Pharmacological Small Molecules against Prostate Cancer by Enhancing Function of Death Receptor 5
Abstract
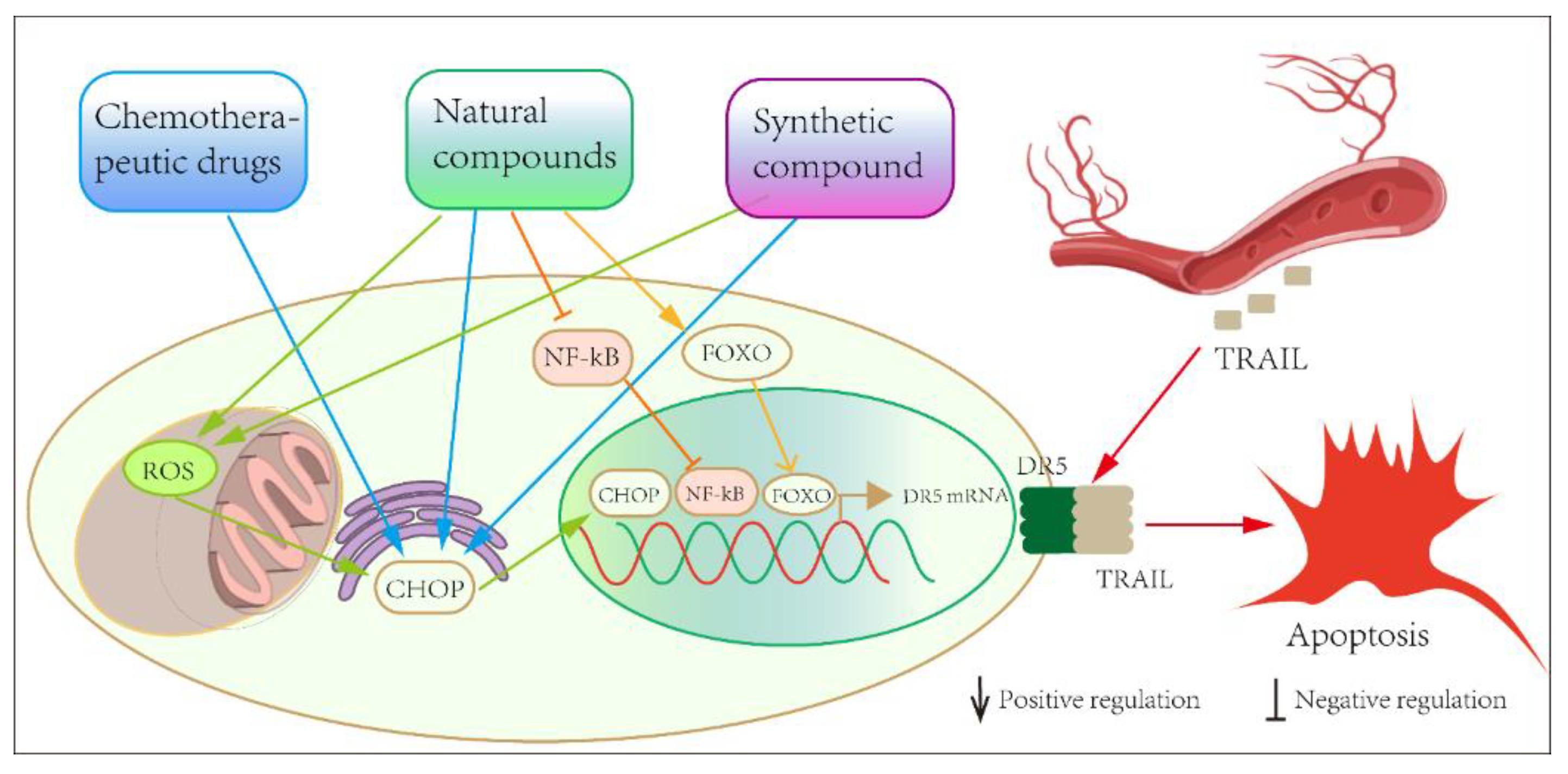
:1. Introduction
2. Chemotherapeutic Agents That Modulate the Death Receptor 5 Signaling Pathway
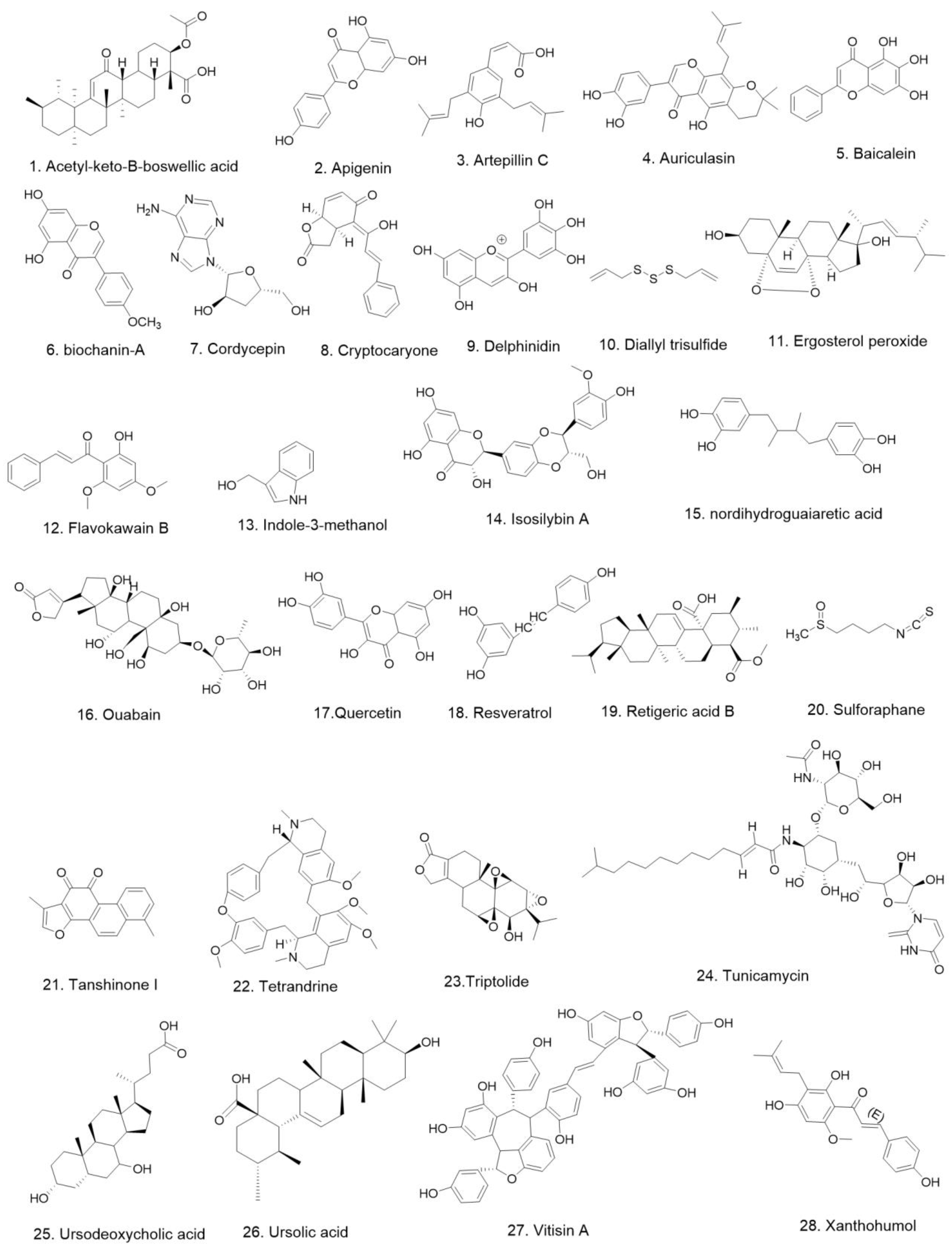
3. Natural Compounds Inhibiting Prostate Cancer by Targeting Death Receptor 5
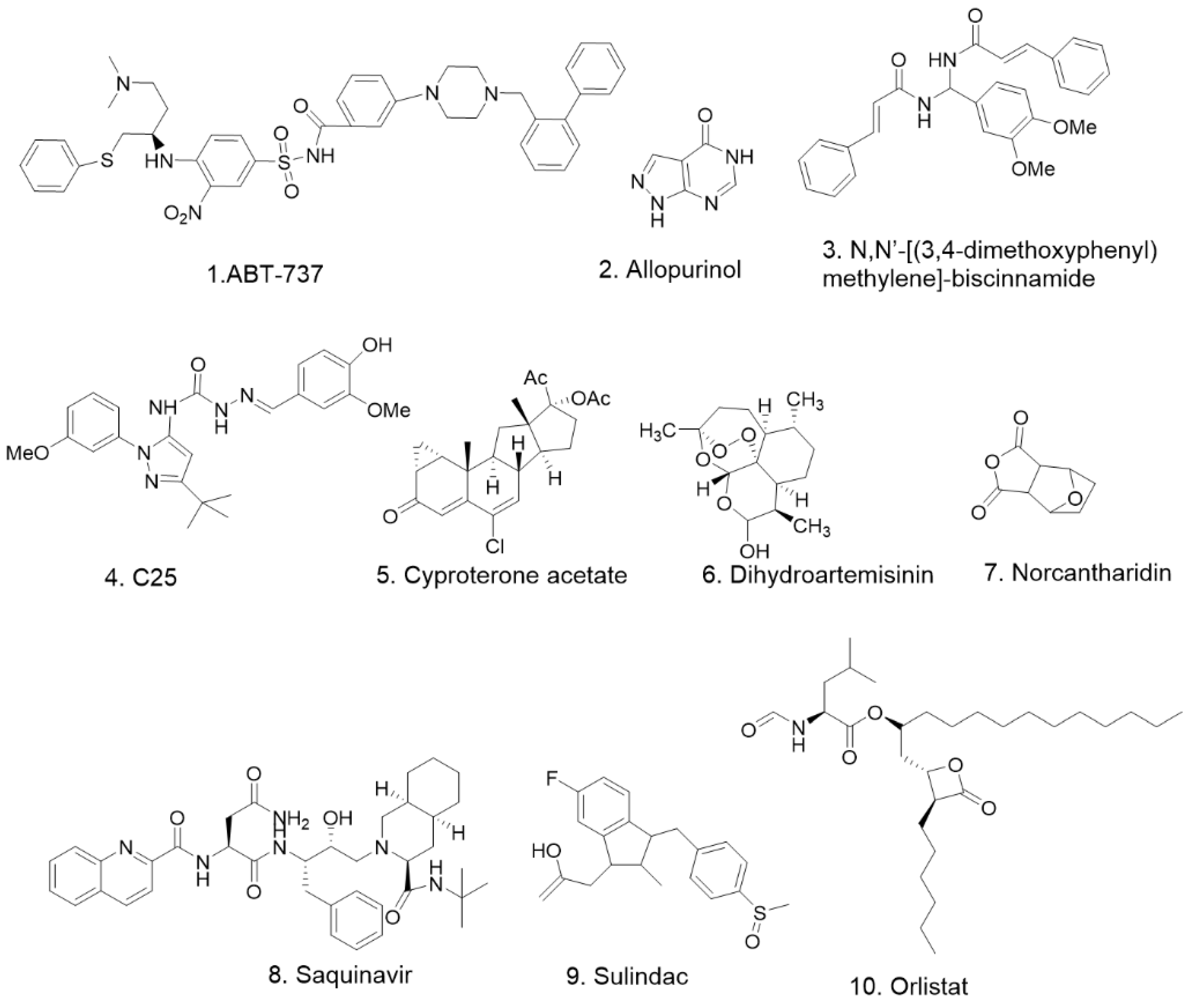
4. Synthesized Compounds Inhibiting Prostate Cancer by Targeting Death Receptor 5
5. Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Snow, O.; Lallous, N.; Singh, K.; Lack, N.; Rennie, P.; Cherkasov, A. Androgen receptor plasticity and its implications for prostate cancer therapy. Cancer Treat. Rev. 2019, 81, 101871. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.H.; Li, J.; Xu, H.E.; Melcher, K.; Yong, E.L. Androgen receptor: Structure, role in prostate cancer and drug discovery. Acta Pharmacol. Sin. 2015, 36, 3–23. [Google Scholar] [CrossRef] [Green Version]
- Shafi, A.A.; Yen, A.E.; Weigel, N.L. Androgen receptors in hormone-dependent and castration-resistant prostate cancer. Pharmacol. Ther. 2013, 140, 223–238. [Google Scholar] [CrossRef] [PubMed]
- Nader, R.; El Amm, J.; Aragon-Ching, J.B. Role of chemotherapy in prostate cancer. Asian J. Androl. 2018, 20, 221–229. [Google Scholar] [CrossRef]
- Pan, G.; Ni, J.; Wei, Y.F.; Yu, G.; Gentz, R.; Dixit, V.M. An antagonist decoy receptor and a death domain-containing receptor for TRAIL. Science 1997, 277, 815–818. [Google Scholar] [CrossRef]
- Chen, M.; Orozco, A.; Spencer, D.M.; Wang, J. Activation of initiator caspases through a stable dimeric intermediate. J. Biol. Chem. 2002, 277, 50761–50767. [Google Scholar] [CrossRef] [Green Version]
- Yuan, X.; Gajan, A.; Chu, Q.; Xiong, H.; Wu, K.; Wu, G.S. Developing TRAIL/TRAIL death receptor-based cancer therapies. Cancer Metastasis Rev. 2018, 37, 733–748. [Google Scholar] [CrossRef]
- Wang, S.; Zhu, H.; Li, Y.; Ding, J.; Wang, F.; Ding, L.; Wang, X.; Zhao, J.; Zhang, Y.; Yao, Y.; et al. First-in-human DR5 PET reveals insufficient DR5 expression in patients with gastrointestinal cancer. J. Immunother. Cancer 2021, 9, 002926. [Google Scholar] [CrossRef]
- Daniels, R.A.; Turley, H.; Kimberley, F.C.; Liu, X.S.; Mongkolsapaya, J.; ChEn, P.; Xu, X.N.; Jin, B.Q.; Pezzella, F.; Screaton, G.R. Expression of TRAIL and TRAIL receptors in normal and malignant tissues. Cell Res. 2005, 15, 430–438. [Google Scholar] [CrossRef]
- Chen, J.J.; Chou, C.W.; Chang, Y.F.; Chen, C.C. Proteasome inhibitors enhance TRAIL-induced apoptosis through the intronic regulation of DR5: Involvement of NF-kappa B and reactive oxygen species-mediated p53 activation. J. Immunol. 2008, 180, 8030–8039. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernandez-Cueto, A.; Hernandez-Cueto, D.; Antonio-Andres, G.; Mendoza-Marin, M.; Jimenez-Gutierrez, C.; Sandoval-Mejia, A.L.; Mora-Campos, R.; Gonzalez-Bonilla, C.; Vega, M.I.; Bonavida, B.; et al. Death receptor 5 expression is inversely correlated with prostate cancer progression. Mol. Med. Rep. 2014, 10, 2279–2286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holland, P.M. Death receptor agonist therapies for cancer, which is the right TRAIL? Cytokine Growth Factor Rev. 2014, 25, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, X.; Shi, M.; Jie, F.; Bai, Y.; Shen, P.; Yu, Z.; Wang, X.; Huang, C.; Tao, M.; Wang, Z.; et al. Phase III study of dulanermin (recombinant human tumor necrosis factor-related apoptosis-inducing ligand/Apo2 ligand) combined with vinorelbine and cisplatin in patients with advanced non-small-cell lung cancer. Investig. New Drugs 2018, 36, 315–322. [Google Scholar] [CrossRef]
- Wang, G.; Wang, X.; Yu, H.; Wei, S.; Williams, N.; Holmes, D.L.; Halfmann, R.; Naidoo, J.; Wang, L.; Li, L.; et al. Small-molecule activation of the TRAIL receptor DR5 in human cancer cells. Nat. Chem. Biol. 2013, 9, 84–89. [Google Scholar] [CrossRef] [Green Version]
- Munshi, A.; McDonnell, T.J.; Meyn, R.E. Chemotherapeutic agents enhance TRAIL-induced apoptosis in prostate cancer cells. Cancer Chemother. Pharmacol. 2002, 50, 46–52. [Google Scholar]
- Shankar, S.; Chen, X.F.; Srivastava, R.K. Effects of sequential treatments with chemotherapeutic drugs followed by TRAIL on prostate cancer in vitro and in vivo. Prostate 2005, 62, 165–186. [Google Scholar] [CrossRef]
- Kelly, W.K.; Halabi, S.; Elfiky, A.; Ou, S.-S.; Bogart, J.; Zelefsky, M.; Small, E. Multicenter phase 2 study of neoadjuvant paclitaxel, estramustine phosphate, and carboplatin plus androgen deprivation before radiation therapy in patients with unfavorable-risk localized prostate cancer: Results of Cancer and Leukemia Group B 99811. Cancer 2008, 113, 3137–3145. [Google Scholar] [CrossRef]
- Millikan, R.; Thall, P.F.; Lee, S.-J.; Jones, D.; Cannon, M.W.; Kuebler, J.P.; Wade, J.; Logothetis, C.J. Randomized, multicenter, phase II trial of two multicomponent regimens in androgen-independent prostate cancer. J. Clin. Oncol. 2003, 21, 878–883. [Google Scholar] [CrossRef]
