Abstract
Isoniazid (INH) is one of the key molecules employed in the treatment of tuberculosis (TB), the most deadly infectious disease worldwide. However, the efficacy of this cornerstone drug has seriously decreased due to emerging INH-resistant strains of Mycobacterium tuberculosis (Mtb). In the present study, we aimed to chemically tailor INH to overcome this resistance. We obtained thirteen novel compounds by linking INH to in-house synthesized sulfonate esters via a hydrazone bridge (SIH1–SIH13). Following structural characterization by FTIR, 1H NMR, 13C NMR, and HRMS, all compounds were screened for their antitubercular activity against Mtb H37Rv strain and INH-resistant clinical isolates carrying katG and inhA mutations. Additionally, the cytotoxic effects of SIH1–SIH13 were assessed on three different healthy host cell lines; HEK293, IMR-90, and BEAS-2B. Based on the obtained data, the synthesized compounds appeared as attractive antimycobacterial drug candidates with low cytotoxicity. Moreover, the stability of the hydrazone moiety in the chemical structure of the final compounds was confirmed by using UV/Vis spectroscopy in both aqueous medium and DMSO. Subsequently, the compounds were tested for their inhibitory activities against enoyl acyl carrier protein reductase (InhA), the primary target enzyme of INH. Although most of the synthesized compounds are hosted by the InhA binding pocket, SIH1–SIH13 do not primarily show their antitubercular activities by direct InhA inhibition. Finally, in silico determination of important physicochemical parameters of the molecules showed that SIH1–SIH13 adhered to Lipinski’s rule of five. Overall, our study revealed a new strategy for modifying INH to cope with the emerging drug-resistant strains of Mtb.
1. Introduction
Mycobacterium tuberculosis (Mtb) is the primary causative agent of the contagious disease tuberculosis (TB) that has devastated humankind for centuries [1]. TB is one of the leading infectious agent-related causes of mortality, as confirmed by the data presented in the latest World Health Organization (WHO) Global TB Report [2]. The successful control of TB by the current chemotherapeutic regimen, mainly consisting of four first-line drugs (isoniazid, rifampicin, pyrazinamide, and ethambutol) [3], is often endangered by emerging drug-resistant Mtb strains [4].
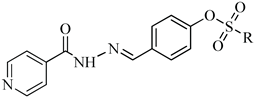
Isoniazid (isonicotinic acid hydrazide, INH) is the cornerstone drug of modern TB therapy [5]. As a prodrug, INH needs to be oxidized by the enzyme catalase-peroxidase (KatG) to inhibit its biological target enoyl-acyl carrier protein reductase (InhA), a critical enzyme employed in the biosynthesis of mycolic acids [6,7]. Therefore, the clinical efficacy of INH in the treatment of drug-resistant TB is restricted due to mutations in katG or inhA and its promoter [8,9]. Furthermore, in humans, INH is metabolized and in this way deactivated by N-acetyltransferase type 2 (NAT2). This enzyme is responsible for the acetylation of the terminal nitrogen of the hydrazide group of INH using acetyl coenzyme A (acetyl-CoA) as the acetyl donor [10]. Due to genetic polymorphism in NAT2, variable acetylation rates arise, resulting in variations in blood drug concentrations among patients treated with INH [11]. These metabolic steps, which ultimately result in the activation and deactivation of INH, are schematically presented in Figure 1.
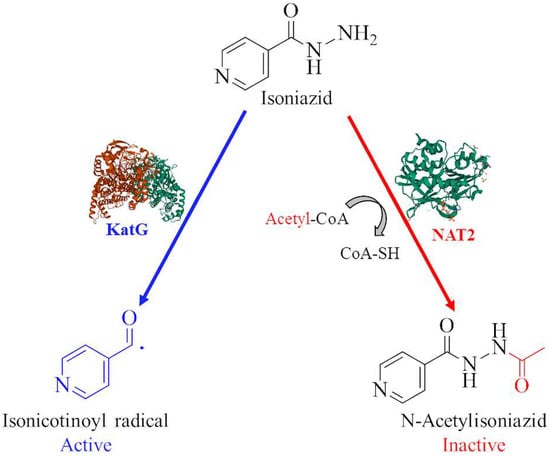
Figure 1.
Schematic depiction of pathways leading to activation and inactivation of INH.
Due to their commonly reported anti-TB properties, hydrazone-possessing molecules are of considerable interest [12]. Particularly, the synthesis of hydrazone derivatives of the current anti-TB drugs such as isoniazid [13], ciprofloxacin [14], and pyrazinamide [15] is a frequently applied antimycobacterial drug design strategy (Figure 2). Therefore, hydrazone is considered to be an excellent linker fragment for newly-designed antitubercular agents.
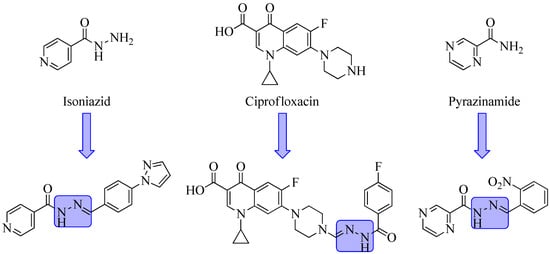
Figure 2.
Biologically active hydrazone derivatives of marketed anti-TB drugs.
As one of the most common ways to design and develop new drugs, molecular hybridization involves merging two or more pharmacophores in a single chemical entity, either directly or by using spacer units. The main goal of this strategy is to improve the biological profile while reducing side effects as much as possible [16,17].
As previously indicated, INH is a significant component of the standardized regimens for TB treatment recommended by WHO. However, inappropriate treatment or poor patient compliance with the therapy often leads to the emergence of INH-resistant strains of Mtb [18]. Thus, tailoring the chemical structure of INH is accepted as a logical approach for designing new antitubercular compounds to overcome emerging resistance. Notably, modifications that allow INH to directly show its antimycobacterial effect without necessitating KatG activation or avoid the hydrazide functionality from acetylation can provide a new avenue for antitubercular drug development [19].
Prompted by these considerations, we set out with the goal of developing new antitubercular agents (SIH1–SIH13) by linking INH to various sulfonate esters that were also reported to exhibit antitubercular activities [20,21] via hydrazone bridge (Figure 3). When choosing the substituents on the sulfonate moiety, we mainly modified the para position of the terminal phenyl ring with various different groups including alkyl, aryl, acyl, halogen, and nitro. In this way, we made sure that the antitubercular activity was due to the substituent type independent from the position. Additionally, we carried out some additional chemical modifications (introducing two halogens, adding more alkyl groups, condensing phenyl to a heterocyclic ring, or changing the position of nitro group) to see how they will affect antimycobacterial activity and to establish preliminary structure-activity relationships for this class of compounds. Subsequently, we tested the antimycobacterial potency of these compounds against the reference Mtb strain H37Rv as well as against INH-resistant clinical isolates carrying katG and inhA promoter mutations.
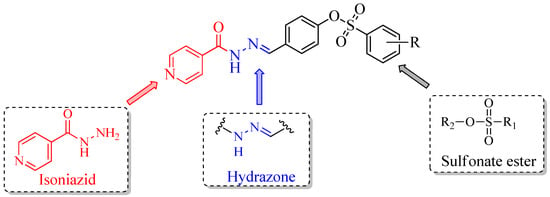
Figure 3.
Design strategy of the studied molecules SIH1–SIH13.
