Improved Database Filtering Technology Enables More Efficient Ab Initio Design of Potent Peptides against Ebola Viruses
Abstract
:1. Introduction
2. Results and Discussion
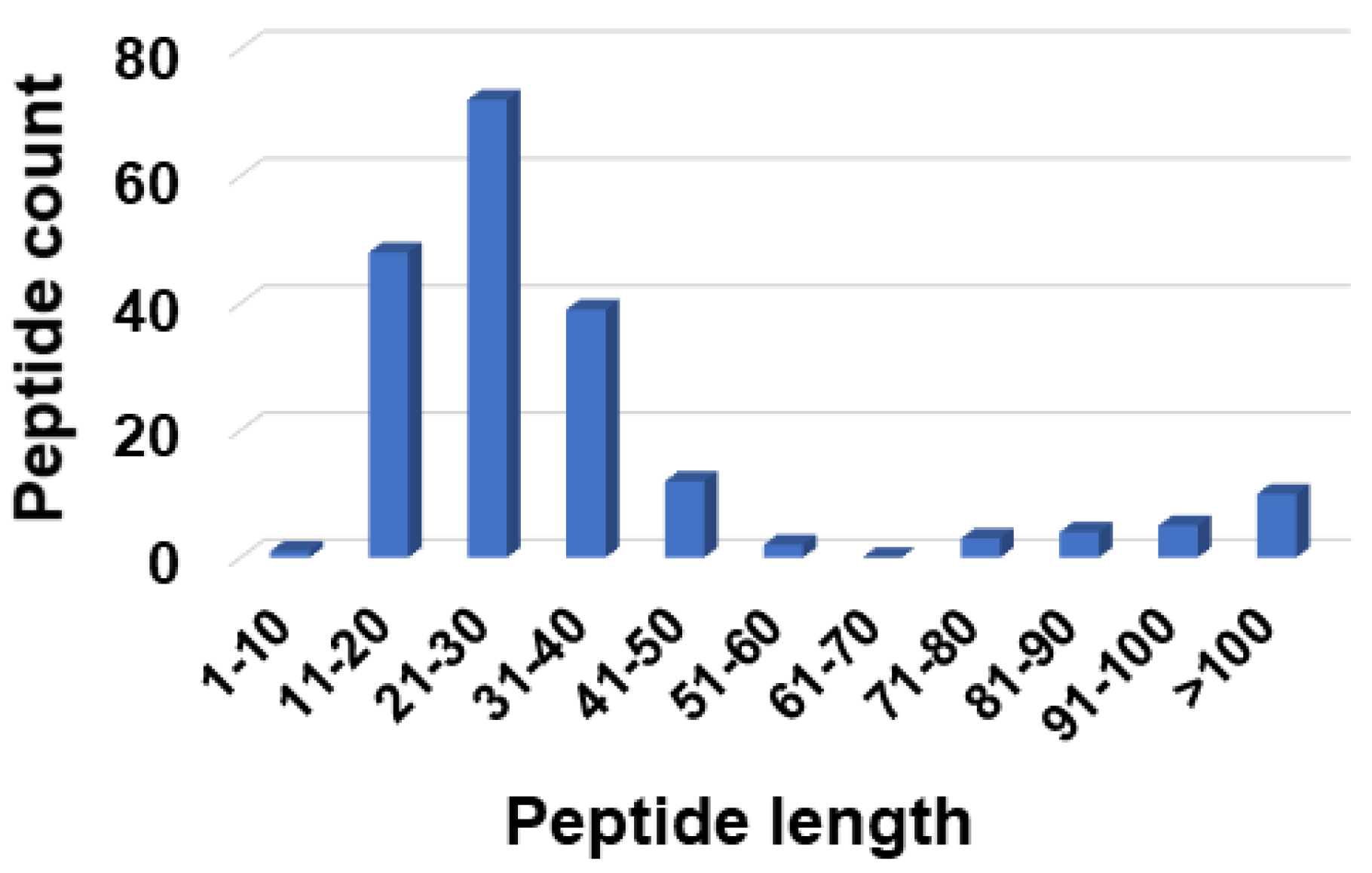
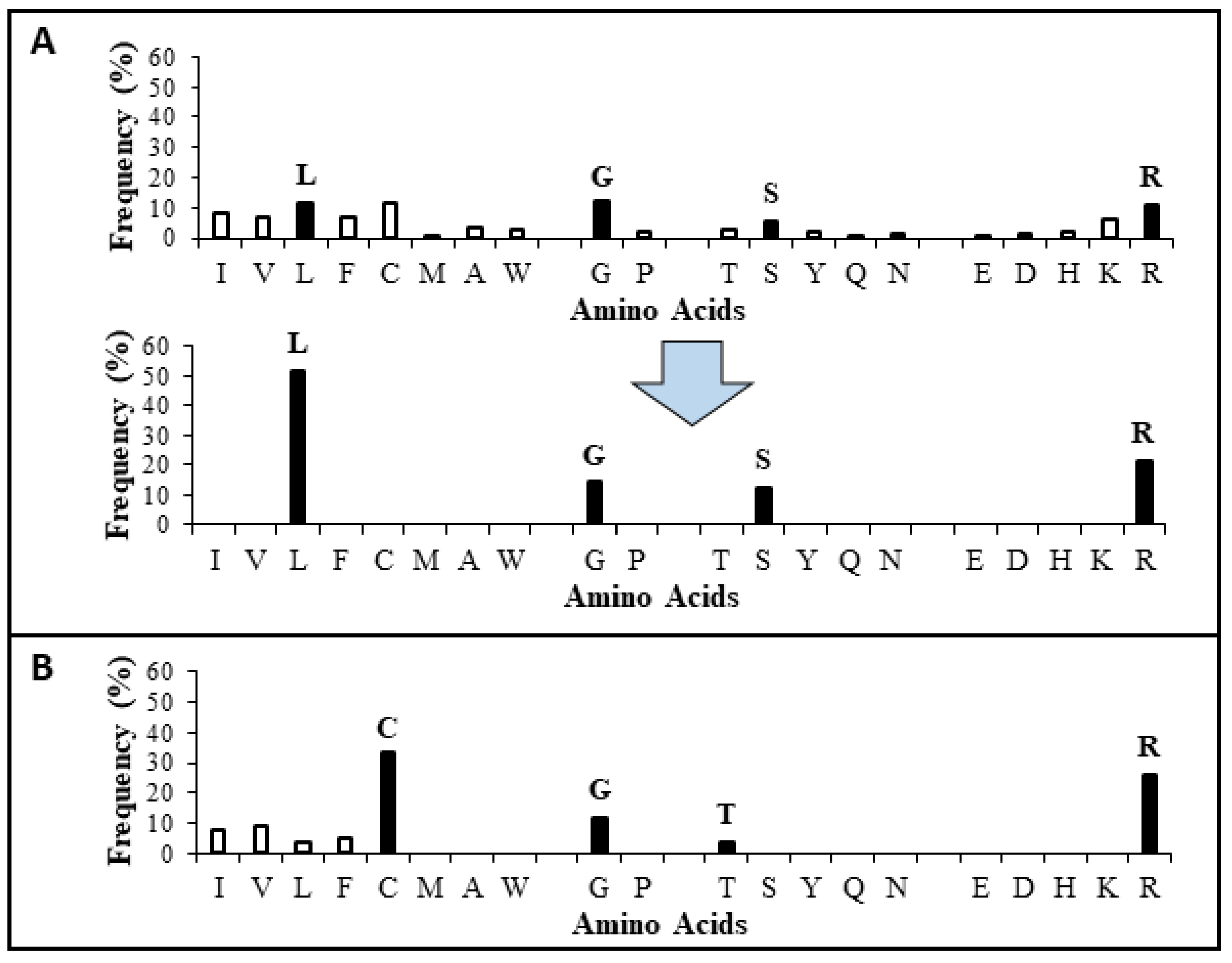
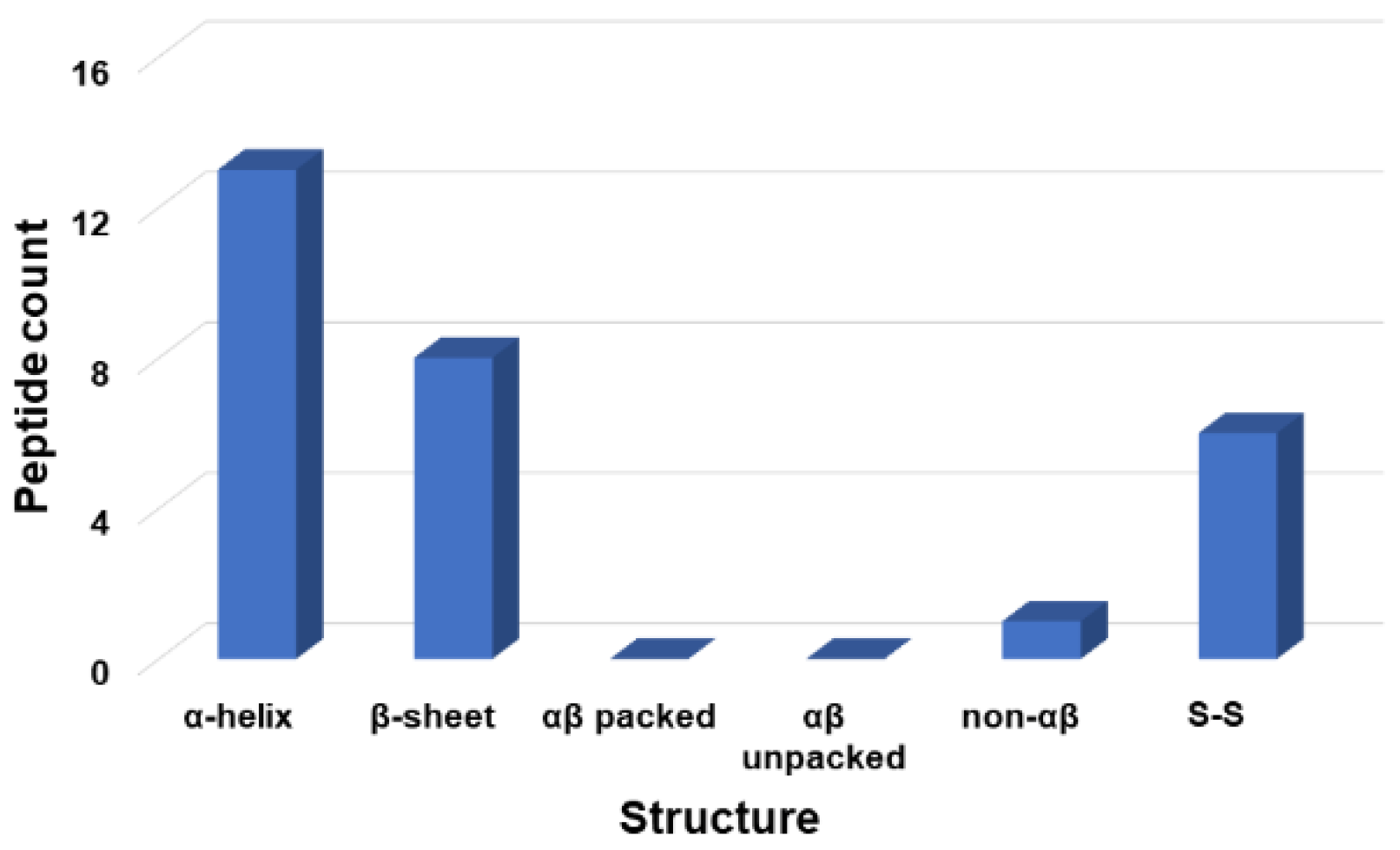
2.1. Peptide Design via an Improved Database Filtering Technology
2.2. Validation of the Most Probable Parameters
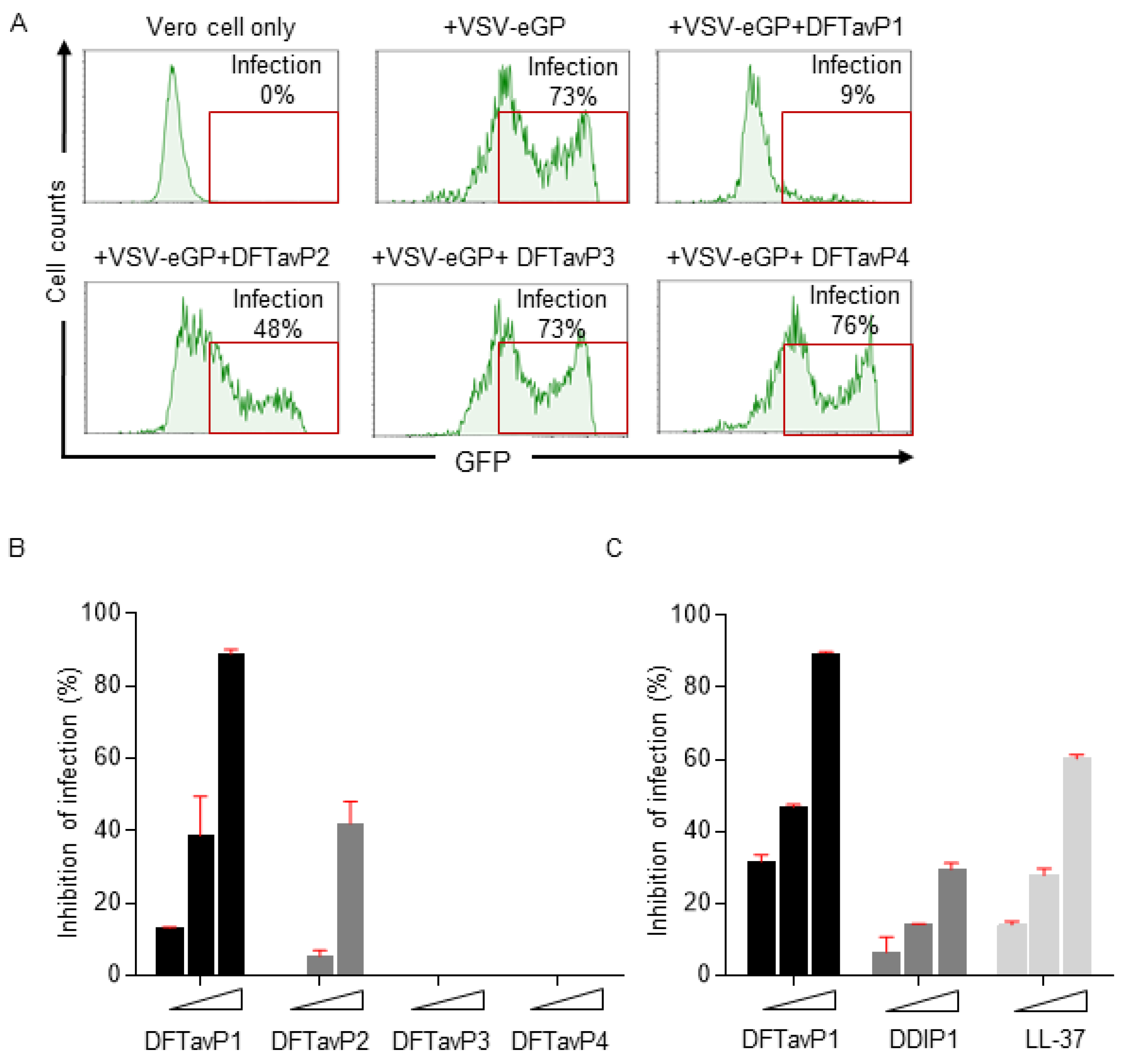
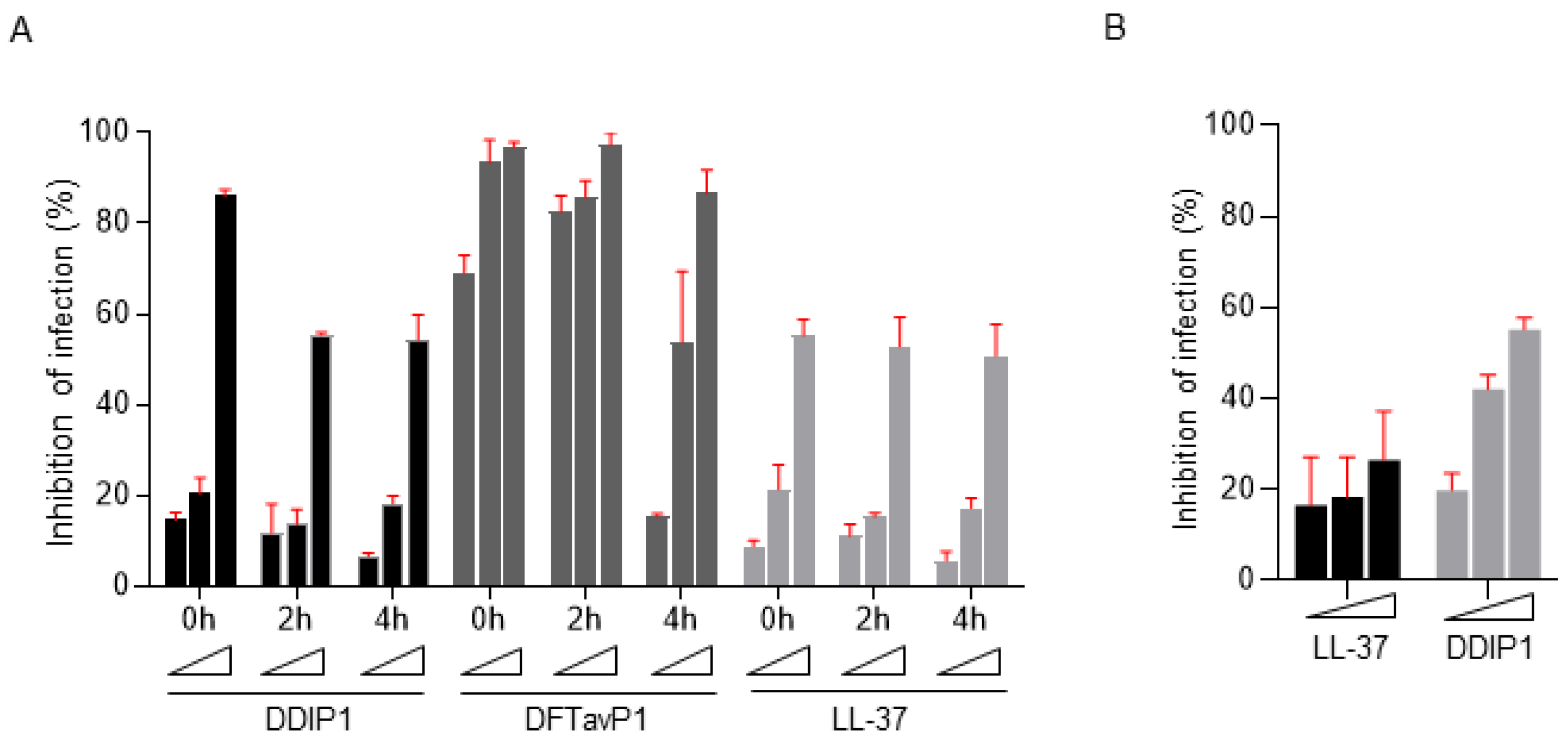
2.3. Antiviral Efficacy of Peptides Treated before or after Viral Infection
2.4. Different Requirements for Antiviral and Antibacterial Properties
3. Materials and Methods
3.1. The Antimicrobial Peptide Database
3.2. Database Filtering Technology (DFT) vs. Improved DFT
3.3. Chemicals and Peptides
3.4. SARS-CoV-2 Safety Statement
3.5. Antiviral Assays
3.6. Antibacterial Assays
3.7. Cytotoxicity
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Website. Available online: https://covid19.who.int/ (accessed on 21 March 2022).
- Da Costa, S.M. The impact of the Ebola crisis on mortality and welfare in Liberia. Health Econ. 2020, 29, 1517–1532. [Google Scholar] [CrossRef]
- Shimizu, K.; Checchi, F.; Warsame, A. Disparities in Health Financing Allocation among Infectious Diseases in Ebola Virus Disease (EVD)-Affected Countries, 2005–2017. Healthcare 2022, 10, 179. [Google Scholar] [CrossRef]
- El-Masry, E.A. Immunization against severe acute respiratory syndrome Coronavirus 2: An overview. Afr. Health Sci. 2021, 21, 1574–1583. [Google Scholar] [CrossRef]