- Laber, D.A.; Eatrides, J.; Jaglal, M.V.; Haider, M.; Visweshwar, N.; Patel, A. A phase I/II study of docetaxel in combination with pegylated liposomal doxorubicin in metastatic castration-resistant prostate cancer. Med. Oncol. 2020, 37, 95. [Google Scholar] [CrossRef]
- Poeckel, D.; Werz, O. Boswellic acids: Biological actions and molecular targets. Curr. Med. Chem. 2006, 13, 3359–3369. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Xia, L.J.; Hua, H.M.; Jing, Y.K. Acety-keto-beta-boswellic acid induces apoptosis through a death receptor 5-mediated pathway in prostate cancer cells. Cancer Res. 2008, 68, 1180–1186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, B.; Liu, H.; Kong, X.; Chen, X.; Wu, C. Synthesis of new chalcone-based homoserine lactones and their antiproliferative activity evaluation. Eur. J. Med. Chem. 2019, 163, 500–511. [Google Scholar] [CrossRef]
- Czeczot, H.; Tudek, B.; Kusztelak, J.; Szymczyk, T.; Dobrowolska, B.; Glinkowska, G.; Malinowski, J.; Strzelecka, H. Isolation and studies of the mutagenic activity in the Ames test of flavonoids naturally occurring in medical herbs. Mutat. Res. 1990, 240, 209–216. [Google Scholar] [CrossRef]
- Chiang, L.-C.; Ng, L.T.; Lin, I.C.; Kuo, P.-L.; Lin, C.-C. Anti-proliferative effect of apigenin and its apoptotic induction in human Hep G2 cells. Cancer Lett. 2006, 237, 207–214. [Google Scholar] [CrossRef]
- Oishi, M.; Iizumi, Y.; Taniguchi, T.; Goi, W.; Miki, T.; Sakai, T. Apigenin sensitizes prostate cancer cells to Apo2L/TRAIL by targeting adenine nucleotide translocase-2. PLoS ONE 2013, 8, e55922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, Y.K.; Paredes-Guzman, J.F.; Aguiar, C.L.; Alencar, S.M.; Fujiwara, F.Y. Chemical constituents in Baccharis dracunculifolia as the main botanical origin of southeastern Brazilian propolis. J. Agric. Food Chem. 2004, 52, 1100–1103. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.A.; Amarante, M.K.; Conti, B.J.; Sforcin, J.M. Cytotoxic constituents of propolis inducing anticancer effects: A review. J. Pharm. Pharmacol. 2011, 63, 1378–1386. [Google Scholar] [CrossRef]
- Szliszka, E.; Zydowicz, G.; Mizgala, E.; Krol, W. Artepillin C (3,5-diprenyl-4-hydroxycinnamic acid) sensitizes LNCaP prostate cancer cells to TRAIL-induced apoptosis. Int. J. Oncol. 2012, 41, 818–828. [Google Scholar] [CrossRef] [Green Version]
- Cho, H.-D.; Lee, J.-H.; Moon, K.-D.; Park, K.-H.; Lee, M.-K.; Seo, K.-I. Auriculasin-induced ROS causes prostate cancer cell death via induction of apoptosis. Food Chem. Toxicol. 2018, 111, 660–669. [Google Scholar] [CrossRef]
- Wang, Y.; Curtis-Long, M.J.; Yuk, H.J.; Kim, D.W.; Tan, X.F.; Park, K.H. Bacterial neuraminidase inhibitory effects of prenylated isoflavones from roots of Flemingia philippinensis. Bioorg. Med. Chem. 2013, 21, 6398–6404. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.D.; Gu, I.A.; Won, Y.S.; Moon, K.D.; Park, K.H.; Seo, K.I. Auriculasin sensitizes primary prostate cancer cells to TRAIL-mediated apoptosis through up-regulation of the DR5-dependent pathway. Food Chem. Toxicol. 2019, 126, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Sekiya, K.; Okuda, H. Selective inhibition of platelet lipoxygenase by baicalein. Biochem. Biophys. Res. Commun. 1982, 105, 1090–1095. [Google Scholar] [CrossRef]
- Wang, J.; Yu, Y.; Hashimoto, F.; Sakata, Y.; Fujii, M.; Hou, D.-X. Baicalein induces apoptosis through ROS-mediated mitochondrial dysfunction pathway in HL-60 cells. Int. J. Mol. Med. 2004, 14, 627–632. [Google Scholar] [CrossRef]
- Taniguchi, H.; Yoshida, T.; Horinaka, M.; Yasuda, T.; Goda, A.E.; Konishi, M.; Wakada, M.; Kataoka, K.; Yoshikawa, T.; Sakai, T. Baicalein overcomes tumor necrosis factor-related apoptosis-inducing ligand resistance via two different cell-specific pathways in cancer cells but not in normal cells. Cancer Res. 2008, 68, 8918–8927. [Google Scholar] [CrossRef] [Green Version]
- Perabo, F.G.; Von Low, E.C.; Ellinger, J.; von Rucker, A.; Muller, S.C.; Bastian, P.J. Soy isoflavone genistein in prevention and treatment of prostate cancer. Prostate Cancer Prostatic Dis. 2008, 11, 6–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Szliszka, E.; Czuba, Z.P.; Mertas, A.; Paradysz, A.; Krol, W. The dietary isoflavone biochanin-A sensitizes prostate cancer cells to TRAIL-induced apoptosis. Urol. Oncol-Semin. Orig. Investig. 2013, 31, 331–342. [Google Scholar] [CrossRef]
- Thomadaki, H.; Tsiapalis, C.M.; Scorilas, A. Polyadenylate polymerase modulations in human epithelioid cervix and breast cancer cell lines, treated with etoposide or cordycepin, follow cell cycle rather than apoptosis induction. Biol. Chem. 2005, 386, 471–480. [Google Scholar] [CrossRef]
- Xiao, L.; Ge, Y.; Sun, L.; Xu, X.; Xie, P.; Zhan, M.; Wang, M.; Dong, Z.; Li, J.; Duan, S.; et al. Cordycepin inhibits albumin-induced epithelial-mesenchymal transition of renal tubular epithelial cells by reducing reactive oxygen species production. Free Radic. Res. 2012, 46, 174–183. [Google Scholar] [CrossRef]
