemisia absinthium L., Cucurbita pepo L., Coriandrum sativum L., Satureja hortensis L. and Calendula officinalis L. on the Embryogenesis of Ascaris Suum Eggs during an In Vitro Experimental Study. Pathogens 2022, 11, 1065. [Google Scholar] [CrossRef] [PubMed]
- Boyko, O.; Brygadyrenko, V. Nematicidal Activity of Essential Oils of Medicinal Plants. Folia Oecologica 2021, 48, 42–48. [Google Scholar] [CrossRef]
- Rafał, I.G.; Króliczewski, B.J.; Górniak, I.; Bartoszewski, R.; Króliczewski, Á.J. Comprehensive Review of Antimicrobial Activities of Plant Flavonoids. Phytochem. Rev. 2018, 18, 241–272. [Google Scholar] [CrossRef]
- Manandhar, S.; Luitel, S.; Dahal, R.K. In Vitro Antimicrobial Activity of Some Medicinal Plants against Human Pathogenic Bacteria. J. Trop. Med. 2019, 2019, 1895340. [Google Scholar] [CrossRef]
- Djeussi, D.E.; Noumedem, J.A.K.; Seukep, J.A.; Fankam, A.G.; Voukeng, I.K.; Tankeo, S.B.; Nkuete, A.H.L.; Kuete, V. Antibacterial Activities of Selected Edible Plants Extracts against Multidrug-Resistant Gram-Negative Bacteria. BMC Complement. Altern. Med. 2013, 13, 164. [Google Scholar] [CrossRef]
- Duraipandiyan, V.; Ayyanar, M.; Ignacimuthu, S. Antimicrobial Activity of Some Ethnomedicinal Plants Used by Paliyar Tribe from Tamil Nadu, India. BMC Complement. Altern. Med. 2006, 6, 35. [Google Scholar] [CrossRef]
- Tambe, S.M.; Mali, S.; Amin, P.D.; Oliveira, M. Neuroprotective Potential of Cannabidiol: Molecular Mechanisms and Clinical Implications. J. Integr. Med. 2023, 3, 1–9. [Google Scholar] [CrossRef]
- Karnwal, A. In Vitro Antibacterial Activity of Hibiscus Rosa Sinensis, Chrysanthemum Indicum, and Calendula officinalis Flower Extracts against Gram Negative and Gram Positive Food Poisoning Bacteria. Adv. Tradit. Med. 2022, 22, 607–619. [Google Scholar] [CrossRef]
- Yalgi, V.S.; Bhat, K.G. Compare and Evaluate the Antibacterial Efficacy of Sodium Hypochlorite and Calendula officinalis against Streptococcus Mutans as a Root Canal Irrigating Solution: An in Vivo Study. J. Int. Oral. Health 2020, 12, 74. [Google Scholar] [CrossRef]
- Darekar, D.; Hate, M. Phytochemical Screening of Calendula officinalis (Linn.) Using Gas-Chromatography-Mass Spectroscopy with Potential Antibacterial Activity. J. Sci. Res. 2021, 65, 131–134. [Google Scholar] [CrossRef]
- Zulfiqer Shahen, M.; Mahmud, S.; Nahid Sohana, S.; Hasan Rony, M.; Abu Sayeed Imran, M.; Abdullah Al Maruf, M.; Afzal Ahmed Azim, M.; Monirul Islam, M.; Rokibul Islam, M.; Ekhlas Uddin, M.; et al. Effect of Antibiotic Susceptibility and Inhibitory Activity for the Control of Growth and Survival of Microorganisms of Extracts of Calendula officinalis. Eur. J. Med. Health Sci. 2019, 1, 1–9. [Google Scholar] [CrossRef]
- Removing Obstacles to Healthy Development: Report on Infectious Diseases. Available online: https://apps.who.int/iris/handle/10665/65847 (accessed on 25 March 2023).
- Samra, R.M.; Maatooq, G.T.; Zaki, A.A. A New Antiprotozoal Compound from Calendula officinalis. Nat. Prod. Res. 2022, 36, 5747–5752. [Google Scholar] [CrossRef] [PubMed]
- Webster, D.; Taschereau, P.; Belland, R.J.; Sand, C.; Rennie, R.P. Antifungal Activity of Medicinal Plant Extracts; Preliminary Screening Studies. J. Ethnopharmacol. 2008, 115, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Martínez, L.G. Preclinical Vascular Activity of an Aqueous Extract from Flowers of Calendula officinalis. J. Pharm. Pharmacol. 2020, 8, 339–344. [Google Scholar] [CrossRef]
- Athaiban, M.A. Issue 6|Page 22–28 Maha A. Athaiban, Effect of Calendula officinalis Extract Against Streptozotocin Induced Diabetes in Male Rats ISSN (Online) 2249-6084 (Print) 2250-1029 EIJPPR. Int. J. Pharm. Phytopharm. Res. 2018, 8, 22–28. [Google Scholar]
- Ebrahimi, E.; Shirali, S.; Talaei, R. The Protective Effect of Marigold Hydroalcoholic Extract in STZ-Induced Diabetic Rats: Evaluation of Cardiac and Pancreatic Biomarkers in the Serum. J. Bot. 2016, 2016, 9803928. [Google Scholar] [CrossRef]
- Gharanjik, F.; Shojaeifard, M.B.; Karbalaei, N.; Nemati, M. The Effect of Hydroalcoholic Calendula officinalis Extract on Androgen-Induced Polycystic Ovary Syndrome Model in Female Rat. Biomed Res. Int. 2022, 2022, 7402598. [Google Scholar] [CrossRef]
- Pandey, P.; Despande, B.; Sarkar, A.K. A Pharmacological Study on the Effect of Calendula officinalis Leaf Extract on Excision Wound Healing in Swiss Albino Mice. Asian Pac. J. Health Sci. 2022, 9, 109–113. [Google Scholar] [CrossRef]
- Ghodoosi, S.; Namazi, Z.; Mashhadiabbas, F.; Bakhtiari, S.; Afraz, E.S. Efficacy of 10% Calendula officinalis Extract Gel for Oral Wound Healing in Rats. J. Biol. Stud. 2022, 5, 52–63. [Google Scholar]
- Rathod, L.; Bhowmick, S.; Patel, P.; Sawant, K. Calendula Flower Extract Loaded PVA Hydrogel Sheet for Wound Management: Optimization, Characterization and in-Vivo Study. J. Drug Deliv. Sci. Technol. 2022, 68, 103035. [Google Scholar] [CrossRef]
- Lohani, A.; Morganti, P. Age-Defying and Photoprotective Potential of Geranium/Calendula Essential Oil Encapsulated Vesicular Cream on Biochemical Parameters against UVB Radiation Induced Skin Aging in Rat. Cosmetics 2022, 9, 43. [Google Scholar] [CrossRef]
- Ali, E.M.; Abd El-Moaty, H. Antifungal Activity of Achillea santolina L. and Calendula officinalis L. Essential Oils and Their Constituents Against Fungal Infection of Liver as Complication of Cyclophosphamide Therapy. J. Essent. Oil Bear. Plants 2017, 20, 1030–1043. [Google Scholar] [CrossRef]
- Mali, S.N.; Tambe, S.; Pratap, A.P.; Cruz, J.N. Molecular Modeling Approaches to Investigate Essential Oils (Volatile compounds) Interacting with Molecular Targets. In Essential Oils: Applications and Trends in Food Science and Technology; Springer: Cham, Switzerland, 2022; pp. 417–442. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).