Patients with Robotic Arm-Assisted Medial Unicompartmental Knee Arthroplasty (mUKA) Regain Their Preoperative Activity Level Two Weeks Earlier Compared to Robotic Arm-Assisted Kinematically Aligned Total Knee Arthroplasty (rKA-TKA)
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Demographics
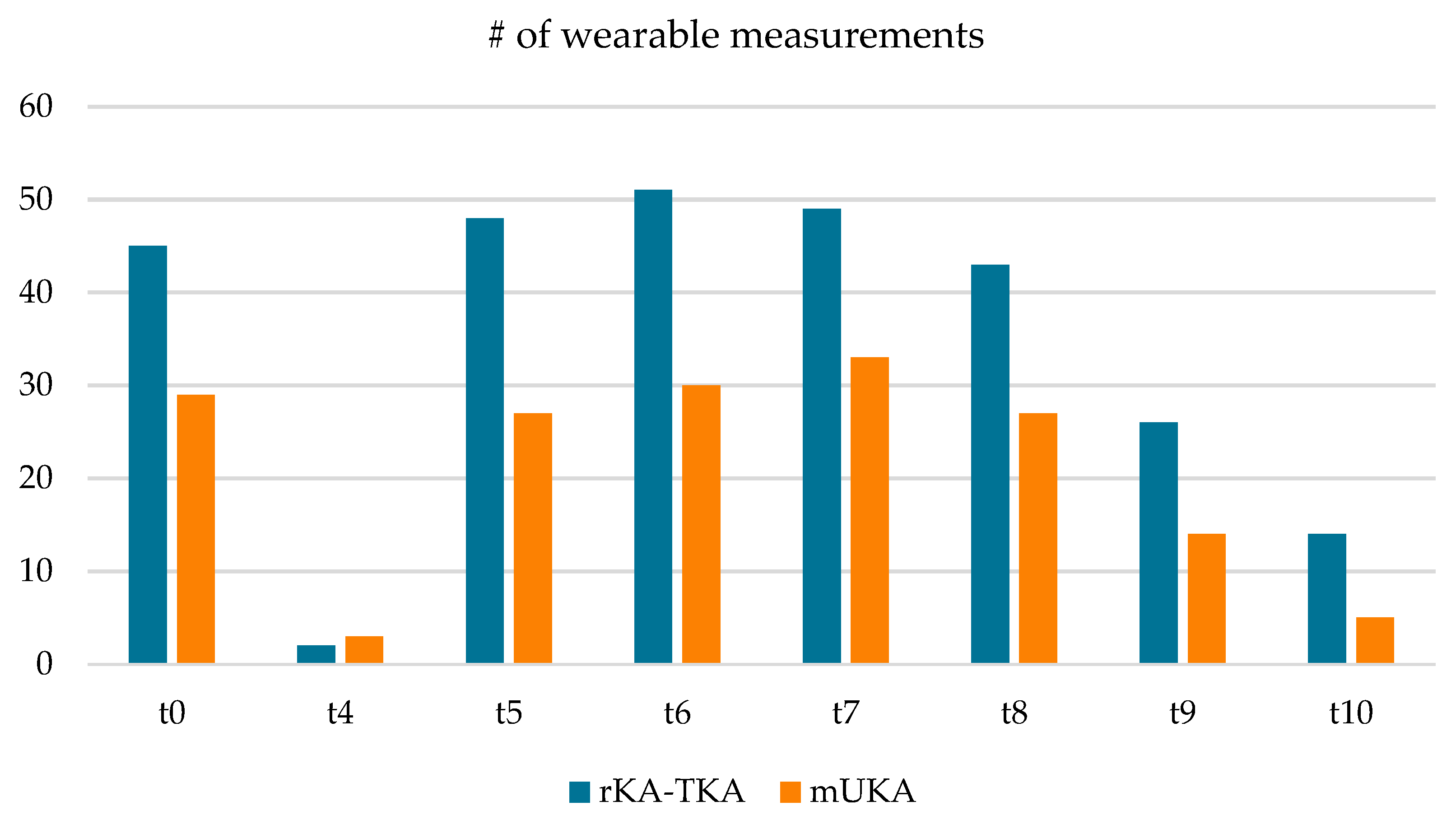
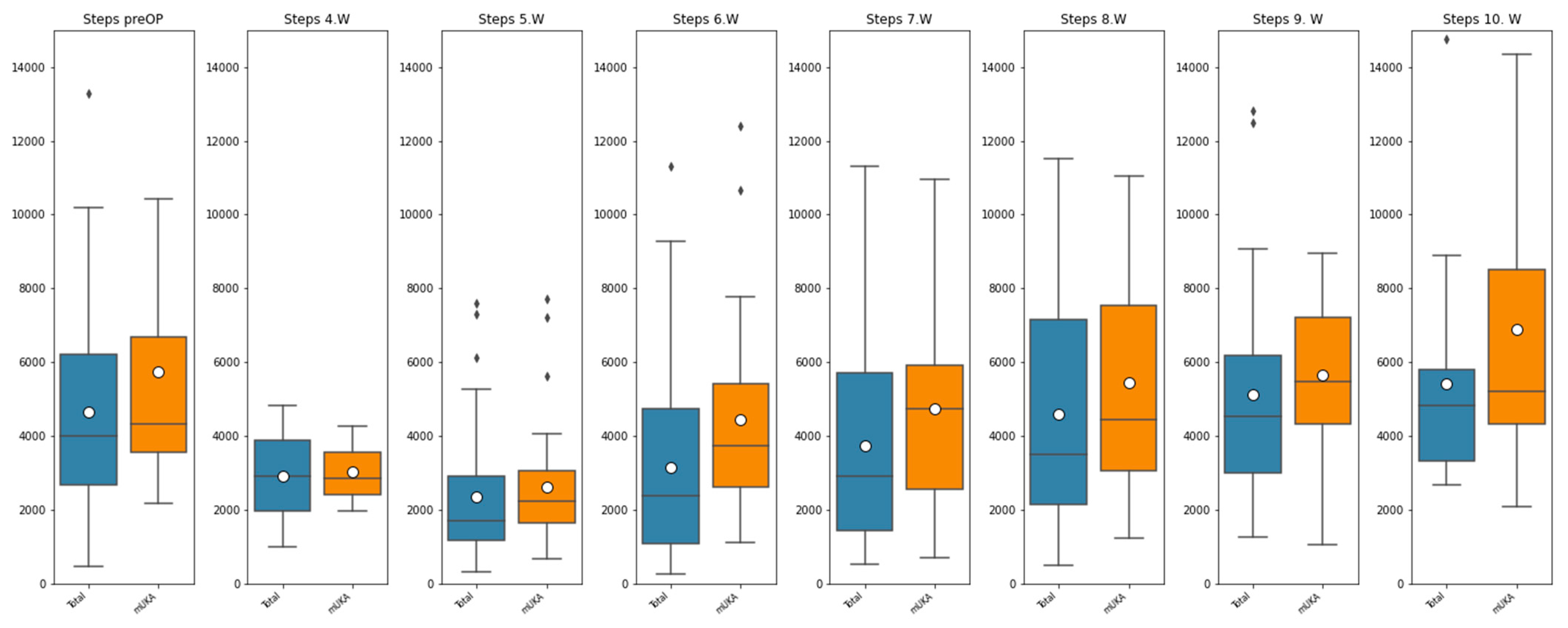
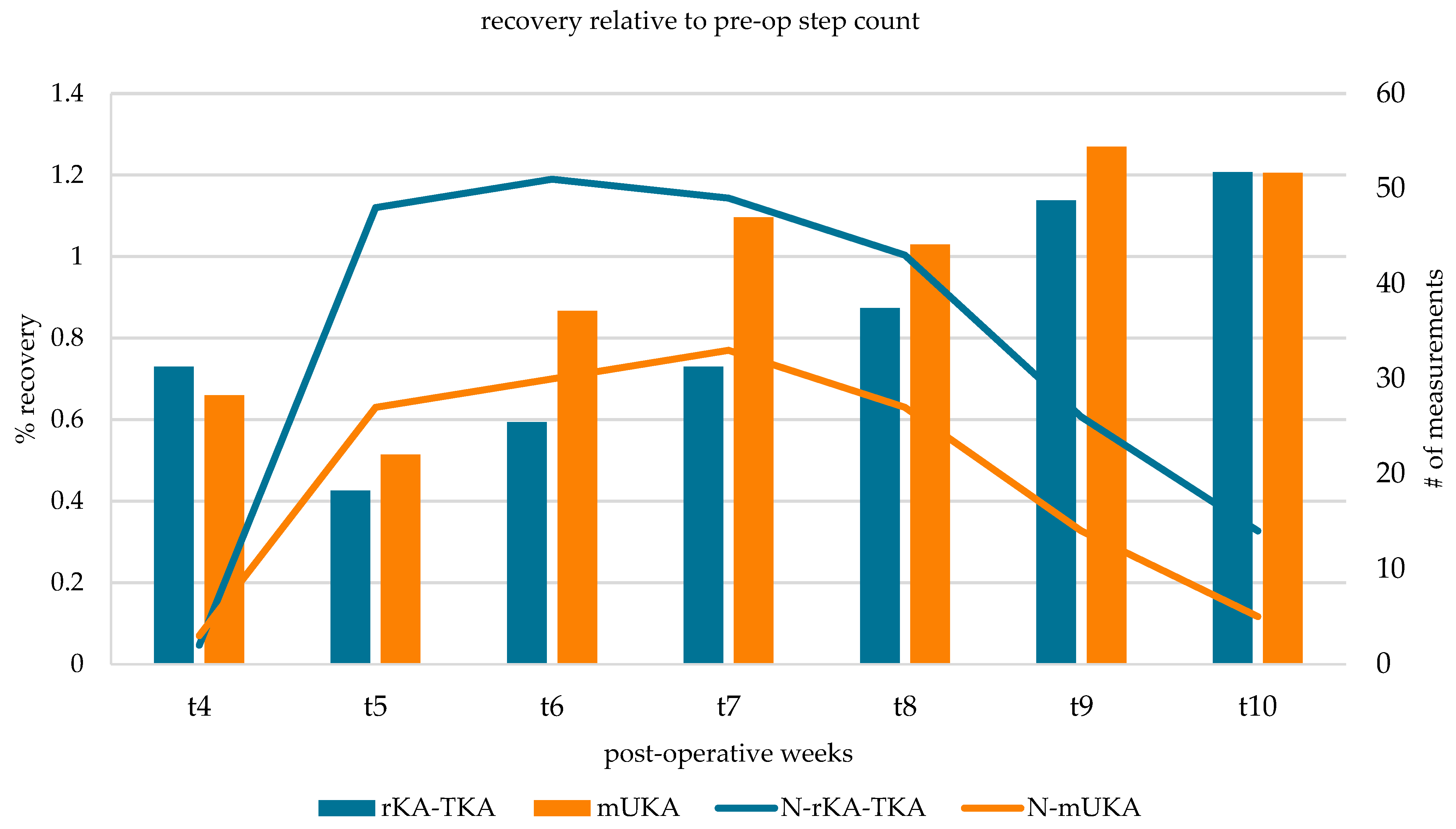
3.2. Activity Data
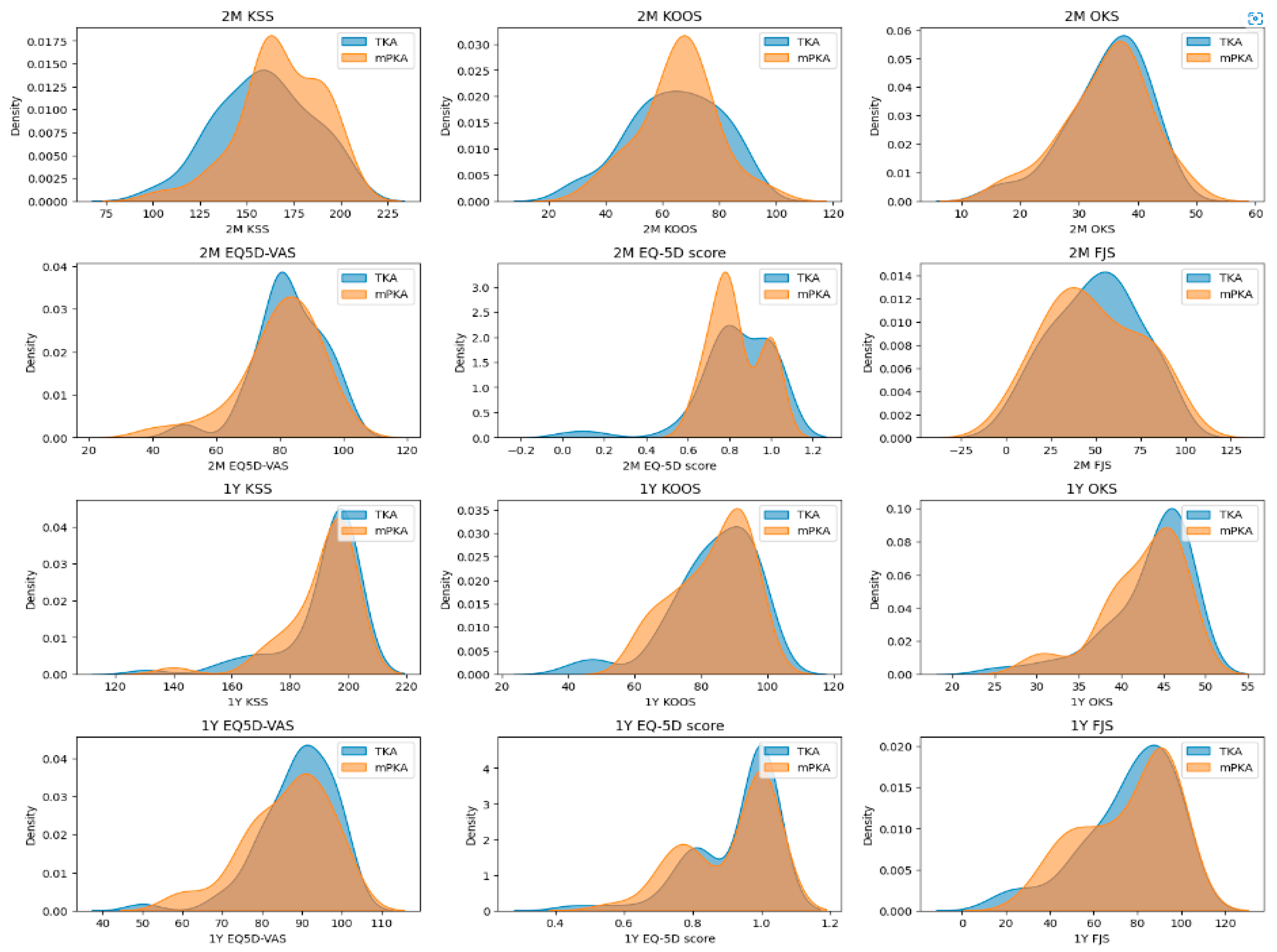
3.3. Clinical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wilson, H.A.; Middleton, R.; Abram, S.G.F.; Smith, S.; Alvand, A.; Jackson, W.F.; Bottomley, N.; Hopewell, S.; Price, A.J. Patient Relevant Outcomes of Unicompartmental versus Total Knee Replacement: Systematic Review and Meta-Analysis. BMJ 2019, 364, l352. [Google Scholar] [CrossRef]
- Maman, D.; Mahamid, A.; Yonai, Y.; Berkovich, Y. Comparing Complication Rates, Costs, and Length of Stay between Unicompartmental and Total Knee Arthroplasty: Insights from a Big Data Analysis Using the National Inpatient Sample Dataset. J. Clin. Med. 2024, 13, 3888. [Google Scholar] [CrossRef]
- Laoruengthana, A.; Reosanguanwong, K.; Rattanaprichavej, P.; Sahasoonthorn, K.; Santisathaporn, N.; Pongpirul, K. Cruciate-Retaining Total Knee Arthroplasty versus Unicompartmental Knee Arthroplasty in Medial Compartmental Osteoarthritis: A Propensity Score-Matched Analysis of Early Postoperative Recovery. Orthop. Res. Rev. 2024, 16, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Liddle, A.D.; Judge, A.; Pandit, H.; Murray, D.W. Adverse Outcomes after Total and Unicompartmental Knee Replacement in 101,330 Matched Patients: A Study of Data from the National Joint Registry for England and Wales. Lancet 2014, 384, 1437–1445. [Google Scholar] [CrossRef]