- Lee, H.H.; Kim, S.O.; Kim, G.Y.; Moon, S.K.; Kim, W.J.; Jeong, Y.K.; Yoo, Y.H.; Choi, Y.H. Involvement of autophagy in cordycepin-induced apoptosis in human prostate carcinoma LNCaP cells. Environ. Toxicol. Pharmacol. 2014, 38, 239–250. [Google Scholar] [CrossRef]
- Chou, T.-H.; Chen, J.-J.; Peng, C.-F.; Cheng, M.-J.; Chen, I.-S. New flavanones from the leaves of Cryptocarya chinensis and their antituberculosis activity. Chem. Biodivers. 2011, 8, 2015–2024. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, L.; Alves de Lima, P.L.; Gomes, J.C.; Stringheta, P.C.; Ribeiro, D.A.; Salvadori, D.M.F. Differential response related to genotoxicity between eggplant (Solanum melanogena) skin aqueous extract and its main purified anthocyanin (delphinidin) in vivo. Food Chem. Toxicol. 2007, 45, 852–858. [Google Scholar] [CrossRef] [PubMed]
- Bin Hafeez, B.; Asim, M.; Siddiqui, I.A.; Adhami, V.M.; Murtaza, I.; Mukhtar, H. Delphinidin, a dietary anthocyanidin in pigmented fruits and vegetables: A new weapon to blunt prostate cancer growth. Cell Cycle 2008, 7, 3320–3326. [Google Scholar] [CrossRef] [Green Version]
- Feng, Z.H.; Zhang, G.M.; Hao, T.L.; Zhou, B.; Zhang, H.; Jiang, Z.Y. Effect of diallyl trisulfide on the activation of T cell and macrophage-mediated cytotoxicity. J. Tongji Med. Univ. 1994, 14, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Shankar, S.; Chen, Q.; Ganapathy, S.; Singh, K.P.; Srivastava, R.K. Diallyl trisulfide increases the effectiveness of TRAIL and inhibits prostate cancer growth in an orthotopic model: Molecular mechanisms. Mol. Cancer Ther. 2008, 7, 2328–2338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lindequist, U.; Niedermeyer, T.H.J.; Jülich, W.-D. The pharmacological potential of mushrooms. Evid. Based Complement. Alternat. Med. 2005, 2, 285–299. [Google Scholar] [CrossRef] [Green Version]
- Rhee, Y.-H.; Jeong, S.-J.; Lee, H.-J.; Lee, H.-J.; Koh, W.; Jung, J.H.; Kim, S.-H.; Sung-Hoon, K. Inhibition of STAT3 signaling and induction of SHP1 mediate antiangiogenic and antitumor activities of ergosterol peroxide in U266 multiple myeloma cells. BMC Cancer 2012, 12, 28. [Google Scholar] [CrossRef] [Green Version]
- Han, J.; Sohn, E.J.; Kim, B.; Kim, S.; Won, G.; Yoon, S.; Lee, J.; Kim, M.J.; Lee, H.; Chung, K.; et al. Upregulation of death receptor 5 and activation of caspase 8/3 play a critical role in ergosterol peroxide induced apoptosis in DU 145 prostate cancer cells. Cancer Cell Int. 2014, 14, 117. [Google Scholar] [CrossRef] [Green Version]
- Zi, X.; Simoneau, A.R. Flavokawain A, a novel chalcone from kava extract, induces apoptosis in bladder cancer cells by involvement of Bax protein-dependent and mitochondria-dependent apoptotic pathway and suppresses tumor growth in mice. Cancer Res. 2005, 65, 3479–3486. [Google Scholar] [CrossRef] [Green Version]
- Tang, Y.; Li, X.; Liu, Z.; Simoneau, A.R.; Xie, J.; Zi, X. Flavokawain B, a kava chalcone, induces apoptosis via up-regulation of death-receptor 5 and Bim expression in androgen receptor negative, hormonal refractory prostate cancer cell lines and reduces tumor growth. Int. J. Cancer 2010, 127, 1758–1768. [Google Scholar] [CrossRef] [Green Version]
- Dashwood, R.H. Indole-3-carbinol: Anticarcinogen or tumor promoter in brassica vegetables? Chem. Biol. Interact. 1998, 110, 1–5. [Google Scholar] [CrossRef]
- Jeon, K.I.; Rih, J.K.; Kim, H.J.; Lee, Y.J.; Cho, C.H.; Goldberg, I.D.; Rosen, E.M.; Bae, I. Pretreatment of indole-3-carbinol augments TRAIL-induced apoptosis in a prostate cancer cell line, LNCaP. FEBS Lett. 2003, 544, 246–251. [Google Scholar] [CrossRef] [Green Version]
- Deep, G.; Oberlies, N.H.; Kroll, D.J.; Agarwal, R. Identifying the differential effects of silymarin constituents on cell growth and cell cycle regulatory molecules in human prostate cancer cells. Int. J. Cancer 2008, 123, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Deep, G.; Gangar, S.C.; Oberlies, N.H.; Kroll, D.J.; Agarwal, R. Isosilybin A Induces Apoptosis in Human Prostate Cancer Cells via Targeting Akt, NF-kappa B, and Androgen Receptor Signaling. Mol. Carcinog. 2010, 49, 902–912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, J.; Chuang, T.; Cheung, J.; Quan, J.; Tsai, J.; Sullivan, C.; Hector, R.F.; Reed, M.J.; Meszaros, K.; King, S.R.; et al. Masoprocol (nordihydroguaiaretic acid): A new antihyperglycemic agent isolated from the creosote bush (Larrea tridentata). Eur. J. Pharmacol. 1998, 346, 77–79. [Google Scholar] [CrossRef]
- Seufferlein, T.; Seckl, M.J.; Schwarz, E.; Beil, M.; v Wichert, G.; Baust, H.; Lührs, H.; Schmid, R.M.; Adler, G. Mechanisms of nordihydroguaiaretic acid-induced growth inhibition and apoptosis in human cancer cells. Br. J. Cancer 2002, 86, 1188–1196. [Google Scholar] [CrossRef]
- Yoshida, T.; Shiraishi, T.; Horinaka, M.; Nakata, S.; Yasuda, T.; Goda, A.E.; Wakada, M.; Mizutani, Y.; Miki, T.; Nishikawa, A.; et al. Lipoxygenase inhibitors induce death receptor 5/TRAIL-R2 expression and sensitize malignant tumor cells to TRAIL-induced apoptosis. Cancer Sci. 2007, 98, 1417–1423. [Google Scholar] [CrossRef]
