Chemical Composition and Antimicrobial Potential of a Plant-Based Substance for the Treatment of Seborrheic Dermatitis
Abstract
1. Introduction
2. Results and Discussion
2.1. GC/MS Analysis of TTO and the Plant-Based Substance
2.2. Antimicrobial Activity
2.3. Antifungal Activity against M. furfur
3. Materials and Methods
3.1. Chemicals and Plant Materials
3.2. Analysis of the Chemical Composition of the Substance
3.3. Antimicrobial Activity
3.3.1. Test Microorganisms and Growth Conditions
3.3.2. Antimicrobial Screening by Determining the MICs for the Substances
3.4. Antifungal Activity
3.4.1. Test Microorganisms and Growth Conditions
3.4.2. Antifungal Screening by Determining the MICs of Substances
3.4.3. Antifungal Screening by Determining the Log10CFU Reduction
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gupta, A.K.; Madzia, S.E.; Batra, R. Etiology and management of Seborrheic dermatitis. Dermatology 2004, 208, 89–93. [Google Scholar] [CrossRef]
- Borda, L.J.; Wikramanayake, T.C. Seborrheic Dermatitis and Dandruff: A Comprehensive Review. J. Clin. Investig. Derm. 2015, 3, 1–22. [Google Scholar]
- Manuel, F.; Ranganathan, S. A new postulate on two stages of dandruff: A clinical perspective. Int. J. Trichol. 2011, 3, 3–6. [Google Scholar]
- Massiot, P.; Clavaud, C.; Thomas, M.; Ott, A.; Guéniche, A.; Panhard, S.; Muller, B.; Michelin, C.; Kerob, D.; Bouloc, A.; et al. Continuous clinical improvement of mild-to-moderate seborrheic dermatitis and rebalancing of the scalp microbiome using a selenium disulfide–based shampoo after an initial treatment with ketoconazole. J. Cosmet. Dermatol. 2022, 21, 2215–2225. [Google Scholar] [CrossRef]
- Park, M.; Cho, Y.-J.; Lee, Y.W.; Jung, W.H. Genomic Multiplication and Drug Efflux Influence Ketoconazole Resistance in Malassezia restricta. Front. Cell. Infect. Microbiol 2020, 10, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Naldi, L.; Rebora, A. Clinical practice. Seborrheic dermatitis. N. Engl. J. Med. 2009, 360, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Okokon, E.O.; Verbeek, J.H.; Ruotsalainen, J.H.; Ojo, A.O.; Bakhoya, V.N. Topical antifungals for seborrhoeic dermatitis. Cochrane Database Syst. Rev. 2015, 5, 1–234. [Google Scholar]
- Del Rosso, J.Q. Adult seborrheic dermatitis: A status report on practical topical management. J. Clin. Aesthet. Derm. 2011, 4, 32–38. [Google Scholar]
- Serwecińska, L. Antimicrobials and antibiotic-resistant bacteria: A risk to the environment and to public health. Water 2020, 12, 3313. [Google Scholar] [CrossRef]
- Samarei, R.; Gharebaghi, N.; Zayer, S. Evaluation of 30 cases of mucormycosis at a university hospital in Iran. Mycoses 2017, 1, 1–7. [Google Scholar] [CrossRef]
- Leong, C.; Kit, J.C.H.; Lee, S.M.; Lam, Y.I.; Goh, J.P.Z.; Ianiri, G.; Dawson, T.L., Jr. Azole resistance mechanisms in pathogenic M. furfur. Antimicrob. Agents Chemother. 2021, 65, e01975. [Google Scholar] [CrossRef] [PubMed]
- Ellah, N.H.A.; Abdel-Aleem, J.A.; Abdo, M.N.; Abou-Ghadir, O.F.; Zahran, K.M.; Hetta, H.F. Efficacy of ketoconazole gel-flakes in the treatment of vaginal candidiasis: Formulation, in vitro and clinical evaluation. Int. J. Pharm. 2019, 567, 1–9. [Google Scholar]