2. Results and Discussion
2.1. Chemistry
The synthesis and chemical structures of the new isoniazid derivatives (SIH1–SIH13) are outlined in Scheme 1. The key intermediates, 4-formylphenyl benzenesulfonates, (III) were prepared through the reaction of aromatic sulfonyl chlorides (I) with 4-hydroxybenzaldehyde (II) in DMF in the presence of triethyl amine (TEA). Our target compounds (SIH1–SIH13) were obtained in 47–77 % yield by refluxing 4-formylphenyl benzenesulfonates (III) and isoniazid (IV) in ethanol in the presence of a catalytic amount of glacial acetic acid.
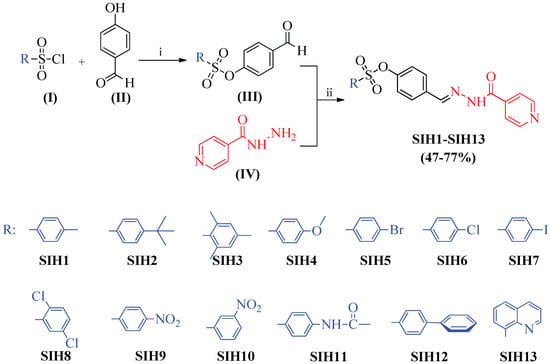
Scheme 1.
Reagents and conditions: (i) TEA/DMF, rt, (ii) EtOH/AcOH, reflux.
The structures of the newly synthesized compounds (SIH1–SIH13) were confirmed by their infrared (IR), 1H NMR, 13C NMR, and HRMS spectral data. In IR spectra, SIH1–SIH13 were characterized by the appearance of absorption bands in the range of 3396–3248 cm−1, 1607–1596 cm−1, and 1676–1651 cm−1 due to N-H, C=N, and C=O stretching vibrations, respectively. Besides these, two characteristic bands for the SO2 stretches were observed in the ranges of 1352–1335 and 1143–1152 cm−1. Furthermore, 1H NMR spectra of the compounds displayed two singlets at 12.21–12.11 ppm (O=C-NH) and 8.46–8.37 ppm (N=CH), respectively. According to the literature, the presence of a singlet downfield resonating (8.46–8.37 ppm) N=CH signal, exclusively accounts for the formation of E-isomers [22]. In addition, 13C NMR spectra of the molecules showed a smaller number of resonances than the exact number of carbons due to the overlapped peaks in the aromatic field. The 13C NMR spectra exhibit the C=O signal at 162.4–162.1 ppm and C=N signal at 140.7–140.8 ppm, confirming the N-acylhydrazone skeleton in the chemical structures of SIH1–SIH13. 1H NMR, 13C NMR, HRMS, and FTIR spectra of the final compounds are provided in Supplementary Material.
2.2. Antitubercular Activity Evaluation and Cytotoxicity Assessment
We tested the antimycobacterial activity of all the compounds obtained against Mtb H37Rv and two INH-resistant clinical isolates (katG and inhA promoter mutants) by applying the Microplate Alamar Blue Assay (MABA) protocol. As toxicity to healthy host cells is a significant barrier to launching new antitubercular drugs, we additionally assessed the cytotoxicity of our compounds against three different cell lines: human embryonic kidney (HEK) 293, human lung cells IMR-90, and human epithelial bronchus cells BEAS-2B. Minimum inhibitory concentration (MIC) values against three Mtb strains tested as well as toxicity data of SIH1–SIH13 are provided in Table 1.

Table 1.
MIC values against Mtb H37Rv and INH-resistant clinical isolates, and cytotoxicity data of SIH1–SIH13.
Based on the activity analyses, four compounds (SIH1, SIH4, SIH12, and SIH13) exhibited MIC values of 0.31 μM against Mtb H37Rv. The other molecules in this series were also efficient as antitubercular agents with MIC values of 0.62 μM. As expected, the MIC values of INH against two defined INH-resistant (inhA promoter mutant and katG S315T mutant) clinical isolates were found to be higher than the value obtained for INH-sensitive Mtb H37Rv. Against the inhA mutant INH-resistant Mtb clinical isolate, SIH1, SIH2, and SIH4 were effective with MIC values of 1.56. Except for two compounds, SIH5 and SIH6 (MIC = 6.25 μM), the remaining compounds displayed antimycobacterial activity with MIC values of 3.12 μM. SIH1–SIH13 were also screened against the other INH-resistant Mtb isolate with katG mutation. Among them, SIH4 was the most effective compound with a MIC value of 6.25 μM which was the same value as calculated for INH. Excluding SIH6 and SIH7, other molecules also represented antitubercular activity with MIC values ranging between 12.5 and 50 μM against katG mutant Mtb clinical isolate.
When the molecules were examined in terms of their chemical structures, it is noteworthy that SIH4 with p-methoxy group on its phenyl ring was the most attractive compound showing the lowest MIC values against all the Mtb strains tested. Moreover, the other most active compounds against Mtb H37Rv carry a methyl (SIH1) or a phenyl (SIH12) group, or a condensed pyridine ring (SIH13) on their terminal phenyl rings. For the inhibition of inhA mutant Mtb strains, methyl (SIH1), t-butyl (SIH2), and methoxy (SIH4) on the para position of the phenyl ring were the most preferential substituents. As extensive molecular modifications were carried out on the phenyl ring of sulfonate esters, it can be concluded that the changes in substituent types, positions, and volumes can easily be tolerated on this scaffold for antitubercular activity.
Furthermore, based on the cytotoxicity data obtained from the colorimetric MTT assay, the compounds were found to be non-toxic against lung cell lines IMR-90 and BEAS-2B. Only SIH12 was slightly toxic towards IMR-90 with IC50 value of 57.7 μM. Against HEK293, except for SIH1, SIH4, SIH12, and SIH13 that were moderately toxic, our compounds did not present cytotoxicity. As TB predominantly is a respiratory disease, it is critical that we identified effective antimycobacterial drug candidates with favorable toxicity profiles, especially against the lung cells included in this study.
2.3. Stability Studies in Water and DMSO
Imine formations are well-known reversible condensation reactions [23]. Solvent type is one of the factors that need to be taken into account while assessing the stability of imines [24]. In the presence of water, the equilibrium may shift in favor of precursors and the target compounds to be tested in activity assays may be misinterpreted. Therefore, we tested the stability of our compounds under aqueous conditions to confirm the stability of the hydrazone functionality. In this way, we could make sure that the antitubercular activity of the molecules studied is not due to INH as one of the hydrolysis products of our compounds. Furthermore, the stability of the selected compounds was also assessed in DMSO, the solvent used in the biological experiments.
Accordingly, we performed stabilization tests for four selected compounds (SIH1, SIH4, SIH12, and SIH13) in both aqueous medium and DMSO by using UV/Vis spectroscopy. These representative compounds were selected based on their low MIC values against Mtb H37Rv strain. Samples with a concentration of 6.0 × 10–5 M were prepared in DMSO and a 28% ethanol-water mixture. The change in λmax values throughout 24 h in the selected solvents was monitored to assess the stability of the hydrazone functionality. As expected, no significant change in λmax values was observed for the compounds. UV/Vis absorption spectra of SIH13 in DMSO and ethanol-water are provided in Figure 4. The results for SIH1, SIH4, and SIH12 are reported in the Supplementary Material.
