A Meta-Analysis of the Analgesic Efficacy of Single-Doses of Ibuprofen Compared to Traditional Non-Opioid Analgesics Following Third Molar Surgery
Abstract
1. Introduction
2. Material and Methods
2.1. Study Registration
2.2. Selection Criteria
2.3. Article Digital Searching
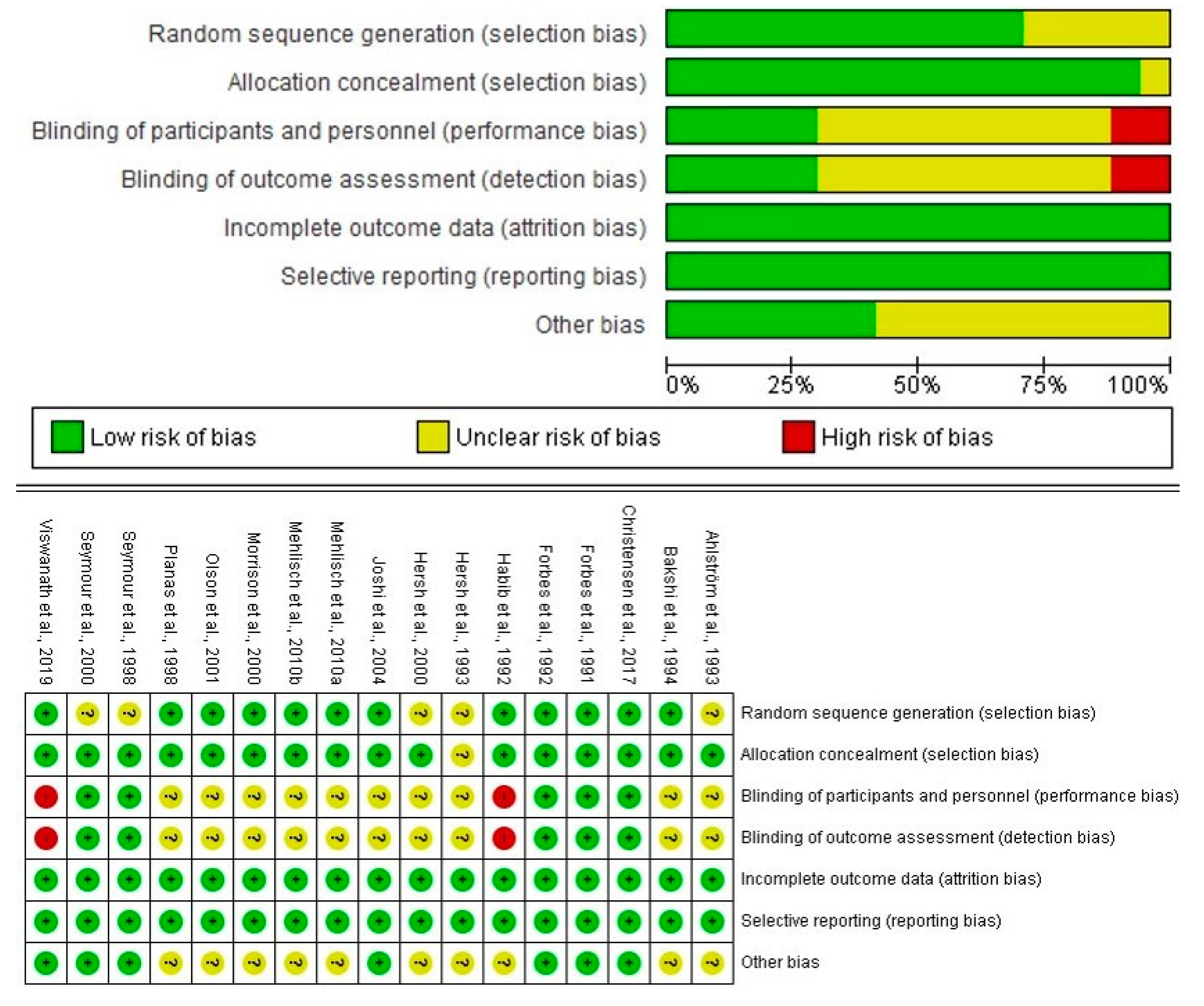
2.4. Quality Assessment
2.5. Data Collection
2.6. Statistical Analysis
3. Results
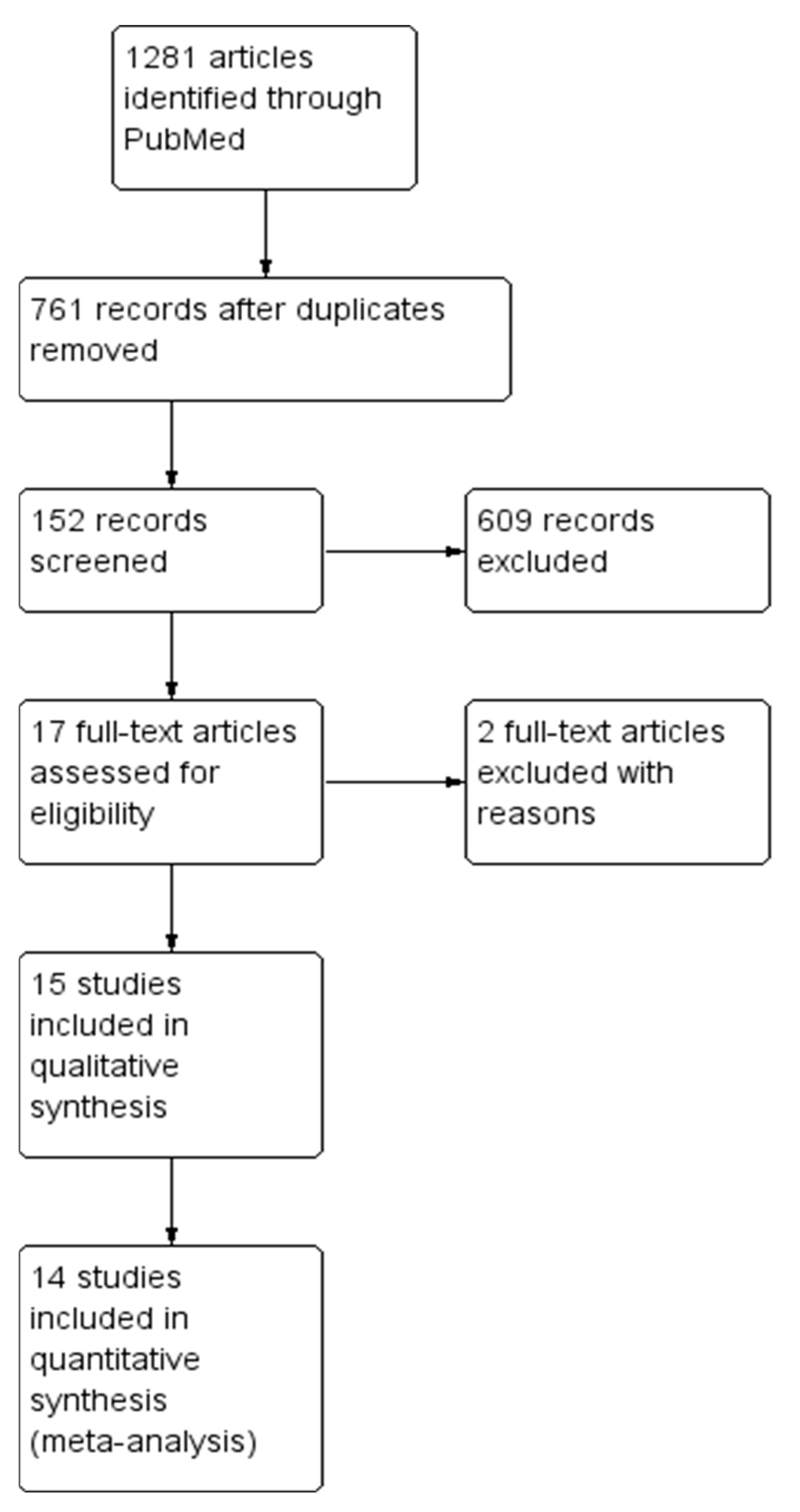
3.1. Digital Search and Assessment of Bias
3.2. Qualitative Evaluation
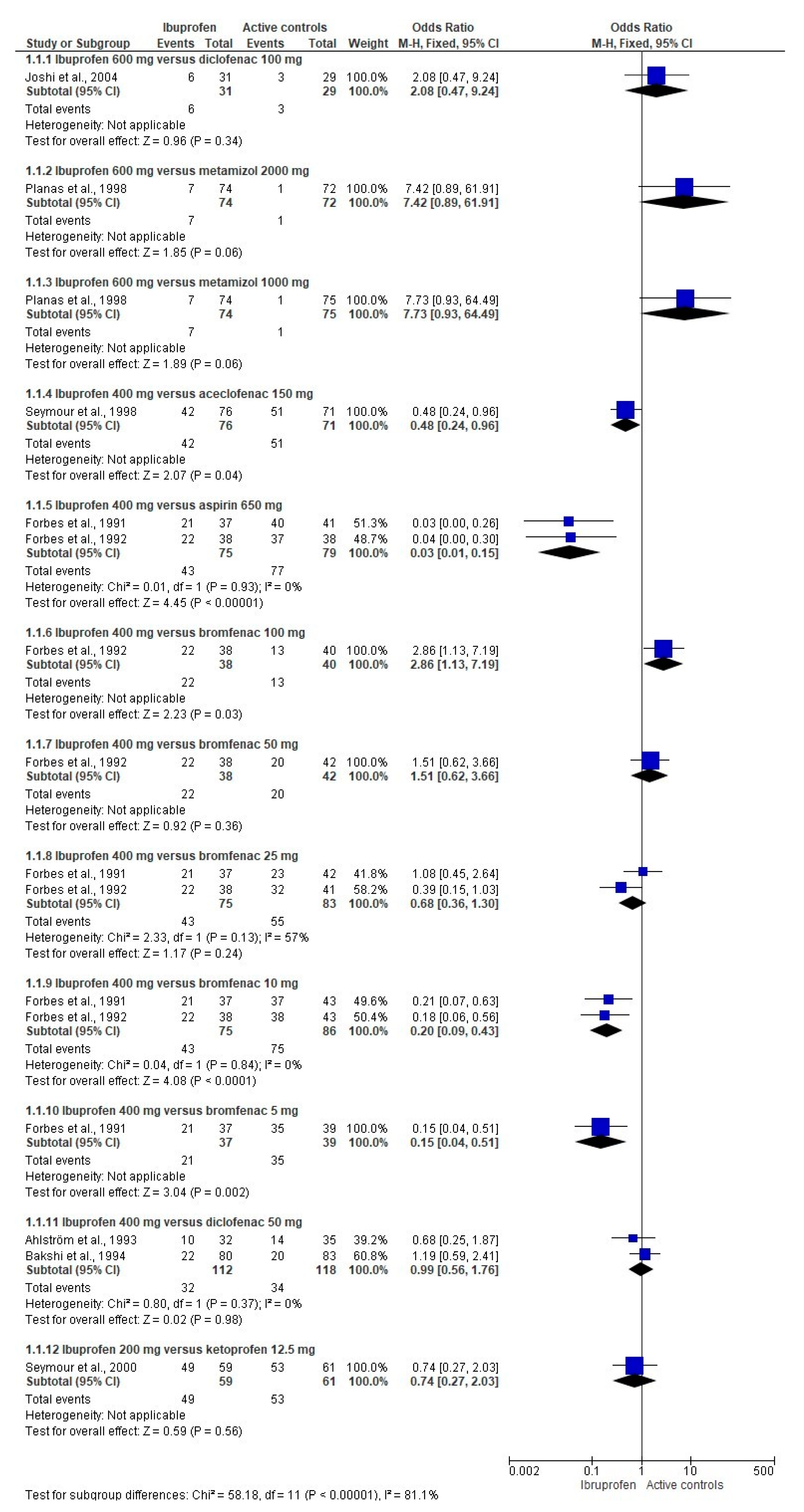
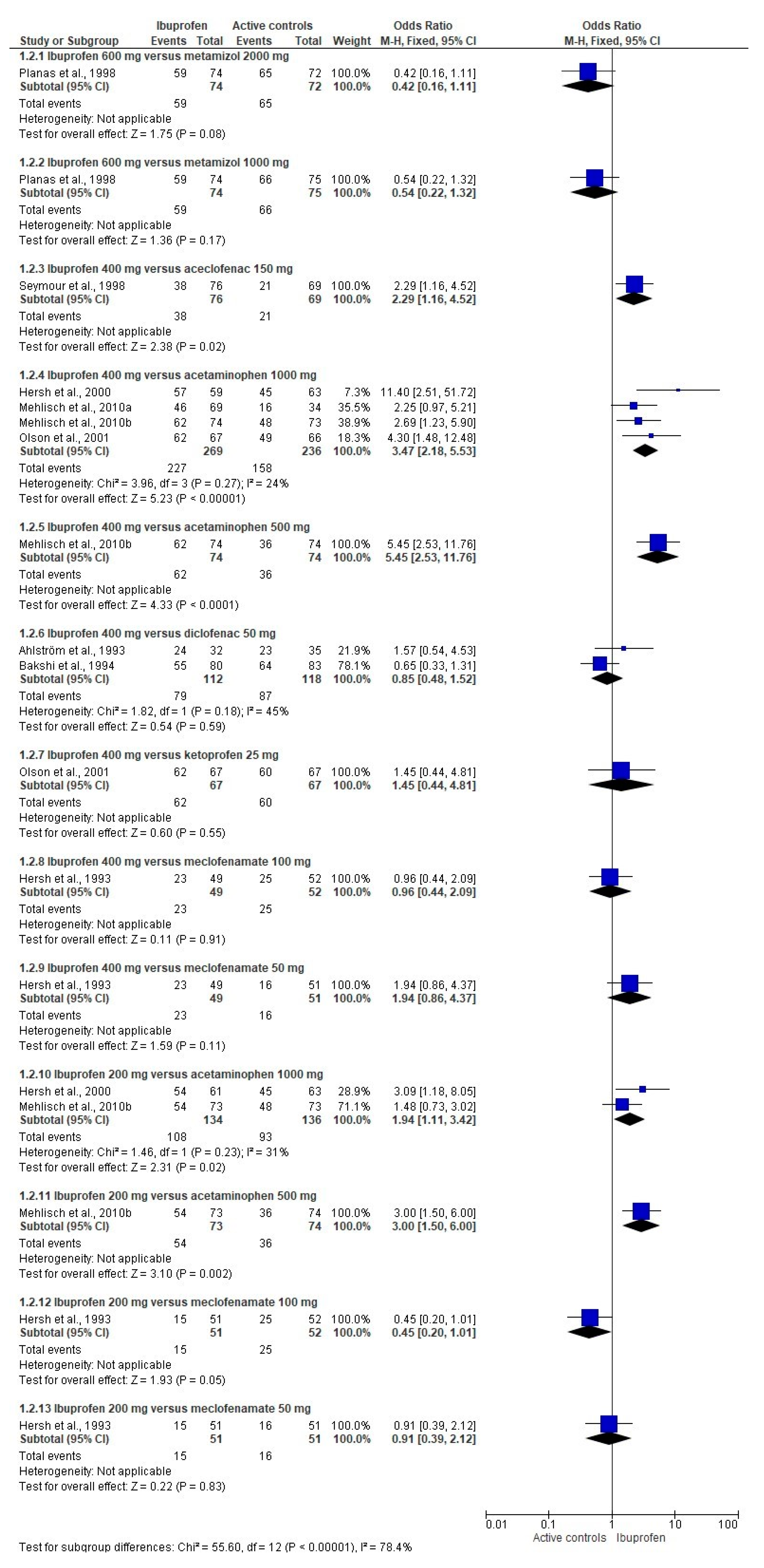
3.3. Analgesic Efficacy
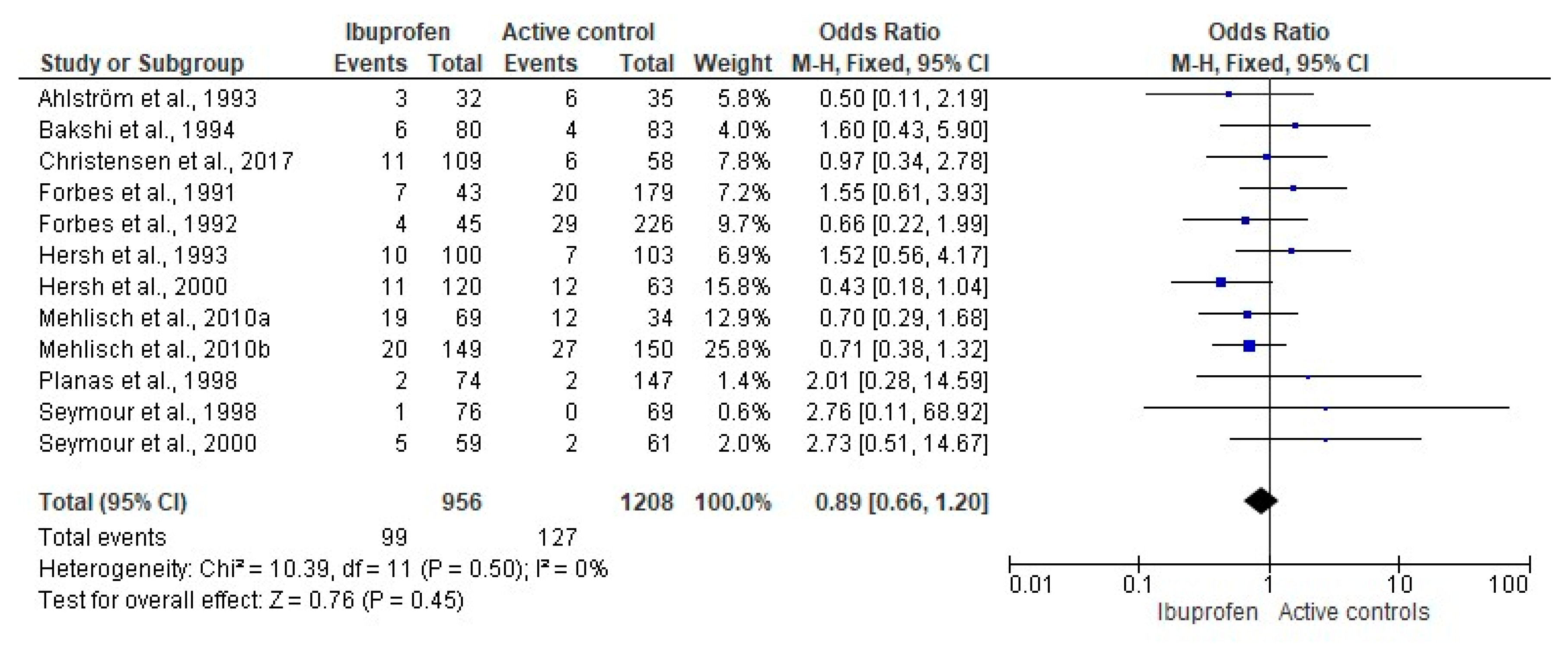
3.4. Adverse Effects
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Osunde, O.D.; Adebola, R.A.; Omeje, U.K. Management of inflammatory complications in third molar surgery: A review of the literature. Afr. Health Sci. 2011, 11, 530–537. [Google Scholar] [PubMed]