- Yap, P.S.X.; Yang, S.K.; Lai, K.S.; Lim, S.H.E. Essential Oils: The Ultimate Solution to Antimicrobial Resistance in Escherichia coli? In Recent Advances on Physiology, Pathogenesis and Biotechnological Applications, 1st ed.; Samie, A., Ed.; IntechOpen: London, UK, 2017; Volume 15, pp. 299–313. [Google Scholar]
- Saxena, R.; Mittal, P.; Clavaud, C.; Dhakan, D.B.; Hegde, P.; Veeranagaiah, M.M.; Saha, S.; Souverain, L.; Roy, N.; Breton, L.; et al. Comparison of Healthy and Dandruff Scalp Microbiome Reveals the Role of Commensals in Scalp Health. Front. Cell. Infect. Microbiol. 2018, 8, 346. [Google Scholar] [CrossRef] [PubMed]
- Grimshaw, S.G.; Smith, A.M.; Arnold, D.S.; Xu, E.; Hoptroff, M.; Murphy, B. The diversity and abundance of fungi and bacteria on the healthy and dandruff affected human scalp. PLoS ONE 2019, 14, e0225796. [Google Scholar] [CrossRef] [PubMed]
- Somerville, D.A. The normal flora of the skin in different age groups. Br. J. Derm. 1969, 81, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Chow, P.S.; Yagnik, C.K. Developing Eco-Friendly Skin Care Formulations with Microemulsions of Essential Oil. Cosmetics 2022, 9, 30. [Google Scholar] [CrossRef]
- Jain, S.; Arora, P.; Nainwal, L.M. Essential Oils as Potential Source of Anti-dandruff Agents: A Review. Comb. Chem. High Throughput Screen 2022, 25, 1411–1426. [Google Scholar]
- Caldefie-Chezet, F.; Guerry, M.; Chalchat, J.C.; Fusillier, C.; Vasson, M.P.; Guillot, J. Anti-inflammatory effects of Melaleuca alternifolia essential oil o human polymorphonuclear neutrophils ad monocytes. Free Radic. Res. 2004, 38, 805–811. [Google Scholar] [CrossRef]
- Miguel, M.G. Antioxidant and anti-inflammatory activities of essential oils: A short review. Molecules 2010, 15, 9252–9287. [Google Scholar] [CrossRef]
- Sharifi-Rad, J.; Sureda, A.; Tenore, G.C.; Daglia, M.; Sharifi-Rad, M.; Valussi, M.; Tundis, R.; Sharifi-Rad, M.; Loizzo, M.R.; Ademiluyi, A.O.; et al. Biological activities of essential oils: From plant chemoecology to traditional healing systems. Molecules 2017, 22, 70. [Google Scholar] [CrossRef]
- Carson, C.F.; Mee, B.J.; Riley, T.V. Mechanism of action of Melaleuca alternifolia (tea tree) oil on Staphylococcus aureus determined by time-kill, lysis, leakage, and salt tolerance assays and electron microscopy. Antimicrob. Agents Chemother. 2002, 46, 1914–1920. [Google Scholar] [CrossRef]
- Banes-Marshall, L.; Cawley, P.; Phillips, C.A. In vitro activity of Melaleuca alternifolia (tea tree) oil against bacterial and Candida spp. isolates from clinical specimens. Br. J. Biomed. Sci. 2001, 58, 139–145. [Google Scholar]
- Hammer, K.A.; Carson, C.F.; Riley, T.V. Susceptibility of transient and commensal skin flora to the essential oil of Melaleuca alternifolia (tea tree oil). Am. J. Infect. Control 1996, 24, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Carson, C.F.; Riley, T.V. Antimicrobial activity of the essential oil of Melaleuca alternifolia. Lett. Appl. Microbiol. 1993, 16, 49–55. [Google Scholar] [CrossRef]
- Nenoff, P.; Haustein, U.F.; Brandt, W. Antifungal activity of the essential oil of melaleuca alternifolia (tea tree oil) against pathogenic fungi in vitro. Ski. Pharm. Physiol 1996, 9, 388–394. [Google Scholar] [CrossRef] [PubMed]