- Friedlander, T.W.; Weinberg, V.K.; Huang, Y.; Mi, J.T.; Formaker, C.G.; Small, E.J.; Harzstark, A.L.; Lin, A.M.; Fong, L.; Ryan, C.J. A phase II study of insulin-like growth factor receptor inhibition with nordihydroguaiaretic acid in men with non-metastatic hormone-sensitive prostate cancer. Oncol. Rep. 2012, 27, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.-T.; Chueh, S.-C.; Teng, C.-M.; Guh, J.-H. Investigation of ouabain-induced anticancer effect in human androgen-independent prostate cancer PC-3 cells. Biochem. Pharmacol. 2004, 67, 727–733. [Google Scholar] [CrossRef]
- Chang, Y.-M.; Shih, Y.-L.; Chen, C.-P.; Liu, K.-L.; Lee, M.-H.; Lee, M.-Z.; Hou, H.-T.; Huang, H.-C.; Lu, H.-F.; Peng, S.-F.; et al. Ouabain induces apoptotic cell death in human prostate DU 145 cancer cells through DNA damage and TRAIL pathways. Environ. Toxicol. 2019, 34, 1329–1339. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kim, E.H.; Park, S.S.; Lim, J.H.; Kwon, T.K.; Choi, K.S. Quercetin sensitizes human hepatoma cells to TRAIL-induced apoptosis via Sp1-mediated DR5 up-regulation and proteasome-mediated c-FLIPS down-regulation. J. Cell Biochem. 2008, 105, 1386–1398. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.H.; Heo, J.; Lee, Y.J.; Kwon, T.K.; Kim, Y.H. Quercetin enhances TRAIL-induced apoptosis in prostate cancer cells via increased protein stability of death receptor 5. Life Sci. 2010, 86, 351–357. [Google Scholar] [CrossRef] [Green Version]
- Chen, Q.; Ganapathy, S.; Singh, K.P.; Shankar, S.; Srivastava, R.K. Resveratrol induces growth arrest and apoptosis through activation of FOXO transcription factors in prostate cancer cells. PLoS ONE 2010, 5, e15288. [Google Scholar] [CrossRef] [PubMed]
- Shankar, S.; Siddiqui, I.; Srivastava, R.K. Molecular mechanisms of resveratrol (3,4,5-trihydroxy-trans-stilbene) and its interaction with TNF-related apoptosis inducing ligand (TRAIL) in androgen-insensitive prostate cancer cells. Mol. Cell. Biochem. 2007, 304, 273–285. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-N.; Zhang, H.-J.; Ren, D.-M.; Ji, M.; Yu, W.-T.; Lou, H.-X. Lobarialides A-C, antifungal triterpenoids from the lichen Lobaria kurokawae. Chem. Biodivers. 2009, 6, 746–753. [Google Scholar] [CrossRef]
- Liu, Y.-Q.; Hu, X.-Y.; Lu, T.; Cheng, Y.-N.; Young, C.Y.F.; Yuan, H.-Q.; Lou, H.-X. Retigeric acid B exhibits antitumor activity through suppression of nuclear factor-κB signaling in prostate cancer cells in vitro and in vivo. PLoS ONE 2012, 7, e38000. [Google Scholar] [CrossRef]
- Liu, Y.; Yue, C.; Li, J.; Wu, J.; Wang, S.; Sun, D.; Guo, Y.; Lin, Z.; Zhang, D.; Wang, R. Enhancement of cisplatin cytotoxicity by Retigeric acid B involves blocking DNA repair and activating DR5 in prostate cancer cells. Oncol. Lett. 2018, 15, 2871–2880. [Google Scholar] [CrossRef] [Green Version]
- Singh, S.V.; Srivastava, S.K.; Choi, S.; Lew, K.L.; Antosiewicz, J.; Xiao, D.; Zeng, Y.; Watkins, S.C.; Johnson, C.S.; Trump, D.L.; et al. Sulforaphane-induced cell death in human prostate cancer cells is initiated by reactive oxygen species. J. Biol. Chem. 2005, 280, 19911–19924. [Google Scholar] [CrossRef] [Green Version]
- Shankar, S.; Ganapathy, S.; Srivastava, R.K. Sulforaphane Enhances the Therapeutic Potential of TRAIL in Prostate Cancer Orthotopic Model through Regulation of Apoptosis, Metastasis, and Angiogenesis. Clin. Cancer Res. 2008, 14, 6855–6866. [Google Scholar] [CrossRef] [Green Version]
- Chang, C.-C.; Lai, J.-S.; Tsai, C.-S.; Ma, S.-W.; Lin, J.-Y.; Huang, L.-R.; Lu, C.-H.; Liao, E.-C.; Ho, T.-F. Proapoptotic and TRAIL-sensitizing constituents isolated from Salvia militiorrhiza (Danshen). J. Biosci. Bioeng. 2013, 116, 516–523. [Google Scholar] [CrossRef]
- Shin, E.A.; Sohn, E.J.; Won, G.; Choi, J.U.; Jeong, M.; Kim, B.; Kim, M.J.; Kim, S.H. Correction: Upregulation of microRNA135a-3p and death receptor 5 plays a critical role in Tanshinone I sensitized prostate cancer cells to TRAIL induced apoptosis. Oncotarget 2018, 9, 30720. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Liu, X.; Li, W. Tetrandrine, a Chinese plant-derived alkaloid, is a potential candidate for cancer chemotherapy. Oncotarget 2016, 7, 40800–40815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shishodia, G.; Koul, S.; Dong, Q.; Koul, H.K. Tetrandrine (TET) Induces Death Receptors Apo Trail R1 (DR4) and Apo Trail R2 (DR5) and Sensitizes Prostate Cancer Cells to TRAIL-Induced Apoptosis. Mol. Cancer Ther. 2018, 17, 1217–1228. [Google Scholar] [CrossRef] [Green Version]
- Wang, G.; Lemos, J.R.; Iadecola, C. Herbal alkaloid tetrandrine: Fron an ion channel blocker to inhibitor of tumor proliferation. Trends Pharmacol. Sci. 2004, 25, 120–123. [Google Scholar] [CrossRef]
- Carter, B.Z.; Mak, D.H.; Schober, W.D.; Dietrich, M.F.; Pinilla, C.; Vassilev, L.T.; Reed, J.C.; Andreeff, M. Triptolide sensitizes AML cells to TRAIL-induced apoptosis via decrease of XIAP and p53-mediated increase of DR5. Blood 2008, 111, 3742–3750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, X.W.; Sun, Y. Triptolide sensitizes TRAIL-induced apoptosis in prostate cancer cells via p53-mediated DR5 up-regulation. Mol. Biol. Rep. 2012, 39, 8763–8770. [Google Scholar] [CrossRef]
