Abstract
This systematic review aimed to reevaluate the available evidence of the use of biologics as treatment candidates for the treatment of severe and advanced COVID-19 disease; what are the rationale for their use, which are the most studied, and what kind of efficacy measures are described? A search through Cochrane, Embase, Pubmed, Medline, medrxiv.org, and Google scholar was performed on the use of biologic interventions in COVID-19/SARS-CoV-2 infection, viral pneumonia, and sepsis, until 11 January 2022. Throughout the research, we identified 4821 records, of which 90 were selected for qualitative analysis. Amongst the results, we identified five popular targets of use: IL6 and IL1 inhibitors, interferons, mesenchymal stem cells treatment, and anti-spike antibodies. None of them offered conclusive evidence of their efficacy with consistency and statistical significance except for some studies with anti-spike antibodies; however, Il6 and IL1 inhibitors as well as interferons show encouraging data in terms of increased survival and favorable clinical course that require further studies with better methodology standardization.
1. Introduction
At the end of 2019, a cluster of patients with pneumonia were identified in the city of Wuhan in the Hubei province in China. The behavior of the disease resulted in a fast-spreading epidemic throughout the country. In the initial approach to etiological mechanisms a hypothesis of zoonotic transmission was established, however, in a short period of time, sustained human-to-human transmission is confirmed, leading to the recognition that the disease had pandemic potential [1]. In February of 2020, the world health organization (WHO), acknowledges the disease as “coronavirus disease 2019” (COVID-19) and the virus that is purified as an etiologic agent as “severe acute respiratory syndrome coronavirus 2” (SARS-CoV-2), given that its genomic sequence is related to the virus responsible for the SARS outbreak in 2003 [2].
This pandemic has claimed over 4.7 million fatalities since its beginning and although the trend shows a progressive decline in new cases and deaths, the situation is still serious with over 3.3 million new cases and over 55,000 new deaths reported in the second half of September 2021, according to the WHO weekly reports [3]. This proportion of cases/deaths are related to the fact that COVID-19 mostly presents itself as a self-limited mild respiratory disease (80% of cases) [4], yet the cumulative number of affected patients determine a large mortality. There is no doubt that there is a need to treat the late stages of the disease, beyond the focus of vaccination as a preventive measure. Amongst the candidates undergoing scrutiny, it is desirable to address the ones with the most specific targets possible in order to avoid severe adverse effects in patients who are already in a situation with a considerable mortality rate. Accordingly, this article will aim to review the available studies regarding the use of biologics in COVID-19 critically or severely ill patients. Biologic medicines are called biologics and can be created using biotechnology or other cutting-edge technologies [5]. The final rule modifies the FDA regulatory definition of “biologic product” to include “any alpha amino acid polymer with a specific defined sequence that is greater than 40 amino acids in size” [6]. Although also biological, they are composed of sugar, proteins, nucleic acids, or complex combinations of these substances. Thus, biologicals include blood components, recombinant proteins, vaccines, monoclonal antibodies, and gene therapy, among others [7].
First, we must briefly review the comprehension of the common pathophysiological model to understand the reasons behind the selected drugs along the review. In the case of COVID-19 disease, three clinical phases can be categorized according to severity: onset of the disease, pulmonary phase, and hyper inflammation phase.
The first stage of the disease is usually characterized by mild symptoms similar to those of seasonal influenza [2]. In this stage, it is considered that the virus contacts the respiratory epithelial tissues as a predilection site of entry. Concerning this phenomenon, the first contact mechanism between the virion and the cell is through the viral crown. The virus has certain structural proteins called “spikes” that protrude from the membrane of the virion; this gives it the characteristic appearance of a crown in electron microscopy, which is reflected in the name of the virus. These spikes are transmembrane trimeric glycoproteins that are composed of two functional subunits, S1 and S2 [8,9]. It is these glycoproteins that determine the diversity of coronaviruses in terms of the tropism towards their hosts and specific tissues in an organism.
SARS-CoV-2 in this aspect shows an affinity for angiotensin-converting enzyme 2 (ACE 2) using it as a functional receptor, however, it is not the only mediator involved in the binding of the virus to the host cell. In the most recognized model, the way of entry of the virus is through endocytosis. Once inside, the virion, must fuse its membrane with the endosome, and thus release its RNA; for this purpose, it uses the transmembrane protease serine 2 (TMPS2) or the L-cathepsin that cleaves the spike into the S1 and S2 subunits. The S1 subunit ensures the stability of the anchorage to the membrane, whereas the splitting of S2 requires a second cleavage at S2 to generate a conformational change to consolidate the fusion [2,9].
Although this is the most accepted model, in fact, the particularity of this virus compared to other coronaviruses is the type of cleavage sequence “reverse-phase protein array (RPPA)” at the S1/S2 site, which is susceptible to furin [10]. Considering the ubiquity of furin, it is not surprising that this virus is highly pathogenic. Although its tropism for the angiotensin-converting enzyme explains its ease of entry through respiratory epithelia, heart, ileum, kidney, and bladder [11], its ability to compromise in other systems and its impact on the reticuloendothelial system may have to do with its RPPA cleavage sequence.
Once inside, the virus must proceed to make use of the nuclear and ribosomal machinery to achieve the replication of its RNA and biosynthesis of structural and non-structural proteins. Considering that the structural components correspond to the membrane, envelope, nucleocapsid, and spikes, non-structural proteins and their interaction with the cellular machinery are of interest as possible therapeutic targets. The evidence regarding cell interactions is extrapolated from the lessons learned in the study of SARS and MERS as close relatives of SARS-CoV-2. In this sense, it is derived that the RNA of our coronavirus consists of 11 open reading frames, which encode 16 non-structural proteins (NSP) that encompass most of the mechanisms implied in the pulmonary phase [12,13,14,15,16,17,18,19,20]. Considering this fact, we will not expand in the function of each NSP and will proceed with the characteristic phase of the critically ill, the hyper inflammation phase.
The hyper inflammation phase axis is the interaction of the virus with the immune system; the primary contact to establish is with the innate immune system. In this category, the pulmonary epithelium mainly has macrophages, which can appear in the apical epithelium, and also dendritic cells are usually found in the sub-epithelium. The immediate predictable consequence is the phagocytosis of apoptotic epithelial cells extrapolating models related to influenza viruses [21]. Koichi Yuki et al. suggest another kind of approach to this issue, implying that the coronavirus has the potential for direct infection in dendritic cells by replacing its ACE2 receptor with the specific adhesion molecule of dendritic cells (non-integrin trapping molecule 3) [9]. The chain of events continues with the presentation of the pathogen to the T cells of the immune system; this event results in the release of chemotactic that promotes the massive recruitment of other lymphocytes. It is possible that the lymphopenia observed in patients with hyperinflammation is related to this fact [22,23].
The presence of multiple inflammatory cytokines has been identified in severely ill COVID-19 patients. Interleukin 1 (IL)-1, IL-6, IL-10, granulocyte colony-stimulating factor (GCSF), monocytic chemoattractant protein 1 (MQP1), macrophage inflammatory protein (MIP) 1α, and tumor necrosis factor (TNF)-α are relevant [22,23,24]. In the study by Yonggang Zhou et al, both the cytokine storm and the distribution of the lymphocyte subpopulations, or at least the expression of the flow cytometry, are evaluated. The presence of CD69, CD38, and CD44 are highlighted, demonstrating the recruitment of both T CD8+ and T CD4+. In turn, it is worth noting the increased expression of control receptors Tm3 and PD-1 in both subpopulations of T cells, displaying depletion of cell populations [23]. It can be suggested that lymphocyte depletion may perpetuate a poor immune response to the pathogen; all this is favored by the mentioned cytokine storm microenvironment. Lymphocytic infiltration and the depletion of T cells is not the only problem that occurs in this microenvironment; it has been reported that, in patients with severe lung injury, there is a correlation with the cellular population predominance of macrophages and neutrophils in the pulmonary epithelium. [25]. To achieve this phenomenon, the immune response must use both interferon (IFN) γ and granulocytic-macrophage colony-stimulating factor (GMCEF). In this scenario, the host uses abnormal CD4 T cells that express both mediators [23].
In this review, we will aim to describe the use of biological drugs in adult patients with confirmed SARS-CoV-2 infection, preferring severe or advanced stage of compromise and their efficacy in clinical practice according to the available evidence so far.
2. Results
The process of selection and the number of articles selected was performed as de-scribed in the following chart (Figure 1). Table 1 shows the biotherapeutics in COVID-19 patients.
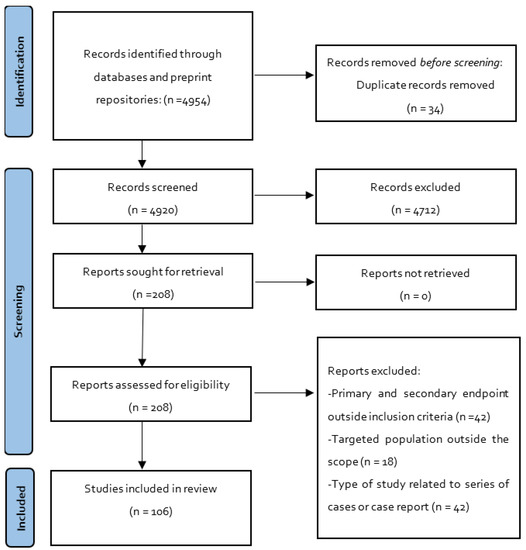
Figure 1.
Flowchart of selected studies.

Table 1.
Biotherapeutics in COVID-19 patients.
2.1. Interleukin 6 Inhibitors
Interleukin 6 (IL-6) is one of the most popular targets regarding the abundance of evidence generated since 2020. It is comprehensible since there is an availability of candidates that do not require further drug development and the pathophysiological involvement can affect one of the axes of direct lung injury. Since 2020, the evidence strongly suggests that the levels of IL-6 correlate with viral load and prognosis in critically ill patients [132]. It is also associated with the presumption that the particular mode of apoptosis in the SARS-CoV-2 infection is pyroptosis, explaining the massive release of IL-1β, IL-2, IL-6, TNF-α, MCP1 and the attrition of CD4 and CD8 T cells [133].
In the initial search, we identified 3051 results of which 43 were selected through the inclusion criteria and relevance; three particular systematic reviews are highlighted amongst the available data. Lan et. al, developed research regarding the effects of tocilizumab in either mortality, intensive care unit admission, or the requirement of mechanical ventilation. They managed to analyze seven studies from a selection of 358 studies, after database research and filtering through inclusion criteria [134]. In their results, they included the studies of Capra et al., Colaneri et al., Klopfenstein et al., Quartuccio et al., Ramaswamy et al., Roumier et al., and Wadud et al. quoted in the Table 1 [26,27,28,29,30,31,32]. According to presented data, the reported studies could not conclude a risk reduction in the overall intervention with tocilizumab, independent of the dose. Taking into account that most of the studies were retrospective in nature, the overall mortality rate for patients with tocilizumab ranged from 3.2% to 38.6% with considerable heterogeneity in the data. Understanding that the authors considered a mean mortality of 24.1% in the control groups, the pooled result did not achieve statistical significance regardless of a pre-established threshold of p = 0.1.