- Bouloux, G.F.; Steed, M.B.; Perciaccante, V.J. Complications of third molar surgery. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Carrasco-Labra, A.; Brignardello-Petersen, R.; Yanine, N.; Araya, I.; Guyatt, G. Secondary versus primary closure techniques for the prevention of postoperative complications following removal of impacted mandibular third molars: A systematic review and meta-analysis of randomized controlled trials. J. Oral Maxillofac. Surg. 2012, 70, e441–e457. [Google Scholar] [CrossRef]
- Sainz de Baranda, B.; Silvestre, F.J.; Silvestre-Rangil, J. Relationship between surgical difficulty of third molar extraction under local anesthesia and the postoperative evolution of clinical and blood parameters. J. Oral Maxillofac. Surg. 2019, 77, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- Al-Delayme, R.M.A. Randomized clinical study comparing Piezoelectric surgery with conventional rotatory osteotomy in mandibular third molars surgeries. Saudi Dent. J. 2021, 33, 11–21. [Google Scholar] [CrossRef]
- Hellem, S.; Persson, G.; Freiberg, N.; Nord, P.G.; Gustafsson, B.; Huitfeldt, B. A model for evaluating the analgesic effect of a new fixed ratio combination analgesic in patients undergoing oral surgery. Int. J. Oral Surg. 1979, 8, 435–442. [Google Scholar] [CrossRef]
- Seymour, R.A.; Walton, J.G. Pain control after third molar surgery. Int. J. Oral Surg. 1984, 13, 457–485. [Google Scholar] [CrossRef]
- Orozco-Solís, M.; García-Ávalos, Y.; Pichardo-Ramírez, C.; Tobías-Azúa, F.; Zapata-Morales, J.R.; Aragon-Martínez, O.H.; Isiordia-Espinoza, M.A. Single dose of diclofenac or meloxicam for control of pain, facial swelling, and trismus in oral surgery. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e127–e134. [Google Scholar] [CrossRef] [PubMed]
- Pérez-González, J.M.; Esparza-Villalpando, V.; Martínez-Rider, R.; Noyola-Frías, M.