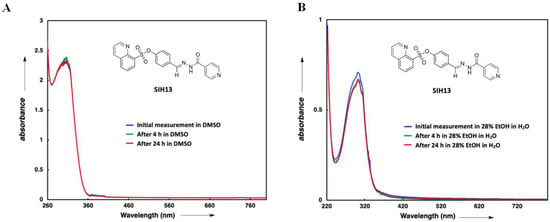
Figure 4.
Stability assessment of SIH13 in DMSO (A) and ethanol-water mixture (B).
2.4. InhA Inhibition
INH principally targets the InhA enzyme that is responsible for the biosynthesis of long-chain fatty acids in Mtb. Fatty acids, particularly mycolic acids, play a crucial role in the survival of Mtb since they are structural components of the bacterial cell wall [25]. Following the activation by KatG, INH produces a reactive isonicotinoyl-radical intermediate that quickly forms a covalent adduct with the InhA cofactor NADH [6]. As mutations in katG reduce the activation of INH and thus yield the most prevalent type of INH resistance, developing direct InhA inhibitors that do not require KatG activation appears as an effective and rational strategy to overcome this resistance problem [26]. Therefore, we screened our INH-based compounds against InhA to determine if they show their antimycobacterial activity via direct inhibition of this enzyme (Table 2).

Table 2.
Inhibitory results for SIH1–SIH13 against InhA enzyme at 50 µM concentration.
Although most of the molecules are recognized by the binding pocket of InhA, our compounds do not primarily represent their antitubercular activity by inhibiting InhA enzyme directly. SIH7 was found to be a moderate inhibitor of InhA with 41% inhibition. As the main structural difference between the tested compounds is the substituent type and position on the phenyl ring of the sulfonate moiety, it is noteworthy that introducing iodine as a bulky and lipophilic halogen can be an important modification to bind to the active site of the enzyme. These data can be used useful for the design of effective antimycobacterial INH derivatives that are also capable of inhibiting InhA.
2.5. Molecular Modeling Studies
2.5.1. Molecular Docking
The active pocket of InhA is large enough to accommodate various direct inhibitors with different chemical scaffolds such as diphenyl ethers, 4-hydroxy-2-pyridones, benzamides, and thiadiazoles [27,28]. Despite this flexibility, in almost every case, the direct inhibitors block the enzyme via forming two key hydrogen bonds to Tyr158 and nicotinamide adenine dinucleotide (NAD) cofactor of InhA. Additional hydrophobic interactions are also required with the terminal lipophilic pockets of the binding site [29]. To rationalize the obtained data and explain the binding mode of our compounds to InhA, we carried out in silico studies. We docked SIH7 into the binding pocket of InhA and compared its interactions to those of GEQ/Genz-10850, a direct inhibitor co-crystallized within the enzyme. The binding modes and the interactions of the compounds within the active pocket of InhA are provided in Supplementary Materials.
2.5.2. In Silico Prediction of Drug-Likeness
The unsuitable physicochemical profiles of drug candidate molecules can be a serious obstacle in the drug development process for the conversion of bioactive compounds into drugs. Thus, we performed theoretical calculations to identify drug-like properties of our compounds. We started with computing the descriptors that constitute the Lipinski’s rule of five. This rule finds out if a chemical compound with preferable biological profile possesses suitable physicochemical properties that make it orally active in humans. Accordingly, to show oral bioavailability, a molecule should not breach more than one of the following requirements: molecular weight (MW) ≤ 500, n-octanol/water partition coefficient (log P) ≤ 5, number of hydrogen bond donors (HBD) ≤ 5 and number of hydrogen bond acceptors (HBA) ≤ 10 [30]. Furthermore, we predicted the compounds’ topological polar surface areas (TPSAs) and numbers of rotatable bonds (NRBs), both of which are regarded to be crucial characteristics for predicting the oral bioavailability of novel molecules [31]. The predicted physicochemical descriptors of SIH1–SIH13 are presented in Table 3.

Table 3.
Calculated molecular properties of SIH1–SIH13.
Based on the estimated parameters, all compounds, except for SIH7, were shown to entirely follow Lipinski’s rule of five. SIH7 displays only one violation with a molecular weight of slightly more than 500. Furthermore, according to the calculated LogP values, the compounds are highly lipophilic compared to INH (LogP = −0.35, calculated in SwissADME). Besides mutations in either katG or the inhA promoter, this low hydrophobicity of INH is linked to the long duration of TB treatment [32]. The mycolic acid outer layer of Mtb is so lipophilic that INH cannot efficiently penetrate and cross it. The permeability of INH in the Mtb granuloma is also low due to its hydrophilic character [33]. Therefore, in this study, we succeeded in increasing the lipophilicity of INH with suitable chemical modifications to enhance its ability to diffuse through the cell membrane. The number of rotatable bonds, a significant descriptor of molecular flexibility, should be less than ten to keep conformational changes at minimum during the interactions with the biological targets. SIH1–SIH13 follow this criterion as they all have ≤10 rotatable bonds. Additionally, TPSA of the compounds varied between 106.10 and 151.92 Å2. Most of the clinically used drug molecules have TPSA less than 140–150 Å2 [34], so our molecules stay in the acceptable range although the values calculated for SIH9 and SIH10 are slightly higher than 150 Å2.
Consequently, the physicochemical properties of SIH1–SIH13 support their potential position as relevant candidates in the antimycobacterial drug development process.
3. Material and Methods
3.1. Chemistry
3.1.1. Experimental
All the chemicals used in this study were purchased from commercial sources and were used without further purification. The completion of reactions and purities of the final compounds were monitored by thin layer chromatography (TLC) using Silica Gel 60 F254 TLC plate (Merck, Darmstadt, Germany). The Rf values of all the synthesized compounds were determined using ethyl acetate:n-hexane:methanol (7:2:1) as mobile phase. The melting points were determined by using Thomas Hoover Capillary Melting Point Apparatus (Philadelphia, PA, USA) and were uncorrected. Infrared (IR) spectra were obtained on Perkin Elmer Spectrum BX FT-IR (Beaconsfield, UK) and reported in the range of 4000–400 cm−1 using ATR accessory (Pike Technologies) with a diamond ATR crystal. The NMR spectra were recorded by Bruker spectrometer. 1H NMR spectra were run at 400 MHz, while 13C NMR spectra were run at 100 MHz in deuterated dimethyl sulfoxide (DMSO-d6). Chemical shifts (δH) and (δC) are expressed in values (ppm) using the solvent peak as the internal standard. All coupling constant (J) values are given in Hertz.
3.1.2. Synthesis
Preparation of aromatic aldehydes (III): Sulfonyl chlorides (1 mmol) and 4-hydroxybenzaldehyde (1.1 mmol) were mixed in DMF (20 mL) for 24 h at room temperature in the presence of triethylamine (1.35 mL). After pouring the mixture into ice, the resulting precipitate was filtered, washed with water, dried, and crystallized from ethanol [35].
General procedure for the synthesis of the target compounds SIH1–SIH13: A mixture of appropriate 4-formylphenyl substituted benzenesulfonate (0.5 mmol) and isoniazid (0.5 mmol) was refluxed with 5 drops of acetic acid in 15 mL methanol for 8 h. After completion of the reaction, the mixture was cooled and the precipitated solid was filtered, dried, and recrystallized from methanol (SIH1-SIH7, SIH11-SIH13) or methanol-ether (8:2) (SIH8-SIH10) [13].