- Diakou, K.I.; Mitsis, T.; Pierouli, K.; Papakonstantinou, E.; Bongcam-Rudloff, E.; Wayengera, M.; Vlachakis, D. Ebola Virus Disease and Current Therapeutic Strategies: A Review. Adv. Exp. Med. Biol. 2021, 1339, 131–137. [Google Scholar]
- Chen, W.H.; Strych, U.; Hotez, P.J.; Bottazzi, M.E. The SARS-CoV-2 Vaccine Pipeline: An Overview. Curr. Trop. Med. Rep. 2020, 7, 61–64. [Google Scholar] [CrossRef] [Green Version]
- Lechmere, T.; Snell, L.B.; Graham, C.; Seow, J.; Shalim, Z.A.; Charalampous, T.; Alcolea-Medina, A.; Batra, R.; Nebbia, G.; Edgeworth, J.D.; et al. Broad Neutralization of SARS-CoV-2 Variants, Including Omicron, following Breakthrough Infection with Delta in COVID-19-Vaccinated Individuals. Mbio 2022, e0379821. [Google Scholar] [CrossRef]
- Boman, H.G. Antibacterial peptides: Basic facts and emerging concepts. J. Intern. Med. 2003, 254, 197–215. [Google Scholar] [CrossRef]
- Etayash, H.; Hancock, R.E.W. Host Defense Peptide-Mimicking Polymers and Polymeric-Brush-Tethered Host Defense Peptides: Recent Developments, Limitations, and Potential Success. Pharmaceutics 2021, 13, 1820. [Google Scholar] [CrossRef]
- Bevins, C.L. Innate immune functions of α-defensins in the small intestine. Dig. Dis. 2013, 31, 299–304. [Google Scholar] [CrossRef]
- Mammari, N.; Krier, Y.; Albert, Q.; Devocelle, M.; Varbanov, M. On Behalf of the Oemonom. Plant-Derived Antimicrobial Peptides as Potential Antiviral Agents in Systemic Viral Infections. Pharmaceuticals 2021, 14, 774. [Google Scholar] [CrossRef]