- Xia, K.; Min, L.; Xie, W.; Yang, G.; Yon, D.K.; Lee, S.W.; Koyanagi, A.; Jacob, L.; Smith, L.; Shin, J.I.; et al. Is Unicompartmental Knee Arthroplasty a Better Choice than Total Knee Arthroplasty for Unicompartmental Osteoarthritis? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Chin. Med. J. 2024, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Papalia, R.; Zampogna, B.; Torre, G.; Diaz Balzani, L.A.; Vasta, S.; Papalia, G.; De Vincentis, A.; Denaro, V. Return to Sport Activity in the Elderly Patients after Unicompartmental Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 1756. [Google Scholar] [CrossRef] [PubMed]
- Lester, D.; Barber, C.; Sowers, C.B.; Cyrus, J.W.; Vap, A.R.; Golladay, G.J.; Patel, N.K. Return to Sport Post-Knee Arthroplasty. Bone Jt. Open 2022, 3, 245–251. [Google Scholar] [CrossRef]
- Zuiderbaan, H.A.; van der List, J.P.; Khamaisy, S.; Nawabi, D.H.; Thein, R.; Ishmael, C.; Paul, S.; Pearle, A.D. Unicompartmental Knee Arthroplasty versus Total Knee Arthroplasty: Which Type of Artificial Joint Do Patients Forget? Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 681–686. [Google Scholar] [CrossRef]
- Tripathy, S.K.; Varghese, P.; Srinivasan, A.; Goyal, T.; Purudappa, P.P.; Sen, R.K.; Chandrappa, M.H. Joint Awareness after Unicompartmental Knee Arthroplasty and Total Knee Arthroplasty: A Systematic Review and Meta-Analysis of Cohort Studies. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3478–3487. [Google Scholar] [CrossRef]
- Canetti, R.; Batailler, C.; Bankhead, C.; Neyret, P.; Servien, E.; Lustig, S. Faster Return to Sport after Robotic-Assisted Lateral Unicompartmental Knee Arthroplasty: A Comparative Study. Arch. Orthop. Trauma Surg. 2018, 138, 1765–1771. [Google Scholar] [CrossRef]
- Rivière, C.; Sivaloganathan, S.; Villet, L.; Cartier, P.; Lustig, S.; Vendittoli, P.-A.; Cobb, J. Kinematic Alignment of Medial UKA Is Safe: A Systematic Review. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 1082–1094. [Google Scholar] [CrossRef] [PubMed]