3-((2-Isonicotinoylhydrazono)methyl)phenyl 4-methylbenzenesulfonate (SIH1): White solid, yield: 52% (205 mg). m.p. 209–210 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.36. IR (ν, cm−1): 3323 (N-H), 1676 (C=O), 1592 (C=N), 1371, and 1152 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.14 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.5 Hz, 2H, Ar-H), 8.42 (s, 1H, =CH), 7.81 (d, J= 4.5 Hz, 2H, Ar-H), 7.75 (d, J = 8.0 Hz, 4H, Ar-H), 7.48 (d, J = 7.9 Hz, 2H, Ar-H), 7.13 (d, J = 8.4 Hz, 2H, Ar-H), 2.42 (s, 3H, CH3); 13C NMR (100 MHz, DMSO-d6) δ 162.2 (C=O), 150.8, 150.6, 147.9, 146.5, 140.8 (-C=N), 133.6, 131.6, 130.8, 129.3, 128.7, 123.1, 121.9, 21.6 (-CH3); HRMS: m/z calcd for C20H17N3O4S [M + H]+: 396.1018; found 396.1015.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 4-(tert-butyl)benzenesulfonate (SIH2): White solid, yield: 64% (280 mg). m.p. 182–183 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.46. IR (ν, cm−1): 3303 (N-H), 1663 (C=O), 1596 (C=N), 1365, and 1152 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.14 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.6 Hz, 2H, Ar-H), 8.43 (s, 1H, =CH), 7.82–7.80 (m, 4H, Ar-H), 7.76 (d, J = 8.1 Hz, 2H), 7.70 (d, J = 8.3 Hz, 2H), 7.15 (d, J = 8.2 Hz, 2H, Ar-H), 1.31 (s, 9H, CH3); 13C NMR (100 MHz, DMSO-d6) δ 162.2 (C=O), 158.9, 150.8, 150.6, 148.0, 140.8 (-C=N), 133.6, 131.9, 129.3, 128.6, 127.2, 123.0, 122.0, 35.6 (-C-(CH3)3), 31.1 (-CH3); HRMS: m/z calcd for C23H23N3O4S [M + H]+: 438.1488; found 438.1482.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 2,4,6-trimethylbenzenesulfonate (SIH3): Yellow solid, yield: 47% (199 mg). m.p. 108–109 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.43. IR (ν, cm−1): 3396 (N-H), 1661 (C=O), 1600 (C=N), 1360, and 1152 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.13 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.4 Hz, 2H, Ar-H), 8.41 (s, 1H, =CH), 7.80 (d, J = 4.6 Hz, 2H, Ar-H), 7.74 (d, J = 8.0 Hz, 2H, Ar-H), 7.16 (s, 2H, Ar-H), 7.09 (d, J = 8.1 Hz, 2H, Ar-H), 2.48 (s, 6H, CH3), 2.31 (s, 3H, -CH3); 13C NMR (100 MHz, DMSO-d6) δ 162.2 (C=O), 150.8, 150.4, 148.0, 144.9, 140.8 (-C=N), 140.3, 133.6, 132.4, 129.8, 129.3, 122.9, 121.9, 22.6 (2x-CH3), 21.06 (-CH3); HRMS: m/z calcd for C22H21N3O4S [M + H]+: 424.1331; found 424.1323.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 4-methoxybenzenesulfonate (SIH4): White solid, yield: 71% (296 mg). m.p. 194–195 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.33. IR (ν, cm−1): 3288 (N-H), 1665 (C=O), 1596 (C=N), 1369, and 1152 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.14 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.5 Hz, 2H, Ar-H), 8.43 (s, 1H, =CH), 7.74–7.81 (m, 6H, Ar-H), 7.17 (d, J = 8.2 Hz, 2H, Ar-H), 7.12 (d, J = 8.1 Hz, 2H, Ar-H), 3.87 (s, 3H, -OCH3); 13C NMR (100 MHz, DMSO-d6) δ 164.6, 162.2 (C=O), 150.8, 150.0, 148.0, 140.8 (-C=N), 133.6, 131.2, 129.3, 125.8, 123.2, 121.9, 115.5, 56.4 (-OCH3); HRMS: m/z calcd for C20H17N3O5S [M + H]+: 412.0967; found 412.0959.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 4-bromobenzenesulfonate (SIH5): White solid, yield: 61% (279 mg). m.p. 217–218 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.42. IR (ν, cm−1): 3306 (N-H), 1673 (C=O), 1599 (C=N), 1379, and 1150 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.15 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.4 Hz, 2H, Ar-H), 8.43 (s, 1H, =CH), 7.90 (d, J = 7.7 Hz, 2H, Ar-H), 7.81–7.77 (m, 6H, Ar-H), 7.16 (d, J = 7.9 Hz, 2H, Ar-H); 13C NMR (100 MHz, DMSO-d6) δ 162.2 (C=O), 150.8, 150.4, 147.9, 140.8 (-C=N), 133.9, 133.8, 133.5, 130.6, 129.9, 129.4, 123.1, 121.9, HRMS: m/z calcd for C19H14BrN3O4S [M + H]+: 459.9967; found 459.9965.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 4-chlorobenzenesulfonate (SIH6): Yellow solid, yield: 55% (228 mg). m.p. 210–211 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.43. IR (ν, cm−1): 3357 (N-H), 1665 (C=O), 1602 (C=N), 1368, and 1149 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.15 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.9 Hz, 2H, Ar-H), 8.43 (s, 1H, =CH), 7.89 (d, J = 8.1 Hz, 2H, Ar-H), 7.82–7.75 (m, 6H, Ar-H), 7.16 (d, J = 7.9 Hz, 2H, Ar-H); 13C NMR (100 MHz, DMSO-d6) δ 162.2 (C=O), 150.8, 150.4, 147.9, 140.8 (-C=N), 140.7, 133.9, 133.4, 130.7, 130.6, 129.4, 123.1, 121.9; HRMS: m/z calcd for C19H14ClN3O4S [M + H]+: 416.0472; found 416.0463.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 4-iodobenzenesulfonate (SIH7): Pale yellow solid, yield: 65% (329 mg). m.p. 240–241 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.44. IR (ν, cm−1): 3263 (N-H), 1660 (C=O), 1599 (C=N), 1378, and 1151 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.15 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.1 Hz, 2H, Ar-H), 8.43 (s, 1H, =CH), 8.07 (d, J = 7.2 Hz, 2H, Ar-H), 7.82–7.76 (m, 4H, Ar-H), 7.62 (d, J = 7.7 Hz, 2H, Ar-H), 7.16 (d, J = 7.9 Hz, 2H, Ar-H); 13C NMR (100 MHz, DMSO-d6) δ 162.2 (C=O), 150.8, 150.4, 147.9, 140.8 (-C=N), 139.3, 134.1, 133.9, 130.1, 129.4, 123.1, 121.9, 104.9; HRMS: m/z calcd for C19H14lN3O4S [M + H]+: 507.9828; found 507.9814.