- Mikus, J.; Harkenthal, M.; Steverding, D.; Reichling, J. In vitro effect of essential oils and isolated mono- and sesquiterpenes on Leishmania major and Trypanosoma brucei. Planta Med. 2000, 66, 366–368. [Google Scholar] [CrossRef]
- Hart, P.H.; Brand, C.; Carson, C.F.; Riley, T.V.; Prager, R.H.; Finlay-Jones, J.J. Terpinen-4-ol, the main component of the essential oil of Melaleuca alternifolia (tea tree oil), suppresses inflammatory mediator production by activated human monocytes. Inflamm. Res. 2000, 49, 619–626. [Google Scholar] [CrossRef]
- Koh, K.J.; Pearce, A.L.; Marshman, G.; Finlay-Jones, J.J.; Hart, P.H. Tea tree oil reduces histamine-induced skin inflammation. Br. J. Derm. 2002, 147, 1212–1217. [Google Scholar] [CrossRef]
- Pearce, A.L.; Finlay-Jones, J.J.; Hart, P.H. Reduction of nickel-induced contact hypersensitivity reactions by topical tea tree oil in humans. Inflamm. Res. 2005, 54, 22–30. [Google Scholar] [CrossRef]
- Mączka, W.; Duda-Madej, A.; Górny, A.; Grabarczyk, M.; Wińska, K. Can eucalyptol replace antibiotics? Molecules 2021, 26, 4933–4949. [Google Scholar] [CrossRef]
- Juergens, L.J.; Worth, H.; Juergens, U.R. New Perspectives for Mucolytic, Anti-inflammatory and Adjunctive Therapy with 1,8-Cineole in COPD and Asthma: Review on the New Therapeutic Approach. Adv. Ther. 2020, 37, 1737–1753. [Google Scholar] [CrossRef] [PubMed]
- Yadav, N.; Chandra, H. Suppression of inflammatory and infection responses in lung macrophages by eucalyptus oil and its constituent 1,8-cineole: Role of pattern recognition receptors TREM-1 and NLRP3, the MAP kinase regulator MKP-1, and NFκB. PLoS ONE 2017, 12, e0188232. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Li, Z.W.; Yin, Z.Q.; Wei, Q.; Jia, R.Y.; Zhou, L.J.; Xu, J.; Song, X.; Zhou, Y.; Du, Y.H. Antibacterial activity of leaf essential oil and its constituents from Cinnamomum longepaniculatum. Int. J. Clin. Exp. Med. 2014, 7, 1721–1727. [Google Scholar] [PubMed]
- Simsek, M.; Duman, R. Investigation of effect of 1,8-cineole on antimicrobial activity of chlorhexidine gluconate. Pharmacogn. Res. 2017, 9, 234–237. [Google Scholar] [CrossRef]
- Kamatou, G.P.P.; Viljoen, A.M. A review of the application and pharmacological properties of α-bisabolol and α-bisabolol-rich oils. J. Am. Oil Chem. Soc. 2010, 87, 1–7. [Google Scholar] [CrossRef]
- Carson, C.F.; Hammer, K.A.; Riley, T.V. Melaleuca alternifolia (tea tree) oil: A review of antimicrobial and other medicinal properties. Clin. Microbiol. Rev. 2006, 19, 50–62. [Google Scholar] [CrossRef]
- De Lucca, A.J.; Pauli, A.; Schilcher, H.; Sien, T.; Bhatnagar, D.; Walsh, T.J. Fungicidal and Bactericidal Properties of Bisabolol and Dragosantol. J. Essent. Oil Res. 2011, 23, 47–54. [Google Scholar] [CrossRef]
- Dhifi, W.; Bellili, S.; Jazi, S.; Bahloul, N.; Mnif, W. Essential Oils’ Chemical Characterization and Investigation of Some Biological Activities: A Critical Review. Medicines 2016, 3, 25. [Google Scholar] [CrossRef]
- Turek, C.; Stintzing, F.C. Stability of Essential Oils: A Review. Compr. Rev. Food Sci. Food Saf. 2013, 12, 40–53. [Google Scholar] [CrossRef]
- Marriott, P.J.; Shellie, R.; Cornwell, C. Gas chromatographic technologies for the analysis of essential oils. J. Chromatogr. A 2001, 936, 1–22. [Google Scholar] [CrossRef]
