Hesperidin-Loaded Lipid Polymer Hybrid Nanoparticles for Topical Delivery of Bioactive Drugs
Abstract
:1. Introduction
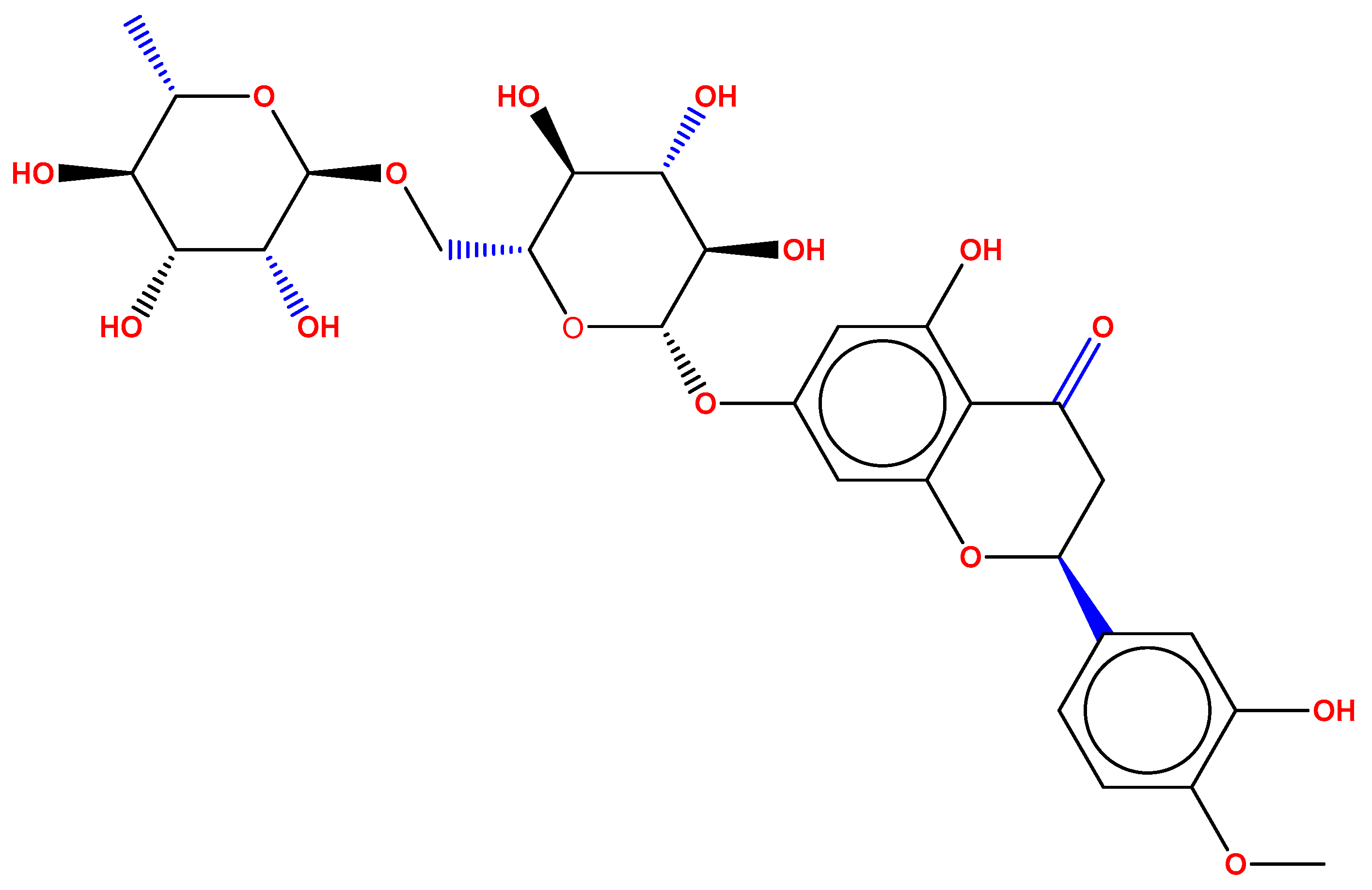
2. Results and Discussions
2.1. Optimization of HLPHNs
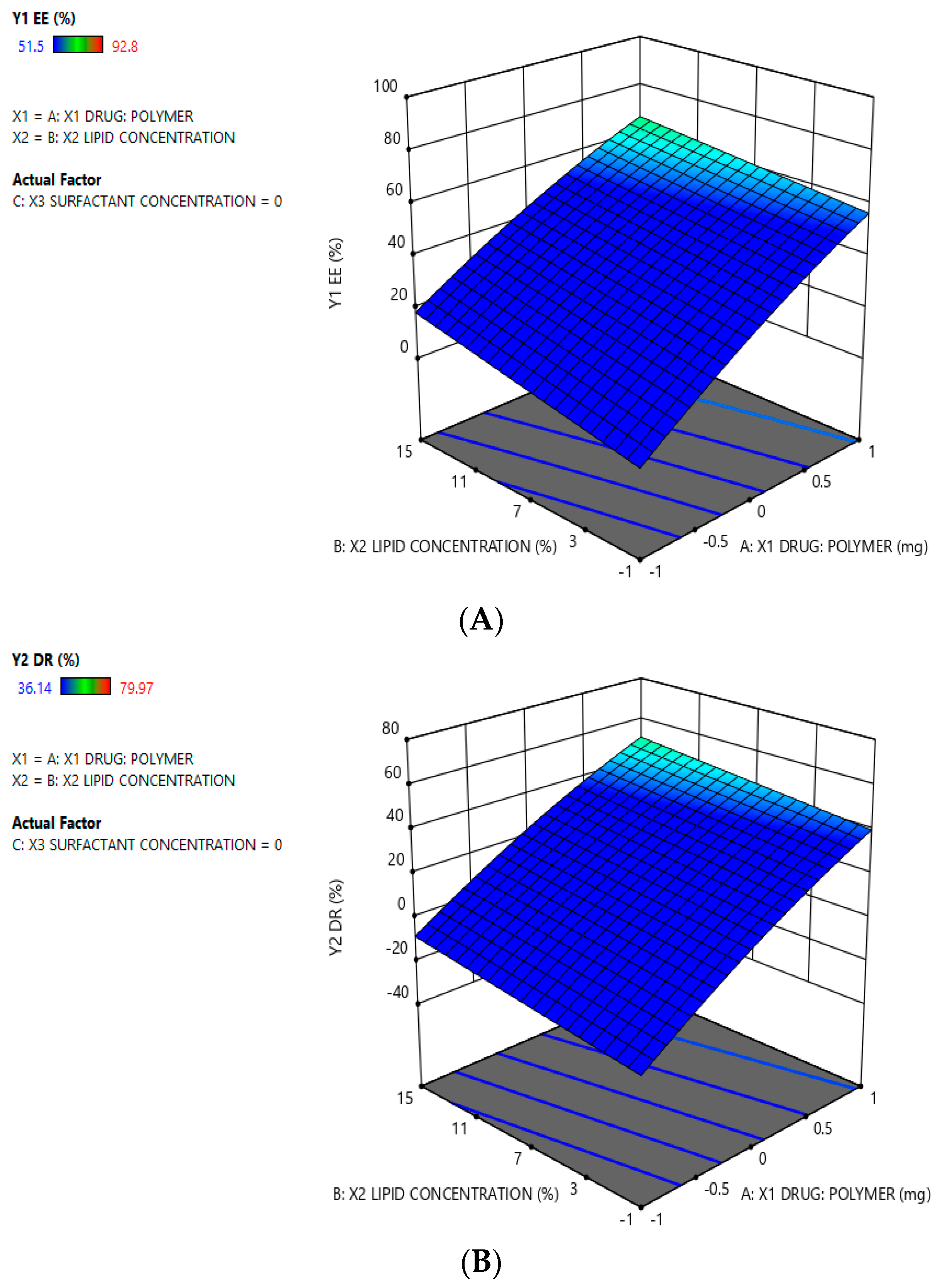
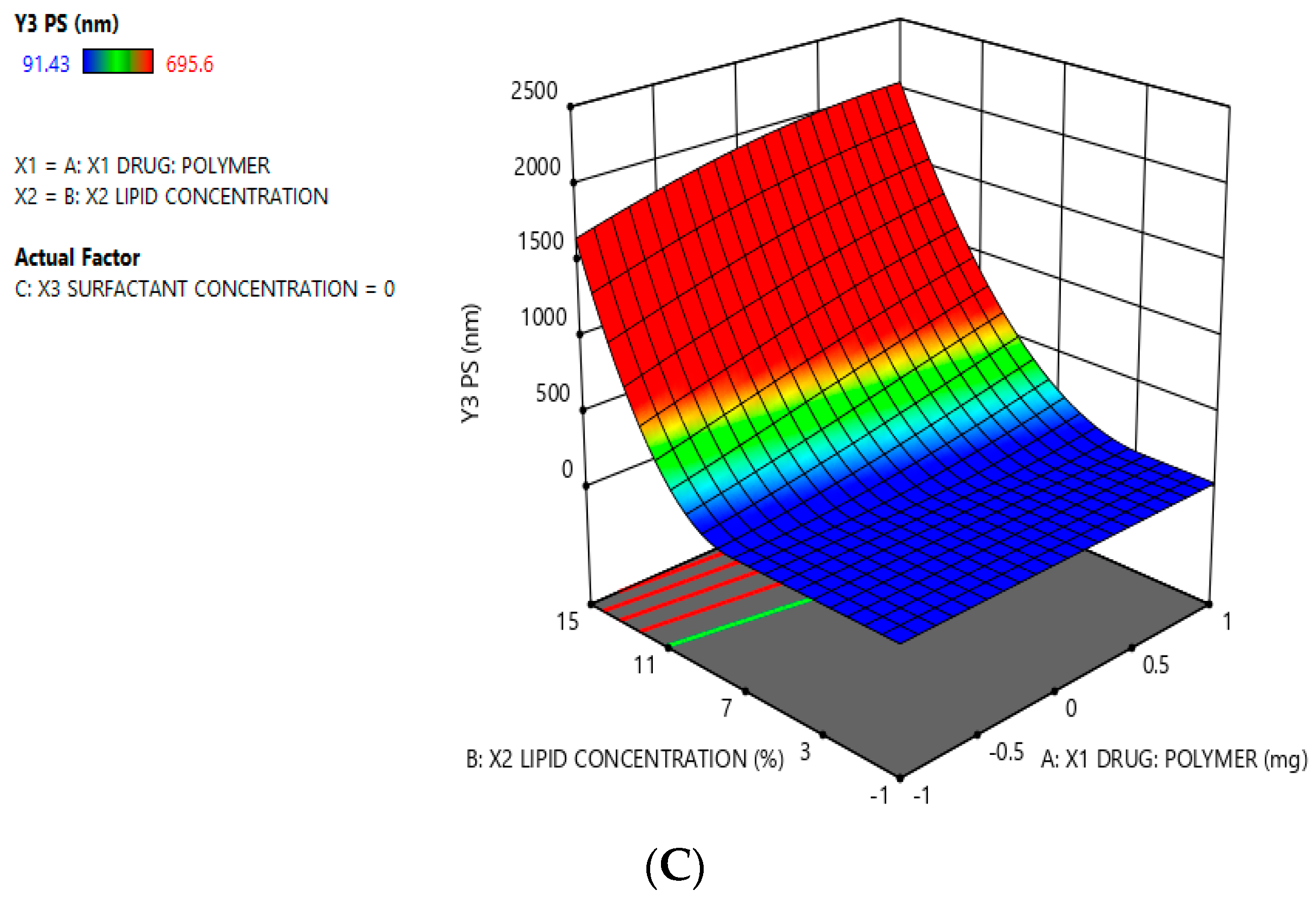
2.2. Analysis of Optimization Data for the HLPHNs
2.3. Screening HLHNPs Using Surface Methodology Using Box-Behnken DESIGN
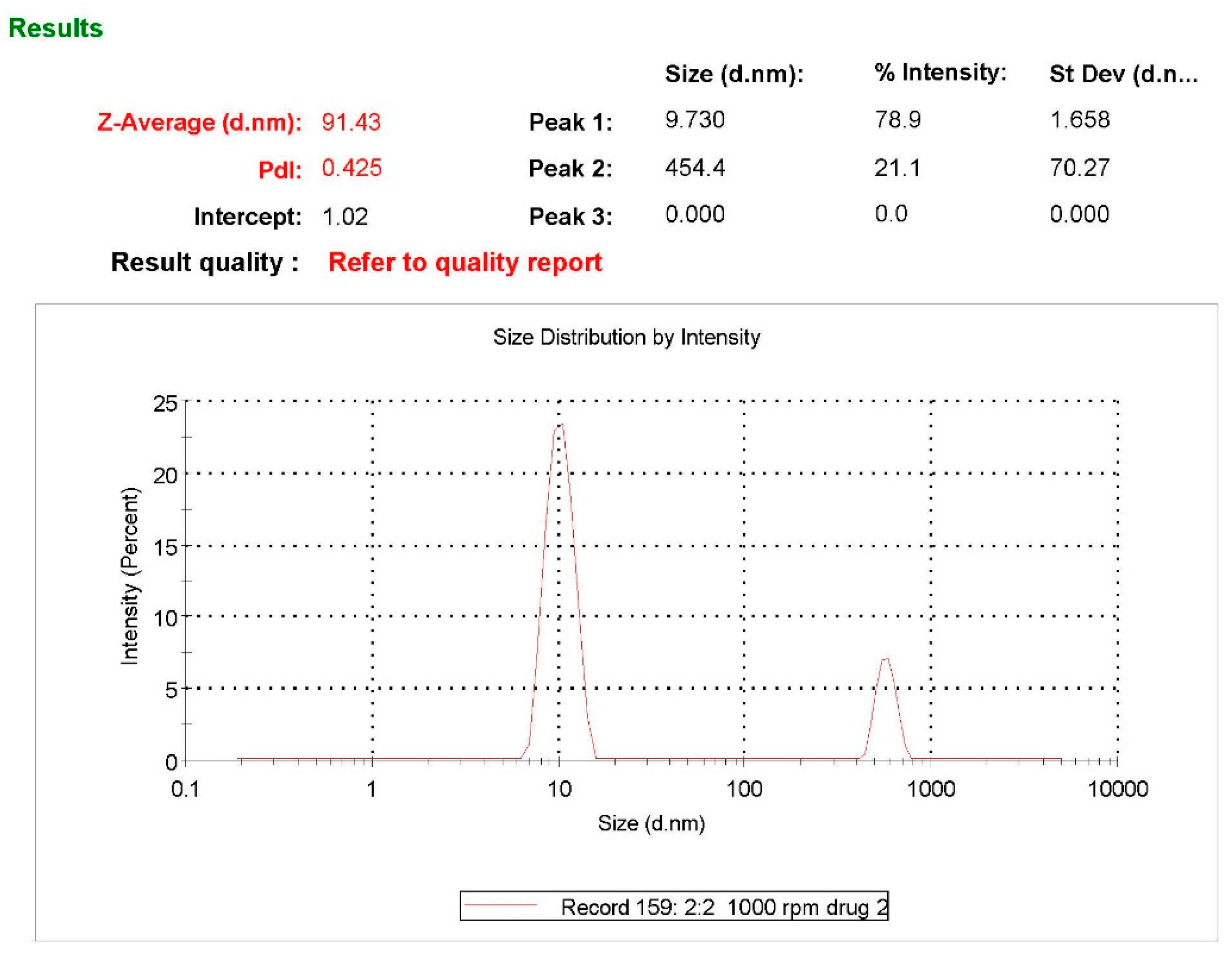
2.4. Particle Size, Zeta Potential and PDI Determination
2.5. Entrapment Efficiency Percentage (%EE)
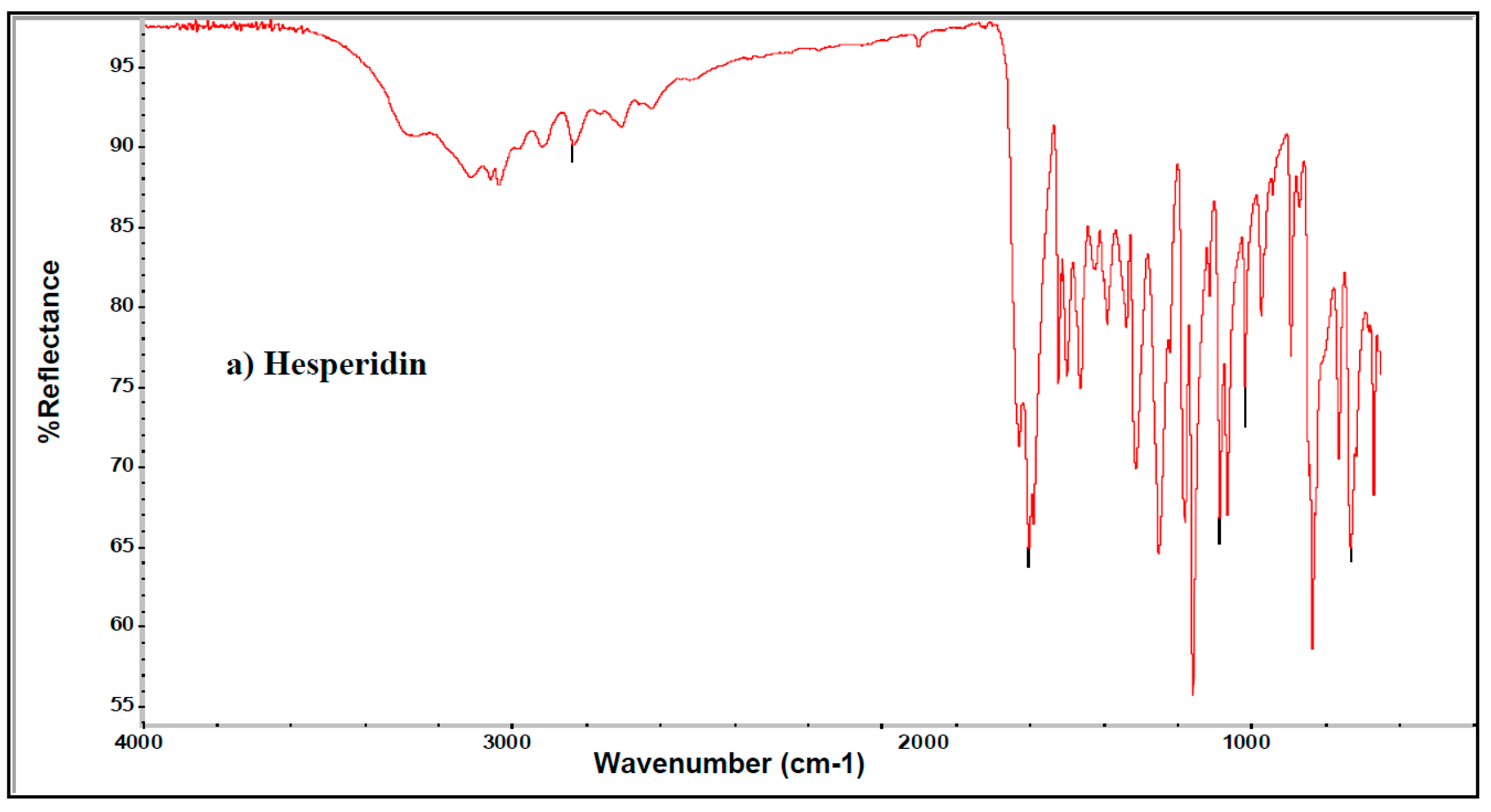
2.6. Infrared (IR) Spectroscopic Analysis of HLPHNs
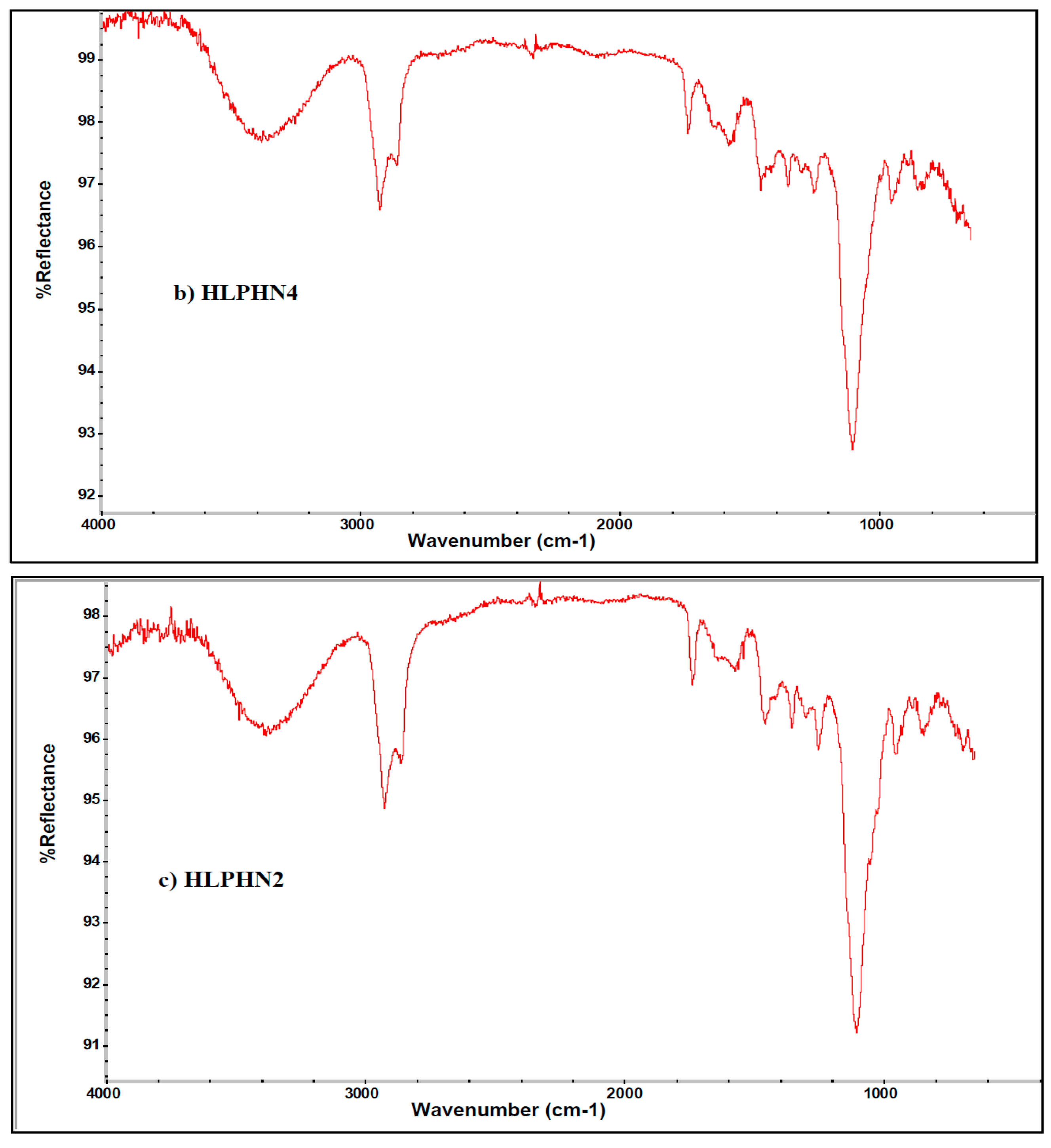
2.7. DSC Study
2.8. XRD Study
2.9. TEM Analysis of Modified HLPHNs
2.10. Antioxidant Activity of the HLPHN4
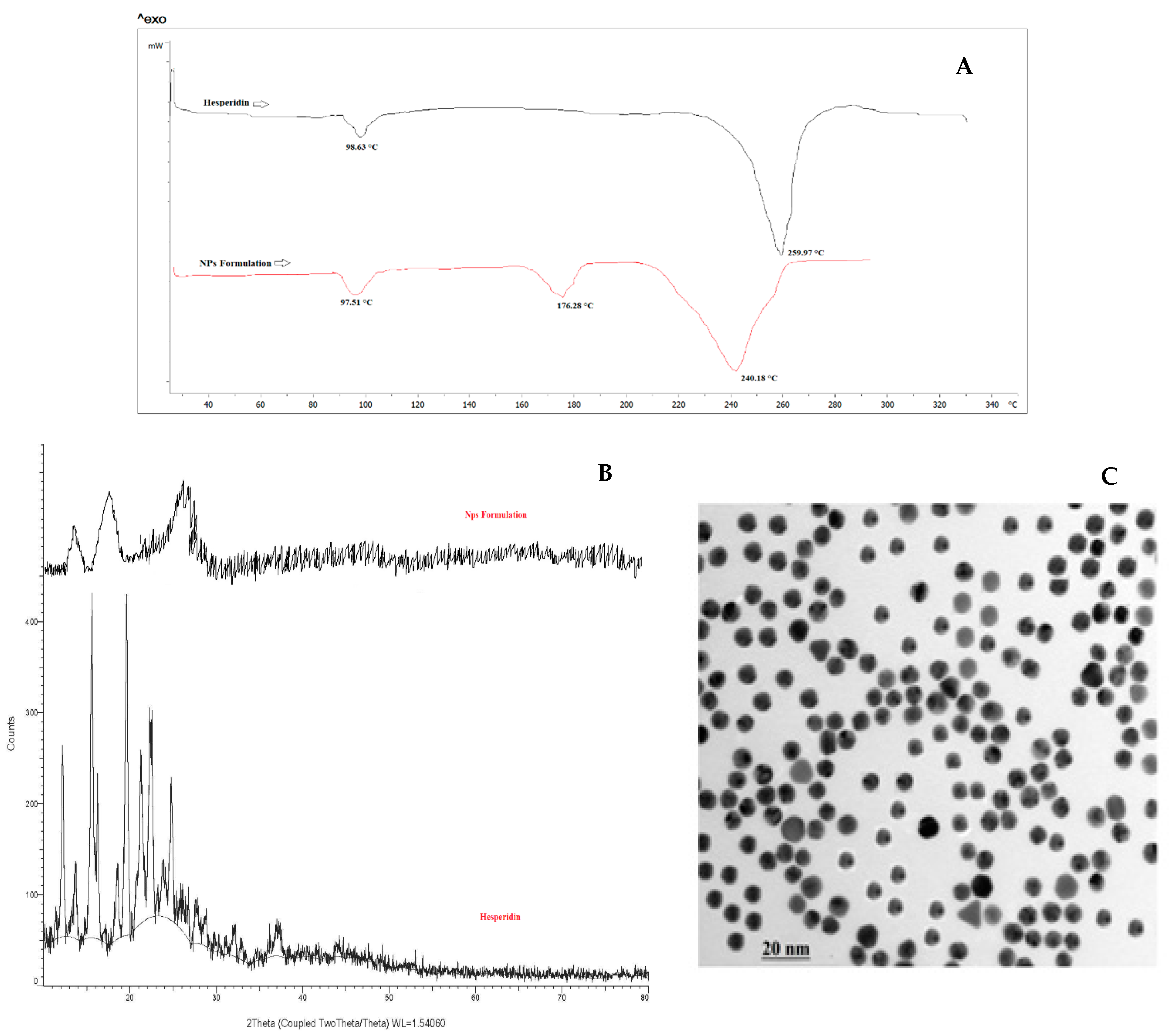
2.11. In-Vitro Drug Release (DR) Studies
2.12. Storage Stability Studies
3. Materials and Method
3.1. Chemical, Reagents and Solution Preparation
3.2. Development of Hesperidin Loaded Lipid-Polymer Hybrid Nanoparticles (HLPHNs)
3.3. Optimization of Modified HLPHNs
3.4. Surface Methodology Using the Box-Behnken Design: Statistical Parameters
3.5. Characterization of Modified HLPHNs
3.5.1. Particle Size, Zeta Potential, and PDI Determination
3.5.2. Fourier Transform Infrared Spectroscopy (FTIR) Analysis of LPHNPs
3.5.3. Differential Scanning Calorimetry (DSC)
3.5.4. X-ray Diffraction (XRD) Analysis
3.5.5. Transmissions Electron Microscopy (TEM) Study
3.6. Antioxidant Activity of the HLPHNs
3.7. Entrapment Efficiency Percentage (%EE)
3.8. In-Vitro Drug Release from HLPHNs as Sensing Probe
3.9. Storage Stability Studies
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wenbin, L.; Kandhare, A.D.; Mukherjee, A.A.; Bodhankar, S.L. Hesperidin a plant flavonoid accelerated the cutaneous wound healing in streptozotocin-induced diabetic rats: Role of TGF-ß/Smads and Ang-1/Tie-2 signaling pathways. EXCLI J. 2018, 17, 399–419. [Google Scholar]