Cortegiani et al. performed a similar review including records regarding the use of tocilizumab in viral pneumonia caused by SARS-CoV-2 or sepsis without any restriction in language or methodology. They identified 2071 articles from which 31 were selected according to relevance [135]. Considering the amount of evidence, we will refer to the overall analysis of the database included in this study; the details of the studies can be found in the adjunct table. Summing all the population included in all the clinical data, 5776 patients were analyzed in this review; regarding the characteristics of the studies, the first thing to mention is the fact that 14 studies did not have a comparator, making the quoted results a descriptive outcome [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,136]. Of the remaining 16 studies, 14 suggested tocilizumab improved outcomes related to mortality/ICU admission, nevertheless, some of the quoted studies revealed effect disappearance in the adjusted analysis, as in the case of Martinez et al. [47]. Not all the differences noticed in the studies achieved statistical significance either. Moreover, it is worth noticing that the studies with the largest samples, ranging from 1221 to 1229 individuals, showed mixed results when considering lethality rates, although the design was not intended for comparison in the case of Perrone et al. [49]. Another noticeable tendency in this review was that the studies with the larger samples included very few patients receiving the IL-6 inhibitor compared to the proportion of patients who did not receive the intervention. Finally, a valuable analysis of Cortegiani et al. added a risk of bias in the mentioned data base using the TheROBINS-I tool (Risk of Bias in Non-randomized Studies of Interventions). This allowed the judgement 13 of the studies with a comparator as being poor quality [135].
Khan included a broader perspective regarding the intervention on this pharmacological target they included the aforementioned studies sample but also managed to include the few studies performed with other drugs that attack this same axis [137]. In this review we did not manage to find other studies than those cited in this article with Siltuximab n = 1 nor Sarilumab n = 3 [71,72,73,74]. Concerning the results, these studies show point estimators that favors the biologic with the same characteristics found in previous studies: observational cohorts with a disproportioned population comparing intervention vs. assigned controls, given the limitations of compassionate use. Two of the Sarilumab studies are descriptive of mortality and most of them have small samples. The Gordon et al. study reflects the tendency with a total population sample n = 803 with 353 patients assigned to tocilizumab, 48 to sarilumab and 402 to control [73].
Finally, in our research we found that a great deal of the available evidence was addressed in the previous systematic reviews, however, new evidence has emerged since then. Regarding these other studies, it is noteworthy that evidence is beginning to accumulate with prospective clinical trials, some of them randomized. Sabbatinelli et al., Hermine et al., Salvarani et al., Malekzadeh et al., Dastan et al. and Rodríguez-Molinero et al. have all addressed the question of Interleukin 6 inhibitor and the outcomes on severe or critical COVID-19 patients [54,55,56,57,58,59]; amongst them two studies found clinical results that favors the intervention groups with Tocilizumab, while two are descriptive with no comparator and two showed no difference with the intervention.
2.2. Interleukin 1 Inhibitors
Having addressed (IL-6) as one of the important mediators in direct lung injury we cannot forget interleukin 1 (IL-1) as one of the principal actors in the same axis mediating the pyroptosis process mentioned before, even more, considering its similitudes with the macrophage activation syndrome that complicates bacterial sepsis. Data in this environment are partially encouraging [138].
Concerning the data obtained in the initial search, we got 508 hits with the quoted search terms and selected 18 articles after the comprehensive evaluation of the inclusion criteria. The first record to be highlighted is a meta-analysis performed by Kyriazopoulou et al., recording the available data in the use of Anakinra. The aggregate data showed a pooled population of 1185 patients from nine selected studies, with a preliminary search of 209 articles [139]. Of these studies, most of them used either prospective or retrospective observational cohort methodology. The first thing to notice is the consistency of the data with point estimators favoring the intervention with Anakinra, witnessing less objective heterogeneity in the data than that observed in the interventions with the (IL-6) inhibitor, compared with the study of Lan et al. [134]. Nevertheless, from the cited studies, some of them do not reach statistical significance, i.e., Balkhair et al., Kooistra et al., and The CORIMUNO19 Collaborative group [77,81,83]. Furthermore, is worth noticing that even if the overall effect is favoring the biologic, the magnitude of the effect is moderately variable [75,76,78,79,80,82]. The pooled data used in the systematic review of Kyriazopoulou et al. finally estimates an odds ratio (OR) for mortality of 0.37 (95% CI 0.27–0.51; I² 31%) without signs of publication bias in the forest plot [139].
Out of the scope of the aforementioned systematic review, we selected several other studies; one study only presented descriptive results with a small sample in a retrospective manner [85], the rest of them presented association measures regarding death-related endpoints. In these observational studies, we see the same phenomena in the association estimators favoring the use of anakinra, emphasizing that two of them did not achieve statistical significance [84,86]. The last one revealed a significant odds ratio: 3.2 for the use of Anakinra as a survival predictor [88]. It is necessary to address the only other randomized trial made by Kyriazopoulou et al. that is not recorded in their previous metanalysis [87]. This clinical trial preselected severe pneumonia SARS-CoV-2 patients according to soluble urokinase plasminogen receptor plasma levels and randomized (double blinded) for standard care group and Anakinra intervention. The results were deemed significant with a sample of 606 and a risk of death at day 28 hazard ratio = 0.45, 95% CI 0.21–0.98, p = 0.045.
Lastly, regarding other less popular IL-1 inhibitors, no studies were found using rilonacept and four studies were selected with the use of Canakinumab. Three of them were observational with descriptive outcomes. Landi et al., described the overall survival rate with no comparator [90], while Katia et al. described reduction in oxygen consumption compared with standard treatment, and Generali et al. referred to a survival rate comparison [91,93]. Although the raw proportion of survival and the reduction in oxygen consumption is statistically significant, the dosage used on interventions are very variable and the samples are relatively small. This leads us to the final piece of evidence in this matter with the only randomized trial found in the effect of Canakinumab and mortality/clinical deterioration measures; Caricchio et al., reported a non-significant mortality risk reduction with Canakinumab with an odds ratio of 0.67 (95%CI, 0.30 to 1.50) regardless of a population sample of 454 patients [92].
2.3. Interferons
The value of interferons intertwining with the pathology of the lung injury in SARS-CoV-2 infection radiate from classical signaling pathways described for the most well-defined type I interferons (IFNs). From the known variety, IFNα and IFNβ are the most studied, describing functions in cell antimicrobial states through limiting the spread of infectious pathogens (particularly true for viruses). They interact with the innate immune system, modulating the production of cytokines, promoting antigen presentation and natural killer cell functions while restraining pro-inflammatory pathways. They interact with the adaptive immune system by promoting the development of antigen-specific T and B cell responses, deriving in immunological memory [140]. It is of particular interest the fact that IFNs interact with the JAK 1 axis to reach specific genome sequences for transcription, since this pathway encodes in several types of proteins that restrain pathogens via the inhibition of viral transcription, translation and replication, the degradation of viral nucleic acids, and the alteration of cellular lipid metabolism [141].
In this review, we encountered 206 articles in the preliminary search with a selection of nine records for analysis. The aforementioned Walz et al., included several interferon studies in his analysis of the clinical relevance of JAK inhibitors; some of the used records were specific of pediatric populations or were epidemiological descriptions of the cured patient’s data that deemed to be out of the scope of this review [142]. Still, of the remaining data we found five articles related to group 1 IFNs to be relevant, three observational studies, and two clinical trials [94,95,96,97,98]. Whereas Monfared et al., performed a clinical trial with mortality primary end point, Hung et al. described nasopharyngeal swabs negativization as a surrogate outcome of the resolution of the disease. Both trials favored the use of IFNs in these circumstances given the significance of the differences [94,96]. In the analysis of Walz, the pooled data also supported the fact that interferon reduced the mortality probability (OR, 0.19; 95% CI, 0.04–0.85); p = 0.03, n = 1906. This, including the other observational data regardless of the descriptive nature of the incidences in these records, is without standardization or control in the disease stage of the intervention, nor the regimes of dosage among centers.
Beyond the noted bibliography, we found only three other studies that complied with the inclusion criteria and were not addressed in other meta-analysis or reviews. Two of the studies referred to group 1 IFNs and one study addressed group 3 IFNs. Zhou et al. described the clearance of real time polymerase chain reaction (RT-PCR) for SARS-CoV-2 as a surrogate of disease improvement to prevent severe pneumonia. They found accelerated viral clearance from the upper respiratory tract in patients who received IFN-a2b treatment (20.4 days, p = 0.002), with a mean difference of 7 days with control group [99]. Rahmani et al., completed a randomized clinical trial with a sample of 80 patients considering the mortality outcome as a secondary outcome. The time to clinical improvement was the primary one depicting significant differences HR = 2.30; 95% CI: 1.33–3.39 for a mean difference in two days for resolution [100]. Finally, the only study to portray the effects of another group of interferon in the COVID-19 patients was the one performed by Feld and colleagues. The decline in SARS-CoV-2 RNA was the main outcome, reporting greater reduction in those treated with peginterferon lambda than placebo from day 3 onwards, with a difference of 2.42 log copies per mL at day 7 (p = 0.0041) [101].
2.4. Mesenchymal Stem Cells
Mesenchymal stem cells are also known as mesenchymal stromal cells. The use of these cells is widely known in certain inflammatory diseases, and also as part of allogenic adoptive transfer therapy and even in graft vs host disease. This might be related to their properties of tissue repair and low immunogenicity. These cells tend to present surface markers, such as CD44, CD90, and CD105, but they are also characterized by the absence of hematopoietic markers, such as CD34, CD45, and HLA-DR. Those characteristics have consequences in cell recognition and may contribute to the anti-inflammatory properties [143].
On the other hand, even if we cannot pinpoint the exact interaction of this pharmacological intervention in the context of SARS-CoV-2 infection, and even if we think of this rationale as insufficient, there is already evidence of its use on other viral-driven lung injuries, such as A/H5N1 acute lung injury [144]. From the available preliminary data, we managed to find 105 articles from which we selected 7 according to the inclusion criteria.
Amongst the selected studies, we managed to find a single meta-analysis. Qu et al., reviewed the available data concerning the use of mesenchymal stromal cells, regardless of the origin (marrow, adipose tissue, or umbilical cord), and evaluated the impact on mortality on adults with acute respiratory distress syndrome (ARDS). They encompass several literatures that addresses ARDS, however, only a single bibliography was related directly with COVID-19 patients. They use indirect evidence to analyze the plausibility of use in critically ill COVID-19 patients. Even more, some of the records used in the review reference to case reports or series of cases. Despite this, it is worth evaluating the conclusions of the pooled data: regarding the secondary outcome of mortality rate, the data seemed to favor treatment with mesenchymal cells without achieving significance: OR 0.63, 95% confidence interval 0.21–1.93. The primary outcome was safety related without reporting any serious adverse events [102].
Regarding the other selected records, only two were observational studies and four of the registries were clinical trials, some of them with randomization and masking. Overall, the studies in this topic tend to have the smallest of samples compared with the above-mentioned pharmacological targets. The consequent analysis derives into mostly descriptive outcomes, regardless of methodology. The incidence of mortality and related outcomes is limited in the small samples. There are studies that in spite of having placebo group as control, did not present a single fatality in either group. All these factors were taken into account in the study design, since most of the outcomes related to either radiological evolution, biomarker evolution, or pulmonary function tests after a predetermined time lapse [103,104,105,106,107]. The characteristics of the studies can be found in the adjunct table.