- Whibley, C.; Pharoah, P.D.P.; Hollstein, M. p53 polymorphisms: Cancer implications. Nat. Rev. Cancer 2009, 9. [Google Scholar] [CrossRef]
- Elbein, A.D. Inhibitors of the biosynthesis and processing of N-linked oligosaccharide chains. Annu. Rev. Biochem. 1987, 56, 497–534. [Google Scholar] [CrossRef]
- Jung, Y.-H.; Lim, E.J.; Heo, J.; Kwon, T.K.; Kim, Y.-H. Tunicamycin sensitizes human prostate cells to TRAIL-induced apoptosis by upregulation of TRAIL receptors and downregulation of cIAF2. Int. J. Oncol. 2012, 40, 1941–1948. [Google Scholar] [CrossRef]
- Shiraishi, T.; Yoshida, T.; Nakata, S.; Horinaka, M.; Wakada, M.; Mizutani, Y.; Miki, T.; Sakai, T. Tunicamycin enhances tumor necrosis factor-related apoptosis-inducing ligand-induced apoptosis in human prostate cancer cells. Cancer Res. 2005, 65, 6364–6370. [Google Scholar] [CrossRef] [Green Version]
- Lefebvre, P.; Cariou, B.; Lien, F.; Kuipers, F.; Staels, B. Role of bile acids and bile acid receptors in metabolic regulation. Physiol. Rev. 2009, 89, 147–191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, S.-C.; Duong, H.-Q.; Choi, J.E.; Lee, T.-B.; Kang, J.-H.; Oh, S.H.; Han, S.I. Lipid raft-dependent death receptor 5 (DR5) expression and activation are critical for ursodeoxycholic acid-induced apoptosis in gastric cancer cells. Carcinogenesis 2011, 32, 723–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, W.S.; Jung, J.H.; Panchanathan, R.; Yun, J.W.; Kim, D.H.; Kim, H.J.; Kim, G.S.; Ryu, C.H.; Shin, S.C.; Hong, S.C.; et al. Ursodeoxycholic Acid Induces Death Receptor-mediated Apoptosis in Prostate Cancer Cells. J. Cancer Prev. 2017, 22, 16–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deepak, M.; Handa, S.S. Antiinflammatory activity and chemical composition of extracts of Verbena officinalis. Phytother. Res. 2000, 14, 463–465. [Google Scholar] [CrossRef]
- Ohigashi, H.; Takamura, H.; Koshimizu, K.; Tokuda, H.; Ito, Y. Search for possible antitumor promoters by inhibition of 12-O-tetradecanoylphorbol-13-acetate-induced Epstein-Barr virus activation; ursolic acid and oleanolic acid from an anti-inflammatory Chinese medicinal plant, Glechoma hederaceae L. Cancer Lett. 1986, 30, 143–151. [Google Scholar] [CrossRef]
- Shin, S.W.; Park, J.-W. Ursolic acid sensitizes prostate cancer cells to TRAIL-mediated apoptosis. Biochim. Biophys. Acta 2013, 1833, 723–730. [Google Scholar] [CrossRef] [Green Version]
- Sung, M.J.; Davaatseren, M.; Kim, W.; Park, S.K.; Kim, S.-H.; Hur, S.J.; Kim, M.S.; Kim, Y.-S.; Kwon, D.Y. Vitisin A suppresses LPS-induced NO production by inhibiting ERK, p38, and NF-kappaB activation in RAW 264.7 cells. Int. Immunopharmacol. 2009, 9, 319–323. [Google Scholar] [CrossRef]
- Shin, D.; Kwon, H.-Y.; Sohn, E.J.; Nam, M.S.; Kim, J.H.; Lee, J.C.; Ryu, S.-Y.; Park, B.; Kim, S.-H. Upregulation of Death Receptor 5 and Production of Reactive Oxygen Species Mediate Sensitization of PC-3 Prostate Cancer Cells to TRAIL Induced Apoptosis by Vitisin A. Cell. Physiol. Biochem. 2015, 36, 1151–1162. [Google Scholar]
- Stevens, J.F.; Page, J.E. Xanthohumol and related prenylflavonoids from hops and beer: To your good health! Phytochemistry 2004, 65, 1317–1330. [Google Scholar] [CrossRef]
- Klosek, M.; Mertas, A.; Krol, W.; Jaworska, D.; Szymszal, J.; Szliszka, E. Tumor Necrosis Factor-Related Apoptosis-Inducing Ligand-Induced Apoptosis in Prostate Cancer Cells after Treatment with Xanthohumol-A Natural Compound Present in Humulus lupulus L. Int. J. Mol. Sci. 2016, 17, 837. [Google Scholar] [CrossRef] [Green Version]
- Oltersdorf, T.; Elmore, S.W.; Shoemaker, A.R.; Armstrong, R.C.; Augeri, D.J.; Belli, B.A.; Bruncko, M.; Deckwerth, T.L.; Dinges, J.; Hajduk, P.J.; et al. An inhibitor of Bcl-2 family proteins induces regression of solid tumours. Nature 2005, 435, 677–681. [Google Scholar] [CrossRef]
- Certo, M.; Del Gaizo Moore, V.; Nishino, M.; Wei, G.; Korsmeyer, S.; Armstrong, S.A.; Letai, A. Mitochondria primed by death signals determine cellular addiction to antiapoptotic BCL-2 family members. Cancer Cell 2006, 9, 351–365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, J.H.; Kandasamy, K.; Kraft, A.S. ABT-737 Induces Expression of the Death Receptor 5 and Sensitizes Human Cancer Cells to TRAIL-induced Apoptosis. J. Biol. Chem. 2008, 283, 25003–25013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamaguchi, H.; Wang, H.G. CHOP is involved in endoplasmic reticulum stress-induced apoptosis by enhancing DR5 expression in human carcinoma cells. J. Biol. Chem. 2004, 279, 45495–45502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berry, C.E.; Hare, J.M. Xanthine oxidoreductase and cardiovascular disease: Molecular mechanisms and pathophysiological implications. J. Physiol. 2004, 555, 589–606. [Google Scholar] [CrossRef]
