Prevalence of Drug-Related Problems and Complementary and Alternative Medicine Use in Malaysia: A Systematic Review and Meta-Analysis of 37,249 Older Adults
Abstract
1. Introduction
2. Results
2.1. Literature Search
2.2. Characteristics of the Included Studies
2.3. Meta-Analysis
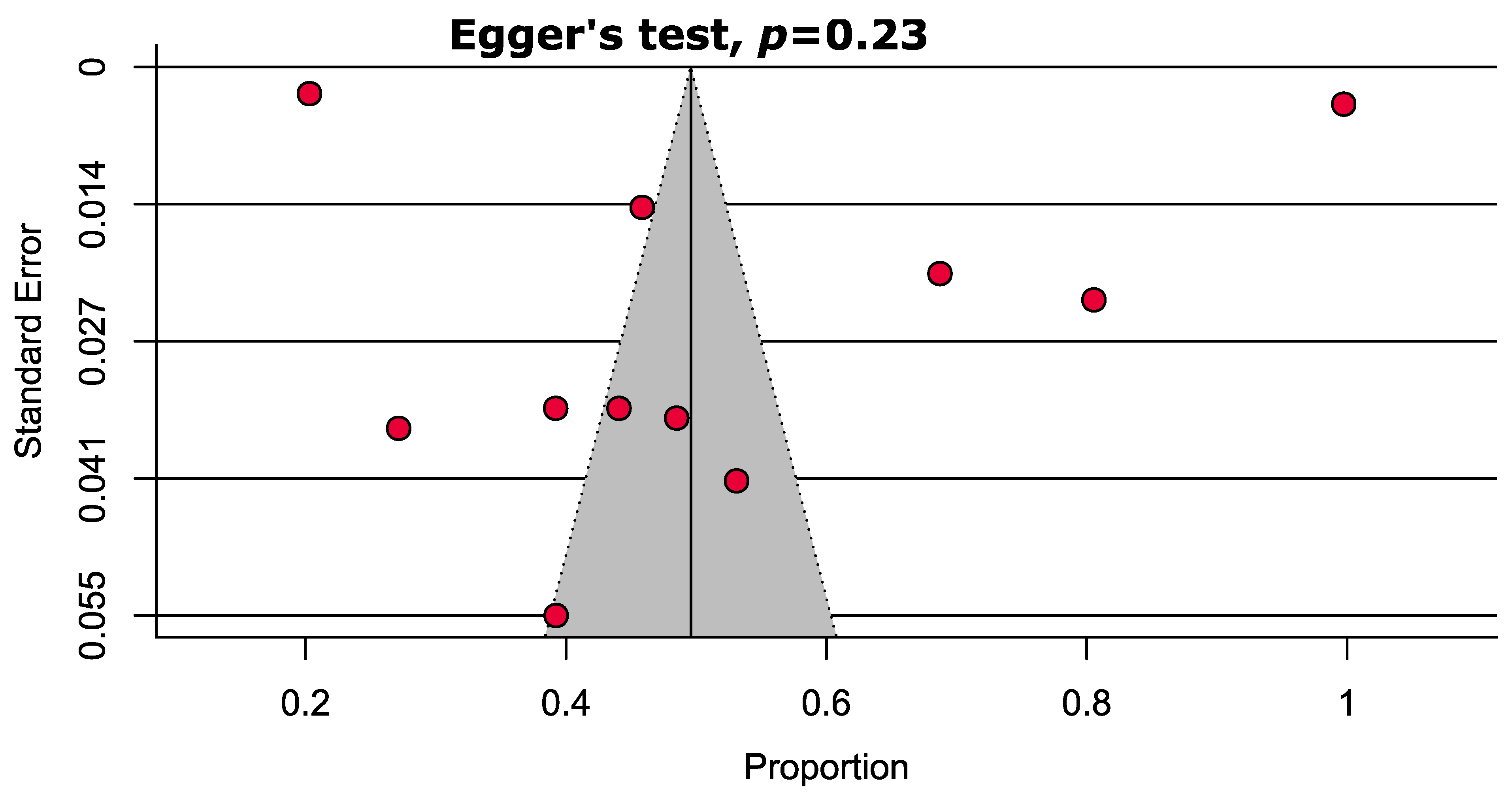
2.4. Study Quality Assessment and Publication Bias
2.5. Sensitivity Analyses
3. Discussion
4. Materials and Methods
4.1. Search Strategies and Eligibility Criteria
4.2. Identification and Selection of Studies
4.3. Data Extraction and Risk of Bias Assessment
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pharmaceutical Care Network Europe. PCNE Classification for Drug-Related Problems V8.01. 2017. Available online: https://www.pcne.org/upload/files/215_PCNE_classification_V8-01.pdf (accessed on 31 December 2020).