Lastly, we must highlight a mesenchymal stem cell derived compound used in a single clinical trial performed by Sengupta et al. In this trial, the authors attempted to use exosomes derived from bone marrow mesenchymal stem cells as immunomodulatory mediators that could avoid the possibility of infusional reactions and allergic responses [108]. The limitations of the study are the same as in the cluster of records mentioned above, nevertheless it opens the possibility to another method of implementing this pharmacological target.
2.5. Anti-Spike Monoclonal Antibodies
SARS-CoV-2 has four main structural proteins: spike (S), envelope, membrane, and nucleocapsid, being the S protein responsible for receptor attachment and membrane fusion, facilitating viral entry into host cells by binding to angiotensin-converting enzyme 2 (ACE2) receptors [145]. Monoclonal antibodies can help neutralize the virus in infected patients and are used as a passive immunotherapy [146].
The most studied anti spike monoclonal antibodies, based on the findings of this study, are Bamlanivimab (monotherapy) [109] and Bamlanivimab plus Etesevimab [110,111,112], followed by sotrovimab [127,128,129,130,131] and Casirivimab plus imdevimab [124,125,126]. Bamlanivimab/etesevimab has shown positive outcomes in mortality, hospitalization rate, and progression of the disease prevention, as well as Casirivimab/imdevimab did. However, Sotrovimab showed non-concluding results; observational studies demonstrated reduction in hospitalization rate and disease progression, while clinical trials compared to the placebo did not show improvements of clinical outcomes among adults hospitalised with COVID-19. There are no ongoing clinical trials for Bebtelovimab and Tixagevimab/cilgavimab, and the evidence available is limited to evauated evidence regarding the outcomes evaluated in this study.
3. Discussion
The use of biologicals in the context of COVID-19 implies a deep understanding of the physiopathological pathways of the infection to address a more directed axis, hoping for new alternatives of management to prevent severe or advanced phases of the illness. However, even if we understand the biological plausibility in each scenario of proposed interventions, we must consider the principle that guides epidemiological studies to endorse interventions. This principle is mainly directed to the degree of certainty that the evidence allows. In a general approach to the complied data in this review, we must stress the common findings in the limitations that these studies share, regardless of the pharmacological target.
First, is the methodological consistency. In this aspect the studies show great variability in their design. We are not referring to the nature of the study itself but the fact that throughout the evolution of the pandemic what is considered standard care changes continuously. If we evaluated what entails standard care in the earliest publications, of each target, we would find that the concomitant use of antivirals, such as lopinavir/ritonavir and the use of Hydroxychloroquine, were considered as standard care. Even if we argue that both control groups and intervention groups were submitted to the same variables, the risk of confounders is there, since we cannot always tell or predict interaction pathways. The multivariate regressions employed in most of the non-descriptive studies can stratify and eliminate some of this burden, however, the standard care in the most recent studies do not entail the same co-interventions.
In this line of thought, we also encounter the difficulty of controlling consistency with over-added variables, according to the selected population in each study, since not every single one performs regressions models. The fact that most of the studies start with a population with severe phase to hyperinflammatory phase, implies that not only are more interventions added as part of the standard care but the fact that dealing with these populations gives different startup lines with great variability in prognosis factors that must be either analyzed or controlled per protocol. The sheer amount of possible prognosis markers and scales can explain in some part the heterogeneity in the cited review studies, as seen in the different conclusions between Lan et. al and Cortegiani et al. [134,135], regarding Tocilizumab.
A second broad point is the inherent limitations in each methodological design. Although observational, cohorts’ studies can evaluate multiple outcomes simultaneously and establish a causal degree of certainty; the control over the multiple variables that can influence the outcome is limited, in contrast to experimental designs. This may sound as an apparent truth, but the volume of observational studies amongst the total of the data extracted may raise some eyebrows regarding of the magnitude of the possibility of unidentified confounding bias. Of course, considering the ethical reservations in the case of a pandemic, this type of study would be popular at the start of the spread since it does not require experiments with an intervention with a preselected population of intervention. Nevertheless, we cannot ignore the strains it poses on the validity of conclusions.
As a third point we must stress the importance of the variable sample size amongst the studies. Even regarding targets with a huge number of studies, such as Il 6, most of the studies have very small sample sizes individually. This can limit the possibility of reaching conclusions that can be extrapolated outside the study environment. Being aware of this might favor methodological designs that prefer surrogate outcomes as biomarkers, pulmonary function tests, radiological improvement, or PCR clearance. These surrogate markers obviously limit the possibility of the wide endorsement use of these pharmacological interventions.
Not only do the sample sizes tend to be small, but also the context of compassionate use determines a disproportionate number of patients in either control groups or intervention groups compared to their counterpart. Many of the cited studies were affected since the view of compassionate use can change in each institution. In some cases, the treatment patients were too few compared to the number of controls even in large samples. In other cases, the number of controls were insufficient as the center where the studies were performed had already implemented the intervention as hospital protocol.
A third point to be addressed is the large amount of evidence that submits pure incidence descriptive outcomes. This type of evidence is valuable to support the notion of the need for randomized trials with larger population samples; however, considering the development of the pandemic with a still relevant number of new deaths, we cannot endorse pharmacological intervention prospects with the analyzed data as a widespread practice. Furthermore, methodological standardization is needed regarding the variability of treatment regimens that differ at each center in each intervention group.
4. Materials and Methods
4.1. Search Eligibility Criteria and Search Strategy
We performed a systematic review of the literature concerning the use of biological drugs in the context of patients infected with SARS-CoV-2, according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement [147]. The systematic review protocol was registered in PROSPERO with the number CRD42022317998. The PICO components sought information regarding adult patients with confirmed SARS-CoV-2 infection, preferring severe or advanced stage of compromise. The selected intervention was the use of biologics, according to the regulatory definition adopted by the “U.S. Food and drug administration” (FDA) prior to the modification “Consolidated Appropriations Act, 2020” that was implemented on 20 December 2019. This was a modification to the norm contemplated in the act: “Biologics Price Competition and Innovation Act of 2009 (BPCI Act)” implemented that year. We chose this definition, taking into account that is aligned with the objective of analyzing the therapies with greater specificity that can bring a benefit to the critically ill patient with COVID-19. Considering that the modification of the end of 2019 allows the inclusion of any chemically synthesized polypeptide and not exclusively of synthesis mediated by cells, tissues, or microorganisms.
Regarding the outcomes for the search, we prioritized any record depicting overall mortality due to SARS-CoV-2 and fatality rates regardless of the nature of primary or secondary outcomes. We also considered time to discharge, risk of mechanical ventilation, and surrogate biomarkers of efficacy.
We performed a search of the relevant bibliographic references through the following databases: Cochrane, Embase, Pubmed, Medline, medrxiv.org, and Google scholar. The search was performed with the following mesh terms: “COVID-19”, “SARS-CoV-2”, “Bio-logical Products”, “Interleukin 6 Receptor Antagonist Protein”, “Interleukin 1 Receptor Antagonist Protein”, “Mesenchymal Stem Cells”, “Mesenchymal Stem Cell Transplantation”, and “anti-spike monoclonal antibody”. We used these terms as exact phrases and a combination of subject headings according to databases syntax. We also performed a search with the most relevant drug names as mesh terms to complement the preliminary findings with the following terms: “Tocilizumab”, “Siltuximab”, “sarilumab”, “Anakinra”, “Canakinumab”, “Interferons” and “Mesenchymal Stem Cells”, “Bamlanivimab plus Etesevimab”, “Casirivimab/imdevimab”, “Bamlanivimab or Casirivimab/imdevimab”, and “Sotrovimab”. The recorded data were also expanded through the relevant references of selected literature on first search. No restriction in language was applied, and the research was performed from its inception until 11 January 2022 (Supplementary Information S1: Search constructs).
4.2. Study Selection, and Data Extraction
Once the search was carried out (M.A.), two independent researchers made a preliminary selection of the studies (H.O. and R-H.B). The selection was based on the titles and abstracts, considering the inclusion and exclusion criteria. If the researchers for the selection of a publication reached no consensus, the decision rested in the criteria of a third evaluator.
In a second stage, we applied the following inclusion criteria: full text studies, review articles, observational studies, meta-analysis, or clinical trials investigating the use of a biological drugs, with the intention of reducing mortality in patients infected by SARS-CoV-2; studies investigating the use of a biological drug with the intention of reducing the stay in the intensive care unit; studies investigating efficacy biomarker outcomes in severe or advanced COVID-19 patients.
We also applied the following exclusion criteria: studies that do not use biological drugs; studies that refer exclusively to anticoagulation methods as an exclusive intervention, even if it is done with drugs that are included in the biological category; studies related to vaccination, even if it is done with drugs that are included in the biological category; case report studies or series of cases studies and studies performed in other populations outside adults.
Finally, we performed a descriptive analysis of the literature found in the research and synthetized in the adjunct table (Table 1). For the review of articles in full text, the following information was taken into account: type of study, drug, therapeutic target, sample size (n), dose, and clinical outcome. All the papers found were collected in RAYYAN®. EndNote X9 has been used to keep track of references. In this table, we included all the studies except meta-analysis since we chose to list the included studies in each compilation article as raw data. The meta-analysis was referenced and described in the result section in each target. In addition, to avoid publication bias we performed an additional search of unpublished and gray literature in the specified databases for this purpose, such as medrxiv.org and Google scholar.
For observational case-control and cohort studies, Risk Of Bias In Non-Randomized Studies—of Interventions (ROBINS-I) have been used. For clinical trials, the Cochrane risk-of-bias tool for randomized trials (RoB 2) have been used. These tools were applied by two researchers independently. Discrepancies have been resolved by consensus. Studies were stratified according to quality (high risk of bias and low risk of bias), to perform a sensitivity analysis.
5. Conclusions
Finally, in conclusion of each case:
Il 6 inhibitors: This pharmacological target has the most amount of accumulated evidence available. We cannot ignore the fact that even with all the limitations mentioned before, most of the point estimators regarding disease resolution, mortality, and mechanical ventilation used tend to favor the intervention in this target. No generalization can be made regarding the use of these pharmacological alternatives since the heterogeneity of the data is high with several studies without statistical significance and a fair number of studies that show no difference with the intervention. We encourage more data recollection with randomized clinical trials, with larger samples, and controlling prognosis factors (i.e., with tools, such as the Charlson score index). The standardization of treatment regimens is needed to accumulate consistent data.
Il 1 inhibitors: The compiled data shows less heterogeneity compared with the Il 6 inhibitors. Most of the point estimators favor this pharmacological group, without overlooking the fact that some of the data are not statistically significant. The number of records and the small samples suggest the need of larger randomized trials, despite the encouraging results. The standardization of treatment regimens is needed to accumulate consistent data.
Interferons: In this group most of the estimators related to death or disease deterioration showed good responses to the intervention, nevertheless, we must stress that half of the data use surrogate or descriptive outcomes and the availability of records within the criteria gives a very small sample. Regardless of the methodology, more data are needed to conclude in this target.