- Yasuda, T.; Yoshida, T.; Goda, A.E.; Horinaka, M.; Yano, K.; Shiraishi, T.; Wakada, M.; Mizutani, Y.; Miki, T.; Sakai, T. Anti-Gout Agent Allopurinol Exerts Cytotoxicity to Human Hormone-Refractory Prostate Cancer Cells in Combination with Tumor Necrosis Factor-Related Apoptosis-Inducing Ligand. Mol. Cancer Res. 2008, 6, 1852–1860. [Google Scholar] [CrossRef] [Green Version]
- Hiromi, I.; Nakata, S.; Uenishi, J. Up-regulation of Death Receptor 5/TRAIL-R2 Mediates Apoptosis Induced by N,N’-[(3,4-dimethoxyphenyl)methylene] Biscinnamide in Cancer Cells. Anticancer Res. 2020, 40, 5035–5041. [Google Scholar] [CrossRef]
- Field, J.J.; Singh, A.J.; Kanakkanthara, A.; Halafihi, T.i.; Northcote, P.T.; Miller, J.H. Microtubule-stabilizing activity of zampanolide, a potent macrolide isolated from the Tongan marine sponge Cacospongia mycofijiensis. J. Med. Chem. 2009, 52, 7328–7332. [Google Scholar] [CrossRef]
- James, M.A.; Seibel, W.L.; Kupert, E.; Hu, X.X.; Potharla, V.Y.; Anderson, M.W. A novel, soluble compound, C25, sensitizes to TRAIL-induced apoptosis through upregulation of DR5 expression. Anti-Cancer Drugs 2015, 26, 518–530. [Google Scholar] [CrossRef]
- Sharma, R.A.; Gescher, A.J.; Steward, W.P. Curcumin: The story so far. Eur. J. Cancer 2005, 41, 1955–1968. [Google Scholar] [CrossRef]
- Kayigil, O.; Atahan, O.; Metin, A. Cyproterone acetate monotherapy in advanced prostatic carcinoma. Int. Urol. Nephrol. 1997, 29, 213–220. [Google Scholar] [CrossRef]
- Chen, L.J.; Wolff, D.W.; Xie, Y.; Lin, M.F.; Tu, Y.P. Cyproterone acetate enhances TRAIL-induced androgen- independent prostate cancer cell apoptosis via up-regulation of death receptor 5. BMC Cancer 2017, 17, 179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bolla, M.; Collette, L.; Blank, L.; Warde, P.; Dubois, J.B.; Mirimanoff, R.-O.; Storme, G.; Bernier, J.; Kuten, A.; Sternberg, C.; et al. Long-term results with immediate androgen suppression and external irradiation in patients with locally advanced prostate cancer (an EORTC study): A phase III randomised trial. Lancet 2002, 360, 103–106. [Google Scholar] [CrossRef]
- Nyein, C.M.; Zhong, X.; Lu, J.; Luo, H.; Wang, J.; Rapposelli, S.; Li, M.; Ou-Yang, Y.; Pi, R.; He, X. Synthesis and anti-glioblastoma effects of artemisinin-isothiocyanate derivatives. RSC Adv. 2018, 8, 40974–40983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, Q.; Shi, J.X.; Shen, X.L.; An, J.; Sun, H.; Wang, L.; Hu, Y.J.; Sun, Q.; Fu, L.C.; Sheikh, M.S.; et al. Dihydroartemisinin upregulates death receptor 5 expression and cooperates with TRAIL to induce apoptosis in human prostate cancer cells. Cancer Biol. Ther. 2010, 9, 819–824. [Google Scholar] [CrossRef]
- Xiao, W.; Dai, B.; Zhu, Y.; Ye, D. Norcantharidin induces autophagy-related prostate cancer cell death through Beclin-1 upregulation by miR-129-5p suppression. Tumour Biol. 2016, 37, 15643–15648. [Google Scholar] [CrossRef]
- Yang, P.-Y.; Hu, D.-N.; Kao, Y.-H.; Lin, I.C.; Chou, C.-Y.; Wu, Y.-C. Norcantharidin induces apoptosis in human prostate cancer cells through both intrinsic and extrinsic pathways. Pharmacol. Rep. 2016, 68, 874–880. [Google Scholar] [CrossRef]
- Pajonk, F.; Himmelsbach, J.; Riess, K.; Sommer, A.; McBride, W.H. The human immunodeficiency virus (HIV)-1 protease inhibitor saquinavir inhibits proteasome function and causes apoptosis and radiosensitization in non-HIV-associated human cancer cells. Cancer Res. 2002, 62, 5230–5235. [Google Scholar]
- Maksimovic-Ivanic, D.; Mijatovic, S.; Miljkovic, D.; Harhaji-Trajkovic, L.; Timotijevic, G.; Mojic, M.; Dabideen, D.; Cheng, K.F.; McCubrey, J.A.; Mangano, K.; et al. The antitumor properties of a nontoxic, nitric oxide-modified version of saquinavir are independent of Akt. Mol. Cancer Ther. 2009, 8, 1169–1178. [Google Scholar] [CrossRef] [Green Version]
- Donia, M.; Maksimovic-Ivanic, D.; Mijatovic, S.; Mojic, M.; Miljkovic, D.; Timotijevic, G.; Fagone, P.; Caponnetto, S.; Al-Abed, Y.; McCubrey, J.A.; et al. In vitro and in vivo anticancer action of Saquinavir-NO, a novel nitric oxide-derivative of the protease inhibitor saquinavir, on hormone resistant prostate cancer cells. Cell Cycle 2011, 10, 492–499. [Google Scholar] [CrossRef] [Green Version]
- Rao, C.V.; Rivenson, A.; Simi, B.; Zang, E.; Kelloff, G.; Steele, V.; Reddy, B.S. Chemoprevention of colon carcinogenesis by sulindac, a nonsteroidal anti-inflammatory agent. Cancer Res. 1995, 55, 1464–1472. [Google Scholar]
- Huang, Y.; He, Q.; Hillman, M.J.; Rong, R.; Sheikh, M.S. Sulindac sulfide-induced apoptosis involves death receptor 5 and the caspase 8-dependent pathway in human colon and prostate cancer cells. Cancer Res. 2001, 61, 6918–6924. [Google Scholar] [PubMed]