- Bayoumi, T.; Burger, J.A.; Zuiderbaan, H.A.; Ruderman, L.V.; Nguyen, J.T.; Pearle, A.D. Robotic-Assisted Medial Unicompartmental Knee Arthroplasty Restores Estimated Pre-Arthritic Coronal Limb Alignment: A Retrospective Cohort Study. Knee 2023, 41, 180–189. [Google Scholar] [CrossRef]
- Mobbs, R.J.; Amin, T.; Stulberg, S.D.; Kerina, J.M.; Hernandez, V.; Bolander, R. Remote Monitoring Using Wearable Technology after Knee Arthroplasty Using a Joint-Specific Wearable Device: A Prospective Cohort Study of 435 Patients with 6 Week Follow Up. J. Orthop. Exp. Innov. 2023, 4. [Google Scholar] [CrossRef]
- Raghav, S.; Singh, A.; Mani, S.; Kumar, M. Wearable and Non-Wearable Technology Assisted Assessment and Rehabilitation Approaches for Gait Improvement among the Patients with Knee Arthroplasty: A Systematic Review. Biosci. Biotechnol. Res. Asia 2022, 19, 473–486. [Google Scholar] [CrossRef]
- Pasqualini, I.; Huffman, N.; Klika, A.; Kamath, A.F.; Higuera-Rueda, C.A.; Deren, M.E.; Murray, T.G.; Piuzzi, N.S. Stepping Up Recovery: Integrating Patient-Reported Outcome Measures and Wearable Technology for Rehabilitation Following Knee Arthroplasty. J. Knee Surg. 2024, 37, 757–763. [Google Scholar] [CrossRef]
- Innocenti, M.; Zanna, L.; Akkaya, M.; Huber, K.; Christen, B.; Calliess, T. Setting the Tibial Component Rotation Based on Femoral Landmarks Allows Congruent Knee Kinematics in Robotic-Assisted Medial Unicompartmental Knee Replacement. J. Pers. Med. 2023, 13, 632. [Google Scholar] [CrossRef] [PubMed]
- Huber, K.; Christen, B.; Calliess, S.; Calliess, T. True Kinematic Alignment Is Applicable in 44% of Patients Applying Restrictive Indication Criteria—A Retrospective Analysis of 111 TKA Using Robotic Assistance. J. Pers. Med. 2021, 11, 662. [Google Scholar] [CrossRef]