Mesenchymal stem cells: This biological has less data available regarding its efficacy with the studies with the smallest of samples. The descriptive nature of biomarkers as surrogate primary endpoints is widespread amongst the studies. We speculate that the availability and logistical challenges in this matter may limit the number of studies to be performed in the future. Furthermore, even if the results reflected encouraging data the possibility of widespread use in certain countries may limit its implementation.
Anti-spike antibodies: In the case of anti-spike antibodies, the improvement in clinical outcomes in patients with COVID-19 is obtained in seronegative patients. Serological tests are decisive, since otherwise the benefit of these antibodies would be very low. Many questions remain to be answered with the use of anti-spike antibodies in the prevention of clinical outcomes in this type of patient and the interaction of the antibodies with the immune response produced by the vaccines against COVID-19. There is still a need to collect information on the safety and efficacy of these anti-spike antibodies and to have evidence of the influence of virus variants on the clinical response of these antibodies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ph15070783/s1, S1: Search constructs, Figure S1: Meta-analysis of the studies that determined mortality with Tocilizumab vs standard therapy.
Author Contributions
Conceptualization, M.A., R.-H.B. and H.O.; methodology, M.A., R.-H.B. and H.O.; validation, M.A., R.-H.B. and H.O.; formal analysis, M.A.; investigation, M.A., S.L.; resources, M.A.; data curation, M.A., R.-H.B. and H.O.; writing—original draft preparation, M.A., S.L.; writing—review and editing, M.A., S.L., R.-H.B. and H.O.; supervision, R.-H.B. and H.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available in article and supplementary material.
Acknowledgments
We would like to thank the Universidad de La Sabana.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Carlos, W.G.; Dela Cruz, C.S.; Cao, B.; Pasnick, S.; Jamil, S. Novel Wuhan (2019-nCoV) Coronavirus. Am. J. Respir. Crit. Care Med. 2020, 201, 7–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dos Santos, W.G. Natural history of COVID-19 and current knowledge on treatment therapeutic options. Biomed. Pharmacother. Biomed. Pharmacother. 2020, 129, 110493. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. COVID-19 Weekly Epidemiological Update. Available online: https://www.who.int/publications/m/item/covid-19-weekly-epidemiological-update (accessed on 15 October 2021).
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. Jama 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Golden, P.; Hennessey, E. Naming of Biological Products. U.S. Pharm. 2020, 45, 33–36. [Google Scholar]
- Food and Drug Administration. Definition of the Term “Biological Product”. Fed. Regist. 2020, 85, 10057–10063. [Google Scholar]
- Park, R.; Wurzburg, J.; Faccenda, M. FDA Final Rule Amends Definition of “Biological Product”. Available online: https://www.thehealthlawpulse.com/2020/03/fda-final-rule-amends-definition-of-biological-product/#:~:text=Under%20the%20final%20rule%2C%20the,are%20regulated%20as%20drugs%20or (accessed on 3 June 2022).
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. Jama 2020, 324, 782–793. [Google Scholar] [CrossRef]
- Yuki, K.; Fujiogi, M.; Koutsogiannaki, S. COVID-19 pathophysiology: A review. Clin. Immunol. 2020, 215, 108427. [Google Scholar] [CrossRef]
- Walls, A.C.; Park, Y.J.; Tortorici, M.A.; Wall, A.; McGuire, A.T.; Veesler, D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 2020, 181, 281–292.e286. [Google Scholar] [CrossRef]
- Zou, X.; Chen, K.; Zou, J.; Han, P.; Hao, J.; Han, Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front. Med. 2020, 14, 185–192. [Google Scholar] [CrossRef] [Green Version]
- Cornillez-Ty, C.T.; Liao, L.; Yates, J.R., 3rd; Kuhn, P.; Buchmeier, M.J. Severe acute respiratory syndrome coronavirus nonstructural protein 2 interacts with a host protein complex involved in mitochondrial biogenesis and intracellular signaling. J. Virol. 2009, 83, 10314–10318. [Google Scholar] [CrossRef] [Green Version]
- Cottam, E.M.; Whelband, M.C.; Wileman, T. Coronavirus NSP6 restricts autophagosome expansion. Autophagy 2014, 10, 1426–1441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hackbart, M.; Deng, X.; Baker, S.C. Coronavirus endoribonuclease targets viral polyuridine sequences to evade activating host sensors. Proc. Natl. Acad. Sci. USA 2020, 117, 8094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, C.; Lokugamage, K.G.; Rozovics, J.M.; Narayanan, K.; Semler, B.L.; Makino, S. SARS coronavirus nsp1 protein induces template-dependent endonucleolytic cleavage of mRNAs: Viral mRNAs are resistant to nsp1-induced RNA cleavage. PLoS Pathog. 2011, 7, e1002433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ivanov, K.A.; Thiel, V.; Dobbe, J.C.; van der Meer, Y.; Snijder, E.J.; Ziebuhr, J. Multiple enzymatic activities associated with severe acute respiratory syndrome coronavirus helicase. J. Virol. 2004, 78, 5619–5632. [Google Scholar] [CrossRef] [Green Version]
- Ma, Y.; Wu, L.; Shaw, N.; Gao, Y.; Wang, J.; Sun, Y.; Lou, Z.; Yan, L.; Zhang, R.; Rao, Z. Structural basis and functional analysis of the SARS coronavirus nsp14–nsp10 complex. Proc. Natl. Acad. Sci. USA 2015, 112, 9436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakai, Y.; Kawachi, K.; Terada, Y.; Omori, H.; Matsuura, Y.; Kamitani, W. Two-amino acids change in the nsp4 of SARS coronavirus abolishes viral replication. Virology 2017, 510, 165–174. [Google Scholar] [CrossRef]
- te Velthuis, A.J.; van den Worm, S.H.; Snijder, E.J. The SARS-coronavirus nsp7+nsp8 complex is a unique multimeric RNA polymerase capable of both de novo initiation and primer extension. Nucleic Acids Res. 2012, 40, 1737–1747. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Sun, Y.; Wu, A.; Xu, S.; Pan, R.; Zeng, C.; Jin, X.; Ge, X.; Shi, Z.; Ahola, T.; et al. Coronavirus nsp10/nsp16 Methyltransferase Can Be Targeted by nsp10-Derived Peptide In Vitro and In Vivo To Reduce Replication and Pathogenesis. J. Virol. 2015, 89, 8416–8427. [Google Scholar] [CrossRef] [Green Version]
- Fujimoto, I.; Pan, J.; Takizawa, T.; Nakanishi, Y. Virus clearance through apoptosis-dependent phagocytosis of influenza A virus-infected cells by macrophages. J. Virol. 2000, 74, 3399–3403. [Google Scholar] [CrossRef] [Green Version]
- Channappanavar, R.; Zhao, J.; Perlman, S. T cell-mediated immune response to respiratory coronaviruses. Immunol. Res. 2014, 59, 118–128. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Y.; Fu, B.; Zheng, X.; Wang, D.; Zhao, C.; Qi, Y.; Sun, R.; Tian, Z.; Xu, X.; Wei, H. Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients. Natl. Sci. Rev. 2020, 7, 998–1002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qin, C.; Zhou, L.; Hu, Z.; Zhang, S.; Yang, S.; Tao, Y.; Xie, C.; Ma, K.; Shang, K.; Wang, W.; et al. Dysregulation of Immune Response in Patients with Coronavirus 2019 (COVID-19) in Wuhan, China. Clin. Infect. Dis. 2020, 71, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Gong, E.; Zhang, B.; Zheng, J.; Gao, Z.; Zhong, Y.; Zou, W.; Zhan, J.; Wang, S.; Xie, Z.; et al. Multiple organ infection and the pathogenesis of SARS. J. Exp. Med. 2005, 202, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Capra, R.; De Rossi, N.; Mattioli, F.; Romanelli, G.; Scarpazza, C.; Sormani, M.P.; Cossi, S. Impact of low dose tocilizumab on mortality rate in patients with COVID-19 related pneumonia. Eur. J. Intern. Med. 2020, 76, 31–35. [Google Scholar] [CrossRef]
- Colaneri, M.; Bogliolo, L.; Valsecchi, P.; Sacchi, P.; Zuccaro, V.; Brandolino, F.; Montecucco, C.; Mojoli, F.; Giusti, E.M.; Bruno, R.; et al. Tocilizumab for Treatment of Severe COVID-19 Patients: Preliminary Results from SMAtteo COvid19 REgistry (SMACORE). Microorganisms 2020, 8, 695. [Google Scholar] [CrossRef]
- Klopfenstein, T.; Zayet, S.; Lohse, A.; Balblanc, J.C.; Badie, J.; Royer, P.Y.; Toko, L.; Mezher, C.; Kadiane-Oussou, N.J.; Bossert, M.; et al. Tocilizumab therapy reduced intensive care unit admissions and/or mortality in COVID-19 patients. Med. Mal. Infect. 2020, 50, 397–400. [Google Scholar] [CrossRef]
- Quartuccio, L.; Sonaglia, A.; McGonagle, D.; Fabris, M.; Peghin, M.; Pecori, D.; De Monte, A.; Bove, T.; Curcio, F.; Bassi, F.; et al. Profiling COVID-19 pneumonia progressing into the cytokine storm syndrome: Results from a single Italian Centre study on tocilizumab versus standard of care. J. Clin. Virol. 2020, 129, 104444. [Google Scholar] [CrossRef]