Á.; Pozos-Guillén, A. Clinical and radiographic characteristics as predictive factors of swelling and trismus after mandibular third molar surgery: A longitudinal approach. Pain Res. Manag. 2018, 7938492. [Google Scholar] [CrossRef]
- Roszkowski, M.T.; Swift, J.Q.; Hargreaves, K.M. Effect of NSAID administration on tissue levels of immunoreactive prostaglandin E2, leukotriene B4, and (S)-flurbiprofen following extraction of impacted third molars. Pain 1997, 73, 339–345. [Google Scholar] [CrossRef]
- Chopra, D.; Rehan, H.S.; Mehra, P.; Kakkar, A.K. A randomized, double-blind, placebo-controlled study comparing the efficacy and safety of paracetamol, serratiopeptidase, ibuprofen and betamethasone using the dental impaction pain model. Int. J. Oral Maxillofac. Surg. 2009, 38, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Schultze-Mosgau, S.; Schmelzeisen, R.; Frölich, J.C.; Schmele, H. Use of ibuprofen and methylprednisolone for the prevention of pain and swelling after removal of impacted third molars. J. Oral Maxillofac. Surg. 1995, 53, 2–7. [Google Scholar] [CrossRef]
- Manvelian, G.; Daniels, S.; Gibofsky, A. A phase 2 study evaluating the efficacy and safety of a novel, proprietary, nano-formulated, lower dose oral diclofenac. Pain Med. 2012, 13, 1491–1498. [Google Scholar] [CrossRef] [PubMed]
- Tuzuner Oncul, A.M.; Yazicioglu, D.; Alanoglu, Z.; Demiralp, S.; Ozturk, A.; Ucok, C. Postoperative analgesia in impacted third molar surgery: The role of preoperative diclofenac sodium, paracetamol and lornoxicam. Med. Princ. Pract. 2011, 20, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Bailey, E.; Worthington, H.V.; van Wijk, A.; Yates, J.M.; Coulthard, P.; Afzal, Z. Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth. Cochr. Database Syst. Rev. 2013, CD004624. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; The Cochrane Collaboration: Oxford, UK, 2011; Available online: http://www.cochrane-handbook.org (accessed on 15 October 2020).