- Smith, J.D.; Guerra, G.; Burkholder, B.G. The Validity and Accuracy of Wrist-Worn Activity Monitors in Lower-Limb Prosthesis Users. Disabil. Rehabil. 2020, 42, 3182–3188. [Google Scholar] [CrossRef]
- Foster, J.I.; Williams, K.L.; Timmer, B.H.B.; Brauer, S.G. Concurrent Validity of the Garmin Vivofit®4 to Accurately Record Step Count in Older Adults in Challenging Environments. J. Aging Phys. Act. 2022, 30, 833–841. [Google Scholar] [CrossRef]
- Virtanen, P.; Gommers, R.; Oliphant, T.E.; Haberland, M.; Reddy, T.; Cournapeau, D.; Burovski, E.; Peterson, P.; Weckesser, W.; Bright, J.; et al. SciPy 1.0: Fundamental Algorithms for Scientific Computing in Python. Nat. Methods 2020, 17, 261–272. [Google Scholar] [CrossRef]
- Liu, B.; Feng, C.; Tu, C. Kinematic Alignment versus Mechanical Alignment in Primary Total Knee Arthroplasty: An Updated Meta-Analysis of Randomized Controlled Trials. J. Orthop. Surg. Res. 2022, 17, 201. [Google Scholar] [CrossRef]
- Gilmour, A.; MacLean, A.D.; Rowe, P.J.; Banger, M.S.; Donnelly, I.; Jones, B.G.; Blyth, M.J.G. Robotic-Arm–Assisted vs Conventional Unicompartmental Knee Arthroplasty. The 2-Year Clinical Outcomes of a Randomized Controlled Trial. J. Arthroplast. 2018, 33, S109–S115. [Google Scholar] [CrossRef] [PubMed]
- Banger, M.; Doonan, J.; Rowe, P.; Jones, B.; MacLean, A.; Blyth, M.J.B. Robotic Arm-Assisted versus Conventional Medial Unicompartmental Knee Arthroplasty: Five-Year Clinical Outcomes of a Randomized Controlled Trial. Bone Jt. J. 2021, 103-B, 1088–1095. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; Bell, A.; Simpson, P.; Macpherson, G.; Patton, J.T.; Hamilton, D.F. Robotic-Assisted Unicompartmental Knee Arthroplasty Has a Greater Early Functional Outcome When Compared to Manual Total Knee Arthroplasty for Isolated Medial Compartment Arthritis. Bone Jt. Res. 2020, 9, 15–22. [Google Scholar] [CrossRef]