- Gomes, D.; Placido, A.I.; Mó, R.; Simões, J.L.; Amaral, O.; Fernandes, I.; Lima, F.; Morgado, M.; Figueiras, A.; Herdeiro, M.T. Daily Medication Management and Adherence in the Polymedicated Elderly: A Cross-Sectional Study in Portugal. Int. J. Environ. Res. Public Health 2020, 17, 200. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, M.N.; Gallagher, P.; O’Mahony, D. Inappropriate prescribing. Drugs Aging 2012, 29, 437–452. [Google Scholar] [CrossRef]
- Brown, J.D.; Hutchison, L.C.; Li, C.; Painter, J.T.; Martin, B.C. Predictive validity of the Beers and STOPP Criteria to detect adverse drug events, hospitalizations, and emergency department visits in the United States. J. Am. Geriatr. Soc. 2016, 64, 22–30. [Google Scholar] [CrossRef]
- O′Mahony, D.; O′Sullivan, D.; Byrne, S.; O′Connor, M.N.; Ryan, C.; Gallagher, P. STOPP/START criteria for potentially inappropriate prescribing in older people: Version 2. Age Ageing 2015, 44, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Zia, A.; Kamaruzzaman, S.B.; Tan, M.P. The consumption of two or more fall risk-increasing drugs rather than polypharmacy is associated with falls. Geriatr. Gerontol. Int. 2017, 17, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Lee, V.W.; Pang, K.K.; Hui, K.C.; Kwok, J.C.; Leung, S.L.; Yu, D.S.F.; Lee, D.T.F. Medication adherence: Is it a hidden drug-related problem in hidden elderly? Geriatr. Gerontol. Int. 2013, 13, 978–985. [Google Scholar] [CrossRef] [PubMed]
- Hugtenburg, J.G.; Timmers, L.; Elders, P.J.; Vervloet, M.; van Dijk, L. Definitions, variants, and causes of nonadherence with medication: A challenge for tailored interventions. Patient Prefer. Adherence 2013, 7, 675–682. [Google Scholar] [CrossRef]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical consequences of polypharmacy in elderly. Expert Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Per, B.L.; Taylor, A.W.; Gill, T.K. Prescription medicines, over-the-counter medicines and complementary and alternative medicines use: A comparison between baby boomers and older South Australians. AIMS Public Health 2019, 6, 380–395. [Google Scholar]
- Azidah, A.; Hasniza, H.; Zunaina, E. Prevalence of falls and its associated factors among elderly diabetes in a tertiary center, Malaysia. Curr. Gerontol. Geriatr. Res. 2012, 2012, 1–6. [Google Scholar] [CrossRef]
- Hasan, S.S.; Kow, C.S.; Verma, R.K.; Ahmed, S.I.; Mittal, P.; Chong, D.W. An evaluation of medication appropriateness and frailty among residents of aged care homes in Malaysia: A cross-sectional study. Medicine 2017, 96, 1–7. [Google Scholar] [CrossRef]
- Lim, L.M.; McStea, M.; Chung, W.W.; Nor Azmi, N.; Abdul Aziz, S.A.; Alwi, S.; Kamarulzaman, A.; Kamaruzzaman, S.B.; Chua, S.S.; Rajasuriar, R. Prevalence, risk factors and health outcomes associated with polypharmacy among urban community-dwelling older adults in multi-ethnic Malaysia. PLoS ONE 2017, 12, e0173466. [Google Scholar] [CrossRef]
- Chen, L.L.; Tangiisuran, B.; Shafie, A.A.; Hassali, M.A.A. Evaluation of potentially inappropriate medications among older residents of Malaysian nursing homes. Int. J. Clin. Pharm. 2012, 34, 596–603. [Google Scholar] [CrossRef]
- Shim, Y.W.; Chua, S.S.; Wong, H.C.; Alwi, S. Collaborative intervention between pharmacists and physicians on elderly patients: A randomized controlled trial. Ther. Clin. Risk Manag. 2018, 14, 1115–1125. [Google Scholar] [CrossRef]
- Hasan, S.S.; Ahmed, S.I.; Bukhari, N.I.; Loon, W.C.W. Use of complementary and alternative medicine among patients with chronic diseases at outpatient clinics. Complement. Ther. Clin. Pract. 2009, 15, 152–157. [Google Scholar] [CrossRef]
- Aziz, A.; Ibrahim, M. Medication noncompliance—A thriving problem. Med. J. Malays. 1999, 54, 192–199. [Google Scholar]
- Hasan, S.S.; Kow, C.S.; Thiruchelvam, K.; Chong, D.W.K.; Ahmed, S.I. An evaluation of the central nervous system medication use and frailty among residents of aged care homes in Malaysia. Neuroepidemiology 2017, 49, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Hasan, S.; Chang, S.; Thiruchelvam, K.; Chong, D.; Babar, Z. Drug burden index, polypharmacy and patient health outcomes in cognitively intact older residents of aged care facilities in Malaysia. J. Pharm. Pract. Res. 2020, 50, 13–21. [Google Scholar] [CrossRef]
- Hor, J. Prescription drug use among elderly admitted to medical wards in a Malaysian government hospital. Med. J. Malays. 2008, 63, 125–130. [Google Scholar]
- Kumar, S.; Wong, P.S.; Hasan, S.S.; Kairuz, T. The relationship between sleep quality, inappropriate medication use and frailty among older adults in aged care homes in Malaysia. PLoS ONE 2019, 14, e0224122. [Google Scholar] [CrossRef]
- Mitha, S.; Nagarajan, V.; Babar, M.G.; Siddiqui, M.J.A.; Jamshed, S.Q. Reasons of using complementary and alternative medicines (CAM) among elderly Malaysians of Kuala Lumpur and Selangor states: An exploratory study. J. Young Pharm. 2013, 5, 50–53. [Google Scholar] [CrossRef] [PubMed]