- Jones, A.; Steel, D. Evaluating the quality of medical evidence in real-world contexts. J. Eval. Clin. Pract. 2018, 24, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Atkins, D.; Eccles, M.; Flottorp, S.; Guyatt, G.H.; Henry, D.; Hill, S.; Liberati, A.; O’Connell, D.; Oxman, A.D.; Phillips, B.; et al. Systems for grading the quality of evidence and the strength of recommendations I: Critical appraisal of existing approaches The GRADE Working Group. BMC Health Serv. Res. 2004, 4, 38. [Google Scholar] [CrossRef] [PubMed]
- Isiordia-Espinoza, M.A.; Aragon-Martinez, O.H.; Bollogna-Molina, R.E.; Alonso-Castro, Á.J. Infection, alveolar osteitis, and adverse effects using metronidazole in healthy patients undergoing third molar surgery: A meta-analysis. J. Maxillofac. Oral Surg. 2018, 17, 142–149. [Google Scholar] [CrossRef]
- Isiordia-Espinoza, M.A.; Aragon-Martinez, O.H.; Martínez-Morales, J.F.; Zapata-Morales, J.R. Risk of wound infection and safety profile of amoxicillin in healthy patients which required third molar surgery: A systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2015, 53, 796–804. [Google Scholar] [CrossRef]
- Isiordia-Espinoza, M.A.; Pozos-Guillén, A.J.; Aragon-Martinez, O.H. Analgesic efficacy and safety of single-dose tramadol and non-steroidal anti-inflammatory drugs in operations on the third molars: A systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2014, 52, 775–783. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Ahlström, U.; Bakshi, R.; Nilsson, P.; Wåhlander, L. The analgesic efficacy of diclofenac dispersible and ibuprofen in postoperative pain after dental extraction. Eur. J. Clin. Pharmacol. 1993, 44, 587–588. [Google Scholar] [CrossRef]
- Bakshi, R.; Frenkel, G.; Dietlein, G.; Meurer-Witt, B.; Schneider, B.; Sinterhauf, U. A placebo-controlled comparative evaluation of diclofenac dispersible versus ibuprofen in postoperative pain after third molar surgery. J. Clin. Pharmacol. 1994, 34, 225–230. [Google Scholar] [CrossRef]
- Christensen, S.; Paluch, E.; Jayawardena, S.; Daniels, S.; Meeves, S. Analgesic efficacy of a new immediate-release/extended-release formulation of ibuprofen: Results from single- and multiple-dose postsurgical dental pain studies. Clin. Pharmacol. Drug. Dev. 2017, 6, 302–312. [Google Scholar] [CrossRef]
- Forbes, J.A.; Edquist, I.A.; Smith, F.G.; Schwartz, M.K.; Beaver, W.T. Evaluation of bromfenac, aspirin, and ibuprofen in postoperative oral surgery pain. Pharmacotherapy 1991, 11, 64–70. [Google Scholar] [PubMed]
- Forbes, J.A.; Beaver, W.T.; Jones, K.F.; Edquist, I.A.; Gongloff, C.M.; Smith, W.K.; Smith, F.G.; Schwartz, M.K. Analgesic efficacy of bromfenac, ibuprofen, and aspirin in postoperative oral surgery pain. Clin. Pharmacol. Ther. 1992, 51, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Hersh, E.V.; Cooper, S.; Betts, N.; Wedell, D.; MacAfee, K.; Quinn, P.; Lamp, C.; Gaston, G.; Bergman, S.; Henry, E. Single dose and multidose analgesic study of ibuprofen and meclofenamate sodium after third molar surgery. Oral Surg. Oral Med. Oral Pathol. 1993, 76, 680–687. [Google Scholar] [CrossRef]
- Hersh, E.V.; Levin, L.M.; Cooper, S.A.; Doyle, G.; Waksman, J.; Wedell, D.; Hong, D.; Secreto, S.A. Ibuprofen liquigel for oral surgery pain. Clin. Ther. 2000, 22, 1306–1318. [Google Scholar] [CrossRef]
- Joshi, A.; Parara, E.; Macfarlane, T.V. A double-blind randomised controlled clinical trial of the effect of preoperative ibuprofen, diclofenac, paracetamol with codeine and placebo tablets for relief of postoperative pain after removal of impacted third molars. Br. J. Oral Maxillofac. Surg. 2004, 42, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Mehlisch, D.R.; Aspley, S.; Daniels, S.E.; Bandy, D.P. Comparison of the analgesic efficacy of concurrent ibuprofen and paracetamol with ibuprofen or paracetamol alone in the management of moderate to severe acute postoperative dental pain in adolescents and adults: A randomized, double-blind, placebo-controlled, parallel-group, single-dose, two-center, modified factorial study. Clin. Ther. 2010, 32, 882–895. [Google Scholar] [PubMed]