- Zambianchi, F.; Daffara, V.; Negri, A.; Franceschi, G.; Schiavon, G.; Catani, F. Preoperative Osteoarthritic Grade Affects Forgotten Joint Status and Patient Acceptable Symptom State After Robotic Arm-Assisted Unicompartmental Knee Arthroplasty. J. Arthroplast. 2021, 36, 3650–3655. [Google Scholar] [CrossRef] [PubMed]
- Daffara, V.; Zambianchi, F.; Festa, E.; Cuoghi Costantini, R.; Clemenza, S.; Catani, F. High Return to Sport Rate in Patients Undergoing Image-Based Robotic Arm Assisted Unicompartmental Knee Arthroplasty. Arch. Orthop. Trauma Surg. 2023, 144, 4037–4044. [Google Scholar] [CrossRef]
- Zambianchi, F.; Franceschi, G.; Rivi, E.; Banchelli, F.; Marcovigi, A.; Khabbazè, C.; Catani, F. Clinical Results and Short-Term Survivorship of Robotic-Arm-Assisted Medial and Lateral Unicompartmental Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1551–1559. [Google Scholar] [CrossRef]
- Zambianchi, F.; Seracchioli, S.; Franceschi, G.; Cuoghi Costantini, R.; Malatesta, A.; Barbo, G.; Catani, F. Image-based Robotic-arm Assisted Unicompartmental Knee Arthroplasty Provides High Survival and Good-to-excellent Clinical Outcomes at Minimum 10 Years Follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5477–5484. [Google Scholar] [CrossRef]
- Abhari, S.; Hsing, T.M.; Malkani, M.M.; Smith, A.F.; Smith, L.S.; Mont, M.A.; Malkani, A.L. Patient Satisfaction Following Total Knee Arthroplasty Using Restricted Kinematic Alignment. Bone Jt. J. 2021, 103-B, 59–66. [Google Scholar] [CrossRef]
- Wu, K.A.; Dilbone, E.S.; Kugelman, D.N.; Goel, R.K.; Ryan, S.P.; Wellman, S.S.; Bolognesi, M.P.; Seyler, T.M. Daily Physical Activity Following Unicompartmental Knee Arthroplasty: A Pilot Study. J. Exp. Orthop. 2024, 11, e70048. [Google Scholar] [CrossRef]
- Crizer, M.P.; Kazarian, G.S.; Fleischman, A.N.; Lonner, J.H.; Maltenfort, M.G.; Chen, A.F. Stepping Toward Objective Outcomes: A Prospective Analysis of Step Count After Total Joint Arthroplasty. J. Arthroplast. 2017, 32, S162–S165. [Google Scholar] [CrossRef] [PubMed]