- Jagetia, G.C.; Rao, K.V. Topical application of hesperidin a citrus bioflavanone accelerates healing of full thickness dermal excision wounds in mice exposed to 6 Gy of whole body γ-radiation. Clin. Res. Dermatol. 2017, 4, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Bagher, Z.; Ehterami, A.; Safdel, M.H.; Khastar, H.; Semiari, H.; Asefnejad, A.; Davachi, S.M.; Mirzaii, M.; Salehi, M. Wound healing with alginate/chitosan hydrogel containing hesperidin in rat model. J. Drug Deliv Sci Technol. 2020, 55, 101379. [Google Scholar] [CrossRef]
- Sulaiman, G.M.; Waheeb, H.M.; Jabir, M.S.; Khazaal, S.H.; Dewir, Y.H.; Naidoo, Y. Hesperidin loaded on gold nanoparticles as a drug delivery system for a successful biocompatible, anti-cancer, anti-inflammatory and phagocytosis inducer model. Sci. Rep. 2020, 10, 9362. [Google Scholar] [CrossRef]
- Mieszawska, A.J.; Gianella, A.; Cormode, D.P.; Zhao, Y.; Meijerink, A.; Langer, R.; Farokhzad, O.C.; Fayad, Z.A.; Mulder, W.J. Engineering of lipid-coated PLGA nanoparticles with a tunable payload of diagnostically active nanocrystals for medical imaging. Chem. Commun. 2012, 48, 5835–5837. [Google Scholar] [CrossRef] [Green Version]
- Tahir, N.; Madni, A.; Balasubramanian, V.; Rehman, M.; Correia, A.; Kashif, P.M.; Mäkilä, E.; Salonen, J.; Santos, H.A. Development and optimization of methotrexate-loaded lipid-polymer hybrid nanoparticles for controlled drug delivery applications. Int. J. Pharm. 2017, 533, 156–168. [Google Scholar] [CrossRef]
- Wu, X.Y. Strategies for optimizing polymer-lipid hybrid nanoparticle-mediated drug delivery. Expert Opin. Drug Deliv. 2016, 13, 609–612. [Google Scholar] [CrossRef]
- Dave, V.; Yadav, R.B.; Kushwaha, K.; Yadav, S.; Sharma, S.; Agrawal, U. Lipid-polymer hybrid nanoparticles: Development & statistical optimization of norfloxacin for topical drug delivery system. Bioact. Mater. 2017, 2, 269–280. [Google Scholar]
- Khoshfetrat, A.B.; Khanmohammadi, M.; Sakai, S.; Taya, M. Enzymatically-gellable galactosylated chitosan: Hydrogel characteristics and hepatic cell behavior. Int. J. Biol. Macromol. 2016, 92, 892–899. [Google Scholar] [CrossRef]