- Mehlisch, D.R.; Aspley, S.; Daniels, S.E.; Southerden, K.A.; Christensen, K.S. A single-tablet fixed-dose combination of racemic ibuprofen/paracetamol in the management of moderate to severe postoperative dental pain in adult and adolescent patients: A multicenter, two-stage, randomized, double-blind, parallel-group, placebo-controlled, factorial study. Clin. Ther. 2010, 32, 1033–1049. [Google Scholar] [PubMed]
- Morrison, B.W.; Fricke, J.; Brown, J.; Yuan, W.; Kotey, P.; Mehlisch, D. The optimal analgesic dose of rofecoxib: Overview of six randomized controlled trials. J. Am. Dent. Assoc. 2000, 131, 1729–1737. [Google Scholar] [CrossRef] [PubMed]
- Olson, N.Z.; Otero, A.M.; Marrero, I.; Tirado, S.; Cooper, S.; Doyle, G.; Jayawardena, S.; Sunshine, A. Onset of analgesia for liquigel ibuprofen 400 mg, acetaminophen 1000 mg, ketoprofen 25 mg, and placebo in the treatment of postoperative dental pain. J. Clin. Pharmacol. 2001, 41, 1238–1247. [Google Scholar] [CrossRef]
- Planas, M.E.; Gay-Escoda, C.; Bagán, J.V.; Santamaría, J.; Peñarrocha, M.; Donado, M.; Puerta, J.L.; García-Magaz, I.; Ruíz., J.; Ortiz, P. Oral metamizol (1 g and 2 g) versus ibuprofen and placebo in the treatment of lower third molar surgery pain: Randomised double-blind multi-centre study. Cooperative Study Group. Eur. J. Clin. Pharmacol. 1998, 53, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Seymour, R.A.; Frame, J.; Negus, T.W.; Hawkesford, J.E.; Marsden, J.; Matthew, I.R. The comparative efficacy of aceclofenac and ibuprofen in postoperative pain after third molar surgery. Br. J. Oral Maxillofac. Surg. 1998, 36, 375–379. [Google Scholar] [CrossRef]
- Seymour, R.A.; Watkinson, H.; Hawkesford, J.E.; Moore, U. The efficacy of buffered ketoprofen in postoperative pain after third molar surgery. Eur. J. Clin. Pharmacol. 2000, 55, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Mehlisch, D.R.; Jasper, R.D.; Brown, P.; Korn, S.H.; McCarroll, K.; Murakami, A.A. Comparative study of ibuprofen lysine and acetaminophen in patients with postoperative dental pain. Clin. Ther. 1995, 17, 852–860. [Google Scholar] [CrossRef]
- Thybo, K.H.; Hägi-Pedersen, D.; Dahl, J.B.; Wetterslev, J.; Nersesjan, M.; Jakobsen, J.C.; Pedersen, N.A.; Overgaard, S.; Schrøder, H.M.; Schmidt, H.; et al. Effect of combination of paracetamol (acetaminophen) and ibuprofen vs either alone on patient-controlled morphine consumption in the first 24 hours after total hip arthroplasty: The PANSAID randomized clinical trial. JAMA 2019, 321, 562–571. [Google Scholar] [CrossRef]
- Kamondetdecha, R.; Tannirandorn, Y. Ibuprofen versus acetaminophen for the relief of perineal pain after childbirth: A randomized controlled trial. J. Med. Assoc. Thail. 2008, 91, 282–286. [Google Scholar] [CrossRef][Green Version]
- Ekinci, M.; Ciftci, B.; Celik, E.C.; Köse, E.A.; Karakaya, M.A.; Ozdenkaya, Y. A randomized, placebo-controlled, double-blind study that evaluates efficacy of intravenous ibuprofen and acetaminophen for postoperative pain treatment following laparoscopic cholecystectomy surgery. J. Gastrointest. Surg. 2020, 24, 780–785. [Google Scholar] [CrossRef]
- Ciftci, B.; Ekinci, M.; Celik, E.C.; Kaciroglu, A.; Karakaya, M.A.; Demiraran, Y.; Ozdenkaya, Y. Comparison of intravenous ibuprofen and paracetamol for postoperative pain management after laparoscopic sleeve gastrectomy. A randomized controlled study. Obes. Surg. 2019, 29, 765–770. [Google Scholar] [CrossRef]
- Erdogan-Kayhan, G.; Sanli, M.; Ozgul, U.; Kirteke, R.; Yologlu, S. Comparison of intravenous ibuprofen and acetaminophen for postoperative multimodal pain management in bariatric surgery: A randomized controlled trial. J. Clin. Anesth. 2018, 50, 5–11. [Google Scholar] [CrossRef]