- Ramaswamy, M.; Mannam, P.; Comer, R.; Sinclair, E.; McQuaid, D.B.; Schmidt, M.L. Off-Label Real World Experience Using Tocilizumab for Patients Hospitalized with COVID-19 Disease in a Regional Community Health System: A Case-Control Study. medRxiv 2020. [Google Scholar] [CrossRef]
- Roumier, M.; Paule, R.; Groh, M.; Vallée, A.; Ackermann, F.; for the Foch, C.-S.G. Interleukin-6 blockade for severe COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Wadud, N.; Ahmed, N.; Shergil, M.; Khan, M.; Krishna, M.; Gilani, A.; Zarif, S.E.; Galaydick, J.; Linga, K.; Koor, S.; et al. Improved survival outcome in SARs-CoV-2 (COVID-19) Acute Respiratory Distress Syndrome patients with Tocilizumab administration. medRxiv 2020. [Google Scholar] [CrossRef]
- Alattar, R.; Ibrahim, T.B.H.; Shaar, S.H.; Abdalla, S.; Shukri, K.; Daghfal, J.N.; Khatib, M.Y.; Aboukamar, M.; Abukhattab, M.; Alsoub, H.A.; et al. Tocilizumab for the treatment of severe coronavirus disease 2019. J. Med. Virol. 2020, 92, 2042–2049. [Google Scholar] [CrossRef] [PubMed]
- Campochiaro, C.; Della-Torre, E.; Cavalli, G.; De Luca, G.; Ripa, M.; Boffini, N.; Tomelleri, A.; Baldissera, E.; Rovere-Querini, P.; Ruggeri, A.; et al. Efficacy and safety of tocilizumab in severe COVID-19 patients: A single-centre retrospective cohort study. Eur. J. Intern. Med. 2020, 76, 43–49. [Google Scholar] [CrossRef]
- Guaraldi, G.; Meschiari, M.; Cozzi-Lepri, A.; Milic, J.; Tonelli, R.; Menozzi, M.; Franceschini, E.; Cuomo, G.; Orlando, G.; Borghi, V.; et al. Tocilizumab in patients with severe COVID-19: A retrospective cohort study. Lancet Rheumatol. 2020, 2, e474–e484. [Google Scholar] [CrossRef]
- Kewan, T.; Covut, F.; Al-Jaghbeer, M.J.; Rose, L.; Gopalakrishna, K.V.; Akbik, B. Tocilizumab for treatment of patients with severe COVID-19: A retrospective cohort study. EClinicalMedicine 2020, 24, 100418. [Google Scholar] [CrossRef] [PubMed]
- Luo, P.; Liu, Y.; Qiu, L.; Liu, X.; Liu, D.; Li, J. Tocilizumab treatment in COVID-19: A single center experience. J. Med. Virol. 2020, 92, 814–818. [Google Scholar] [CrossRef] [PubMed]
- Morena, V.; Milazzo, L.; Oreni, L.; Bestetti, G.; Fossali, T.; Bassoli, C.; Torre, A.; Cossu, M.V.; Minari, C.; Ballone, E.; et al. Off-label use of tocilizumab for the treatment of SARS-CoV-2 pneumonia in Milan, Italy. Eur. J. Intern. Med. 2020, 76, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Price, C.C.; Altice, F.L.; Shyr, Y.; Koff, A.; Pischel, L.; Goshua, G.; Azar, M.M.; McManus, D.; Chen, S.C.; Gleeson, S.E.; et al. Tocilizumab Treatment for Cytokine Release Syndrome in Hospitalized Patients with Coronavirus Disease 2019: Survival and Clinical Outcomes. Chest 2020, 158, 1397–1408. [Google Scholar] [CrossRef]
- Sciascia, S.; Aprà, F.; Baffa, A.; Baldovino, S.; Boaro, D.; Boero, R.; Bonora, S.; Calcagno, A.; Cecchi, I.; Cinnirella, G.; et al. Pilot prospective open, single-arm multicentre study on off-label use of tocilizumab in patients with severe COVID-19. Clin. Exp. Rheumatol. 2020, 38, 529–532. [Google Scholar]
- Toniati, P.; Piva, S.; Cattalini, M.; Garrafa, E.; Regola, F.; Castelli, F.; Franceschini, F.; Airò, P.; Bazzani, C.; Beindorf, E.A.; et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: A single center study of 100 patients in Brescia, Italy. Autoimmun. Rev. 2020, 19, 102568. [Google Scholar] [CrossRef]
- Xu, X.; Han, M.; Li, T.; Sun, W.; Wang, D.; Fu, B.; Zhou, Y.; Zheng, X.; Yang, Y.; Li, X.; et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc. Natl. Acad. Sci. USA 2020, 117, 10970. [Google Scholar] [CrossRef]
- Fomina, D.S.; Lysenko, M.A.; Beloglazova, I.P.; Mutovina, Z.Y.; Poteshkina, N.G.; Samsonova, I.V.; Kruglova, T.S.; Chernov, A.A.; Karaulov, A.V. Temporal Clinical and Laboratory Response to Interleukin-6 Receptor Blockade with Tocilizumab in 89 Hospitalized Patients With COVID-19 Pneumonia. Pathog. Immun. 2020, 5, 327–341. [Google Scholar] [CrossRef] [PubMed]
- Górgolas Hernández-Mora, M.; Cabello Úbeda, A.; Prieto-Pérez, L.; Villar Álvarez, F.; Álvarez Álvarez, B.; Rodríguez Nieto, M.J.; Carrillo Acosta, I.; Fernández Ormaechea, I.; Al-Hayani, A.W.M.; Carballosa, P.; et al. Compassionate use of tocilizumab in severe SARS-CoV2 pneumonia. Int. J. Infect. Dis. 2021, 102, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Ip, A.; Berry, D.A.; Hansen, E.; Goy, A.H.; Pecora, A.L.; Sinclaire, B.A.; Bednarz, U.; Marafelias, M.; Berry, S.M.; Berry, N.S.; et al. Hydroxychloroquine and tocilizumab therapy in COVID-19 patients—An observational study. PLoS ONE 2020, 15, e0237693. [Google Scholar] [CrossRef]
- Kimmig, L.M.; Wu, D.; Gold, M.; Pettit, N.N.; Pitrak, D.; Mueller, J.; Husain, A.N.; Mutlu, E.A.; Mutlu, G.M. IL-6 Inhibition in Critically Ill COVID-19 Patients Is Associated with Increased Secondary Infections. Front. Med. 2020, 7, 583897. [Google Scholar] [CrossRef]
- Martínez-Sanz, J.; Muriel, A.; Ron, R.; Herrera, S.; Pérez-Molina, J.A.; Moreno, S.; Serrano-Villar, S. Effects of tocilizumab on mortality in hospitalized patients with COVID-19: A multicentre cohort study. Clin. Microbiol. Infect. 2021, 27, 238–243. [Google Scholar] [CrossRef]
- Moreno-García, E.; Rico, V.; Albiach, L.; Agüero, D.; Ambrosioni, J.; Bodro, M.; Cardozo, C.; Chumbita, M.; De la Mora, L.; García-Pouton, N.; et al. Tocilizumab is associated with reduced risk of ICU admission and mortality in patients with SARS-CoV-2 infection. medRxiv 2020. [Google Scholar] [CrossRef]
- Perrone, F.; Piccirillo, M.C.; Ascierto, P.A.; Salvarani, C.; Parrella, R.; Marata, A.M.; Popoli, P.; Ferraris, L.; Marrocco-Trischitta, M.M.; Ripamonti, D.; et al. Tocilizumab for patients with COVID-19 pneumonia. The single-arm TOCIVID-19 prospective trial. J. Transl. Med. 2020, 18, 405. [Google Scholar] [CrossRef]
- Petrak, R.M.; Skorodin, N.C.; Van Hise, N.W.; Fliegelman, R.M.; Pinsky, J.; Didwania, V.; Anderson, M.; Diaz, M.; Shah, K.; Chundi, V.V.; et al. Tocilizumab as a Therapeutic Agent for Critically Ill Patients Infected with SARS-CoV-2. Clin. Transl. Sci. 2021, 14, 2146–2151. [Google Scholar] [CrossRef]
- Rossi, B.; Nguyen, L.S.; Zimmermann, P.; Boucenna, F.; Dubret, L.; Baucher, L.; Guillot, H.; Bouldouyre, M.A.; Allenbach, Y.; Salem, J.E.; et al. Effect of Tocilizumab in Hospitalized Patients with Severe COVID-19 Pneumonia: A Case-Control Cohort Study. Pharmaceuticals 2020, 13, 317. [Google Scholar] [CrossRef]
- Sánchez-Montalvá, A.; Sellarés-Nadal, J.; Espinosa-Pereiro, J.; Fernández-Hidalgo, N.; Pérez-Hoyos, S.; Salvador, F.; Durà, X.; Miarons, M.; Antón, A.; Eremiev-Eremiev, S.; et al. Early outcomes of tocilizumab in adults hospitalized with severe COVID-19 - The Vall d’Hebron COVID-19 prospective cohort study. medRxiv 2020. [Google Scholar] [CrossRef]
- Somers, E.C.; Eschenauer, G.A.; Troost, J.P.; Golob, J.L.; Gandhi, T.N.; Wang, L.; Zhou, N.; Petty, L.A.; Baang, J.H.; Dillman, N.O.; et al. Tocilizumab for Treatment of Mechanically Ventilated Patients With COVID-19. Clin. Infect. Dis. 2021, 73, e445–e454. [Google Scholar] [CrossRef] [PubMed]
- Sabbatinelli, J.; Giuliani, A.; Matacchione, G.; Latini, S.; Laprovitera, N.; Pomponio, G.; Ferrarini, A.; Svegliati Baroni, S.; Pavani, M.; Moretti, M.; et al. Decreased serum levels of the inflammaging marker miR-146a are associated with clinical non-response to tocilizumab in COVID-19 patients. Mech. Ageing Dev. 2021, 193, 111413. [Google Scholar] [CrossRef] [PubMed]
- Hermine, O.; Mariette, X.; Tharaux, P.L.; Resche-Rigon, M.; Porcher, R.; Ravaud, P. Effect of Tocilizumab vs Usual Care in Adults Hospitalized with COVID-19 and Moderate or Severe Pneumonia: A Randomized Clinical Trial. JAMA Intern. Med. 2021, 181, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Salvarani, C.; Dolci, G.; Massari, M.; Merlo, D.F.; Cavuto, S.; Savoldi, L.; Bruzzi, P.; Boni, F.; Braglia, L.; Turrà, C.; et al. Effect of Tocilizumab vs Standard Care on Clinical Worsening in Patients Hospitalized with COVID-19 Pneumonia: A Randomized Clinical Trial. JAMA Intern. Med. 2021, 181, 24–31. [Google Scholar] [CrossRef]
- Malekzadeh, R.; Abedini, A.; Mohsenpour, B.; Sharifipour, E.; Ghasemian, R.; Javad-Mousavi, S.A.; Khodashahi, R.; Darban, M.; Kalantari, S.; Abdollahi, N.; et al. Subcutaneous tocilizumab in adults with severe and critical COVID-19: A prospective open-label uncontrolled multicenter trial. Int. Immunopharmacol. 2020, 89, 107102. [Google Scholar] [CrossRef]
- Dastan, F.; Saffaei, A.; Haseli, S.; Marjani, M.; Moniri, A.; Abtahian, Z.; Abedini, A.; Kiani, A.; Seifi, S.; Jammati, H.; et al. Promising effects of tocilizumab in COVID-19: A non-controlled, prospective clinical trial. Int. Immunopharmacol. 2020, 88, 106869. [Google Scholar] [CrossRef]