- Logith, R.K.; KeshavNarayan, A.; Dhivya, S.; Chawla, A.; Saravanan, S.; Selvamurugan, N. A review of chitosan and its derivatives in bone tissue engineering. Carbohydr. Polym. 2016, 151, 172–188. [Google Scholar]
- Kalita, B.; Patwary, B.N. Formulation and In Vitro Evaluation of Hesperidin-Phospholipid Complex and its Antioxidant Potential. Curr. Drug Ther. 2020, 15, 28–36. [Google Scholar] [CrossRef]
- Xia, H.J.; Zhang, Z.H.; Jin, X.; Hu, Q.; Chen, X.Y.; Jia, X.B. A novel drug-phospholipid complex enriched with micelles: Preparation and evaluation in vitro and in vivo. Int. J. Nanomed. 2013, 8, 545–554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Udapurkar, P.P.; Bhusnure, O.G.; Kamble, S.R. Diosmin Phytosomes: Development, Optimization and Physicochemical Characterization. Indian J. Pharm. Educ. Res. 2018, 52, S29–S36. [Google Scholar] [CrossRef] [Green Version]
- Aswathy, K.N.; Asdaq, S.M.B.; Saritha, C.K.; Thomas, L.; Haridas, N.; Viswanad, V.; Sahu, R.K.; Fattepur, S.; Alamri, A.S.; Alsanie, W.F.; et al. Formulation and In-vitro Characterization of Fast-Disintegrating Herbal Extract Sublingual Immunotherapy Tablet for Peanut-Induced Allergic Asthma. Saudi J. Biol. Sci. 2021. [Google Scholar] [CrossRef]
- Kim, M.S.; Jin, S.J.; Kim, J.S.; Park, H.J.; Song, H.S.; Neubert, R.H.; Hwang, S.J. Preparation, characterization and in vivo evaluation of amorphous atorvastatin calcium nanoparticles using supercritical antisolvent (SAS) process. Eur. J. Pharm. Biopharm. 2008, 69, 454–465. [Google Scholar] [CrossRef]
- Jara, M.O.; Warnken, Z.N.; Williams, R.O., III. Amorphous Solid Dispersions and the Contribution of Nanoparticles to In Vitro Dissolution and In Vivo Testing: Niclosamide as a Case Study. Pharmaceutics 2021, 13, 97. [Google Scholar] [CrossRef]
- Comino-Sanz, I.M.; López-Franco, M.D.; Castro, B.; Pancorbo-Hidalgo, P.L. The Role of Antioxidants on Wound Healing: A Review of the Current Evidence. J. Clin. Med. 2021, 10, 3558. [Google Scholar] [CrossRef]
- Zhao, R.Z.; Jiang, S.; Zhang, L.; Yu, Z.B. Mitochondrial electron transport chain, ROS generation and uncoupling (Review). Int. J. Mol. Med. 2019, 44, 3–15. [Google Scholar] [CrossRef] [Green Version]