- Esteller-Martínez, V.; Paredes-García, J.; Valmaseda-Castellón, E.; Berini-Aytés, L.; Gay-Escoda, C. Analgesic efficacy of diclofenac sodium versus ibuprofen following surgical extraction of impacted lower third molars. Med. Oral Patol. Oral Cir. Bucal 2004, 9, 448–453. [Google Scholar] [PubMed]
- Gazal, G.; Al-Samadani, K.H. Comparison of paracetamol, ibuprofen, and diclofenac potassium for pain relief following dental extractions and deep cavity preparations. Saudi Med. J. 2017, 38, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.A.; Derry, S.; Aldington, D.; Wiffen, P.J. Single dose oral analgesics for acute postoperative pain in adults-an overview of Cochrane reviews. Cochrane Database Syst. Rev. 2015, 2015, CD008659. [Google Scholar] [CrossRef]
- Southey, E.R.; Soares-Weiser, K.; Kleijnen, J. Systematic review and meta-analysis of the clinical safety and tolerability of ibuprofen compared with paracetamol in paediatric pain and fever. Curr. Med. Res. Opin. 2009, 25, 2207–2222. [Google Scholar] [CrossRef]
- Tan, E.; Braithwaite, I.; McKinlay, C.J.D.; Dalziel, S.R. Comparison of acetaminophen (paracetamol) with ibuprofen for treatment of fever or pain in children younger than 2 years: A systematic review and meta-analysis. JAMA Netw. Open 2020, 3, e2022398. [Google Scholar] [CrossRef]
- van Walsem, A.; Pandhi, S.; Nixon, R.M.; Guyot, P.; Karabis, A.; Moore, R.A. Relative benefit-risk comparing diclofenac to other traditional non-steroidal anti-inflammatory drugs and cyclooxygenase-2 inhibitors in patients with osteoarthritis or rheumatoid arthritis: A network meta-analysis. Arthritis Res. Ther. 2015, 17, 66. [Google Scholar] [CrossRef] [PubMed]
- Panic, N.; Leoncini, E.; de Belvis, G.; Ricciardi, W.; Boccia, S. Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLoS ONE 2013, 8, e83138. [Google Scholar] [CrossRef]
- Argimon-Pallás, J.M.; Jiménez-Villa, J. Métodos de Investigación Clínica y Epidemiológica, 5th ed.; Elsevier: Barcelona, Spain, 2019. [Google Scholar]
- Dawson, B.; Trapp, R.G. Bioestadística Médica, 4th ed.; Editorial El Manual Moderno: Mexico City, Mexico, 2005. [Google Scholar]
- Akinbade, A.O.; Ndukwe, K.C.; Owotade, F.J. Comparative analgesic effects of ibuprofen, celecoxib and tramadol after third molar surgery: A randomized double blind controlled trial. J. Contemp. Dent. Pract. 2018, 19, 1334–1340. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franco-de la Torre, L.; Figueroa-Fernández, N.P.; Franco-González, D.L.; Alonso-Castro, Á.J.; Rivera-Luna, F.; Isiordia-Espinoza, M.A. A Meta-Analysis of the Analgesic Efficacy of Single-Doses of Ibuprofen Compared to Traditional Non-Opioid Analgesics Following Third Molar Surgery. Pharmaceuticals 2021, 14, 360. https://doi.org/10.3390/ph14040360
Franco-de la Torre L, Figueroa-Fernández NP, Franco-González DL, Alonso-Castro ÁJ, Rivera-Luna F, Isiordia-Espinoza MA. A Meta-Analysis of the Analgesic Efficacy of Single-Doses of Ibuprofen Compared to Traditional Non-Opioid Analgesics Following Third Molar Surgery. Pharmaceuticals. 2021; 14(4):360. https://doi.org/10.3390/ph14040360
Chicago/Turabian StyleFranco-de la Torre, Lorenzo, Norma Patricia Figueroa-Fernández, Diana Laura Franco-González, Ángel Josabad Alonso-Castro, Federico Rivera-Luna, and Mario Alberto Isiordia-Espinoza. 2021. "A Meta-Analysis of the Analgesic Efficacy of Single-Doses of Ibuprofen Compared to Traditional Non-Opioid Analgesics Following Third Molar Surgery" Pharmaceuticals 14, no. 4: 360. https://doi.org/10.3390/ph14040360
APA StyleFranco-de la Torre, L., Figueroa-Fernández, N. P., Franco-González, D. L., Alonso-Castro, Á. J., Rivera-Luna, F., & Isiordia-Espinoza, M. A. (2021). A Meta-Analysis of the Analgesic Efficacy of Single-Doses of Ibuprofen Compared to Traditional Non-Opioid Analgesics Following Third Molar Surgery. Pharmaceuticals, 14(4), 360. https://doi.org/10.3390/ph14040360