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 2,5-dichlorobenzenesulfonate (SIH8): Yellow solid, yield: 59% (265 mg). m.p. 177–178 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.42. IR (ν, cm−1): 3303 (N-H), 1667 (C=O), 1598 (C=N), 1390, and 1143 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.21 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.8 Hz, 2H, Ar-H), 8.46 (s, 1H, =CH), 7.93–7.78 (m, 7H, Ar-H), 7.25 (d, J = 8.3 Hz, 2H, Ar-H); 13C NMR (100 MHz, DMSO-d6) δ 162.2 (C=O), 150.8, 150.1, 147.9, 140.7 (-C=N), 136.9, 134.8, 134.1, 133.2, 131.7, 131.2, 129.6, 122.7, 122.0, 121.5; HRMS: m/z calcd for C19H13Cl2N3O4S [M + H]+: 450.0082; found 450.0076.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 4-nitrobenzenesulfonate (SIH9): White solid, yield: 77% (328 mg). m.p. 211–212 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.51. IR (ν, cm−1): 3248 (N-H), 1663 (C=O), 1602 (C=N), 1379, and 1147 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.17 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.5 Hz, 2H, Ar-H), 8.46 (d, J = 8.3 Hz, 2H, Ar-H), 8.43 (s, 1H, =CH), 8.17 (d, J = 8.1 Hz, 2H, Ar-H), 7.81–7.77 (m, 4H, Ar-H), 7.18 (d, J = 8.0 Hz, 2H, Ar-H); 13C NMR (100 MHz, DMSO-d6) δ 162.4 (C=O), 151.6, 150.8, 150.2, 148.0, 140.7 (-C=N), 139.7, 133.9, 130.5, 129.6, 125.5, 123.1, 122.0; HRMS: m/z calcd for C19H14N4O6S [M + H]+: 427.0707; found 427.0685.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 3-nitrobenzenesulfonate (SIH10): White solid, yield: 64% (264 mg). m.p. 203–204 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.58. IR (ν, cm−1): 3267 (N-H), 1651 (C=O), 1607 (C=N), 1379, and 1148 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.17 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.8 Hz, 2H, Ar-H), 8.66 (d, J = 8.0 Hz, 1H, Ar-H), 8.50 (s, 1H, Ar-H), 8.43 (s, 1H, =CH), 8.29 (d, J = 8.1 Hz, 1H, Ar-H), 7.97 (t, J = 8.0 Hz, 1H, Ar-H), 7.81–7.76 (m, 4H, Ar-H), 7.22 (d, J = 8.1 Hz, 2H, Ar-H); 13C NMR (100 MHz, DMSO-d6) δ 162.2 (C=O), 150.8, 150.2, 148.6, 147.9, 140.8 (-C=N), 135.8, 134.6, 134.1, 132.5, 130.2, 129.5, 123.5, 123.3, 122.0; HRMS: m/z calcd for C19H14N4O6S [M + H]+: 427.0707; found 427.0682.
3-((2-Isonicotinoylhydrazono)methyl)phenyl 4-acetamidobenzenesulfonate (SIH11): White solid, yield: 68% (298 mg). m.p. 193–194 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.35. IR (ν, cm−1): 3257 (N-H), 1670 (C=O), 1597 (C=N), 1352, and 1147 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.13 (s, 1H, -NH, D2O exchangeable) 10.50 (s, 1H, -NH), 8.77 (d, J = 3.8 Hz, 2H, Ar-H), 8.42 (s, 1H, =CH), 7.82–7.74 (m, 8H, Ar-H), 7.12 (d, J = 8.0 Hz, 2H, Ar-H), 2.10 (s, 3H, -CH3); 13C NMR (100 MHz, DMSO-d6) δ 169.9 (C=O), 162.2 (C=O), 150.8, 150.6, 148.1, 145.5, 140.8 (-C=N), 133.6, 130.2, 129.3, 127.5, 123.2, 121.9, 119.2, 24.7 (-CH3); HRMS: m/z calcd for C21H18N4O5S [M + H]+: 439.1076; found 439.1066.
3-((2-Isonicotinoylhydrazono)methyl)phenyl [1,1′-biphenyl]-4-sulfonate (SIH12): Orange solid, yield: 53% (242 mg).. m.p. 118–119 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.44. IR (ν, cm−1): 3382 (N-H), 1660 (C=O), 1596 (C=N), 1372, and 1151 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.16 (s, 1H, -NH, D2O exchangeable), 8.78 (d, J = 4.7 Hz, 2H, Ar-H), 8.43 (s, 1H, =CH), 8.00–7.94 (m, 4H, Ar-H), 7.81–7.77 (m, 5H, Ar-H), 7.55–7.45 (m, 4H, Ar-H), 7.19 (d, J = 8.3 Hz, 2H, Ar-H); 13C NMR (100 MHz, DMSO-d6) δ 162.2 (C=O), 150.8, 150.5, 148.0, 146.8, 140.8 (-C=N), 138.2, 133.7, 133.2, 129.7, 129.6, 129.4, 128.3, 127.7, 127.5, 123.6, 121.9; HRMS: m/z calcd for C25H19N3O4S [M + H]+: 458.1175; found 458.1166.
3-((2-Isonicotinoylhydrazono)methyl)phenyl quinoline-8-sulfonate (SIH13): White solid, yield: 72% (327 mg). m.p. 231–232 °C. Rf (EtOAc:n-Hexane:MeOH = 7:2:1): 0.22. IR (ν, cm−1): 3294 (N-H), 1670 (C=O), 1598 (C=N), 1359, and 1142 (SO2 stretch). 1H NMR (400 MHz, DMSO-d6) δ 12.11 (s, 1H, -NH, D2O exchangeable), 9.23 (s, 1H, Ar-H), 8.77 (d, J = 4.2 Hz, 2H, Ar-H), 8.64 (d, J = 8.2 Hz, 1H, Ar-H), 8.47 (d, J = 8.1 Hz, 1H, Ar-H), 8.39 (d, J = 4.9 Hz, 1H, Ar-H), 8.37 (s, 1H, =CH), 7.82–7.77 (m, 4H, Ar-H), 7.68 (d, J = 8.2 Hz, 2H, Ar-H), 7.10 (d, J = 8.2 Hz, 2H, Ar-H); 13C NMR (100 MHz, DMSO-d6) δ 162.1 (C=O), 152.9, 150.9, 150.8, 148.0, 143.5, 140.8 (-C=N), 137.7, 136.9, 134.5, 133.4, 131.7, 129.2, 126.2, 123.6, 122.9, 122.5, 121.9; HRMS: m/z calcd for C22H16N4O4S [M+Na]+: 455.0790; found 455.0788.
3.2. Microplate Alamar Blue Assay (MABA) Protocol
Mycobacterium tuberculosis H37Rv (Mtb) obtained from the American Type Culture Collection (ATCC) and drug-resistant clinical isolates from Oslo University Hospital were streaked onto 7H10+OADC agar plates and incubated at 37 °C. In OADC-enriched liquid Middlebrook 7H9 medium, pure colonies from agar plates were grown to the middle of the log phase. Subsequently, Mtb cultures were exponentially grown and inoculated into Middlebrook 7H9 medium on 96-well plates at progressively higher concentrations of the testing chemicals, with approximately 4 × 105 CFU/mL in 200 µL of each well. Before receiving 32.5 µL of a resazurin-tween mixture (8:5 ratio of 0.6 mM Resazurin in 1× PBS to 20% Tween 80), plates were incubated at 37 °C for one week. The production of fluorescent resorufin assists in determining the minimum inhibitory concentration (MIC) of the compounds tested [13].