- Cano, S.M.; Lancel, S.; Boulanger, E.; Neviere, R. Targeting Oxidative Stress and Mitochondrial Dysfunction in the Treatment of Impaired Wound Healing: A Systematic Review. Antioxidants 2018, 7, 98. [Google Scholar] [CrossRef] [Green Version]
- Ascenso, A.; Margarida, R.H.; Cabral, M.H.; Simoes, S. Topical Delivery of Antioxidants. Current Drug Delivery 2011, 8, 640–660. [Google Scholar] [CrossRef]
- Dai, X.; Liu, J.; Zheng, H.; Wichmann, J.; Hopfner, U.; Sudhop, S.; Prein, C.; Shen, Y.; Machens, H.-G.; Schilling, A.F. Nano-formulated curcumin accelerates acute wound healing through Dkk-1-mediated fibroblast mobilization and MCP-1-mediated anti-inflammation. NPG Asia Mater 2017, 9, e368. [Google Scholar] [CrossRef] [Green Version]
- Merrell, J.G.; McLaughlin, S.W.; Tie, L.; Laurencin, C.T.; Chen, A.F.; Nair, L.S. Curcumin-loaded poly(epsilon-caprolactone) nanofibres: Diabetic wound dressing with anti-oxidant and anti-inflammatory properties. Clin. Exp. Pharmacol. Physiol. 2009, 36, 1149–1156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costa, R.; Costa Lima, S.A.; Gameiro, P.; Reis, S. On the Development of a Cutaneous Flavonoid Delivery System: Advances and Limitations. Antioxidants 2021, 10, 1376. [Google Scholar] [CrossRef]
- Colobatiu, L.; Gavan, A.; Mocan, A.; Bogdan, C.; Mirel, S.; Tomuta, I. Development of bioactive compounds-loaded chitosan films by using a QbD approach—A novel and potential wound dressing material. React. Funct. Polym. 2019, 138, 46–54. [Google Scholar] [CrossRef]
- Ali, S.H.; Sulaiman, G.M.; Al-Halbosiy, M.M.; Jabir, M.S.; Hameed, A.H. Fabrication of hesperidin nanoparticles loaded by poly lactic co-Glycolic acid for improved therapeutic efficiency and cytotoxicity. Artif. Cells Nanomed. Biotechnol. 2019, 47, 378–394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jangde, R.; Rabsanjani; Khute, S. Design and Development of Ciprofloxacin Lipid Polymer Hybrid Nanoparticle by Response Surface Methodology. Res. J. Pharm. Tech. 2020, 13, 3249–3256. [Google Scholar] [CrossRef]