- Brice, D.C.; Diamond, G. Antiviral Activities of Human Host Defense Peptides. Curr. Med. Chem. 2020, 27, 1420–1443. [Google Scholar] [CrossRef]
- Bhopale, G.M. Antimicrobial Peptides: A Promising Avenue for Human Healthcare. Curr. Pharm. Biotechnol. 2020, 21, 90–96. [Google Scholar] [CrossRef]
- Ferrera, L.; Cappiello, F.; Loffredo, M.R.; Puglisi, E.; Casciaro, B.; Botta, B.; Galietta, L.J.V.; Mori, M.; Mangoni, M.L. Esc peptides as novel potentiators of defective cystic fibrosis transmembrane conductance regulator: An unprecedented property of antimicrobial peptides. Cell. Mol. Life Sci. 2021, 79, 67. [Google Scholar] [CrossRef]
- Xu, C.; Wang, A.; Marin, M.; Honnen, W.; Ramasamy, S.; Porter, E.; Subbian, S.; Pinter, A.; Melikyan, G.B.; Lu, W.; et al. Human Defensins Inhibit SARS-CoV-2 Infection by Blocking Viral Entry. Viruses 2021, 13, 1246. [Google Scholar] [CrossRef]
- Wang, C.; Wang, S.; Li, D.; Chen, P.; Han, S.; Zhao, G.; Chen, Y.; Zhao, J.; Xiong, J.; Qiu, J.; et al. Human Cathelicidin Inhibits SARS-CoV-2 Infection: Killing Two Birds with One Stone. ACS Infect. Dis. 2021, 7, 1545–1554. [Google Scholar] [CrossRef]
- Solanki, S.S.; Singh, P.; Kashyap, P.; Sansi, M.S.; Ali, S.A. Promising role of defensins peptides as therapeutics to combat against viral infection. Microb. Pathog. 2021, 155, 104930. [Google Scholar] [CrossRef]
- Fu, Y.; Jaarsma, A.H.; Kuipers, O.P. Antiviral activities and applications of ribosomally synthesized and post-translationally modified peptides (RiPPs). Cell. Mol. Life Sci. 2021, 78, 3921–3940. [Google Scholar] [CrossRef]