- Neoh, C.F.; Long, C.M.; Lim, S.M.; Ramasamy, K.; Shahar, S.; Majeed, A.B.A. Medication use and adherence among multi-ethnic community-dwelling older adults in Malaysia. Geriatr. Gerontol. Int. 2016, 17, 1214–1220. [Google Scholar] [CrossRef]
- Ramachandran, M.; Loi, B.; Ariff, N.M.; Chuan, N.O.; Sham, S.Y.Z.; Thambiah, S.C.; Samsudin, I.N. Appropriateness of metformin prescription for type 2 diabetes mellitus patients with chronic kidney disease (Stages 3–5). Malays. J. Pathol. 2020, 42, 71–76. [Google Scholar] [PubMed]
- Teow, Y.E.E.; Ng, S.C.; Azmi, A.H.M.; Hamzah, M.R.; Kaur, J.; Mathiarasu, D.S.; Mogan, D.; Ong, S.C.; Subramaniam, Y.P.; Sweneson, T. A Cross-Sectional Evaluation of Complementary and Alternative Medicine Use in a Non-urban Malaysian Population. J. Community Health 2020, 1–7. [Google Scholar] [CrossRef]
- Wahab, I.A.; Akbar, B.; Zainal, Z.A.; Pa, M.F.C.; Naina, B. The Use of Medicines with Anti-cholinergic Properties and Their Health Impacts among Hospitalised Malaysian Geriatric Patients. Malays. J. Med. Sci. MJMS 2019, 26, 77–87. [Google Scholar] [CrossRef]
- Zia, A.; Kamaruzzaman, S.; Myint, P.K.; Tan, M.P. Anticholinergic burden is associated with recurrent and injurious falls in older individuals. Maturitas 2016, 84, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Al Aqqad, S.M.; Chen, L.L.; Shafie, A.A.; Hassali, M.A.; Tangiisuran, B. The use of potentially inappropriate medications and changes in quality of life among older nursing home residents. Clin. Interv. Aging 2014, 9, 201–207. [Google Scholar]
- Yeong, U.; Tan, S.; Yap, J.; Choo, W. Prevalence of falls among community-dwelling elderly and its associated factors: A cross-sectional study in Perak, Malaysia. Malays. Fam. Physician 2016, 11, 7–14. [Google Scholar]
- Akkawi, M.E.; Mohamed, M.H.N.; Aris, M.A.M. Does inappropriate prescribing affect elderly patients’ quality of life? A study from a Malaysian tertiary hospital. Qual. Life Res. 2019, 28, 1913–1920. [Google Scholar] [CrossRef]
- Kew, Y.; Chia, Y.L.; Lai, S.M.; Chong, K.Y.; Ho, X.L.; Liew, D.W.; Moy, F.M.; Selvarajah, S. Traditional and complementary medicine (TCM) among study population with cardiovascular risk; use and substitution for conventional medicine in Pahang, Malaysia. Med. J. Malays. 2015, 70, 86–92. [Google Scholar]
- Lim, K.K.; Sivasampu, S.; Khoo, E.M. Antihypertensive drugs for elderly patients: A cross-sectional study. Singap. Med. J. 2015, 56, 291–297. [Google Scholar] [CrossRef]
- Ong, S.M.; Lim, Y.M.F.; Sivasampu, S.; Khoo, E.M. Variation of polypharmacy in older primary care attenders occurs at prescriber level. BMC Geriatr. 2018, 18, 1–12. [Google Scholar] [CrossRef]
- Siti, Z.; Tahir, A.; Farah, A.I.; Fazlin, S.A.; Sondi, S.; Azman, A.; Maimunah, A.; Haniza, M.; Haslinda, M.S.; Zulkarnain, A. Use of traditional and complementary medicine in Malaysia: A baseline study. Complement. Ther. Med. 2009, 17, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Akkawi, M.E.; Mohamed, M.H.N.; Aris, M.A.M. The impact of a multifaceted intervention to reduce potentially inappropriate prescribing among discharged older adults: A before-and-after study. J. Pharm. Policy Pract. 2020, 13, 1–11. [Google Scholar] [CrossRef]
- Liew, N.Y.; Chong, Y.Y.; Yeow, S.H.; Kua, K.P.; San Saw, P.; Lee, S.W.H. Prevalence of potentially inappropriate medications among geriatric residents in nursing care homes in Malaysia: A cross-sectional study. Int. J. Clin. Pharm. 2019, 41, 895–902. [Google Scholar] [CrossRef]
- Omar, M.S.; Ariandi, A.H.; Tohit, N.M. Practical problems of medication use in the elderly Malaysians and their beliefs and attitudes toward deprescribing of medications. J. Res. Pharm. Pract. 2019, 8, 105. [Google Scholar] [CrossRef] [PubMed]
- Nobili, A.; Garattini, S.; Mannucci, P.M. Multiple diseases and polypharmacy in the elderly: Challenges for the internist of the third millennium. J. Comorbidity 2011, 1, 28–44. [Google Scholar] [CrossRef] [PubMed]
- Mamun, K.; Lien, C.; Goh-Tan, C.; Ang, W. Polypharmacy and inappropriate medication use in Singapore nursing homes. Ann. Acad. Med. Singap. 2004, 33, 49–52. [Google Scholar]
- Harugeri, A.; Joseph, J.; Parthasarathi, G.; Ramesh, M.; Guido, S. Prescribing patterns and predictors of high-level polypharmacy in the elderly population: A prospective surveillance study from two teaching hospitals in India. Am. J. Geriatr. Pharmacother. 2010, 8, 271–280. [Google Scholar] [CrossRef]
- Morgan, T.K.; Williamson, M.; Pirotta, M.; Stewart, K.; Myers, S.P.; Barnes, J. A national census of medicines use: A 24-hour snapshot of Australians aged 50 years and older. Med. J. Aust. 2012, 196, 50–53. [Google Scholar] [CrossRef] [PubMed]
- Onder, G.; Liperoti, R.; Fialova, D.; Topinkova, E.; Tosato, M.; Danese, P.; Gallo, P.F.; Carpenter, I.; Finne-Soveri, H.; Gindin, J. Polypharmacy in nursing home in Europe: Results from the SHELTER study. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2012, 67, 698–704. [Google Scholar] [CrossRef]
- World Health Organization. Medication Safety in Polypharmacy: Technical Report. 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/325454/WHO-UHC-SDS-2019.11-eng.pdf (accessed on 1 January 2021).