- Sur, S.; Rathore, A.; Dave, V.; Reddy, K.R.; Chouhan, R.S.; Sadhu, V. Recent developments in functionalized polymer nanoparticles for efficient drug delivery system. Nano-Struct. Nano-Objects 2019, 20, 100397. [Google Scholar] [CrossRef]
- Bose, R.J.; Lee, S.H.; Park, H. Lipid-based surface engineering of PLGA nanoparticles for drug and gene delivery applications. Biomater. Res. 2016, 20, 34. [Google Scholar] [CrossRef] [Green Version]
- Mukherjee, A.; Waters, A.K.; Kalyan, P.; Achrol, A.S.; Kesari, S.; Yenugonda, V.M. Lipid–polymer hybrid nanoparticles as a next-generation drug delivery platform: State of the art, emerging technologies, and perspectives. Int. J. Nanomed. 2019, 14, 1937–1952. [Google Scholar] [CrossRef] [Green Version]
- Garakani, S.S.; Davachi, S.M.; Bagher, Z.; Esfahani, A.H.; Jenabi, N.; Atoufi, Z.; Khanmohammadi, M.; Abbaspourrad, A.; Rashedi, H.; Jalessi, M. Fabrication of chitosan/polyvinylpyrrolidone hydrogel scaffolds containing PLGA microparticles loaded with dexamethasone for biomedical applications. Int. J. Biol. Macromol. 2020, 164, 356–370. [Google Scholar] [CrossRef]
- Atoufi, Z.; Kamrava, S.K.; Davachi, S.M.; Hassanabadi, M.; Garakani, S.S.; Alizadeh, R.; Farhadi, M.; Tavakol, S.; Bagher, Z.; Motlagh, G.H. Injectable PNIPAM/Hyaluronic acid hydrogels containing multipurpose modified particles for cartilage tissue engineering: Synthesis, characterization, drug release and cell culture study. Int J Biol Macromol. 2019, 139, 1168–1181. [Google Scholar] [CrossRef] [PubMed]
- Du, M.; Ouyang, Y.; Meng, F.; Zhang, X.; Ma, Q.; Zhuang, Y.; Liu, H.; Pang, M.; Cai, T.; Cai, Y. Polymer-lipid hybrid nanoparticles: A novel drug delivery system for enhancing the activity of Psoralen against breast cancer. Int. J. Pharm. 2019, 561, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Hu, J.; Chan, H.F.; Skibba, M.; Liang, G.; Chen, M. iRGD decorated lipid-polymer hybrid nanoparticles for targeted co-delivery of doxorubicin and sorafenib to enhance anti-hepatocellular carcinoma efficacy. Nanomed. Nanotech. Bio. Med. 2016, 12, 1303–1311. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, P.; Geng, T.; Mahanty, A.; Li, T.; Zong, L.; Wang, B. Integrating the drug, disulfiram into the vitamin E-TPGS-modified PEGylated nanostructured lipid carriers to synergize its repurposing for anti-cancer therapy of solid tumors. Int. J. Pharm. 2019, 557, 374–389. [Google Scholar] [CrossRef]
- Gidwani, B.; Vyas, A. Preparation, characterization, and optimization of altretamine-loaded solid lipid nanoparticles using Box-Behnken design and response surface methodology. Artif Cells Nanomed Biotechnol. 2016, 44, 571–580. [Google Scholar] [CrossRef]
- Moretti, E.; Mazzi, L.; Bonechi, C.; Salvatici, M.C.; Iacoponi, F.; Rossi, C.; Collodel, G. Effect of Quercetin-loaded liposomes on induced oxidative stress in human spermatozoa. Reprod. Toxicol. 2016, 60, 140–147. [Google Scholar] [CrossRef]
- Jangde, R.; Singh, D. Preparation and optimization of quercetin-loaded liposomes for wound healing, using response surface methodology. Artif. Cells Nanomed. Biotechnol. 2016, 44, 635–641. [Google Scholar] [CrossRef]
- Jangde, R.; Srivastava, S.; Singh, M.R.; Singh, D. In vitro and In vivo characterization of quercetin loaded multiphase hydrogel for wound healing application. Int. J. Biol. Macromol. 2018, 115, 1211–1217. [Google Scholar] [CrossRef]
- Lalrinzuali, K.; Vabeiryureilai, M.; Jagetia, G.C. Topical application of stem bark ethanol extract of Sonapatha, Oroxylum indicum (L.) Kurz accelerates healing of deep dermal excision wound in Swiss albino mice. J. Ethnopharmacol. 2018, 227, 290–299. [Google Scholar] [CrossRef]
| Variables | df | SS | Ms | F | p | R2 | SD |
|---|---|---|---|---|---|---|---|
| %EE | |||||||
| Model | 5 | 2262.16 | 452.43 | 16.56 | <0.0001 | 0.8827 | 5.23 |
| Residual | 11 | 300.59 | 27.33 | - | - | - | - |
| Total | 16 | 2562.74 | - | - | - | - | - |
| %DR | |||||||
| Model | 5 | 2799.73 | 559.95 | 20.30 | <0.0001 | 0.9022 | 5.25 |
| Residual | 11 | 303.37 | 27.58 | - | - | - | - |
| Total | 16 | 3103.10 | - | - | - | - | - |