- Twiggs, J.; Salmon, L.; Kolos, E.; Bogue, E.; Miles, B.; Roe, J. Measurement of Physical Activity in the Pre- and Early Post-Operative Period after Total Knee Arthroplasty for Osteoarthritis Using a Fitbit Flex Device. Med. Eng. Phys. 2018, 51, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Cushner, F.D.; Hunter, O.F.; Lee, D.C. How Active Are Our Patients in the First 6 Weeks Following Total Knee Arthroplasty? J. Arthroplast. 2024, 39, S125–S129. [Google Scholar] [CrossRef]
- Bensa, A.; Sangiorgio, A.; Deabate, L.; Illuminati, A.; Pompa, B.; Filardo, G. Robotic-Assisted Unicompartmental Knee Arthroplasty Improves Functional Outcomes, Complications, and Revisions a Systematic Review and Meta-Analysis. Bone Jt. Open 2024, 5, 374–384. [Google Scholar] [CrossRef] [PubMed]
- Begum, F.A.; Kayani, B.; Morgan, S.D.J.; Ahmed, S.S.; Singh, S.; Haddad, F.S. Robotic Technology: Current Concepts, Operative Techniques and Emerging Uses in Unicompartmental Knee Arthroplasty. EFORT Open Rev. 2020, 5, 312–318. [Google Scholar] [CrossRef]
- Fontalis, A.; Raj, R.D.; Haddad, I.C.; Donovan, C.; Plastow, R.; Oussedik, S.; Gabr, A.; Haddad, F.S. Length of Stay and Discharge Dispositions Following Robotic Arm-Assisted Total Knee Arthroplasty and Unicompartmental Knee Arthroplasty versus Conventional Technique and Predictors of Delayed Discharge. Bone Jt. Open 2023, 4, 791–800. [Google Scholar] [CrossRef]
- Bhimani, S.J.; Bhimani, R.; Smith, A.; Eccles, C.; Smith, L.; Malkani, A. Robotic-Assisted Total Knee Arthroplasty Demonstrates Decreased Postoperative Pain and Opioid Usage Compared to Conventional Total Knee Arthroplasty. Bone Jt. Open 2020, 1, 8–12. [Google Scholar] [CrossRef]