- Ros, J.; Koekkoek, T.; Kalf, A.; van den Bemt, P.; Van Kan, H. Impact of joint consultation by a clinical pharmacist and a clinical geriatrician to improve inappropriate prescribing for elderly patients. Eur. J. Hosp. Pharm. 2017, 24, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.G.; Amorim, W.W.; de Jesus, S.R.; Rodrigues, V.A.; Passos, L.C. Factors associated with potentially inappropriate medication use by the elderly in the Brazilian primary care setting. Int. J. Clin. Pharm. 2012, 34, 626–632. [Google Scholar] [CrossRef]
- Arellano, C.; Saldivia, G.; Córdova, P.; Fernández, P.; Morales, F.; López, M.; Villa, L. Using two tools to identify Potentially Inappropriate Medications (PIM) in elderly patients in Southern Chile. Arch. Gerontol. Geriatr. 2016, 67, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Fadare, J.O.; Agboola, S.M.; Opeke, O.A.; Alabi, R.A. Prescription pattern and prevalence of potentially inappropriate medications among elderly patients in a Nigerian rural tertiary hospital. Ther. Clin. Risk Manag. 2013, 9, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Hosia-Randell, H.M.; Muurinen, S.M.; Pitkälä, K.H. Exposure to potentially inappropriate drugs and drug-drug interactions in elderly nursing home residents in Helsinki, Finland. Drugs Aging 2008, 25, 683–692. [Google Scholar] [CrossRef]
- Stafford, A.C.; Alswayan, M.S.; Tenni, P.C. Inappropriate prescribing in older residents of Australian care homes. J. Clin. Pharm. Ther. 2011, 36, 33–44. [Google Scholar] [CrossRef]
- Barnett, K.; McCowan, C.; Evans, J.; Gillespie, N.D.; Davey, P.G.; Fahey, T. Prevalence and outcomes of use of potentially inappropriate medicines in older people: Cohort study stratified by residence in nursing home or in the community. BMJ Qual. Saf. 2011, 20, 275–281. [Google Scholar] [CrossRef]
- Cooper, J.A.; Cadogan, C.A.; Patterson, S.M.; Kerse, N.; Bradley, M.C.; Ryan, C.; Hughes, C.M. Interventions to improve the appropriate use of polypharmacy in older people: A Cochrane systematic review. BMJ Open 2015, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Rankin, A.; Cadogan, C.A.; Patterson, S.M.; Kerse, N.; Cardwell, C.R.; Bradley, M.C.; Ryan, C.; Hughes, C. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst. Rev. 2018, 1–186. [Google Scholar] [CrossRef] [PubMed]
- Ramli, A.; Ahmad, N.S.; Paraidathathu, T. Medication adherence among hypertensive patients of primary health clinics in Malaysia. Patient Prefer. Adherence 2012, 6, 613–622. [Google Scholar]
- Aziz, H.; Hatah, E.; Makmor-Bakry, M.; Islahudin, F.; Hamdi, N.A.; Wan, I.M.P. A comparison of medication adherence between subsidized and self-paying patients in Malaysia. Malays. Fam. Physician Off. J. Acad. Fam. Physicians Malays. 2018, 13, 2–9. [Google Scholar]
- Tan, B.Y.; Shafie, A.A.; Hassali, M.A.A.; Saleem, F. Assessment of medication adherence and the costs associated with a calendar blister pack intervention among hypertensive patients in Malaysia: A randomized controlled trial. SAGE Open Med. 2017, 5, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zelko, E.; Klemenc-Ketis, Z.; Tusek-Bunc, K. Medication adherence in elderly with polypharmacy living at home: A systematic review of existing studies. Mater. Socio Med. 2016, 28, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Gellad, W.F.; Grenard, J.L.; Marcum, Z.A. A systematic review of barriers to medication adherence in the elderly: Looking beyond cost and regimen complexity. Am. J. Geriatr. Pharmacother. 2011, 9, 11–23. [Google Scholar] [CrossRef]