3.3. Cytotoxicity Protocol
The MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) test was used to assess the cytotoxicity of the compounds against the cell lines Human Embryonic Kidney cells (HEK 293), Normal Lung Fibroblasts (IMR-90), and Human non-tumorigenic lung epithelial cells (BEAS-2B). All cell lines were obtained from ATCC. When testing compounds SIH1–SIH13, they were added by the use of double dilution across 6 dosages ranging from 100 µM to 3.12 µM to a sterile 96 well microtiter plate containing 1 × 104 cells/well and cultured for 48 h at 37 °C with 5% CO2. The medium was removed, and 10 µL of MTT reagent (5 mg/mL) was added to the wells and incubated for another 3 h. The MTT reagent was then removed, and 100 µL of DMSO was added into each well. DMSO dissolves the formazan crystals that have formed in the wells. The absorbance was measured at 580 nm against a blank using the Thermo Scientific varioskan lux microplate reader, and the IC50 values were calculated by using GraphPad Prism [36,37].
3.4. Stability Studies
The T80+ series of UV/Vis Spectrophotometers (PG Instruments Ltd.) were used for stability assessment studies. The stability experiments were performed at 25 °C with wavelength ranges of 260–800 nm. DMSO and EtOH were purchased as reagent grade and used without any purification. Samples with a concentration of 6.0 × 10–5 M were prepared in DMSO and EtOH-water. The change in λmax values throughout the 24 h in the selected solvents was monitored to assess the stability of the hydrazone moieties.
3.5. InhA Inhibition
3.5.1. Production and Purification of InhA
InhA sequence (UniProtKB: P9WGR1) has been optimized for Escherichia coli BL21 DE3 strain with GenSmart™ Codon Optimization (GenScript) and inserted in pET15b plasmid using the NdeI and BamHI restriction sites. BL21 (DE3) strains have been transformed with pET15b-InhA plasmid. A colony from this transformation was grown in LB medium containing 100 mg/mL ampicillin at 37 °C 180 rpm overnight. Then, 10 mL of this solution was added to 990 mL of LB medium containing ampicillin (100 mg/mL) and incubated at 37 °C 150 rpm until an optical density (OD) at 600 nm of 0.6–0.8 was reached. Once the OD600 was reached, 1 mL of 1 M isopropyl β-D-1-thiogalactopyranoside (IPTG) was added and the solution was incubated at 30 °C for 4 h at 150 rpm. Bacteria cells were collected by centrifugation at 6000× g for 30 min at 4 °C. Cells from pellets were solubilized with buffer (20 mM Tris-HCl, 300 mM NaCl, 10 mM imidazole, pH 7.9) and lysed using an Emulsiflex-C5 cell disruptor (Avestin). The lysate was centrifuged at 25,000× g for 30 min at 4 °C, the supernatant was filtered off with a 0.2 µm filter and injected into a nickel-chelated Hi-Trap HP 1 mL (Cytiva) column previously equilibrated with washing buffer (20 mM Tris-HCl, 300 mM NaCl, 10 mM imidazole, pH 7.9). After washing out the unbound proteins, bound His6-InhA was eluted using a buffer with higher imidazole concentration (20 mM Tris-HCl, 300 mM NaCl, 300 mM imidazole, pH 7.9). Fractions corresponding to His6-InhA were pooled together and concentrated using centrifugal concentrator (Vivaspin 10,000 MWCO). Then, the concentrated protein solution was centrifuged at 10,000× g for 10 min at 4 °C to remove aggregates and injected into a SepFast 16/60 6–600 kDa pg column (BioToolomics) previously equilibrated with buffer (30 mM PIPES, 150 mM NaCl, pH 6.8). Fractions corresponding to His6-InhA were pooled together then aliquots of 200 µL at 5 µM were prepared followed by flash freezing in liquid nitrogen. Frozen His6-InhA proteins were stored at −80 °C until usage.
3.5.2. Enzymatic Assay
InhA activity assays were monitored by following NADH concentration at 340 nm with a Cary 300 UV-vis (Agilent) spectrophotometer. As described previously [38], 2-trans-dodecenoyl-CoA (DDCoA) was used as an analogue of the substrate for this reaction. Briefly, to 840 µL of buffer (30 mM PIPES, 150 mM NaCl, pH 6.8) in 1 mL cuvette, inhibitor in DMSO at constant 5% v/v of DMSO (50 µL), 50 µL DDCoA of 1 mM stock in buffer and 50 µL of NADH (Alfa Aesar) of 5 mM stock in buffer were added. After a short period of 2 min pre-incubation at 25 °C, the reaction was started by the addition of 10 µL His6-InhA from a 5 µM stock solution prepared as explained before. Rate of NADH oxidation during His6-InhA activity is monitored in the presence or in the absence of inhibitor. The inhibitory activity of tested molecules is expressed as the percentage inhibition of His6-InhA activity (with respect to control reaction) without inhibitor, as shown below. All activity assays were performed in duplicate or triplicate.
3.6. In Silico Studies
3.6.1. Molecular Docking
The 3D crystal structure of Mycobacterium tuberculosis enoyl-ACP reductase (InhA) with its native inhibitor GEQ, (4-(9H-fluoren-9-yl)piperazin-1-yl)(1H-indol-5-yl)methanone, was downloaded from Protein Data Bank under the PDB Code 1P44 [39]. The chemical structure of SIH7 showing the best inhibition value against InhA among the tested compounds was sketched and MMFF94 force field in LigandScout 4.4 was used to minimize the energy of the 3D structure [40]. SIH7 was docked into the binding pocket of InhA with default parameters of AutoDock [41], implemented in LigandScout 4.4. The obtained modes were ranked based on their estimated binding energies and the figures of the most plausible binding pose were generated using LigandScout and Maestro [42].
3.6.2. Prediction of Drug-Likeness
The chemical structures of all compounds were drawn and their significant parameters were predicted by using SwissADME [43].
4. Conclusions
The rapid emergence and global spread of drug-resistant strains of Mtb have once again made TB an urgent concern to human health around the world. Particularly, the resistance developed against INH, as the frontline drug of TB treatment, has appeared as a significant handicap to controlling the global prevalence of the disease. In this study, we focused on the chemical modifications of inexpensive INH to provide a new route towards the antitubercular drug development process. Accordingly, we synthesized new INH derivatives by linking this scaffold to sulfonate esters with a hydrazone functionality (SIH1–SIH13). We established the stability of the compounds both in DMSO and water to eliminate the possibility that the antitubercular effect was due to INH released by hydrolyzation during biological experiments. The antitubercular and toxicity data obtained from MABA and MTT assays respectively confirmed the potential of the compounds in TB treatment. Testing the inhibitory activity of SIH1–SIH13 against InhA, the primary target of INH, showed that our compounds can be hosted within the binding pocket of the enzyme. However, the antimycobacterial activity was not mainly due to InhA inhibition. Calculating some critical physicochemical descriptors of the compounds confirmed their drug-likeness and emphasized the importance of the increased lipophilicity in the biological profile of SIH1–SIH13 as compared to INH. Altogether, our study presented a new approach for modifying INH to overcome the challenging drug resistance problem in TB treatment.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ph15101301/s1, 1H NMR, 13C NMR, FTIR, and HRMS spectra of all synthesized compounds, InhA optimised sequence, UV/Vis spectra of SIH1, SIH4, and SIH12 in DMSO and EtOH-water, and molecular docking figures and discussion are provided.
Author Contributions
Conceptualization, Ş.D.D. and M.G.G.; Investigation, E.K.A., M.İ.H., V.S.K., R.T. and C.D.; Data curation, E.K.A., M.İ.H., V.S.K. and R.T.; Formal analysis, E.K.A., M.İ.H., V.S.K., R.T. and C.D.; Supervision, Ş.D.D., M.G.G., C.L., L.M. and T.T.; Funding acquisition, T.T. and M.G.G.; Writing original draft, M.İ.H., E.K.A., M.G.G., C.D., V.S.K. and R.T.; Writing-review & editing, Ş.D.D., C.L., L.M., T.T. and M.G.G. All authors have read and agreed to the published version of the manuscript.