- Chessa, C.; Bodet, C.; Jousselin, C.; Wehbe, M.; Lévêque, N.; Garcia, M. Antiviral and Immunomodulatory Properties of Antimicrobial Peptides Produced by Human Keratinocytes. Front. Microbiol. 2020, 11, 1155. [Google Scholar] [CrossRef]
- Hartshorn, K.L. Role of surfactant protein A and D (SP-A and SP-D) in human antiviral host defense. Front. Biosci (Schol. Ed.) 2010, 2, 527–546. [Google Scholar] [CrossRef] [Green Version]
- Laneri, S.; Brancaccio, M.; Mennitti, C.; De Biasi, M.G.; Pero, M.E.; Pisanelli, G.; Scudiero, O.; Pero, R. Antimicrobial Peptides and Physical Activity: A Great Hope against COVID 19. Microorganisms 2021, 9, 1415. [Google Scholar] [CrossRef]
- Rani, P.; Kapoor, B.; Gulati, M.; Atanasov, A.G.; Alzahrani, Q.; Gupta, R. Antimicrobial peptides: A plausible approach for COVID-19 treatment. Expert Opin. Drug Discov. 2022, in press. [Google Scholar] [CrossRef]
- Enayathullah, M.G.; Parekh, Y.; Banu, S.; Ram, S.; Nagaraj, R.; Kumar, B.K.; Idris, M.M. Gramicidin S and melittin: Potential anti-viral therapeutic peptides to treat SARS-CoV-2 infection. Sci. Rep. 2022, 12, 3446. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Cooper, C.L.; Wang, G.; Morwitzer, M.J.; Kota, K.; Tran, J.P.; Bradfute, S.B.; Liu, Y.; Shao, J.; Zhang, A.K.; et al. Engineered Human Cathelicidin Antimicrobial Peptides Inhibit Ebola Virus Infection. Iscience 2020, 23, 100999. [Google Scholar] [CrossRef]