- Cross, A.J.; Elliott, R.A.; Petrie, K.; Kuruvilla, L.; George, J. Interventions for improving medication-taking ability and adherence in older adults prescribed multiple medications. Cochrane Database Syst. Rev. 2020, 5, CD012419. [Google Scholar] [CrossRef] [PubMed]
- Granger, B.B.; Bosworth, H. Medication adherence: Emerging use of technology. Curr. Opin. Cardiol. 2011, 26, 279–287. [Google Scholar] [CrossRef]
- Hill, K.; Schwarz, J. Assessment and management of falls in older people. Intern. Med. J. 2004, 34, 557–564. [Google Scholar] [CrossRef]
- Bloch, F.; Thibaud, M.; Dugué, B.; Brèque, C.; Rigaud, A.; Kemoun, G. Episodes of falling among elderly people: A systematic review and meta-analysis of social and demographic pre-disposing characteristics. Clinics 2010, 65, 895–903. [Google Scholar] [CrossRef]
- Kwan, M.M.S.; Close, J.C.; Wong, A.K.W.; Lord, S.R. Falls incidence, risk factors, and consequences in Chinese older people: A systematic review. J. Am. Geriatr. Soc. 2011, 59, 536–543. [Google Scholar] [CrossRef]
- Seppala, L.J.; van de Glind, E.M.; Daams, J.G.; Ploegmakers, K.J.; de Vries, M.; Wermelink, A.M.; van der Velde, N.; Blain, H.; Bousquet, J.; Bucht, G. Fall-Risk-Increasing drugs: A systematic review and meta-analysis: III. others. J. Am. Med. Dir. Assoc. 2018, 19, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2012, CD007146. [Google Scholar] [CrossRef] [PubMed]
- Gahche, J.J.; Bailey, R.L.; Potischman, N.; Dwyer, J.T. Dietary supplement use was very high among older adults in the United States in 2011–2014. J. Nutr. 2017, 147, 1968–1976. [Google Scholar] [CrossRef]
- Agbabiaka, T.B.; Wider, B.; Watson, L.K.; Goodman, C. Concurrent use of prescription drugs and herbal medicinal products in older adults: A systematic review. Drugs Aging 2017, 34, 891–905. [Google Scholar] [CrossRef]
- Foley, H.; Steel, A.; Cramer, H.; Wardle, J.; Adams, J. Disclosure of complementary medicine use to medical providers: A systematic review and meta-analysis. Sci. Rep. 2019, 9, 1–17. [Google Scholar] [CrossRef]
- Berretta, M.; Della Pepa, C.; Tralongo, P.; Fulvi, A.; Martellotta, F.; Lleshi, A.; Nasti, G.; Fisichella, R.; Romano, C.; De Divitiis, C. Use of Complementary and Alternative Medicine (CAM) in cancer patients: An Italian multicenter survey. Oncotarget 2017, 8, 24401. [Google Scholar] [CrossRef] [PubMed]
- Berretta, M.; Bignucolo, A.; Di Francia, R.; Comello, F.; Facchini, G.; Ceccarelli, M.; Iaffaioli, R.V.; Quagliariello, V.; Maurea, N. Resveratrol in cancer patients: From bench to bedside. Int. J. Mol. Sci. 2020, 21, 2945. [Google Scholar] [CrossRef] [PubMed]
- Berretta, M.; Quagliariello, V.; Maurea, N.; Di Francia, R.; Sharifi, S.; Facchini, G.; Rinaldi, L.; Piezzo, M.; Manuela, C.; Nunnari, G. Multiple Effects of Ascorbic Acid against Chronic Diseases: Updated Evidence from Preclinical and Clinical Studies. Antioxidants 2020, 9, 1182. [Google Scholar] [CrossRef] [PubMed]
- Santos, N.S.D.; Marengo, L.L.; Moraes, F.D.S.; Barberato Filho, S. Interventions to reduce the prescription of inappropriate medicines in older patients. Rev. Saude Publica 2019, 53, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Pharmacy Program, Protocol MTAC Geriatric. 2014. Available online: https://www.pharmacy.gov.my/v2/sites/default/files/document-upload/book.protocol-geriatrik-fa-ver2_0.pdf (accessed on 7 November 2020).