- Adams, R.P. Identification of Essential Oil Components by Gas Chromatography/Mass Spectroscopy, 4th ed.; Allured Publishing Corporation: Carol Stream, IL, USA, 2007; pp. 1–804. [Google Scholar]
- Brophy, J.J.; Davies, N.W.; Southwell, I.A.; Stiff, I.A.; Williams, L.R. Gas chromatographic quality control for oil of Melaleuca terpinen-4-ol type (Australian tea tree). J. Agric. Food Chem. 1989, 37, 1330–1335. [Google Scholar] [CrossRef]
- Kumari, K.M.U.; Yadav, N.P.; Luqman, S. Promising Essential Oils/Plant Extracts in the Prevention and Treatment of Dandruff Pathogenesis. Curr. Top. Med. Chem. 2022, 22, 1104–1133. [Google Scholar] [PubMed]
- Ergin, A.; Arikan, S. Comparison of microdilution and disc diffusion methods in assessing the in vitro activity of fluconazole and Melaleuca alternifolia (tea tree) oil against vaginal Candida isolates. J. Chemother. 2002, 14, 465–472. [Google Scholar] [CrossRef]
- Mondello, F.; De Bernardis, F.; Girolamo, A.; Cassone, A.; Salvatore, G. In vivo activity of terpinen-4-ol, the main bioactive component of Melaleuca alternifolia Cheel (tea tree) oil against azole-susceptible and -resistant human pathogenic Candida species. BMC Infect. Dis. 2006, 6, 158. [Google Scholar] [CrossRef] [PubMed]
- Hendry, E.R.; Worthington, T.; Conway, B.R.; Lambert, P.A. Antimicrobial efficacy of eucalyptus oil and 1,8-cineole alone and in combination with chlorhexidine digluconate against microorganisms grown in planktonic and biofilm cultures. J. Antimicrob. Chemother. 2009, 64, 1219–1225. [Google Scholar] [CrossRef]
- Sikkema, J.; de Bont, J.A.M.; Poolman, B. Mechanisms of membrane toxicity of hydrocarbons. Microbiol. Rev. 1995, 59, 201–222. [Google Scholar] [CrossRef]
- Zengin, H.; Baysal, A.H. Antibacterial and antioxidant activity of essential oil terpenes against pathogenic and spoilage-forming bacteria and cell structure-activity relationships evaluated by SEM microscopy. Molecules 2014, 19, 17773–17798. [Google Scholar] [CrossRef]
- Merghni, A.; Noumi, E.; Hadded, O.; Dridi, N.; Panwar, H.; Ceylan, O.; Mastouri, M.; Snoussi, M. Assessment of the antibiofilm and antiquorum sensing activities of Eucalyptus globulus essential oil and its main component 1,8-cineole against methicillin-resistant Staphylococcus aureus strains. Microb. Pathog. 2018, 118, 74–80. [Google Scholar] [CrossRef]
- Draelos, Z.D. A Pilot Study Investigating the Efficacy of Botanical Anti-Inflammatory Agents in an OTC Eczema Therapy. J. Cosmet. Derm. 2016, 15, 117–119. [Google Scholar] [CrossRef]
- Leite, G.O.; Leite, L.H.I.; Sampaio, R.S.; Araruna, M.K.A.; Menezes, I.R.A.; Costa, J.G.M.C.; Campos, A.R. (-)-α-Bisabolol At-tenuates Visceral Nociception and Inflammation in Mice. Fitoterapia 2011, 82, 208–211. [Google Scholar] [CrossRef]
- Femenıa-Font, A.; Balaguer-Fernandez, C.; Merino, V.; Rodilla, V.; López-Castellano, A. Effect of chemical enhancers on the in vitro percutaneous absorption of sumatriptan succinate. Eur. J. Pharm. Biopharm. 2005, 61, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Romagnoli, C.; Baldisserotto, A.; Malisardi, G.; Vicentini, C.B.; Mares, D.; Andreotti, E.; Vertuani, S.; Manfredini, S. A Multi-Target Approach Toward the Development of Novel Candidates for Antidermatophytic Activity: Ultra-structural Evidence on α-Bisabolol-Treated Microsporum Gypseum. Molecules 2015, 20, 11765–11776. [Google Scholar] [CrossRef] [PubMed]