- Maman, D.; Laver, L.; Becker, R.; Mahamid, A.; Berkovich, Y. Robotic-assisted Total Knee Arthroplasty Reduces Postoperative Complications and Length of Stay without Increased Cost Compared to Navigation-guided Techniques: A National Analysis. Knee Surg. Sports Traumatol. Arthrosc. 2024, 33, 336–342. [Google Scholar] [CrossRef]
- Kievit, A.J.; Kuijer, P.P.F.M.; de Haan, L.J.; Koenraadt, K.L.M.; Kerkhoffs, G.M.M.J.; Schafroth, M.U.; van Geenen, R.C.I. Patients Return to Work Sooner after Unicompartmental Knee Arthroplasty than after Total Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 2905–2916. [Google Scholar] [CrossRef]
| rKA-TKA (n = 53) | mUKA (n = 359) | p-Value | |
|---|---|---|---|
| Age (mean, SD) | 68.6 (7.7) | 66.7 (8.8) | 0.283 |
| Height (mean, SD) | 169.1 (8.6) | 171.5 (9.1) | 0.227 |
| Weight (mean, SD) | 79.9 (17.6) | 81.9 (14.4) | 0.578 |
| BMI (mean, SD) | 27.8 (4.9) | 27.7 (3.6) | 0.912 |
| Gender (F:M) | 66%:34% | 51%:49% | 0.251 |
| Side (L:R) | 66%:34% | 43%:57% | 0.054 |
| ASA (I:II:III) | 13%:74%:13% | 34%:46%:20% | 0.023 * |
| Physical demand level (A:B:C:D) | 19%:49%:26%:6% | 9%:40%:42%:9% | 0.274 |
| t0 | t4 | t5 | t6 | t7 | t8 | t9 | t10 | ||
|---|---|---|---|---|---|---|---|---|---|
| rKA-TKA | count | 45 | 2 | 48 | 51 | 49 | 43 | 26 | 14 |
| median | 3988 | 2911 | 1700 | 2370 | 2910 | 3383 | 4538 | 4814 | |
| min | 462 | 987 | 325 | 263 | 516 | 480 | 1241 | 2662 | |
| max | 13,297 | 4834 | 7608 | 11,307 | 11,317 | 11,523 | 12,822 | 14,755 | |
| IQR | 2674–6220 | 1949–3872 | 1158–2920 | 1067–4742 | 1433–5704 | 2133–7140 | 2982–6182 | 3314–5803 | |
| mUKA | count | 29 | 3 | 27 | 30 | 33 | 27 | 14 | 5 |
| median | 4315 | 2846 | 2217 | 3741 | 4730 | 4444 | 5479 | 5203 | |
| min | 2173 | 1971 | 667 | 1093 | 703 | 1230 | 1058 | 2082 | |
| max | 20,729 | 4254 | 7715 | 12,391 | 10,945 | 11,032 | 8948 | 14,336 | |
| IQR | 3540–6683 | 2409–3065 | 2619–5406 | 2619–5406 | 2556–5923 | 4044–7549 | 4308–7223 | 4328–8496 | |