Funding
T.T. acknowledges the financial support provided by the Research Council of Norway (RCN project numbers #234506, #261669 and #309592) and JPIAMR (RCN project number #298410). M.G.G. acknowledges the financial support provided by the BAGEP Award of the Science Academy.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article or Supplementary Materials.
Acknowledgments
M.G.G. also would like to thank Gerhard Wolber, Freie Universität Berlin, for providing the license for LigandScout 4.4. RT thanks Université Fédérale Toulouse Midi-Pyrénées and Occitanie region for PhD grant.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Migliori, G.B.; Ong, C.W.M.; Petrone, L.; D’ambrosio, L.; Centis, R.; Goletti, D. The definition of tuberculosis infection based on the spectrum of tuberculosis disease. Breathe 2021, 17, 210079. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Tuberculosis Report. 2020. Available online: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2020 (accessed on 5 June 2022).
- Pontali, E.; Raviglione, M.C.; Migliori, G.B.; Akkerman, O.W.; Alffenaar, J.W.; Blanc, F.X.; Borisov, S.; Cirillo, D.M.; Dalcolmo, M.; Dheda, K.; et al. Regimens to treat multidrug-resistant tuberculosis: Past, present and future perspectives. Eur. Respir. Rev. 2019, 28, 190035. [Google Scholar] [CrossRef] [PubMed]
- Khawbung, J.L.; Nath, D.; Chakraborty, S. Drug resistant Tuberculosis: A review. Comp. Immunol. Microbiol. Infect. Dis. 2021, 74, 101574. [Google Scholar] [CrossRef] [PubMed]
- Vilchèze, C.; Jacobs, W.R. The Isoniazid Paradigm of Killing, Resistance, and Persistence in Mycobacterium tuberculosis. J. Mol. Biol. 2019, 431, 3450–3461. [Google Scholar] [CrossRef] [PubMed]
- Reingewertz, T.H.; Meyer, T.; McIntosh, F.; Sullivan, J.; Meir, M.; Chang, Y.F.; Behr, M.A.; Barkana, D. Differential sensitivity of mycobacteria to isoniazid is related to differences in katg-mediated enzymatic activation of the drug. Antimicrob. Agents Chemother. 2020, 64, e01899-19. [Google Scholar] [CrossRef]
- de Ávila, M.B.; Bitencourt-Ferreira, G.; de Azevedo, W.F. Structural Basis for Inhibition of Enoyl-[Acyl Carrier Protein] Reductase (InhA) from Mycobacterium tuberculosis. Curr. Med. Chem. 2018, 27, 745–759. [Google Scholar] [CrossRef]
- Bollela, V.R.; Namburete, E.I.; Feliciano, C.S.; Macheque, D.; Harrison, L.H.; Caminero, J.A. Detection of katG and inhA mutations to guide isoniazid and ethionamide use for drug-resistant tuberculosis. Int. J. Tuberc. Lung Dis. 2016, 20, 1099–1104. [Google Scholar] [CrossRef]
- Belete, T.M. Recent Progress in the Development of Novel Mycobacterium Cell Wall Inhibitor to Combat Drug-Resistant Tuberculosis. Microbiol. Insights 2022, 15, 117863612210998. [Google Scholar] [CrossRef]
- Upton, A.M.; Mushtaq, A.; Victor, T.C.; Sampson, S.L.; Sandy, J.; Smith, D.-M.; van Helden, P.V.; Sim, E. Arylamine N-acetyltransferase of Mycobacterium tuberculosis is a polymorphic enzyme and a site of isoniazid metabolism. Mol. Microbiol. 2001, 42, 309–317. [Google Scholar] [CrossRef]
- Kinzig-Schippers, M.; Tomalik-Scharte, D.; Jetter, A.; Scheidel, B.; Jakob, V.; Rodamer, M.; Cascorbi, I.; Doroshyenko, O.; Sörgel, F.; Fuhr, U. Should we use N-acetyltransferase type 2 genotyping to personalize isoniazid doses? Antimicrob. Agents Chemother. 2005, 49, 1733–1738. [Google Scholar] [CrossRef]
- Sharma, P.C.; Sharma, D.; Sharma, A.; Saini, N.; Goyal, R.; Ola, M.; Chawla, R.; Thakur, V.K. Hydrazone comprising compounds as promising anti-infective agents: Chemistry and structure-property relationship. Mater. Today Chem. 2020, 18, 100349. [Google Scholar] [CrossRef]
- Koçak Aslan, E.; Krishna, V.S.; Armaković, S.J.; Armaković, S.; Şahin, O.; Tønjum, T.; Gündüz, M.G. Linking azoles to isoniazid via hydrazone bridge: Synthesis, crystal structure determination, antitubercular evaluation and computational studies. J. Mol. Liq. 2022, 354, 118873. [Google Scholar] [CrossRef]
- Vavříková, E.; Polanc, S.; Kočevar, M.; Horváti, K.; Bősze, S.; Stolaříková, J.; Vávrová, K.; Vinšová, J. New fluorine-containing hydrazones active against MDR-tuberculosis. Eur. J. Med. Chem. 2011, 46, 4937–4945. [Google Scholar] [CrossRef] [PubMed]
- Vergara, F.M.F.; Lima, C.H.d.S.; das Graças de Oliveira Henriques, M.; Candéa, A.L.P.; Lourenço, M.C.S.; de Lima Ferreira, M.; Kaiser, C.R.; de Souza, M.V.N. Synthesis and antimycobacterial activity of N′-[(E)-(monosubstituted-benzylidene)]-2-pyrazinecarbohydrazide derivatives. Eur. J. Med. Chem. 2009, 44, 4954–4959. [Google Scholar] [CrossRef] [PubMed]
- Ivasiv, V.; Albertini, C.; Gonçalves, A.E.; Rossi, M.; Bolognesi, M.L. Molecular hybridization as a tool for designing multitarget drug candidates for complex diseases. Curr. Top. Med. Chem. 2019, 19, 1694–1711. [Google Scholar] [CrossRef] [PubMed]
- Viegas, C., Jr.; Eliezer, J.B.; Manssour Fraga, C.A. Molecular Hybridization: A Useful Tool in the Design of New Drug Prototypes. Curr. Med. Chem. 2007, 14, 1829–1852. [Google Scholar] [CrossRef]
- Stagg, H.R.; Lipman, M.C.; McHugh, T.D.; Jenkins, H.E. Isoniazid-resistant tuberculosis: A cause for concern? Int. J. Tuberc. Lung Dis. 2017, 21, 129–139. [Google Scholar] [CrossRef]
- Tonge, P.; Kisker, C.; Slayden, R. Development of Modern InhA Inhibitors to Combat Drug Resistant Strains of Mycobacterium tuberculosis. Curr. Top. Med. Chem. 2007, 7, 489–498. [Google Scholar] [CrossRef]
- Li, P.; Wang, B.; Fu, L.; Guo, K.; Ma, C.; Wang, B.; Lin, Z.; Li, G.; Huang, H.; Lu, Y. Identification of novel benzothiopyranones with ester and amide motifs derived from active metabolite as promising leads against Mycobacterium tuberculosis. Eur. J. Med. Chem. 2021, 222, 113603. [Google Scholar] [CrossRef]