- de Groot, A.C.; Schmidt, E. Tea tree oil: Contact allergy and chemical composition. Contact Dermat. 2016, 75, 129–143. [Google Scholar] [CrossRef] [PubMed]
- Dakah, A.M.M. Antileishmanial and Antibacterial Activity of Essential Oils of Medicinal Plant Achillea santolina L. OnLine J. Biol. Sci. 2019, 19, 69–76. [Google Scholar] [CrossRef]
- Shameem, S.K.; Khaliquz, Z.K.; Waza, A.A.; Shah, A.H. Bioactivities and chemoprofiling comparisons of Chenopodium ambrosioides L and Chenopodium botrys L. growing in Kashmir India. Asian J. Pharm. Clin. Res. 2019, 12, 124. [Google Scholar] [CrossRef]
- Mulyaningsih, S.; Sporer, F.; Zimmermann, S.; Reichling, J.; Wink, M. Synergistic proper-ties of the terpenoids aromadendrene and 1,8-cineole from the essential oil of eucalyptus globulus against antibiotic-susceptible and antibiotic-resistant pathogens. Phytomedicine 2010, 17, 1061–1066. [Google Scholar] [CrossRef]
- Sikkema, J.; De Bont, J.A.M.; Poolman, B. Interactions of cyclic hydrocarbons with bio-logical membranes. J. Biol. Chem. 1994, 269, 8022–8028. [Google Scholar] [CrossRef]
- Wink, M. Evolutionary Advantage and Molecular Modes of Action of Multi-Component Mixtures Used in Phytomedicine. Curr. Drug Metab. 2008, 9, 996–1009. [Google Scholar] [CrossRef]
- Burt, S. Essential oils: Their antibacterial properties and potential applications in foods-A review. Int. J. Food Microbiol. 2004, 94, 223–253. [Google Scholar] [CrossRef]
- Lee, C.J.; Chen, L.W.; Chen, L.G.; Chang, T.L.; Huang, C.W.; Huang, M.C.; Wang, C.C. Correlations of the components of tea tree oil with its antibacterial effects and skin irritation. J. Food Drug Anal. 2013, 21, 169–176. [Google Scholar] [CrossRef]
- Połeć, K.; Wójcik, A.; Flasiński, M.; Wydro, P.; Broniatowski, M.; Hąc-Wydro, K. The influence of terpinen-4-ol and eucalyptol-The essential oil components-on fungi and plant sterol monolayers. Biochim. Biophys. Acta Biomembr. 2019, 1861, 1093–1102. [Google Scholar] [CrossRef]
- Sanguinetti, M.; Posteraro, B.; Fiori, B.; Ranno, S.; Torelli, R.; Fadda, G. Mechanisms of azole resistance in clinical isolates of Candida glabrata collected during a hospital survey of antifungal resistance. Antimicrob. Agents Chemother. 2005, 49, 668–679. [Google Scholar] [CrossRef] [PubMed]
- Cox, S.D.; Mann, C.M.; Markham, J.L.; Gustafson, J.E.; Warmington, J.R.; Wyllie, S.G. Determining the antimicrobial actions of tea tree oil. Molecules 2001, 6, 87–91. [Google Scholar] [CrossRef]
- Chao, S.; Young, G.; Oberg, C.; Nakaoka, K. Inhibition of methicillin-resistant Staphylococcus aureus (MRSA) by essential oils. Flavour Fragr J 2008, 23, 444–449. [Google Scholar] [CrossRef]
- Kon, K.V.; Rai, M.K. Plant essential oils and their constituents in coping with multidrug-resistant bacteria. Expert Rev Anti Infect 2012, 10, 775–790. [Google Scholar] [CrossRef] [PubMed]
- Woo, K.J.; Hye, C.K.; Ki, W.K.; Shin, S.; So, H.K.; Yong, H.P. Antibacterial activity and mechanism of action of the silver ion in Staphylococcus aureus and Escherichia coli. Appl. Env. Microbiol. 2008, 74, 2171–2178. [Google Scholar]