| PS (nm) | |||||||
| Model | 5 | 339.63 | 67.93 | 3.98 | 0.6262 | 0.6442 | 4.13 |
| Residual | 11 | 187.60 | 17.05 | - | - | - | - |
| Total | 16 | 527.23 | - | - | - | - | - |
| Variable | Predicted Value | Observed Value | Bias Percentage |
|---|---|---|---|
| %DR | 65.94 | 60.95 | 7.34 |
| %EE | 68.8 | 72.36 | −5.17 |
| PS (nm) | 73.32 | 80.10 | −9.24 |
| Formulation Code | Coded level | Actual Level | %EE | %DR | PS(nm) | PDI | Zeta Potential (mv) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| X1 | X2 | X3 | X1 | X2 | X3 | ||||||
| HLPHN 1 | −1 | 0 | −1 | 1:1 | 10 | 0.5 | 91 | 75.96 | 695.6 | 0.026 | 16.6 |
| HLPHN 2 | +1 | 0 | +1 | 2:3 | 10 | 1.5 | 58.9 | 41.6 | 490.8 | 0.071 | −0.0771 |
| HLPHN 3 | −1 | −1 | 0 | 1:1 | 5 | 1 | 70 | 77.96 | 695.6 | 0.043 | 37.9 |
| HLPHN 4 | 0 | 0 | 0 | 1.5:2 | 10 | 1 | 92.8 | 53.93 | 91.43 | 0.056 | 15.6 |
| HLPHN 5 | 0 | 0 | 0 | 1.5:2 | 10 | 1 | 92.6 | 62.2 | 143.1 | 0.036 | 0.242 |
| HLPHN 6 | +1 | 0 | −1 | 2:3 | 10 | 0.5 | 51.5 | 36.14 | 158.4 | 0.029 | 46.9 |
| HLPHN 7 | 0 | 0 | 0 | 1.5:2 | 10 | 1 | 91.8 | 57.25 | 158.1 | 0.098 | 37.5 |
| HLPHN 8 | −1 | −1 | 0 | 1:1 | 5 | 1 | 72.8 | 78.96 | 672.6 | 0.362 | 37.5 |
| HLPHN 9 | 0 | 0 | 0 | 1.5:2 | 10 | 1 | 78.2 | 65.25 | 649 | 0.348 | −0.0372 |
| HLPHN 10 | 0 | −1 | +1 | 1.5:2 | 5 | 1.5 | 82.4 | 69.94 | 390.9 | 0.650 | 38.2 |
| HLPHN 11 | 0 | +1 | −1 | 1.5:2 | 15 | 0.5 | 88 | 73.94 | 551.2 | 0.257 | 4.82 |
| HLPHN12 | −1 | 0 | −1 | 1:1 | 10 | 0.5 | 76 | 79.97 | 675.3 | 0.342 | 6.83 |
| HLPHN 13 | +1 | +1 | 0 | 2:3 | 15 | 1 | 65.9 | 46.43 | 494.3 | 0.453 | 0.242 |
| HLPHN 14 | 0 | +1 | +1 | 1:1 | 15 | 1.5 | 85.5 | 72.94 | 556.4 | 0.619 | 32.3 |
| HLPHN 15 | 0 | 0 | +1 | 1:1 | 10 | 1.5 | 90.5 | 74.95 | 670.1 | 0.552 | 34.1 |
| HLPHN 16 | +1 | −1 | 0 | 2:3 | 5 | 1 | 67 | 49.89 | 468.6 | 0.196 | 4.82 |
| HLPHN 17 | 0 | −1 | −1 | 1.5:2 | 5 | 0.5 | 82.1 | 67.94 | 538.1 | 0.369 | −0.0372 |
| Concentration (µg/mL) | DPPH Scavenging % |
|---|---|
| 50 | 46.2 ± 0.14 |
| 100 | 63.7 ± 0.29 |
| 150 | 98.1 ± 0.07 |
| 200 | 121.4 ± 0.56 |
| 250 | 153.6 ± 0.33 |