- The Joanna Briggs Institute (JBI). Critical Appraisal Tools. South Australia: The University of Adelaide. 2018. Available online: https://joannabriggs.org/critical-appraisal-tools (accessed on 7 November 2020).
- Islam, M.A.; Alam, S.S.; Kundu, S.; Hossan, T.; Kamal, M.A.; Cavestro, C. Prevalence of Headache in Patients with Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-Analysis of 14,275 Patients. Front. Neurol. 2020, 11, 1–9. [Google Scholar] [CrossRef]

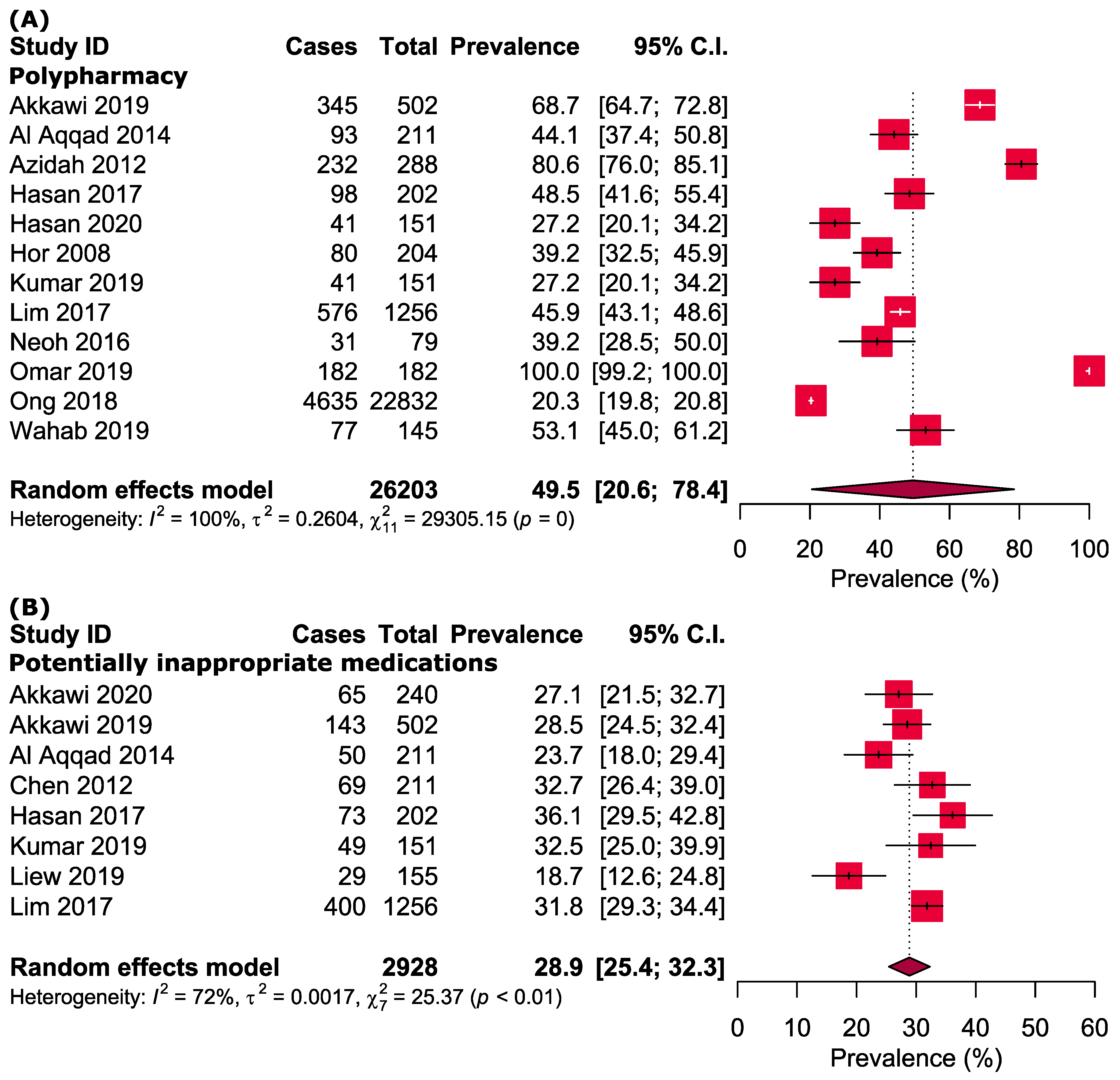
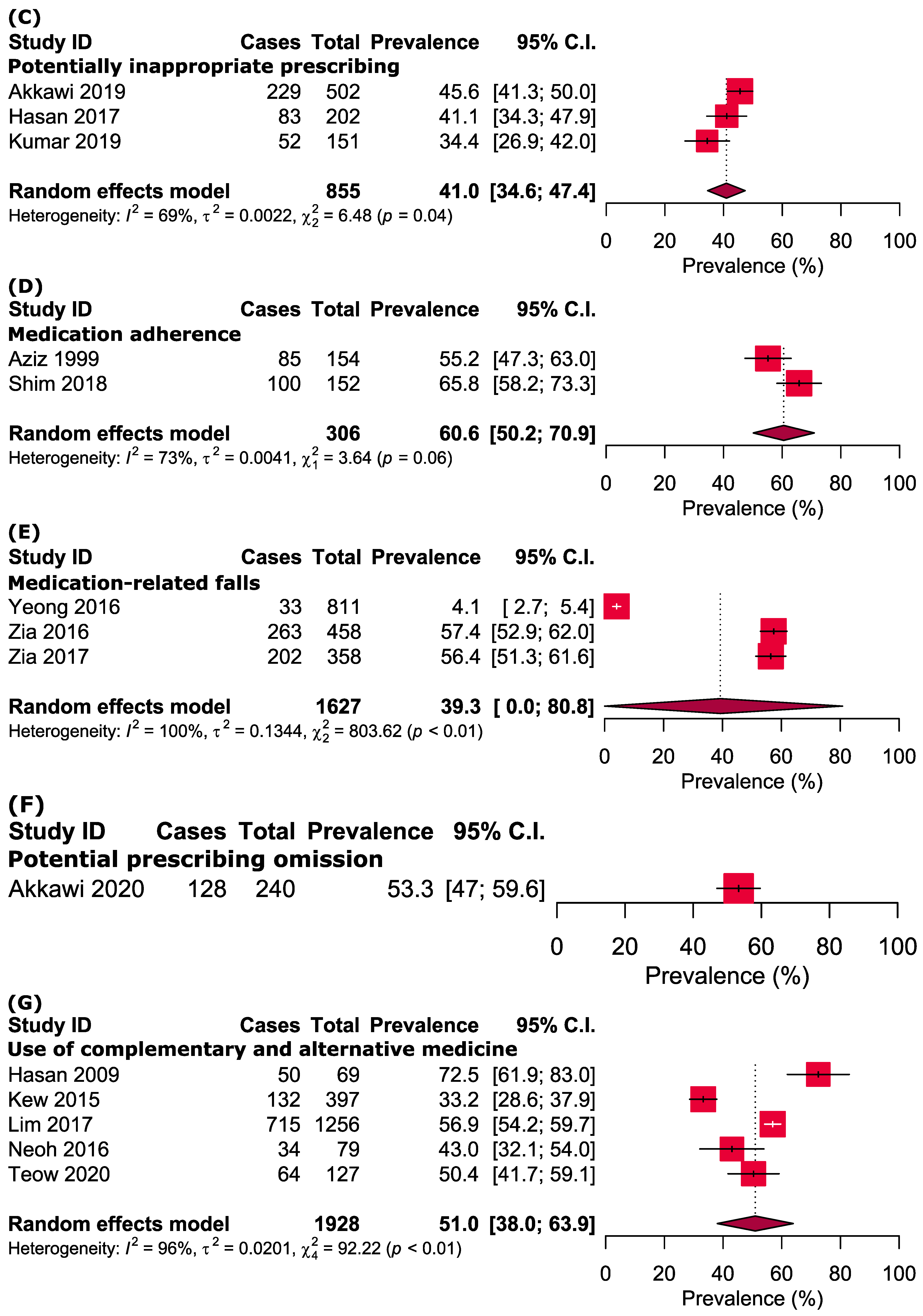
| No. | Study ID [reference] | Study Design, Settings | Sample Size (Female) | Age (Years) (Mean ± SD/Median (IQR)) | Tools/Criteria | Outcome Measurement | Results |
|---|---|---|---|---|---|---|---|
| 1 | Akkawi 2020 [35] | Cross-sectional, hospital | 240 (99) | 71.9 ± 5.8 | STOPP/START | i. PIMs ii. PPOs | i. 27% of the patients experienced PIMs. ii. 53.3% experienced PPOs. |
| 2 | Akkawi 2019 [30] | Cross-sectional, hospital | 502 (244) | 72.4 ± 5.9 | STOPP/START | i. Polypharmacy (≥5 medications) ii. PIMs iii. PPOs | i. 68.7% were taking ≥5 medications. ii. PIMs were found in 28.5%. iii. PPOs were found in 45.6%. |
| 3 | Al Aqqad 2014 [28] | Cohort study, nursing home | 211 (128) | 77.7 ± 7.0 | STOPP | i. Polypharmacy (≥5 medications) ii. PIMs | i. 44.0% were taking ≥5 medications. ii. The prevalence of PIMs was 23.7%. |
| 4 | Azidah 2012 [11] | Cross-sectional, hospital | 288 (156) | 66.9 ± 5.8 | NR | i. Polypharmacy | i. 80.6% had polypharmacy. |
| 5 | Aziz 1999 [17] | Cross-sectional, clinic | 154 (NR) | NR | Questionnaire | i. Compliance towards medication | i. 85 out of 154 elderly were not compliant towards their medications. |
| 6 | Chen 2012 [14] | Cross-sectional, nursing home | 211 (128) | 77.7 ± 7.0 | Beers criteria, STOPP/START | i. PIMs | i. PIM: 32.7% residents. |
| 7 | Hasan 2020 [19] | Cross-sectional, nursing home | 151 (74) | 74.5 ± 8.4 | Drug burden index | i. Polypharmacy | i. 27.2% of participants were taking more than five medications. |
| 8 | Hasan 2017 [18] | Cross-sectional, nursing home | 202 (126) | 76.8 ± 7.8 | Medication appropriateness index, Beers criteria and STOPP/START | i. Polypharmacy ii. PIP iii. PIMs | i. 48.3% had ≥5 prescribed medications. ii. 40.9% had at least one PIP. iii. 36.0% had at least one PIM. |
| 9 | Hasan 2009 [16] | Cross-sectional, hospital | 69 (NR) | 55.6 ± 11.2 | Questionnaire | i. CAM | i. 72.5% of the elderly used CAM. |
| 10 | Hor 2008 [20] | Cross-sectional, hospital | 204 (103) | 68.2 ± 6.3 | Questionnaire | i. Polypharmacy | i. 39.2% taking ≥5 drugs. |
| 11 | Kew 2015 [31] | Cross-sectional, community dwelling | 397 (NR) | NR | Questionnaire | i. CAM | i. 33.2% elderly respondents had experienced CAM use. |
| 12 | Kumar 2019 [21] | Cross-sectional, nursing home | 151 (74) | 74.5 ± 8.4 | Beers and STOPP | i. Polypharmacy ii. PIMs iii. PIP | i. 27.1% residents exhibited polypharmacy (≥5 medications). ii. 32.2% were exposed to PIMs. iii. 34.2% exposed to PIPs. |
| 13 | Liew 2019 [36] | Cross-sectional, nursing home | 155 (69) | 75.1 ± 8.5 | Beers and STOPP/START | i. PIMs | i. The prevalence of PIMs was 17.6% |
| 14 | Lim 2017 [13] | Cross-sectional, community dwelling | 1256 (724) | 69.0 (63.0–74.0) | Beers, Thompson Micromedex 12.0 interaction database | i. Polypharmacy ii. PIMs | i. 45.9% were using at least five medications. ii. 31.8% experienced PIMs |