- Prabuseenivasan, S.; Jayakumar, M.; Ignacimuthu, S. In vitro antibacterial activity of some plant essential oils. BMC Complement Altern. Med. 2006, 6, 39–47. [Google Scholar] [CrossRef] [PubMed]
- NIST Chemistry WebBook: NIST Standard Reference Database Number 69. Available online: http://webbook.nist.gov/chemistry/ (accessed on 15 December 2022).
- Sparkman, D.O. Identification of essential oil components by gas chromatography/quadrupole mass spectroscopy Robert, P. Adams. J. Am. Soc. Mass Spectrom. 2005, 16, 1902–1903. [Google Scholar] [CrossRef]
- Babushok, V.I.; Linstrom, P.J.; Zenkevich, I.G. Retention indices for frequently reported compounds of plant essential oils. J. Phys. Chem. Ref. Data 2011, 40, 043101. [Google Scholar] [CrossRef]
- Linstrom, P.J.; Mallard, W.G. The NIST Chemistry WebBook: A Chemical Data Re-source on the Internet. J. Chem. Eng. Data 2001, 46, 1059–1063. [Google Scholar] [CrossRef]
- Hoskovec, M.; Grygarová, D.; Cvacka, J.; Streinz, L.; Zima, J.; Verevkin, S.P.; Koutek, B. Determining the vapour pressures of plant volatiles from gas chromatographic retention data. J. Chromatogr. A 2005, 1083, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Adamczak, A.; Ozarowski, M.; Karpinski, T.M. Curcumin, a Natural Antimicrobial Agent with Strain-Specific Activity. Pharmaceuticals 2020, 13, 153–165. [Google Scholar] [CrossRef]
- CLSI. Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts, 2nd ed.; Clinical and Laboratory Standards Institute: Berwyn, PA, USA, 2002. [Google Scholar]
- Leclercq, R.; Cantón, R.; Brown, D.F.J.; Giske, C.G.; Heisig, P.; Macgowan, A.P.; Mouton, J.W.; Nordmann, P.; Rodloff, A.C.; Rossolini, G.M. EUCAST expert rules in antimicrobial susceptibility testing. Clin. Microbiol. Infect. 2013, 19, 141–160. [Google Scholar] [CrossRef] [PubMed]
- Javadpour, M.M.; Juban, M.M.; Lo, W.C.J.; Bishop, S.M.; Alberty, J.B.; Cowell, S.M.; Becker, C.L.; McLaughlin, M.L. De novo antimicrobial peptides with low mammalian cell toxicity. J. Med. Chem. 1996, 39, 3107–3113. [Google Scholar] [CrossRef] [PubMed]
- Aruna, V.; Soundharya, R.; Amruthavalli, G.V.; Gayathri, R. Competitive Binding of AD Agents to Scalp from Shampoo–A Novel Method for Evaluation. J. Cosmetol. 2019, 3, 1–6. [Google Scholar]
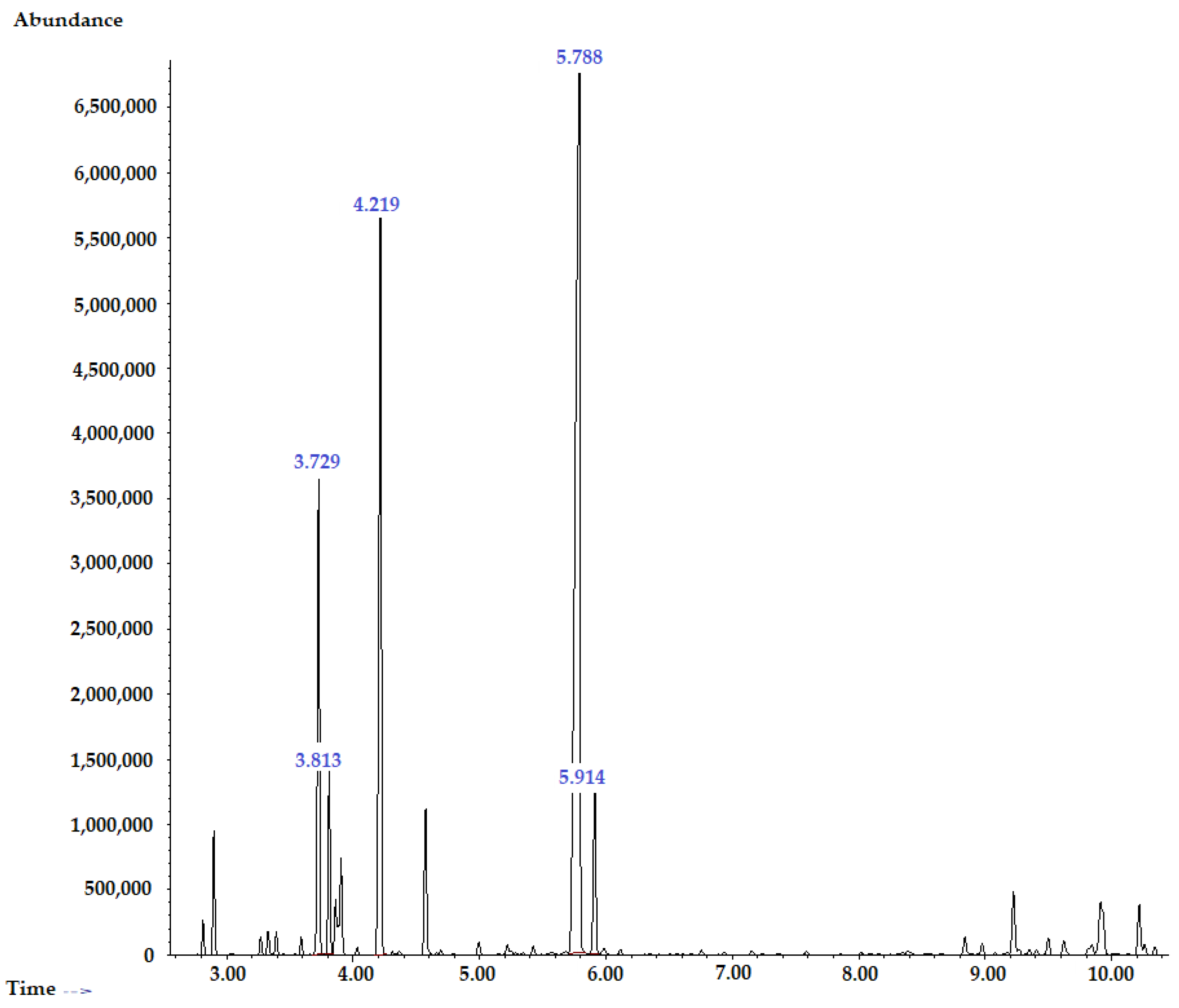




| No. | Compound a | MW b | Class of Terpenes | Retention Time | RI c |
|---|---|---|---|---|---|
| 1 | α-Thujene | 136.23 | Bicyclic monoterpene | 2.816 | 924 |
| 2 | α-Pinene | 136.23 | Bicyclic monoterpene | 2.901 | 932 |
| 3 | β-Pinene | 136.23 | Bicyclic monoterpene | 3.331 | 974 |
| 4 | Myrcene | 136.23 | Acyclic monoterpene | 3.394 | 988 |
| 5 | α-Terpinene | 136.23 | Cyclic monoterpene | 3.729 | 1014 |
| 6 | o-Cymene | 134.22 | Aromatic monoterpene | 3.813 | 1022 |
| 7 | D-Limonene | 136.23 | Cyclic monoterpene | 3.864 | 1024 |
| 8 | 1,8-Cineole (eucalyptol) | 154.25 | Bicyclic epoxy monoterpene | 3.907 | 1026 |
| 9 | γ-Terpinene | 136.23 | Cyclic monoterpene | 4.219 | 1054 |
| 10 | α-Terpinolene | 136.23 | Cyclic monoterpene | 4.575 | 1086 |
| 11 | Terpinen-4-ol | 154.25 | Cyclic monoterpene | 5.788 | 1174 |
| 12 | α-Terpineol | 154.25 | Cyclic monoterpene | 5.914 | 1186 |
| 13 | Aromadendrene | 204.35 | Sesquiterpene | 9.227 | 1439 |
| 14 | Viridiflorene (ledene) | 204.35 | Sesquiterpene | 9.914 | 1496 |
| 15 | δ-Cadinene | 204.35 | Sesquiterpene | 10.219 | 1522 |