- Wang, G.; Li, X.; Wang, Z. APD2: The updated antimicrobial peptide database and its application in peptide design. Nucleic Acids Res. 2009, 37, D933-7. [Google Scholar] [CrossRef] [Green Version]
- Kyte, J.; Doolittle, R.F. A simple method for displaying the hydropathic character of a protein. J. Mol. Biol. 1982, 157, 105–132. [Google Scholar] [CrossRef] [Green Version]
- Wang, G. Database-Guided Discovery of Potent Peptides to Combat HIV-1 or Superbugs. Pharmaceuticals 2013, 6, 728–758. [Google Scholar] [CrossRef]
- Mishra, B.; Wang, G. Ab initio design of potent anti-MRSA peptides based on database filtering technology. J. Am. Chem. Soc. 2012, 134, 12426–12429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, Y.Q.; Yuan, J.; Osapay, G.; Osapay, K.; Tran, D.; Miller, C.J.; Ouellette, A.J.; Selsted, M.E. A cyclic antimicrobial peptide produced in primate leukocytes by the ligation of two truncated alpha-defensins. Science 1999, 286, 498–502. [Google Scholar] [CrossRef] [Green Version]
- Wang, G.; Watson, K.M.; Peterkofsky, A.; Buckheit, R.W., Jr. Identification of novel human immunodeficiency virus type 1-inhibitory peptides based on the antimicrobial peptide database. Antimicrob. Agents Chemother. 2010, 54, 1343–1346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahmud, S.; Paul, G.K.; Biswas, S.; Afrose, S.; Mita, M.A.; Hasan, M.R.; Shimu, M.S.S.; Hossain, A.; Promi, M.M.; Ema, F.K.; et al. Prospective Role of Peptide-Based Antiviral Therapy Against the Main Protease of SARS-CoV-2. Front. Mol. Biosci. 2021, 8, 628585. [Google Scholar] [CrossRef]