- Rodríguez-Molinero, A.; Pérez-López, C.; Gálvez-Barrón, C.; Miñarro, A.; Macho, O.; López, G.F.; Robles, M.T.; Dapena, M.D.; Martínez, S.; Rodríguez, E.; et al. Matched cohort study on the efficacy of tocilizumab in patients with COVID-19. One Health 2021, 12, 100214. [Google Scholar] [CrossRef]
- Vela, D.; Vela-Gaxha, Z.; Rexhepi, M.; Olloni, R.; Hyseni, V.; Nallbani, R. Efficacy and safety of tocilizumab versus standard care/placebo in patients with COVID-19; a systematic review and meta-analysis of randomized clinical trials. Br. J. Clin. Pharmacol. 2022, 88, 1955–1963. [Google Scholar] [CrossRef]
- Duarte-Millán, M.A.; Mesa-Plaza, N.; Guerrero-Santillán, M.; Morales-Ortega, A.; Bernal-Bello, D.; Farfán-Sedano, A.I.; García de Viedma-García, V.; Velázquez-Ríos, L.; Frutos-Pérez, B.; De Ancos-Aracil, C.L.; et al. Prognostic factors and combined use of tocilizumab and corticosteroids in a Spanish cohort of elderly COVID-19 patients. J. Med. Virol. 2022, 94, 1540–1549. [Google Scholar] [CrossRef]
- Moosazadeh, M.; Mousavi, T. Combination therapy of tocilizumab and steroid for COVID-19 patients: A meta-analysis. J. Med. Virol. 2022, 94, 1350–1356. [Google Scholar] [CrossRef]
- Martínez-Guerra, B.A.; de-León-Cividanes, N.A.; Tamez-Torres, K.M.; Román-Montes, C.M.; Rajme-López, S.; Ortiz-Brizuela, E.; Aguilar-Salinas, C.A.; Sierra-Madero, J.; Sifuentes-Osornio, J.; Ponce-de-León, A.; et al. Effect of Tocilizumab in Mortality among Patients with Severe and Critical COVID-19: Experience in a Third-Level Medical Center. Rev. Investig. Clin. Organo Hosp. Enferm. Nutr. 2022, 74, 40–50. [Google Scholar] [CrossRef] [PubMed]
- AlQahtani, H.; AlBilal, S.; Mahmoud, E.; Aldibasi, O.; Alharbi, A.; Shamas, N.; Alsaedy, A.; Owaidah, K.; Alqahtani, F.Y.; Aleanizy, F.S.; et al. Outcomes associated with tocilizumab with or without corticosteroid versus dexamethasone for treatment of patients with severe to critical COVID-19 pneumonia. J. Infect. Public Health 2022, 15, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Mushtaq, M.Z.; Mahmood, S.B.Z.; Almas, A.; Ather Wasti, S.; Ahsan Ali, S. Tocilizumab in critically ill COVID-19 patients: An observational study. Int. Immunopharmacol. 2022, 102, 108384. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.N.; Hernández-Sánchez, J.; Nagel, S.; Feng, Y.; Cai, F.; Rabin, J.; Morse, C.G.; Nadig, N.R.; Ashraf, O.; Gotur, D.B.; et al. Safety and Efficacy of Tocilizumab 4 or 8 mg/kg in Hospitalized Patients with Moderate to Severe Coronavirus Disease 2019 Pneumonia: A Randomized Clinical Trial. Open Forum Infect. Dis. 2021, 9, ofab608. [Google Scholar] [CrossRef] [PubMed]
- Çelik Ekinci, S.; Akkaya Işık, S. A retrospective evaluation of COVID-19 patients treated with Tocilizumab: Who should be treated? J. Infect. Dev. Ctries. 2021, 15, 1825–1832. [Google Scholar] [CrossRef]
- Karampitsakos, T.; Malakounidou, E.; Papaioannou, O.; Dimakopoulou, V.; Zarkadi, E.; Katsaras, M.; Tsiri, P.; Tsirikos, G.; Georgiopoulou, V.; Oikonomou, I.; et al. Tocilizumab improves 28-day survival in hospitalized patients with severe COVID-19: An open label, prospective study. Respir. Res. 2021, 22, 317. [Google Scholar] [CrossRef]
- Naik, N.B.; Puri, G.D.; Kajal, K.; Mahajan, V.; Bhalla, A.; Kataria, S.; Singla, K.; Panigrahi, P.; Singh, A.; Lazar, M.; et al. High-Dose Dexamethasone Versus Tocilizumab in Moderate to Severe COVID-19 Pneumonia: A Randomized Controlled Trial. Cureus 2021, 13, e20353. [Google Scholar] [CrossRef]
- Abdelnaby, H.; Aboelhassan, W.; Al-Jarallah, M.; Rajan, R.; Dashti, R.; Zhanna, K.D.; Alsaber, A.R.; Abd El-Aleem, A.; Ashry, I.; Abdullah, M.; et al. Outcomes of tocilizumab therapy in severe or critical COVID-19 patients: A retrospective cohort, single-centre study. Trop. Med. Int. Health 2021, 26, 1689–1699. [Google Scholar] [CrossRef]
- Gritti, G.; Raimondi, F.; Ripamonti, D.; Riva, I.; Landi, F.; Alborghetti, L.; Frigeni, M.; Damiani, M.; Micò, C.; Fagiuoli, S.; et al. IL-6 signalling pathway inactivation with siltuximab in patients with COVID-19 respiratory failure: An observational cohort study. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Della-Torre, E.; Campochiaro, C.; Cavalli, G.; De Luca, G.; Napolitano, A.; La Marca, S.; Boffini, N.; Da Prat, V.; Di Terlizzi, G.; Lanzillotta, M.; et al. Interleukin-6 blockade with sarilumab in severe COVID-19 pneumonia with systemic hyperinflammation: An open-label cohort study. Ann. Rheum. Dis. 2020, 79, 1277–1285. [Google Scholar] [CrossRef]
- The Remap-CAP Investigators; Gordon, A.C.; Mouncey, P.R.; Al-Beidh, F.; Rowan, K.M.; Nichol, A.D.; Arabi, Y.M.; Annane, D.; Beane, A.; van Bentum-Puijk, W.; et al. Interleukin-6 Receptor Antagonists in Critically Ill Patients with COVID-19—Preliminary report. medRxiv 2021. [Google Scholar] [CrossRef]
- Gremese, E.; Cingolani, A.; Bosello, S.L.; Alivernini, S.; Tolusso, B.; Perniola, S.; Landi, F.; Pompili, M.; Murri, R.; Santoliquido, A.; et al. Sarilumab use in severe SARS-CoV-2 pneumonia. EClinicalMedicine 2020, 27, 100553. [Google Scholar] [CrossRef]
- Cauchois, R.; Koubi, M.; Delarbre, D.; Manet, C.; Carvelli, J.; Blasco, V.B.; Jean, R.; Fouche, L.; Bornet, C.; Pauly, V.; et al. Early IL-1 receptor blockade in severe inflammatory respiratory failure complicating COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 18951–18953. [Google Scholar] [CrossRef]
- Huet, T.; Beaussier, H.; Voisin, O.; Jouveshomme, S.; Dauriat, G.; Lazareth, I.; Sacco, E.; Naccache, J.M.; Bézie, Y.; Laplanche, S.; et al. Anakinra for severe forms of COVID-19: A cohort study. Lancet. Rheumatol. 2020, 2, e393–e400. [Google Scholar] [CrossRef]
- CORIMUNO-19 Collaborative Group. Effect of anakinra versus usual care in adults in hospital with COVID-19 and mild-to-moderate pneumonia (CORIMUNO-ANA-1): A randomised controlled trial. Lancet Respir. Med. 2021, 9, 295–304. [Google Scholar] [CrossRef]
- Bozzi, G.; Mangioni, D.; Minoia, F.; Aliberti, S.; Grasselli, G.; Barbetta, L.; Castelli, V.; Palomba, E.; Alagna, L.; Lombardi, A.; et al. Anakinra combined with methylprednisolone in patients with severe COVID-19 pneumonia and hyperinflammation: An observational cohort study. J. Allergy Clin. Immunol. 2021, 147, 561–566. [Google Scholar] [CrossRef]
- Cavalli, G.; Larcher, A.; Tomelleri, A.; Campochiaro, C.; Della-Torre, E.; De Luca, G.; Farina, N.; Boffini, N.; Ruggeri, A.; Poli, A.; et al. Interleukin-1 and interleukin-6 inhibition compared with standard management in patients with COVID-19 and hyperinflammation: A cohort study. Lancet Rheumatol. 2021, 3, e253–e261. [Google Scholar] [CrossRef]
- Pontali, E.; Volpi, S.; Signori, A.; Antonucci, G.; Castellaneta, M.; Buzzi, D.; Montale, A.; Bustaffa, M.; Angelelli, A.; Caorsi, R.; et al. Efficacy of early anti-inflammatory treatment with high doses of intravenous anakinra with or without glucocorticoids in patients with severe COVID-19 pneumonia. J. Allergy Clin. Immunol. 2021, 147, 1217–1225. [Google Scholar] [CrossRef]
- Kooistra, E.J.; Waalders, N.J.B.; Grondman, I.; Janssen, N.A.F.; de Nooijer, A.H.; Netea, M.G.; van de Veerdonk, F.L.; Ewalds, E.; van der Hoeven, J.G.; Kox, M.; et al. Anakinra treatment in critically ill COVID-19 patients: A prospective cohort study. Crit. Care 2020, 24, 688. [Google Scholar] [CrossRef]
- Kyriazopoulou, E.; Panagopoulos, P.; Metallidis, S.; Dalekos, G.N.; Poulakou, G.; Gatselis, N.; Karakike, E.; Saridaki, M.; Loli, G.; Stefos, A.; et al. An open label trial of anakinra to prevent respiratory failure in COVID-19. eLife 2021, 10. [Google Scholar] [CrossRef]
- Balkhair, A.; Al-Zakwani, I.; Al Busaidi, M.; Al-Khirbash, A.; Al Mubaihsi, S.; BaTaher, H.; Al Aghbari, J.; Al Busaidi, I.; Al Kindi, M.; Baawain, S.; et al. Anakinra in hospitalized patients with severe COVID-19 pneumonia requiring oxygen therapy: Results of a prospective, open-label, interventional study. Int. J. Infect. Dis. 2021, 103, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Langer-Gould, A.; Smith, J.B.; Gonzales, E.G.; Castillo, R.D.; Figueroa, J.G.; Ramanathan, A.; Li, B.H.; Gould, M.K. Early identification of COVID-19 cytokine storm and treatment with anakinra or tocilizumab. Int. J. Infect. Dis. 2020, 99, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Iglesias-Julián, E.; López-Veloso, M.; de-la-Torre-Ferrera, N.; Barraza-Vengoechea, J.C.; Delgado-López, P.D.; Colazo-Burlato, M.; Ubeira-Iglesias, M.; Montero-Baladía, M.; Lorenzo-Martín, A.; Minguito-de-la-Iglesia, J.; et al. High dose subcutaneous Anakinra to treat acute respiratory distress syndrome secondary to cytokine storm syndrome among severely ill COVID-19 patients. J. Autoimmun. 2020, 115, 102537. [Google Scholar] [CrossRef] [PubMed]