| No. | Compound a | MW b | Class of Terpenes | Retention Time (Min) c | RI d | Relative Content, % |
|---|---|---|---|---|---|---|
| 1 | α-Pinene | 136.23 | Bicyclic monoterpene | 2.521 | 932 | 1.30% |
| 2 | Sabinene | 136.23 | Bicyclic monoterpene | 2.850 | 969 | 0.20% |
| 3 | β-Pinene | 136.23 | Bicyclic monoterpene | 2.901 | 974 | 0.26% |
| 4 | α-Phellandrene | 136.23 | Cyclic monoterpene | 2.448 | 1002 | 0.32% |
| 5 | α-Terpinene | 136.23 | Cyclic monoterpene | 3.264 | 1014 | 1.91% |
| 6 | o-Cymene | 134.22 | Aromatic monoterpene | 3.355 | 1022 | 8.16% |
| 7 | 1,8-Cineole (eucalyptol) | 154.25 | Bicyclic epoxydenated monoterpene | 3.457 | 1026 | 22.28% |
| 8 | γ-Terpinene | 136.23 | Cyclic monoterpene | 3.713 | 1054 | 6.09% |
| 9 | α-Terpinolene | 136.23 | Cyclic monoterpene | 4.041 | 1086 | 1.28% |
| 10 | 1-Methyl-4-(1-methylethenyl)-2-cyclohexene-1-ol | 154.25 | Cyclic oxygenated monoterpene | 4.438 | 1127 | 0.36% |
| 11 | Terpinen-4-ol | 154.25 | Cyclic oxygenated monoterpene | 5.204 | 1174 | 20.89% |
| 12 | α-Terpineol | 154.25 | Cyclic oxygenated monoterpene | 5.324 | 1186 | 2.96% |
| 13 | Trans-ascaridole glycol | 170.25 | Cyclic oxygenated monoterpene | 6.314 | 1273 | 1.08% |
| 14 | Nonidentified compound | - | - | 6.966 | - | 0.56% |
| 15 | Alloaromadendrene | 204.35 | Sesquiterpene | 8.564 | 1445 | 1.49% |
| 16 | δ-Cadinene | 204.35 | Sesquiterpene | 9.575 | 1522 | 1.09% |
| 17 | Nonidentified compound | - | - | 10.258 | - | 0.34% |
| 18 | Nonidentified compound | - | - | 10.340 | - | 0.46% |
| 19 | Trans-caryophyllene | 204.35 | Bicyclic sesquiterpene | 11.245 | 1531 | 1.08% |
| 20 | (-)-α-Bisabolol | 222.37 | Monocyclic sesquiterpene alcohol | 11.534 | 1685 | 25.73% |
| 21 | Farnesol | 222.37 | Acyclic sesquiterpene alcohol | 11.301 | 1698 | 2.16% |
| Total identified (%) | 98.64% | |||||
| Chemical classes (%) | ||||||
| Monoterpene hydrocarbons | 19.52% | |||||
| Oxygenated monoterpenes | 47.57% | |||||
| Sesquiterpene hydrocarbons | 31.55% | |||||
| Nonidentified compounds | 1.36% |
| No. | Compound a | MW b | Chemical Formula | m/z Peaks c | |
|---|---|---|---|---|---|
| Top Peak | Highest Peaks | ||||
| 1 | α-Pinene | 136.23 | C10H16 | 93.1 | 39.1; 53.1; 67.1; 77.1; 105.1; 121.1; 136.2 |
| 2 | Sabinene | 136.23 | C10H16 | 93.1 | 41.1; 53.1; 65.1; 77.1; 121.1; 136.2 |
| 3 | β-Pinene | 136.23 | C10H16 | 93.1 | 41.1; 69.2; 121.2 |
| 4 | α-Phellandrene | 136.23 | C10H16 | 93.1 | 39.1; 65.1; 77.1; 115.0; 136.2 |
| 5 | α-Terpinene | 136.23 | C10H16 | 93.1 | 77.1; 91.0; 121.2; 136.0 |
| 6 | o-Cymene | 134.22 | C10H14 | 119.2 | 39.1; 65.1; 91.1; 134.2 |
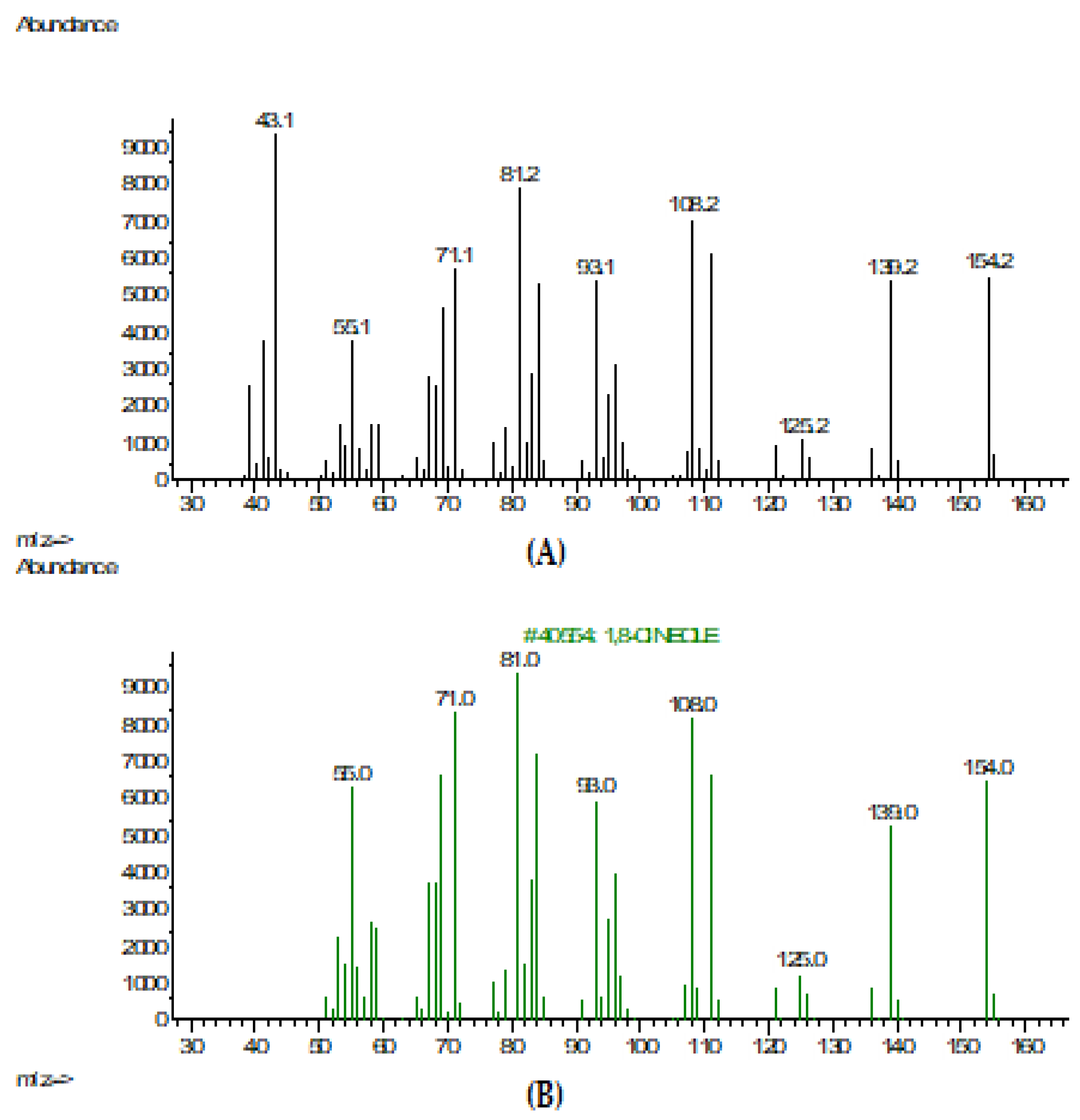
| 7 | 1,8-Cineole (eucalyptol) | 154.25 | C10H18O | 43.1 | 58.1; 71.0; 81.2; 93.0; 108.2; 139.2; 154.2 |
| 8 | γ-Terpinene | 136.23 | C10H16 | 93.1 | 39.1; 51.1; 65.1; 77.1; 105.1; 121.2; 136.2 |
| 9 | α-Terpinolene | 136.23 | C10H16 | 93.1 | 42.1; 79.0; 91.0; 121.1; 136.2 |
| 10 | 1-Methyl-4-(1-methylethenyl)-2-cyclohexene-1-ol | 154.25 | C10H18O | 43.0 | 71.0; 93.1; 139.2 |
| 11 | Terpinen-4-ol | 154.25 | C10H18O | 71.1 | 43.1; 93.1; 111.1; 136.2; 154.2 |
| 12 | α-Terpineol | 154.25 | C10H18O | 59.1 | 43.1; 81.1; 93.1; 107.1; 121.1; 136.2 |
| 13 | Trans-ascaridole glycol | 170.25 | C10H16O2 | 109.0 | 43.0; 9.0; 71.0; 81.0; 127.0 |