| IC50 | 64.49 (µg/mL) |
| Independent Variable | −1 (Low) | 0 (Medium) | +1 (High) |
|---|---|---|---|
| Drug: polymer (mg) (X1) | 1:1 | 1.5:2 | 2:3 |
| Lipid concentration (%) (X2) | 5 | 10 | 15 |
| Surfactant concentration (ml) (X3) | 0.5 | 1 | 1.5 |
| Formulation Code | Amount of Drug (Hesperidin) (mg) | Amount of Polymer (Chitosan) (mg) | Amount of Lipid (Soya Lecithin) (mg) | Amount of Surfactant (mL) |
|---|---|---|---|---|
| HLPHN 1 | 10 | 10 | 10 | 0.5 |
| HLPHN 2 | 20 | 30 | 10 | 1.5 |
| HLPHN 3 | 10 | 10 | 5 | 1 |
| HLPHN 4 | 15 | 20 | 10 | 1 |
| HLPHN 5 | 15 | 20 | 10 | 1 |
| HLPHN 6 | 20 | 30 | 10 | 0.5 |
| HLPHN 7 | 15 | 20 | 10 | 1 |
| HLPHN 8 | 10 | 10 | 5 | 1 |
| HLPHN 9 | 15 | 20 | 10 | 1 |
| HLPHN 10 | 15 | 20 | 5 | 1.5 |
| HLPHN 11 | 15 | 20 | 15 | 0.5 |
| HLPHN12 | 10 | 10 | 10 | 0.5 |
| HLPHN 13 | 20 | 30 | 15 | 1 |
| HLPHN 14 | 10 | 10 | 15 | 1.5 |
| HLPHN 15 | 10 | 10 | 10 | 1.5 |
| HLPHN 16 | 20 | 30 | 5 | 1 |
| HLPHN 17 | 15 | 20 | 5 | 0.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jangde, R.; Elhassan, G.O.; Khute, S.; Singh, D.; Singh, M.; Sahu, R.K.; Khan, J. Hesperidin-Loaded Lipid Polymer Hybrid Nanoparticles for Topical Delivery of Bioactive Drugs. Pharmaceuticals 2022, 15, 211. https://doi.org/10.3390/ph15020211
Jangde R, Elhassan GO, Khute S, Singh D, Singh M, Sahu RK, Khan J. Hesperidin-Loaded Lipid Polymer Hybrid Nanoparticles for Topical Delivery of Bioactive Drugs. Pharmaceuticals. 2022; 15(2):211. https://doi.org/10.3390/ph15020211
Chicago/Turabian StyleJangde, Rajendra, Gamal Osman Elhassan, Sulekha Khute, Deependra Singh, Manju Singh, Ram Kumar Sahu, and Jiyauddin Khan. 2022. "Hesperidin-Loaded Lipid Polymer Hybrid Nanoparticles for Topical Delivery of Bioactive Drugs" Pharmaceuticals 15, no. 2: 211. https://doi.org/10.3390/ph15020211
APA StyleJangde, R., Elhassan, G. O., Khute, S., Singh, D., Singh, M., Sahu, R. K., & Khan, J. (2022). Hesperidin-Loaded Lipid Polymer Hybrid Nanoparticles for Topical Delivery of Bioactive Drugs. Pharmaceuticals, 15(2), 211. https://doi.org/10.3390/ph15020211