- Borie, R.; Savale, L.; Dossier, A.; Ghosn, J.; Taillé, C.; Visseaux, B.; Jebreen, K.; Diallo, A.; Tesmoingt, C.; Morer, L.; et al. Glucocorticoids with low-dose anti-IL1 anakinra rescue in severe non-ICU COVID-19 infection: A cohort study. PLoS ONE 2020, 15, e0243961. [Google Scholar] [CrossRef] [PubMed]
- Kyriazopoulou, E.; Poulakou, G.; Milionis, H.; Metallidis, S.; Adamis, G.; Tsiakos, K.; Fragkou, A.; Rapti, A.; Damoulari, C.; Fantoni, M.; et al. Early treatment of COVID-19 with anakinra guided by soluble urokinase plasminogen receptor plasma levels: A double-blind, randomized controlled phase 3 trial. Nat. Med. 2021, 27, 1752–1760. [Google Scholar] [CrossRef]
- Franzetti, M.; Forastieri, A.; Borsa, N.; Pandolfo, A.; Molteni, C.; Borghesi, L.; Pontiggia, S.; Evasi, G.; Guiotto, L.; Erba, M.; et al. IL-1 Receptor Antagonist Anakinra in the Treatment of COVID-19 Acute Respiratory Distress Syndrome: A Retrospective, Observational Study. J. Immunol. 2021, 206, 1569. [Google Scholar] [CrossRef]
- Kharazmi, A.B.; Moradi, O.; Haghighi, M.; Kouchek, M.; Manafi-Rasi, A.; Raoufi, M.; Shoaei, S.D.; Hadavand, F.; Nabavi, M.; Miri, M.M.; et al. A randomized controlled clinical trial on efficacy and safety of anakinra in patients with severe COVID-19. Immun. Inflamm. Dis. 2022, 10, 201–208. [Google Scholar] [CrossRef]
- Landi, L.; Ravaglia, C.; Russo, E.; Cataleta, P.; Fusari, M.; Boschi, A.; Giannarelli, D.; Facondini, F.; Valentini, I.; Panzini, I.; et al. Blockage of interleukin-1β with canakinumab in patients with COVID-19. Sci. Rep. 2020, 10, 21775. [Google Scholar] [CrossRef]
- Katia, F.; Myriam, D.P.; Ucciferri, C.; Auricchio, A.; Di Nicola, M.; Marchioni, M.; Eleonora, C.; Emanuela, S.; Cipollone, F.; Vecchiet, J. Efficacy of canakinumab in mild or severe COVID-19 pneumonia. Immun. Inflamm. Dis. 2021, 9, 399–405. [Google Scholar] [CrossRef]
- Caricchio, R.; Abbate, A.; Gordeev, I.; Meng, J.; Hsue, P.Y.; Neogi, T.; Arduino, R.; Fomina, D.; Bogdanov, R.; Stepanenko, T.; et al. Effect of Canakinumab vs Placebo on Survival without Invasive Mechanical Ventilation in Patients Hospitalized with Severe COVID-19: A Randomized Clinical Trial. Jama 2021, 326, 230–239. [Google Scholar] [CrossRef]
- Generali, D.; Bosio, G.; Malberti, F.; Cuzzoli, A.; Testa, S.; Romanini, L.; Fioravanti, A.; Morandini, A.; Pianta, L.; Giannotti, G.; et al. Canakinumab as treatment for COVID-19-related pneumonia: A prospective case-control study. Int. J. Infect. Dis. 2021, 104, 433–440. [Google Scholar] [CrossRef]
- Davoudi-Monfared, E.; Rahmani, H.; Khalili, H.; Hajiabdolbaghi, M.; Salehi, M.; Abbasian, L.; Kazemzadeh, H.; Yekaninejad, M.S. A Randomized Clinical Trial of the Efficacy and Safety of Interferon β-1a in Treatment of Severe COVID-19. Antimicrob. Agents Chemother. 2020, 64, e01061-20. [Google Scholar] [CrossRef] [PubMed]
- Estébanez, M.; Ramírez-Olivencia, G.; Mata, T.; Martí, D.; Gutierrez, C.; de Dios, B.; Herrero, M.D.; Roel, A.; Martínez, Y.; Aguirre, A.; et al. Clinical evaluation of IFN beta1b in COVID-19 pneumonia: A retrospective study. medRxiv 2020. [Google Scholar] [CrossRef]
- Hung, I.F.; Lung, K.C.; Tso, E.Y.; Liu, R.; Chung, T.W.; Chu, M.Y.; Ng, Y.Y.; Lo, J.; Chan, J.; Tam, A.R.; et al. Triple combination of interferon beta-1b, lopinavir-ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: An open-label, randomised, phase 2 trial. Lancet 2020, 395, 1695–1704. [Google Scholar] [CrossRef]
- Pereda, R.; González, D.; Rivero, H.B.; Rivero, J.C.; Pérez, A.; López, L.D.R.; Mezquia, N.; Venegas, R.; Betancourt, J.R.; Domínguez, R.E. Therapeutic Effectiveness of Interferon-α2b Against COVID-19: The Cuban Experience. J. Interferon Cytokine Res. 2020, 40, 438–442. [Google Scholar] [CrossRef]
- Wang, N.; Zhan, Y.; Zhu, L.; Hou, Z.; Liu, F.; Song, P.; Qiu, F.; Wang, X.; Zou, X.; Wan, D.; et al. Retrospective Multicenter Cohort Study Shows Early Interferon Therapy Is Associated with Favorable Clinical Responses in COVID-19 Patients. Cell Host Microbe 2020, 28, 455–464.e452. [Google Scholar] [CrossRef]
- Zhou, Q.; Chen, V.; Shannon, C.P.; Wei, X.-S.; Xiang, X.; Wang, X.; Wang, Z.-H.; Tebbutt, S.J.; Kollmann, T.R.; Fish, E.N. Interferon-α2b Treatment for COVID-19. Front. Immunol. 2020, 11, 1061. [Google Scholar] [CrossRef]
- Rahmani, H.; Davoudi-Monfared, E.; Nourian, A.; Khalili, H.; Hajizadeh, N.; Jalalabadi, N.Z.; Fazeli, M.R.; Ghazaeian, M.; Yekaninejad, M.S. Interferon β-1b in treatment of severe COVID-19: A randomized clinical trial. Int. Immunopharmacol. 2020, 88, 106903. [Google Scholar] [CrossRef]
- Feld, J.J.; Kandel, C.; Biondi, M.J.; Kozak, R.A.; Zahoor, M.A.; Lemieux, C.; Borgia, S.M.; Boggild, A.K.; Powis, J.; McCready, J.; et al. Peginterferon lambda for the treatment of outpatients with COVID-19: A phase 2, placebo-controlled randomised trial. Lancet Respir. Med. 2021, 9, 498–510. [Google Scholar] [CrossRef]
- Qu, W.; Wang, Z.; Hare, J.M.; Bu, G.; Mallea, J.M.; Pascual, J.M.; Caplan, A.I.; Kurtzberg, J.; Zubair, A.C.; Kubrova, E.; et al. Cell-based therapy to reduce mortality from COVID-19: Systematic review and meta-analysis of human studies on acute respiratory distress syndrome. Stem Cells Transl. Med. 2020, 9, 1007–1022. [Google Scholar] [CrossRef]
- Leng, Z.; Zhu, R.; Hou, W.; Feng, Y.; Yang, Y.; Han, Q.; Shan, G.; Meng, F.; Du, D.; Wang, S.; et al. Transplantation of ACE2(-) Mesenchymal Stem Cells Improves the Outcome of Patients with COVID-19 Pneumonia. Aging Dis. 2020, 11, 216–228. [Google Scholar] [CrossRef] [Green Version]
- Shu, L.; Niu, C.; Li, R.; Huang, T.; Wang, Y.; Huang, M.; Ji, N.; Zheng, Y.; Chen, X.; Shi, L.; et al. Treatment of severe COVID-19 with human umbilical cord mesenchymal stem cells. Stem Cell Res. Ther. 2020, 11, 361. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Xu, R.; Wang, S.; Xu, Z.; Zhang, C.; Li, Y.; Yang, T.; Shi, L.; Fu, J.; Jiang, T.; et al. Human umbilical cord-derived mesenchymal stem cell therapy in patients with COVID-19: A phase 1 clinical trial. Signal Transduct. Target. Ther. 2020, 5, 172. [Google Scholar] [CrossRef]
- Armitage, J.; Tan, D.B.A.; Troedson, R.; Young, P.; Lam, K.-v.; Shaw, K.; Sturm, M.; Weiss, D.J.; Moodley, Y.P. Mesenchymal stromal cell infusion modulates systemic immunological responses in stable COPD patients: A phase I pilot study. Eur. Respir. J. 2018, 51, 1702369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, L.; Huang, H.; Lu, X.; Yan, X.; Jiang, X.; Xu, R.; Wang, S.; Zhang, C.; Yuan, X.; Xu, Z.; et al. Effect of human umbilical cord-derived mesenchymal stem cells on lung damage in severe COVID-19 patients: A randomized, double-blind, placebo-controlled phase 2 trial. Signal Transduct. Target. Ther. 2021, 6, 58. [Google Scholar] [CrossRef]
- Sengupta, V.; Sengupta, S.; Lazo, A.; Woods, P.; Nolan, A.; Bremer, N. Exosomes Derived from Bone Marrow Mesenchymal Stem Cells as Treatment for Severe COVID-19. Stem Cells Dev. 2020, 29, 747–754. [Google Scholar] [CrossRef]
- Chen, P.; Nirula, A.; Heller, B.; Gottlieb, R.L.; Boscia, J.; Morris, J.; Huhn, G.; Cardona, J.; Mocherla, B.; Stosor, V.; et al. SARS-CoV-2 Neutralizing Antibody LY-CoV555 in Outpatients with COVID-19. N. Engl. J. Med. 2021, 384, 229–237. [Google Scholar] [CrossRef]
- Dougan, M.; Nirula, A.; Azizad, M.; Mocherla, B.; Gottlieb, R.L.; Chen, P.; Hebert, C.; Perry, R.; Boscia, J.; Heller, B.; et al. Bamlanivimab plus Etesevimab in Mild or Moderate COVID-19. N. Engl. J. Med. 2021, 385, 1382–1392. [Google Scholar] [CrossRef]
- Xiang, H.R.; He, B.; Li, Y.; Cheng, X.; Zhang, Q.Z.; Peng, W.X. Bamlanivimab plus etesevimab treatment have a better outcome against COVID-19: A meta-analysis. J. Med. Virol. 2022, 94, 1893–1905. [Google Scholar] [CrossRef]
- Murchu, E.; Spillane, S.; Byrne, P.; O’Neill, M.; Harrington, P.; Ryan, M. Interventions in an Ambulatory Setting to Prevent Progression to Severe Disease in Patients with COVID-19: A Systematic Review. Ann. Pharmacother. 2022, 56, 309–318. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Randomised Evaluation of COVID-19 Therapy (RECOVERY). Available online: https://clinicaltrials.gov/ct2/show/record/NCT04381936 (accessed on 11 January 2022).
- ClinicalTrials.gov. COVID-19 Study Assessing the Efficacy and Safety of Anti-Spike SARS CoV-2 Monoclonal Antibodies for Prevention of SARS CoV-2 Infection Asymptomatic in Healthy Adults and Adolescents Who Are Household Contacts to an Individual with a Positive SARS-CoV-2 RT-PCR Assay. Available online: https://clinicaltrials.gov/ct2/show/NCT04452318 (accessed on 4 November 2021).