- Joaquim, A.R.; Gionbelli, M.P.; Gosmann, G.; Fuentefria, A.M.; Lopes, M.S.; Fernandes De Andrade, S. Novel Antimicrobial 8-Hydroxyquinoline-Based Agents: Current Development, Structure-Activity Relationships, and Perspectives. J. Med. Chem. 2021, 64, 16349–16379. [Google Scholar] [CrossRef]
- Lima, P.C.; Lima, L.M.; Da Silva, K.C.M.; Léda, P.H.O.; De Miranda, A.L.P.; Fraga, C.A.M.; Barreiro, E.J. Synthesis and analgesic activity of novel N-acylarylhydrazones and isosters, derived from natural safrole. Eur. J. Med. Chem. 2000, 35, 187–203. [Google Scholar] [CrossRef]
- Belowich, M.E.; Stoddart, J.F. Dynamic imine chemistry. Chem. Soc. Rev. 2012, 41, 2003–2024. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, P.F.M.; Guidetti, B.; Chamayou, A.; André-Barrès, C.; Madacki, J.; Korduláková, J.; Mori, G.; Orena, B.S.; Chiarelli, L.R.; Pasca, M.R.; et al. Mechanochemical Synthesis and Biological Evaluation of Novel Isoniazid Derivatives with Potent Antitubercular Activity. Molecules 2017, 22, 1457. [Google Scholar] [CrossRef] [PubMed]
- Prasad, M.S.; Bhole, R.P.; Khedekar, P.B.; Chikhale, R.V. Mycobacterium enoyl acyl carrier protein reductase (InhA): A key target for antitubercular drug discovery. Bioorg. Chem. 2021, 115, 105242. [Google Scholar] [CrossRef]
- Rivière, E.; Whitfield, M.G.; Nelen, J.; Heupink, T.H.; Van Rie, A. Identifying isoniazid resistance markers to guide inclusion of high-dose isoniazid in tuberculosis treatment regimens. Clin. Microbiol. Infect. 2020, 26, 1332–1337. [Google Scholar] [CrossRef] [PubMed]
- Rožman, K.; Sosič, I.; Fernandez, R.; Young, R.J.; Mendoza, A.; Gobec, S.; Encinas, L. A new ‘golden age’ for the antitubercular target InhA. Drug Discov. Today 2017, 22, 492–502. [Google Scholar] [CrossRef]
- Guardia, A.; Gulten, G.; Fernandez, R.; Gómez, J.; Wang, F.; Convery, M.; Blanco, D.; Martínez, M.; Pérez-Herrán, E.; Alonso, M.; et al. N-Benzyl-4-((heteroaryl)methyl)benzamides: A New Class of Direct NADH-Dependent 2-trans Enoyl–Acyl Carrier Protein Reductase (InhA) Inhibitors with Antitubercular Activity. ChemMedChem 2016, 11, 687–701. [Google Scholar] [CrossRef]
- Chollet, A.; Maveyraud, L.; Lherbet, C.; Bernardes-Génisson, V. An overview on crystal structures of InhA protein: Apo-form, in complex with its natural ligands and inhibitors. Eur. J. Med. Chem. 2018, 146, 318–343. [Google Scholar] [CrossRef]
- Lipinski, C.A.; Lombardo, F.; Dominy, B.W.; Feeney, P.J. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv. Drug Deliv. Rev. 2001, 46, 3–26. [Google Scholar] [CrossRef]
- Veber, D.F.; Johnson, S.R.; Cheng, H.Y.; Smith, B.R.; Ward, K.W.; Kopple, K.D. Molecular properties that influence the oral bioavailability of drug candidates. J. Med. Chem. 2002, 45, 2615–2623. [Google Scholar] [CrossRef]
- Khan, S.R.; Manialawy, Y.; Siraki, A.G. Isoniazid and host immune system interactions: A proposal for a novel comprehensive mode of action. Br. J. Pharmacol. 2019, 176, 4599–4608. [Google Scholar] [CrossRef] [PubMed]
- Kjellsson, M.C.; Via, L.E.; Goh, A.; Weiner, D.; Low, K.M.; Kern, S.; Pillai, G.; Barry, C.E.; Dartois, V. Pharmacokinetic evaluation of the penetration of antituberculosis agents in rabbit pulmonary lesions. Antimicrob. Agents Chemother. 2012, 56, 446–457. [Google Scholar] [CrossRef] [PubMed]
- Ertl, P.; Rohde, B.; Selzer, P. Fast Calculation of Molecular Polar Surface Area as a Sum of Fragment-Based Contributions and Its Application to the Prediction of Drug Transport Properties. J. Med. Chem. 2000, 43, 3714–3717. [Google Scholar] [CrossRef] [PubMed]
- Tokalı, F.S.; Demir, Y.; Demircioğlu, İ.H.; Türkeş, C.; Kalay, E.; Şendil, K.; Beydemir, Ş. Synthesis, biological evaluation, and in silico study of novel library sulfonates containing quinazolin-4(3H)-one derivatives as potential aldose reductase inhibitors. Drug Dev. Res. 2022, 83, 586–604. [Google Scholar] [CrossRef] [PubMed]
- Biava, M.; Porretta, G.C.; Poce, G.; Supino, S.; Deidda, D.; Pompei, R.; Molicotti, P.; Manetti, F.; Botta, M. Antimycobacterial agents. Novel diarylpyrrole derivatives of BM212 endowed with high activity toward Mycobacterium tuberculosis and low cytotoxicity. J. Med. Chem. 2006, 49, 4946–4952. [Google Scholar] [CrossRef]
- Atıcı, R.K.; Doğan, Ş.D.; Gündüz, M.G.; Krishna, V.S.; Chebaiki, M.; Homberset, H.; Lherbet, C.; Mourey, L.; Tønjum, T. Urea derivatives carrying a thiophenylthiazole moiety: Design, synthesis, and evaluation of antitubercular and InhA inhibitory activities. Drug Dev. Res. 2022, 83, 1292–1304. [Google Scholar] [CrossRef]
- Rodriguez, F.; Saffon, N.; Sammartino, J.C.; Degiacomi, G.; Pasca, M.R.; Lherbet, C. First triclosan-based macrocyclic inhibitors of InhA enzyme. Bioorg. Chem. 2020, 95, 103498. [Google Scholar] [CrossRef]
- Kuo, M.R.; Morbidoni, H.R.; Alland, D.; Sneddon, S.F.; Gourlie, B.B.; Staveski, M.M.; Leonard, M.; Gregory, J.S.; Janjigian, A.D.; Yee, C.; et al. Targeting Tuberculosis and Malaria through Inhibition of Enoyl Reductase. J. Biol. Chem. 2003, 278, 20851–20859. [Google Scholar] [CrossRef]
- Wolber, G.; Langer, T. LigandScout: 3-D pharmacophores derived from protein-bound ligands and their use as virtual screening filters. J. Chem. Inf. Model. 2005, 45, 160–169. [Google Scholar] [CrossRef]
- Morris, G.M.; Huey, R.; Lindstrom, W.; Sanner, M.F.; Belew, R.K.; Goodsell, D.S.; Olson, A.J. AutoDock4 and AutoDockTools4: Automated docking with selective receptor flexibility. J. Comput. Chem. 2009, 30, 2785–2791. [Google Scholar] [CrossRef]
- Schrödinger Release 2019-1: Maestro; Schrödinger, LLC: New York, NY, USA, 2019.
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).