- Wang, G.; Watson, K.M.; Buckheit, R.W., Jr. Anti-human immunodeficiency virus type 1 activities of antimicrobial peptides derived from human and bovine cathelicidins. Antimicrob. Agents Chemother. 2008, 52, 3438–3440. [Google Scholar] [CrossRef] [Green Version]
- Wong, J.H.; Legowska, A.; Rolka, K.; Ng, T.B.; Hui, M.; Cho, C.H.; Lam, W.W.; Au, S.W.; Gu, O.W.; Wan, D.C. Effects of cathelicidin and its fragments on three key enzymes of HIV-1. Peptides 2011, 2, 1117–1122. [Google Scholar] [CrossRef] [PubMed]
- Lakshmaiah Narayana, J.; Mishra, B.; Lushnikova, T.; Wu, Q.; Chhonker, Y.S.; Zhang, Y.; Zarena, D.; Salnikov, E.S.; Dang, X.; Wang, F.; et al. Two distinct amphipathic peptide antibiotics with systemic efficacy. Proc. Natl Acad. Sci. USA 2020, 117, 19446–19454. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, A.S.; Reehl, S.M.; Kehn-Hall, K.; Bishop, B.; Webb-Robertson, B.M. Better understanding and prediction of antiviral peptides through primary and secondary structure feature importance. Sci. Rep. 2020, 10, 19260. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Sutherland, D.; Hammond, S.A.; Yang, C.; Taho, F.; Bergman, L.; Houston, S.; Warren, R.L.; Wong, T.; Hoang, L.M.N.; et al. AMPlify: Attentive deep learning model for discovery of novel antimicrobial peptides effective against WHO priority pathogens. BMC Genom. 2022, 23, 77. [Google Scholar] [CrossRef]