- Weinreich, D.M.; Sivapalasingam, S.; Norton, T.; Ali, S.; Gao, H.; Bhore, R.; Musser, B.J.; Soo, Y.; Rofail, D.; Im, J.; et al. REGN-COV2, a Neutralizing Antibody Cocktail, in Outpatients with COVID-19. N. Engl. J. Med. 2021, 384, 238–251. [Google Scholar] [CrossRef]
- O’Brien, M.P.; Forleo-Neto, E.; Musser, B.J.; Isa, F.; Chan, K.C.; Sarkar, N.; Bar, K.J.; Barnabas, R.V.; Barouch, D.H.; Cohen, M.S.; et al. Subcutaneous REGEN-COV Antibody Combination to Prevent COVID-19. N. Engl. J. Med. 2021, 385, 1184–1195. [Google Scholar] [CrossRef]
- Weinreich, D.M.; Sivapalasingam, S.; Norton, T.; Ali, S.; Gao, H.; Bhore, R.; Xiao, J.; Hooper, A.T.; Hamilton, J.D.; Musser, B.J.; et al. REGEN-COV Antibody Combination and Outcomes in Outpatients with COVID-19. N. Engl. J. Med. 2021, 385, e81. [Google Scholar] [CrossRef]
- Ganesh, R.; Philpot, L.M.; Bierle, D.M.; Anderson, R.J.; Arndt, L.L.; Arndt, R.F.; Culbertson, T.L.; Destro Borgen, M.J.; Hanson, S.N.; Kennedy, B.D.; et al. Real-World Clinical Outcomes of Bamlanivimab and Casirivimab-Imdevimab Among High-Risk Patients With Mild to Moderate Coronavirus Disease 2019. J. Infect. Dis. 2021, 224, 1278–1286. [Google Scholar] [CrossRef] [PubMed]
- Du, L.; Yang, Y.; Zhang, X. Neutralizing antibodies for the prevention and treatment of COVID-19. Cell Mol. Immunol. 2021, 18, 2293–2306. [Google Scholar] [CrossRef] [PubMed]
- Cardwell, K.; O Murchu, E.; Byrne, P.; Broderick, N.; Walsh, K.A.; O’Neill, S.M.; Smith, S.M.; Harrington, P.; Ryan, M.; O’Neill, M. Pharmacological interventions to prevent COVID-19 disease: A rapid review. Rev. Med. Virol. 2022, 32, e2299. [Google Scholar] [CrossRef]
- Verderese, J.P.; Stepanova, M.; Lam, B.; Racila, A.; Kolacevski, A.; Allen, D.; Hodson, E.; Aslani-Amoli, B.; Homeyer, M.; Stanmyre, S.; et al. Neutralizing Monoclonal Antibody Treatment Reduces Hospitalization for Mild and Moderate Coronavirus Disease 2019 (COVID-19): A Real-World Experience. Clin. Infect. Dis. 2022, 74, 1063–1069. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.J.; Banu, S.; Sasikala, M.; Parsa, K.V.L.; Sowpati, D.T.; Yadav, R.; Tallapaka, K.B.; Siva, A.B.; Vishnubhotla, R.; Rao, G.V.; et al. Effectiveness of REGEN-COV antibody cocktail against the B.1.617.2 (delta) variant of SARS-CoV-2: A cohort study. J. Intern. Med. 2022, 291, 380–383. [Google Scholar] [CrossRef] [PubMed]
- Mutoh, Y.; Umemura, T.; Ota, A.; Okuda, K.; Moriya, R.; Tago, M.; Soejima, K.; Noguchi, Y.; Bando, T.; Ota, S.; et al. Effectiveness of monoclonal antibody therapy for COVID-19 patients using a risk scoring system. J. Infect. Chemother. 2022, 28, 352–355. [Google Scholar] [CrossRef]
- Sakurai, A.; Marshall, S.; Ogasawara, T.; Ogasawara, T.; Aoka, Y.; Sakura, H.; Uchigata, Y.; Ogawa, T. REGN-COV2 antibody cocktail in patients with SARS-CoV-2: Observational study from a single institution in Japan. J. Infect. Chemother. 2022, 28, 943–947. [Google Scholar] [CrossRef]
- Falcone, M.; Tiseo, G.; Valoriani, B.; Barbieri, C.; Occhineri, S.; Mazzetti, P.; Vatteroni, M.L.; Suardi, L.R.; Riccardi, N.; Pistello, M.; et al. Efficacy of Bamlanivimab/Etesevimab and Casirivimab/Imdevimab in Preventing Progression to Severe COVID-19 and Role of Variants of Concern. Infect. Dis. Ther. 2021, 10, 2479–2488. [Google Scholar] [CrossRef]
- Razonable, R.R.; Pawlowski, C.; O’Horo, J.C.; Arndt, L.L.; Arndt, R.; Bierle, D.M.; Borgen, M.D.; Hanson, S.N.; Hedin, M.C.; Lenehan, P.; et al. Casirivimab-Imdevimab treatment is associated with reduced rates of hospitalization among high-risk patients with mild to moderate coronavirus disease-19. EClinicalMedicine 2021, 40, 101102. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Gonzalez-Rojas, Y.; Juarez, E.; Crespo Casal, M.; Moya, J.; Falci, D.R.; Sarkis, E.; Solis, J.; Zheng, H.; Scott, N.; et al. Early Treatment for COVID-19 with SARS-CoV-2 Neutralizing Antibody Sotrovimab. N. Engl. J. Med. 2021, 385, 1941–1950. [Google Scholar] [CrossRef] [PubMed]
- Kreuzberger, N.; Hirsch, C.; Chai, K.L.; Tomlinson, E.; Khosravi, Z.; Popp, M.; Neidhardt, M.; Piechotta, V.; Salomon, S.; Valk, S.J.; et al. SARS-CoV-2-neutralising monoclonal antibodies for treatment of COVID-19. Cochrane Database Syst. Rev. 2021, 9, CD013825. [Google Scholar] [CrossRef] [PubMed]
- ACTIV-3/Therapeutics for Inpatients with COVID-19 (TICO) Study Group. Efficacy and safety of two neutralising monoclonal antibody therapies, sotrovimab and BRII-196 plus BRII-198, for adults hospitalised with COVID-19 (TICO): A randomised controlled trial. Lancet Infect. Dis. 2022, 22, 622–635. [Google Scholar] [CrossRef]
- Siemieniuk, R.A.; Bartoszko, J.J.; Diaz Martinez, J.P.; Kum, E.; Qasim, A.; Zeraatkar, D.; Izcovich, A.; Mangala, S.; Ge, L.; Han, M.A.; et al. Antibody and cellular therapies for treatment of covid-19: A living systematic review and network meta-analysis. BMJ 2021, 374, n2231. [Google Scholar] [CrossRef]
- Aggarwal, N.R.; Beaty, L.E.; Bennett, T.D.; Carlson, N.E.; Davis, C.B.; Kwan, B.M.; Mayer, D.A.; Ong, T.C.; Russell, S.; Steele, J.; et al. Real World Evidence of the Neutralizing Monoclonal Antibody Sotrovimab for Preventing Hospitalization and Mortality in COVID-19 Outpatients. medRxiv 2022. [Google Scholar] [CrossRef]
- Chen, X.; Zhao, B.; Qu, Y.; Chen, Y.; Xiong, J.; Feng, Y.; Men, D.; Huang, Q.; Liu, Y.; Yang, B.; et al. Detectable Serum Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load (RNAemia) Is Closely Correlated with Drastically Elevated Interleukin 6 Level in Critically Ill Patients with Coronavirus Disease 2019. Clin. Infect. Dis. 2020, 71, 1937–1942. [Google Scholar] [CrossRef]
- Tay, M.Z.; Poh, C.M.; Rénia, L.; MacAry, P.A.; Ng, L.F.P. The trinity of COVID-19: Immunity, inflammation and intervention. Nat. Rev. Immunol. 2020, 20, 363–374. [Google Scholar] [CrossRef]
- Lan, S.H.; Lai, C.C.; Huang, H.T.; Chang, S.P.; Lu, L.C.; Hsueh, P.R. Tocilizumab for severe COVID-19: A systematic review and meta-analysis. Int. J. Antimicrob. Agents 2020, 56, 106103. [Google Scholar] [CrossRef]
- Cortegiani, A.; Ippolito, M.; Greco, M.; Granone, V.; Protti, A.; Gregoretti, C.; Giarratano, A.; Einav, S.; Cecconi, M. Rationale and evidence on the use of tocilizumab in COVID-19: A systematic review. Pulmonology 2021, 27, 52–66. [Google Scholar] [CrossRef]
- Rimland, C.A.; Morgan, C.E.; Bell, G.J.; Kim, M.K.; Hedrick, T.; Marx, A.; Bramson, B.; Swygard, H.; Napravnik, S.; Schmitz, J.L.; et al. Clinical characteristics and early outcomes in patients with COVID-19 treated with tocilizumab at a United States academic center. medRxiv 2020. [Google Scholar] [CrossRef]
- Khan, F.A.; Stewart, I.; Fabbri, L.; Moss, S.; Robinson, K.; Smyth, A.R.; Jenkins, G. Systematic review and meta-analysis of anakinra, sarilumab, siltuximab and tocilizumab for COVID-19. Thorax 2021, 76, 907–919. [Google Scholar] [CrossRef] [PubMed]
- Shakoory, B.; Carcillo, J.A.; Chatham, W.W.; Amdur, R.L.; Zhao, H.; Dinarello, C.A.; Cron, R.Q.; Opal, S.M. Interleukin-1 Receptor Blockade Is Associated with Reduced Mortality in Sepsis Patients with Features of Macrophage Activation Syndrome: Reanalysis of a Prior Phase III Trial. Crit. Care Med. 2016, 44, 275–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kyriazopoulou, E.; Huet, T.; Cavalli, G.; Gori, A.; Kyprianou, M.; Pickkers, P.; Eugen-Olsen, J.; Clerici, M.; Veas, F.; Chatellier, G.; et al. Effect of anakinra on mortality in patients with COVID-19: A systematic review and patient-level meta-analysis. Lancet Rheumatol. 2021, 3, e690–e697. [Google Scholar] [CrossRef]
- Ivashkiv, L.B.; Donlin, L.T. Regulation of type I interferon responses. Nat. Rev. Immunol. 2014, 14, 36–49. [Google Scholar] [CrossRef] [Green Version]
- MacMicking, J.D. Interferon-inducible effector mechanisms in cell-autonomous immunity. Nat. Rev. Immunol. 2012, 12, 367–382. [Google Scholar] [CrossRef]
- Walz, L.; Cohen, A.J.; Rebaza, A.P.; Vanchieri, J.; Slade, M.D.; Dela Cruz, C.S.; Sharma, L. JAK-inhibitor and type I interferon ability to produce favorable clinical outcomes in COVID-19 patients: A systematic review and meta-analysis. BMC Infect. Dis. 2021, 21, 47. [Google Scholar] [CrossRef]
- Hunt, C.L.; Her, Y.F.; Law, L.A.; Bydon, M.; Nassr, A.; Smith, J.; Mauck, W.D.; Eldrige, J.S.; Malanga, G.A.; Qu, W. Five generations of cell preparation: A translational framework for categorizing regenerative stem cell therapies. J. Am. Acad. Regen. Med. 2017, 1, 1. [Google Scholar] [CrossRef]
- Loy, H.; Kuok, D.I.T.; Hui, K.P.Y.; Choi, M.H.L.; Yuen, W.; Nicholls, J.M.; Peiris, J.S.M.; Chan, M.C.W. Therapeutic Implications of Human Umbilical Cord Mesenchymal Stromal Cells in Attenuating Influenza A(H5N1) Virus-Associated Acute Lung Injury. J. Infect. Dis. 2019, 219, 186–196. [Google Scholar] [CrossRef]
- Miguez-Rey, E.; Choi, D.; Kim, S.; Yoon, S.; Sandulescu, O. Monoclonal antibody therapies in the management of SARS-CoV-2 infection. Expert Opin. Investig. Drugs 2022, 31, 41–58. [Google Scholar] [CrossRef]
- Taylor, P.C.; Adams, A.C.; Hufford, M.M.; de la Torre, I.; Winthrop, K.; Gottlieb, R.L. Neutralizing monoclonal antibodies for treatment of COVID-19. Nat. Rev. Immunol. 2021, 21, 382–393. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).