- Kridel, S.J.; Axelrod, F.; Rozenkrantz, N.; Smith, J.W. Orlistat is a novel inhibitor of fatty acid synthase with antitumor activity. Cancer Res. 2004, 64, 2070–2075. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fujiwara, J.; Sowa, Y.; Horinaka, M.; Koyama, M.; Wakada, M.; Miki, T.; Sakai, T. The anti-obesity drug orlistat promotes sensitivity to TRAIL by two different pathways in hormone-refractory prostate cancer cells. Int. J. Oncol. 2012, 40, 1483–1491. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmieri, R.; Buckley, S.A.; Othus, M.; Halpern, A.B.; Percival, M.-E.M.; Scott, B.L.; Hendrie, P.C.; Becker, P.S.; Oehler, V.G.; Estey, E.H.; et al. Randomized phase 1 study of sequential (primed) vs. concurrent decitabine in combination with cladribine, cytarabine, G-CSF, and mitoxantrone (CLAG-M) in adults with newly diagnosed or relapsed/refractory acute myeloid leukemia (AML) or other high-grade myeloid neoplasm. Leuk. Lymphoma 2020, 61, 1728–1731. [Google Scholar] [CrossRef]
- Reed, G.A.; Peterson, K.S.; Smith, H.J.; Gray, J.C.; Sullivan, D.K.; Mayo, M.S.; Crowell, J.A.; Hurwitz, A. A phase I study of indole-3-carbinol in women: Tolerability and effects. Cancer Epidemiol. Biomarkers Prev. 2005, 14, 1953–1960. [Google Scholar] [CrossRef] [Green Version]
- Zwicker, J.I.; Schlechter, B.L.; Stopa, J.D.; Liebman, H.A.; Aggarwal, A.; Puligandla, M.; Caughey, T.; Bauer, K.A.; Kuemmerle, N.; Wong, E.; et al. Targeting protein disulfide isomerase with the flavonoid isoquercetin to improve hypercoagulability in advanced cancer. JCI Insight 2019, 4, e125851. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, A.V.; Martinez, M.; Stamos, M.J.; Moyer, M.P.; Planutis, K.; Hope, C.; Holcombe, R.F. Results of a phase I pilot clinical trial examining the effect of plant-derived resveratrol and grape powder on Wnt pathway target gene expression in colonic mucosa and colon cancer. Cancer Manag. Res. 2009, 1, 25–37. [Google Scholar] [PubMed]
- Zhang, Z.; Garzotto, M.; Davis, E.W.; Mori, M.; Stoller, W.A.; Farris, P.E.; Wong, C.P.; Beaver, L.M.; Thomas, G.V.; Williams, D.E.; et al. Sulforaphane Bioavailability and Chemopreventive Activity in Men Presenting for Biopsy of the Prostate Gland: A Randomized Controlled Trial. Nutr. Cancer 2020, 72, 74–87. [Google Scholar] [CrossRef]
- van Heumen, B.W.H.; Roelofs, H.M.J.; Vink-Börger, M.E.; Dekker, E.; Mathus-Vliegen, E.M.H.; Dees, J.; Koornstra, J.J.; Langers, A.M.J.; Nagtegaal, I.D.; Kampman, E.; et al. Ursodeoxycholic acid counteracts celecoxib in reduction of duodenal polyps in patients with familial adenomatous polyposis: A multicentre, randomized controlled trial. Orphanet J. Rare Dis. 2013, 8, 118. [Google Scholar] [CrossRef] [Green Version]
- Spina, M.; Nagy, Z.; Ribera, J.M.; Federico, M.; Aurer, I.; Jordan, K.; Borsaru, G.; Pristupa, A.S.; Bosi, A.; Grosicki, S.; et al. FLORENCE: A randomized, double-blind, phase III pivotal study of febuxostat versus allopurinol for the prevention of tumor lysis syndrome (TLS) in patients with hematologic malignancies at intermediate to high TLS risk. Ann. Oncol. 2015, 26, 2155–2161. [Google Scholar] [CrossRef]
- Thompson, P.A.; Huang, C.; Yang, J.; Wertheim, B.C.; Roe, D.; Zhang, X.; Ding, J.; Chalasani, P.; Preece, C.; Martinez, J.; et al. Sulindac, a Nonselective NSAID, Reduces Breast Density in Postmenopausal Women with Breast Cancer Treated with Aromatase Inhibitors. Clin. Cancer Res. 2021, 27, 5660–5668. [Google Scholar] [CrossRef] [PubMed]
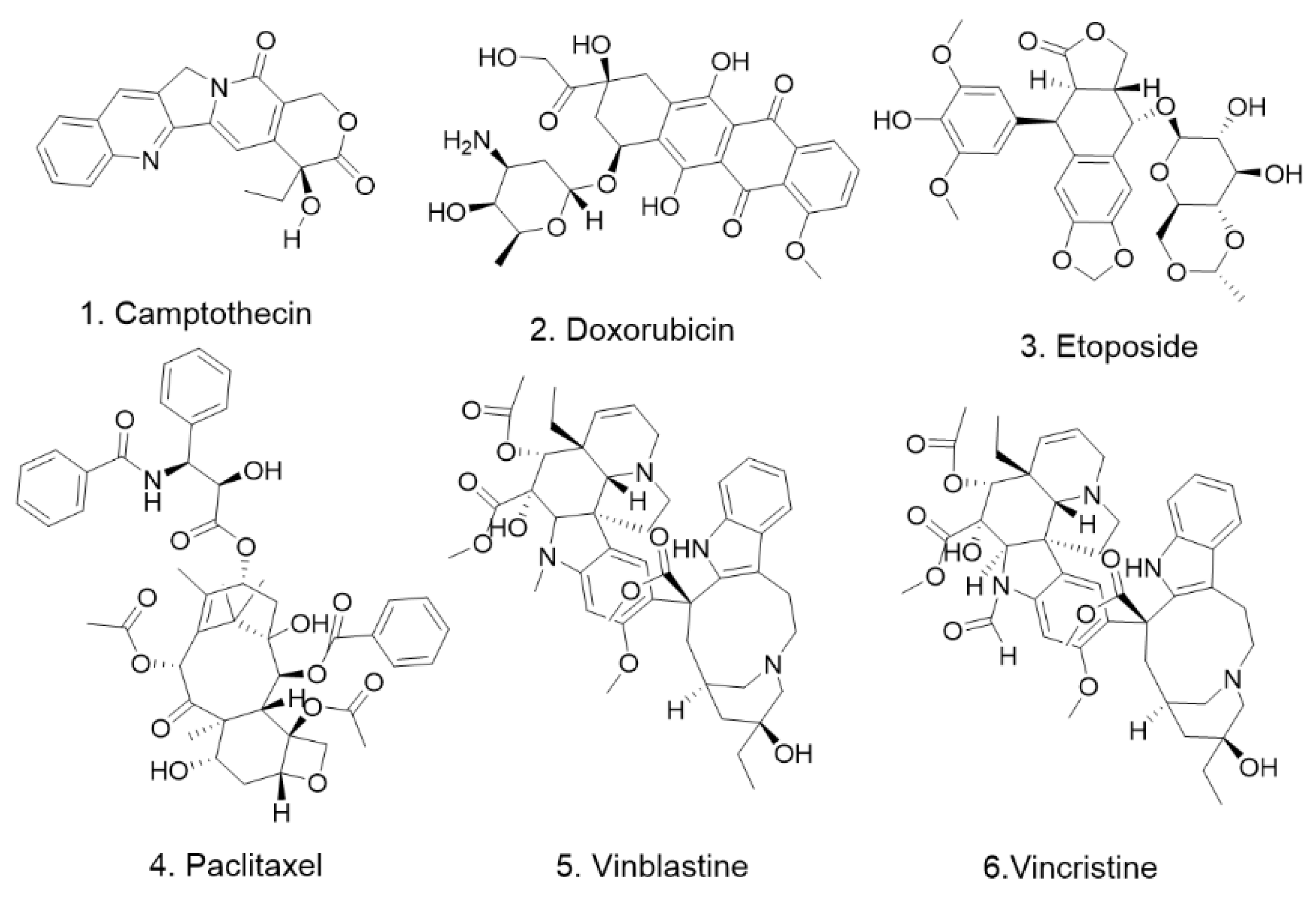
| No. | Name | Source | Cell Line | Cell Experimental Concentration | Animal Experimental Concentration | Reference |
|---|---|---|---|---|---|---|
| 1 | Camptothecin | Camptotheca acuminata Decne | PC3/LNCaP/DU145 | 0 μM–50 μM | 15 mg/kg (Balb/c nu/nu mice) | [17] |
| 2 | Doxorubicin | Boraginaceae | PC3/LNCaP/DU145 | 0 μM–50 μM | 15 mg/kg (Balb/c nu/nu mice) | [17] |
| 3 | Etoposide | Podophyllotoxin | PC3/LNCaP/DU145 | 0 μM–50 μM | 15 mg/kg (Balb/c nu/nu mice) | [17] |
| 4 | Paclitaxel | Pacific yew, Chinese yew | PC3/LNCaP/DU145 | 0 μM–50 μM | 15 mg/kg (Balb/c nu/nu mice) | [17] |
| 5 | Vinblastine | Madagascar rosy periwinkle | PC3/LNCaP/DU145 | 0 μM–50 μM | N.D. | [17] |
| 6 | Vincristine | Madagascar rosy periwinkle | PC3/LNCaP/DU145 | 0 μM–50 μM | N.D. | [17] |
| No. | Name | Source | Cell Line | Cell Experimental Concentration | Animal Experimental Concentration | Reference |
|---|---|---|---|---|---|---|
| 1 | Acetyl-Keto-β-Boswellic Acid | Boswellia serrata and Boswellia carterri Birdw. | PC3/LNCaP | 10 mg/mL–20 mg/mL | N.D. | [22] |
| 2 | Apigenin | Chamomile, honeybee, Perilla, verbena, yarrow | DU145/LNCap | 5 μM, 10 μM, 20 μM | N.D. | [26] |
| 3 | Artepillin C | Baccharis dracunculiforia | LNCaP | 50 μM–100 μM | N.D. | [29] |
| 4 | Auriculasin | Flemingia philippinensis | RWPE-1, RC-58T/h/SA#4 | 5 μM–10 μM | N.D. | [32] |
| 5 | Baicalein | Scutellaria baicalensis | PC-3 | 10 μM, 20 μM, 40 μM, 80 μM | N.D. | [35] |
| 6 | Biochanin-A | soy and red clover | LNCaP/DU145 | 20 μM, 50 μM, 100 μM | N.D. | [93] |
| 7 | Cordycepin | Cordyceps militaris | LNCap | 20 μg/mL, 100 μg/mL, 150 μg/mL, 200 μg/mL | N.D. | [40] |
| 8 | Cryptocaryone | Cryptocarya infectoria | PC3/LNCaP/DU145 | PC3, IC50 = 1.6 μM; DU145, IC50 = 2.3 μM; LNCaP, IC50 = 3.4 μM | N.D. | [41] |