- Ma, Y.; Guo, Z.; Xia, B.; Zhang, Y.; Liu, X.; Yu, Y.; Tang, N.; Tong, X.; Wang, M.; Ye, X.; et al. Identification of antimicrobial peptides from the human gut microbiome using deep learning. Nat. Biotechnol. 2022. [Google Scholar] [CrossRef]
- Wang, G.; Vaisman, I.I.; van Hoek, M.L. Machine Learning Prediction of Antimicrobial Peptides. Methods Mol Biol. 2022, 2405, 1–37. [Google Scholar] [PubMed]
- Khabbaz, H.; Karimi-Jafari, M.H.; Saboury, A.A.; BabaAli, B. Prediction of antimicrobial peptides toxicity based on their physico-chemical properties using machine learning techniques. BMC Bioinform. 2021, 22, 549. [Google Scholar] [CrossRef] [PubMed]
- Yaseen, A.; Gull, S.; Akhtar, N.; Amin, I.; Minhas, F. HemoNet: Predicting hemolytic activity of peptides with integrated feature learning. J. Bioinform. Comput. Biol. 2021, 19, 2150021. [Google Scholar] [CrossRef] [PubMed]
- Timmons, P.B.; Hewage, C.M. HAPPENN is a novel tool for hemolytic activity prediction for therapeutic peptides which employs neural networks. Sci. Rep. 2020, 10, 10869. [Google Scholar] [CrossRef]
- Plisson, F.; Ramírez-Sánchez, O.; Martínez-Hernández, C. Machine learning-guided discovery and design of non-hemolytic peptides. Sci. Rep. 2020, 10, 16581. [Google Scholar] [CrossRef] [PubMed]
- Porto, W.F.; Ferreira, K.C.V.; Ribeiro, S.M.; Franco, O.L. Sense the moment: A highly sensitive antimicrobial activity predictor based on hydrophobic moment. Biochim. Biophys. Acta Gen. Subj. 2022, 1866, 130070. [Google Scholar] [CrossRef] [PubMed]
- The Antimicrobial Peptide Database. Available online: https://aps.unmc.edu (accessed on 1 June 2021).