| 15 | Lim 2015 [32] | Cross-sectional, clinic | 614 (354) | 68.6 ± 6.5 | Questionnaire | i. PIPs | i. Four types of PIPs. |
| 16 | Mitha 2013 [22] | Cross-sectional, community dwelling | 256 (164) | NR | Questionnaire | i. CAMs | i. 31.0% used CAM |
| 17 | Neoh 2016 [23] | Cross-sectional, community-dwelling | 79 (42) | 69.3 ± 5.9 | Questionnaire | i. Polypharmacy ii. Medication adherence | i. 39.2% had ≥4 prescribed medications. ii. 50.6% reported high adherence, 36.7% medium and 12.7% low. iii. 38.0% had problems remembering to take their medications. |
| 18 | Omar 2019 [37] | Cross-sectional, clinic | 189 (95) | 72.0 (68.0–77.0) | Questionnaire | i. Polypharmacy | i. All participants had four or more medications. ii. 47.8% of participants experienced practical problems with their medication. use, with opening medication as the most common problem. |
| 19 | Ong 2018 [33] | Cross-sectional, clinic | 22832 (13265) | 71.2 (67.3–76.0) | Questionnaire | i. Polypharmacy | i. 20.3% of the older persons presented with polypharmacy. |
| 20 | Ramachandran 2020 [24] | Cross-sectional, clinic | 90 (NR) | NR | Appropriateness of metformin prescription based on cut-off on different stages of CKD | Maximum metformin daily dose in study subjects based on CKD stage | i. 7.7% of the subjects had inappropriate metformin prescription. |
| 21 | Shim 2018 [15] | Randomized controlled trial, hospital | 152 (65) | 71.0 ± 7.0 | Medication appropriateness index and Malaysian medication adherence scale | i. Medication adherence ii. Medication appropriateness index | i. 65.8% medication nonadherence. |
| 22 | Siti 2009 [34] | Cross-sectional, community-dwelling | 6947 (NR) | NR | Questionnaire | i. CAM | i. There was no significant difference across all groups in the usage of biological-based therapies for health issues. |
| 23 | Teow 2020 [25] | Cross-sectional, community dwelling | 127 (NR) | NR | Questionnaire | i. CAM | i. 22.8% used CAM. |
| 24 | Wahab 2019 [26] | Cross-sectional, hospital | 145 (75) | 71.5 ± 8.0 | Anticholinergic drug scale | i. Polypharmacy | i. 53.1% took ≥5 drugs. ii. Patients who received medicines with ach properties had a higher risk of falls. |
| 25 | Yeong 2016 [29] | Cross-sectional, community-dwelling | 811 (448) | 70.2 ± 7.2 | Questionnaire | i. Falls | i. 4.07% elderly experienced fall in the past 1 year. ii. The odds of fall was not significantly associated with the increased number of medication use. |
| 26 | Zia 2017 [6] | Case-control, hospital | 358 (242) | Case: 75.2 ± 7.1 Control: 72.2 ± 5.5 | Structured interview | i. Fall ii. Polypharmacy and fall | i. 56.4% elderly experienced fall. ii. Polypharmacy was not associated with falls. |
| 27 | Zia 2016 [27] | Case-control, hospital | 458 (363) | Case: 75.3 ± 7.3 Control: 72.1 ± 5.5 | Anticholinergic cognitive burden scale | i. Fall ii. Anticholinergic burden association with fall | i. 57.4% elderly experienced fall in the past 12 months. |
| Subgroups | Prevalence [95% CIs] (%) | Number of Studies Analyzed | Total Number of Subjects | Heterogeneity | |
|---|---|---|---|---|---|
| I2 | p-Value | ||||
| Polypharmacy | |||||
| Community dwelling | 44.7 [39.7–49.6] | 2 | 1335 | 27% | 0.24 |
| Hospital/primary care clinic | 60.3 [16.9–100.0] | 6 | 24,153 | 100% | <0.0001 |