| 9 | Delphinidin | fruits and vegetables | LNCaP/DU145 | 30 μM, 60 μM, 90 μM | N.D. | [43] |
| 10 | Diallyl trisulfide | garlic | PC3/LNCaP | 10 μM–40 μM | 40 mg/kg (BALB/c nu/nu mice) | [45] |
| 11 | Ergosterol peroxide | Sarcodon aspratus | DU 145 | 6.25 μM, 12.5 μM, 25μM, 50 μM | N.D. | [48] |
| 12 | Flavokawain B | Piper methystticum | LNCaP, LAPC4, DU145 and PC-3 | 1.1 μM, 2.2 μM, 4.4 μM, 8.8 μM, 17.6 μM | 50 mg/kg | [50] |
| 13 | Indole-3-methanol | fruits and vegetables | LNCaP, DU145 | 30 μM, 60 μM, 90 μM | N.D. | [52] |
| 14 | Isosilybin A | Silybum marianum | LNCaP, LAPC4, 22Rv1 | 90 μM–180 μM | N.D. | [54] |
| 15 | Nordihydroguaiaretic acid | larra triedentata | DU145 | 2.5μM, 5 μM, 10 μM, 20 μM, 40 μM, 80 μM | N.D. | [55] |
| 16 | Ouabain | Strophanthus gratus and Acocanthera ouabaio | DU145 | 1.25 μM–40 μM | N.D. | [60] |
| 17 | Quercetin | Bauhinia longifolia (Bong.) | PC3/LNCaP/DU145/YPEN-1 | 10 μM–100 µM | N.D. | [61] |
| 18 | Resveratrol | grapes peanuts | PC3/DU145 | 0 μM–30 μM | N.D. | [63] |
| 19 | Retigeric acid B | Lobaria kurokawae Yoshim, | PC-3, DU145 | 2 μM, 4 μM, 6 μM, 8 μM and 10 µM | N.D. | [67] |
| 20 | Sulforaphane | Brassica oleracea italica | PC3/LNCaP | 20 μM–40 μM | 40 mg/kg (BALB/c nu/nu) | [69] |
| 21 | Tanshinone I | Salvia miltiorrhiza | PC3/DU145/M2182 | 20 μM, 40 μM, 80 μM | N.D. | [71] |
| 22 | Tetrandrine | Stephania tetrandra | LNCaP/PC3/RWPE-1 | 5 μM, 10 μM, 20 μM | N.D. | [73] |
| 23 | Triptolide | Tripterygium wilfordii | PC3/LNCaP/RWPE-2 | 50 nM–200 nM | N.D. | [76] |
| 24 | Tunicamycin | Streptomyces lysosuperficus | PC3/DU145 | 0.25 μg/mL, 0.5 µg/mL, 1 µg/mL, 2 µg/mL, 4 µg/mL | N.D. | [79] |
| 25 | Ursodeoxycholic acid | Bear bile | DU145 | 10 μg/mL, 20 μg/mL, 50 μg/mL, 100 μg/mL, 200 μg/mL | N.D. | [83] |
| 26 | Ursolic acid | Ligustrum lucidum Ait. | LNCaP, DU145, PC-3 | 10 μM, 20 μM, 30 μM, 40 μM | N.D. | [86] |
| 27 | Vitisin A | wine grapes | PC3/LNCaP/DU145 | 4 μM | N.D. | [87] |
| 28 | Xanthohumol | Humulus lupulus L | LNCaP | 20 μM, 30 μM, 50 μM | N.D. | [90] |
| No. | Name | Cell Line | Cell Experimental Concentration | Animal Experimental Concentration | Reference |
|---|---|---|---|---|---|
| 1 | ABT-737 | PC3/LNCaP | 1 μM, 5 μM, 10 μM | N.D. | [93] |
| 2 | Allopurinol | PC3/DU145 | 12.5 μM, 25 μM, 50 μM, 200 μM | N.D. | [96] |
| 3 | N, N’-[(3,4-dimethoxyphenyl) methylene]-biscinnamide | PC-3 | 10 μM, 30 μM | N.D. | [99] |
| 4 | C25 | LNCaP | 10 μM, 15 μM | N.D. | [99] |
| 5 | Cyproterone acetate | HEK293/PC3/DU145 | 50 μM | N.D. | [102] |
| 6 | Dihydroartemisinin | PC3/LNCaP/DU145 | 10 μM, 30 μM, 50 μM | 100 mg/kg (mouse) | [105] |
| 7 | Norcantharidin | 22Rv1/DU145 | 3 μg/mL, 10μg/mL, 30 μg/mL | N.D. | [107] |
| 8 | Saquinavir-NO | PC3 | 4.7 μM, 9.4 μM, 18.8 μM | 0.2 mg/mouse (BALB/c female athymic nude mice) | [110] |
| 9 | Sulindac | DU145 | 200 μM | N.D. | [112] |
| 10 | Orlistat | DU145 and PC3 | 25 μM, 50 μM, 100 μM, 200 μM | N.D. | [114] |
| No. | Name | Cancer | Phase | Reference |
|---|---|---|---|---|
| 1 | ABT-737 | ovarian Cancer | Ex Vivo | https://clinicaltrials.gov/ct2/show/NCT01440504?term=ABT-737&cond=cancer&draw=2&rank=1 (accessed on 15 August 2022) |
| 2 | cordycepin | advanced cancers, lymphomas, solid tumors, and bone marrow tumors | I/II | [115] |
| 3 | Indole-3-carbinol | breast cancer | I | [116] |
| 4 | Nordihydroguaiaretic acid | prostate cancer | II | [58] |
| 5 | Quercetin | oral cancer | II | [117] |
| 6 | Resveratrol | colon cancer and liver cancer | I/II | [118] |
| 7 | Sulforaphane | bladder and prostate cancer and breast cancer | II | [119] |
| 8 | Triptolide | solid tumors | I (Recruiting) | https://clinicaltrials.gov/ct2/show/NCT05166616?term=Triptolide&cond=cancer&draw=2&rank=1 (accessed on 15 August 2022) |
| 9 | Ursodeoxycholic acid | duodenal tumors | III | [120] |
| 10 | Allopurin | small cell tumors | I | [121] |
| 11 | Cyproterone acetate | prostate cancer | III | [103] |
| 12 | Norcantharidin | solid tumors | I (Recruiting) | https://www.clinicaltrials.gov/ct2/show/NCT04673396?term=Norcantharidin&draw=2&rank=1 (accessed on 15 August 2022) |
| 13 | Sulindal | colorectal, breast, and thyroid-free cancers | II | [122] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gan, X.; Liu, Y.; Wang, X. Pharmacological Small Molecules against Prostate Cancer by Enhancing Function of Death Receptor 5. Pharmaceuticals 2022, 15, 1029. https://doi.org/10.3390/ph15081029
Gan X, Liu Y, Wang X. Pharmacological Small Molecules against Prostate Cancer by Enhancing Function of Death Receptor 5. Pharmaceuticals. 2022; 15(8):1029. https://doi.org/10.3390/ph15081029
Chicago/Turabian StyleGan, Xia, Yonghong Liu, and Xueni Wang. 2022. "Pharmacological Small Molecules against Prostate Cancer by Enhancing Function of Death Receptor 5" Pharmaceuticals 15, no. 8: 1029. https://doi.org/10.3390/ph15081029
APA StyleGan, X., Liu, Y., & Wang, X. (2022). Pharmacological Small Molecules against Prostate Cancer by Enhancing Function of Death Receptor 5. Pharmaceuticals, 15(8), 1029. https://doi.org/10.3390/ph15081029