| Peptide | Amino Acid Sequence a | Length | Net Charge | Pho b | Boman Index c | GRAVY |
|---|---|---|---|---|---|---|
| DFTavP1 | RWLRGLLSGLLRRLLSGLLL | 20 | +5 | 55 | 0.6 | 0.815 |
| DFTavP2 | RWLRGLLSGLLRRLLS | 16 | +5 | 50 | 1.73 | 0.331 |
| DFTavP3 | RWLRGLLSGLLR | 12 | +4 | 50 | 1.61 | 0.25 |
| DFTavP4 | RWVRGVVSGVVRRVVS | 16 | +5 | 50 | 2.12 | 0.506 |
| DDIP1 d | GLRCRLGRLLRRLGRCLLR | 19 | +7 | 47 | 3.4 | −0.0579 |
| Peptide | S. aureus USA300 | Staphylococcus epidermidis 1457 | Escherichia coli E416-7 | Pseudomonas aeruginosa #2 | Klebsiella pneumoniae E406-17 | Acinetobacter baumannii B28-16 |
|---|---|---|---|---|---|---|
| DFTavP1 | 8–16 | 8–16 | 16 | 32 | 16–32 | 8 |
| DFTavP2 | 4 | 2 | 4 | 8 | 4 | 2 |
| DFTavP3 | 4 | 8 | 2–4 | 4–8 | 8 | 4 |
| DFTavP4 | >64 | NA | 16 | NA | NA | NA |
| DDIP1 | 4 | 4–8 | 2 | 4 | 4 | 2–4 |
| Peptide | hRBC HC50 a | mRBC HC50 b | HaCaT TC50 c | Vero Cell TC50 | Calu3 Cell TC50 |
|---|---|---|---|---|---|
| DFTavP1 | <12.5 µM | <10 µM | 25 µM | 2.39 | 11.88 |
| DDIP1 | >160 µM | >160 µM | >100 µM | 13 | 14.25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ripperda, T.; Yu, Y.; Verma, A.; Klug, E.; Thurman, M.; Reid, S.P.; Wang, G. Improved Database Filtering Technology Enables More Efficient Ab Initio Design of Potent Peptides against Ebola Viruses. Pharmaceuticals 2022, 15, 521. https://doi.org/10.3390/ph15050521
Ripperda T, Yu Y, Verma A, Klug E, Thurman M, Reid SP, Wang G. Improved Database Filtering Technology Enables More Efficient Ab Initio Design of Potent Peptides against Ebola Viruses. Pharmaceuticals. 2022; 15(5):521. https://doi.org/10.3390/ph15050521
Chicago/Turabian StyleRipperda, Thomas, Yangsheng Yu, Atul Verma, Elizabeth Klug, Michellie Thurman, St Patrick Reid, and Guangshun Wang. 2022. "Improved Database Filtering Technology Enables More Efficient Ab Initio Design of Potent Peptides against Ebola Viruses" Pharmaceuticals 15, no. 5: 521. https://doi.org/10.3390/ph15050521
APA StyleRipperda, T., Yu, Y., Verma, A., Klug, E., Thurman, M., Reid, S. P., & Wang, G. (2022). Improved Database Filtering Technology Enables More Efficient Ab Initio Design of Potent Peptides against Ebola Viruses. Pharmaceuticals, 15(5), 521. https://doi.org/10.3390/ph15050521