| Nursing home | 36.8 [25.8–47.7] | 4 | 715 | 90% | <0.0001 |
| Central region | 40.1 [33.1–47.1] | 7 | 2188 | 89% | <0.0001 |
| Eastern region | 74.6 [63.0–86.2] | 2 | 790 | 93% | <0.0001 |
| Northern region | 44.1 [37.4–50.8] | 1 | 211 | NA | NA |
| Potentially Inappropriate Medications | |||||
| Community dwelling | 31.8 [29.3–34.4] | 1 | 1256 | NA | NA |
| Hospital/primary care clinic | 28.0 [24.8–31.3] | 2 | 742 | 0% | 0.68 |
| Nursing home | 28.6 [22.1–35.1] | 5 | 930 | 80% | 0.0004 |
| Central region | 32.4 [30.1–34.7] | 3 | 1609 | 0% | 0.49 |
| Eastern region | 28.5 [24.5–32.4] | 1 | 502 | NA | NA |
| Northern region | 28.1 [19.3–36.9] | 2 | 422 | 77% | 0.03 |
| Use of Complementary and Alternative Medicines | |||||
| Community dwelling | 46.0 [32.0–59.9] | 4 | 1859 | 96% | <0.0001 |
| Hospital/primary care clinic | 72.5 [61.9–83.0] | 1 | 69 | NA | NA |
| Central region | 55.7 [46.7–64.8] | 4 | 1531 | 82% | 0.0008 |
| Eastern region | 33.2 [28.6–37.9] | 1 | 397 | NA | NA |
| Strategies of Sensitivity Analyses | Prevalence [95% CIs] (%) | Difference of Pooled Prevalence Compared to the Main Result | Number of Studies Analyzed | Total Number of Subjects | Heterogeneity | |
|---|---|---|---|---|---|---|
| I2 | p-Value | |||||
| Polypharmacy | ||||||
| Excluding small studies | 50.4 [20.0–80.0] | 1.8% higher | 11 | 26,131 | 100% | <0.0001 |
| Excluding low- and moderate-quality studies | 49.8 [28.1–71.5] | 0.6% higher | 6 | 25,293 | 100% | <0.0001 |
| Considering only cross-sectional studies | 50.0 [19.5–80.5] | 1.0% higher | 11 | 25,999 | 100% | <0.0001 |
| Excluding outlier studies | 38.2 [27.3–49.1] | 22.8% lower | 9 | 25,231 | 98% | <0.0001 |
| Potentially Inappropriate Medications | ||||||
| Excluding small studies | No small studies were available in this category | |||||
| Excluding low- and moderate-quality studies | 28.4 [24.9–31.9] | 1.7% lower | 4 | 2209 | 63% | 0.04 |
| Considering only cross-sectional studies | 29.6 [26.0–33.2] | 2.4% higher | 7 | 2717 | 71% | 0.001 |
| Excluding outlier studies | 30.2 [27.4–32.9] | 4.5% higher | 7 | 2773 | 52% | 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, C.-T.; Ang, J.-Y.; Islam, M.A.; Chan, H.-K.; Cheah, W.-K.; Gan, S.H. Prevalence of Drug-Related Problems and Complementary and Alternative Medicine Use in Malaysia: A Systematic Review and Meta-Analysis of 37,249 Older Adults. Pharmaceuticals 2021, 14, 187. https://doi.org/10.3390/ph14030187
Chang C-T, Ang J-Y, Islam MA, Chan H-K, Cheah W-K, Gan SH. Prevalence of Drug-Related Problems and Complementary and Alternative Medicine Use in Malaysia: A Systematic Review and Meta-Analysis of 37,249 Older Adults. Pharmaceuticals. 2021; 14(3):187. https://doi.org/10.3390/ph14030187
Chicago/Turabian StyleChang, Chee-Tao, Ju-Ying Ang, Md Asiful Islam, Huan-Keat Chan, Wee-Kooi Cheah, and Siew Hua Gan. 2021. "Prevalence of Drug-Related Problems and Complementary and Alternative Medicine Use in Malaysia: A Systematic Review and Meta-Analysis of 37,249 Older Adults" Pharmaceuticals 14, no. 3: 187. https://doi.org/10.3390/ph14030187
APA StyleChang, C.-T., Ang, J.-Y., Islam, M. A., Chan, H.-K., Cheah, W.-K., & Gan, S. H. (2021). Prevalence of Drug-Related Problems and Complementary and Alternative Medicine Use in Malaysia: A Systematic Review and Meta-Analysis of 37,249 Older Adults. Pharmaceuticals, 14(3), 187. https://doi.org/10.3390/ph14030187