| 14 | Nonidentified compound | - | - | - | - |
| 15 | Alloaromadendrene | 204.35 | C15H24 | 41.1; 91; 1; 161.2 | 67.0; 77.1; 105.1; 119.1; 133.1; 147.2; 175.2; 189.2; 204.2 |
| 16 | δ-Cadinene | 204.35 | C15H24 | 161.2 | 41.1; 91.1; 105.1; 119.1; 134.2; 189.2; 204.2 |
| 17 | Nonidentified compound | - | - | - | - |
| 18 | Nonidentified compound | - | - | - | - |
| 19 | Trans-caryophyllene | 204.35 | C15H24 | 133.1 | 41.1; 79.1; 91.1; 93.1 |
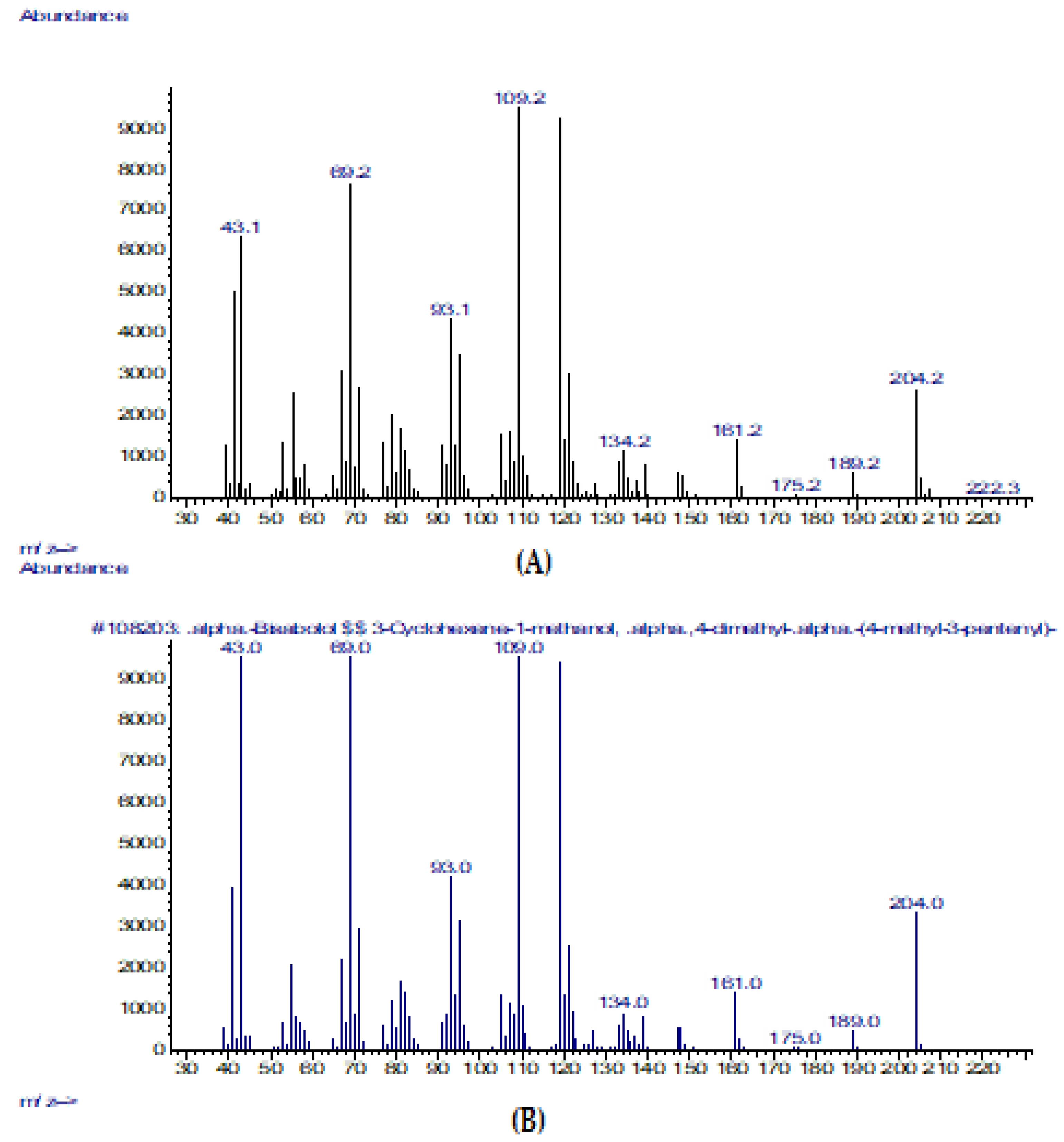
| 20 | (-)-α-Bisabolol | 222.37 | C15H26O | 109.2 | 43.1; 69.2; 93.1; 119.1; 134.2; 161.2; 189.2; 204.2 |
| 21 | Farnesol | 222.37 | C15H26O | 69.2 | 41.1; 81.0; 93.1; 121.2; 161.2 |
| No. | Strain b | MIC (mg/mL) a | ||||
|---|---|---|---|---|---|---|
| TTO | 1,8-cineole | (-)-α-bisabolol | Plant-Based Substance in a 1:1:1 Ratio | Benzalkonium Chloride | ||
| 1 | S. aureus ATCC 29213 | 40.00 | 40.00 | 5.00 | 1.25 | 5.00 |
| 2 | S. epidermidis ATCC 14990 | 1.25 | 2.50 | 1.25 | 1.25 | 5.00 |
| 3 | M. luteus ATCC 10240a | 40.00 | 40.00 | 20.00 | 20.00 | 5.00 |
| 4 | C. albicans ATCC 10231 | 5.00 | 40.00 | 20.00 | 1.25 | 10.00 |
| No. | Strain b | MIC (%) a | ||
|---|---|---|---|---|
| Plant-Based Substance at a Ratio of 1:1:1 | Climbazole | Ketoconazole | ||
| 1 | M. furfur ATCC 14251 | 0.50% | 1.00% | 0.25% |
| 2 | C. albicans ATCC 10231 | 0.25% | 1.00% | 0.25% |
| No. | Strain b | Log10CFU, Mean ± SD a | ||||
|---|---|---|---|---|---|---|
| Negative Control | 0.125% | 0.25% | 0.50% | 1.00% | ||
| 1 | Plant-based substance at a ratio of 1:1:1 | 5.85 | 5.67 ± 0.18 | 4.42 ± 0.11 | 3.25 ± 0.13 * | 3.04 ± 0.10 * |
| 2 | Climbazole | 5.08 ± 0.21 | 5.04 ± 0.14 | 4.95 ± 0.08 | 4.92 ± 0.11 | |
| 3 | Ketoconazole | 4.22 ± 0.04 | <1.00 * | <1.00 * | <1.00 * | |
| No. | Chemical | Origin | CAS Number | Manufacturer |
|---|---|---|---|---|
| 1 | Essential oil of M. alternifolia | Leaves of M. alternifolia | 68647-73-4 | Bernardi Group, Grasse, France |
| 2 | 1,8-cineole (eucalyptol) | Leaves of Eucalyptus spp. | 470-82-6 | Wuxi Lotus Essence Co., Ltd., Wuxi, Jiangsu, China |
| 3 | (-)-α-Bisabolol | Leaves of Hymenocrater yazdianus | 23089-26-1 | Merck KGaA, Darmstadt, Germany |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Filatov, V.A.; Kulyak, O.Y.; Kalenikova, E.I. Chemical Composition and Antimicrobial Potential of a Plant-Based Substance for the Treatment of Seborrheic Dermatitis. Pharmaceuticals 2023, 16, 328. https://doi.org/10.3390/ph16030328
Filatov VA, Kulyak OY, Kalenikova EI. Chemical Composition and Antimicrobial Potential of a Plant-Based Substance for the Treatment of Seborrheic Dermatitis. Pharmaceuticals. 2023; 16(3):328. https://doi.org/10.3390/ph16030328
Chicago/Turabian StyleFilatov, Viktor A., Olesya Yu. Kulyak, and Elena I. Kalenikova. 2023. "Chemical Composition and Antimicrobial Potential of a Plant-Based Substance for the Treatment of Seborrheic Dermatitis" Pharmaceuticals 16, no. 3: 328. https://doi.org/10.3390/ph16030328
APA StyleFilatov, V. A., Kulyak, O. Y., & Kalenikova, E. I. (2023). Chemical Composition and Antimicrobial Potential of a Plant-Based Substance for the Treatment of Seborrheic Dermatitis. Pharmaceuticals, 16(3), 328. https://doi.org/10.3390/ph16030328