| p-value | 0.128 ‡ | N/A | 0.277 ‡ | 0.015 ‡ * | 0.048 ‡ * | 0.193 ‡ | 0.275 ‡ | N/A |
| 2 Months Follow-Up | 1 Year Follow-Up | |||||
|---|---|---|---|---|---|---|
| rKA-TKA | mUKA | p-Value | rKA-TKA | mUKA | p-Value | |
| n = | 49 | 35 | - | 49 | 34 | - |
| KSS (mean, SD) | 159.0 (24.7) | 168.0 (21.5) | 0.083 † | 191.2 (14.0) | 190.5 (12.3) | 0.495 ‡ |
| KOOS (mean, SD) | 64.4 (15.7) | 65.5 (13.3) | 0.744 † | 83.5 (12.9) | 83.1 (10.9) | 0.581 ‡ |
| OKS (mean, SD) | 34.7 (6.9) | 34.5 (7.2) | 0.881 † | 43.4 (5.1) | 42.5 (4.7) | 0.214 ‡ |
| EQ-5D-VAS (mean, SD) | 82.8 (10.7) | 80.0 (12.8) | 0.42 ‡ | 88.9 (9.4) | 86.2 (10.5) | 0.253 ‡ |
| EQ-5D-5L (mean, SD) | 0.83 (0.19) | 0.83 (0.12) | 0.451 ‡ | 0.92 (0.12) | 0.91 (0.13) | 0.458 ‡ |
| FJS (mean, SD) | 50.0 (23.8) | 48.1 (26.0) | 0.734 † | 76.1 (20.9) | 75.4 (20.3) | 0.791 ‡ |
| FJS (median, IQR) | 51.0 (34.4) | 46.9 (37.0) | - | 79.2 (28.1) | 85.4 (29.2) | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Theus-Steinmann, C.; Witvoet-Braam, S.; Huber, K.; Calliess, S.; Christen, B.; Calliess, T. Patients with Robotic Arm-Assisted Medial Unicompartmental Knee Arthroplasty (mUKA) Regain Their Preoperative Activity Level Two Weeks Earlier Compared to Robotic Arm-Assisted Kinematically Aligned Total Knee Arthroplasty (rKA-TKA). Sensors 2025, 25, 1668. https://doi.org/10.3390/s25061668
Theus-Steinmann C, Witvoet-Braam S, Huber K, Calliess S, Christen B, Calliess T. Patients with Robotic Arm-Assisted Medial Unicompartmental Knee Arthroplasty (mUKA) Regain Their Preoperative Activity Level Two Weeks Earlier Compared to Robotic Arm-Assisted Kinematically Aligned Total Knee Arthroplasty (rKA-TKA). Sensors. 2025; 25(6):1668. https://doi.org/10.3390/s25061668
Chicago/Turabian StyleTheus-Steinmann, Carlo, Sietske Witvoet-Braam, Kim Huber, Sarah Calliess, Bernhard Christen, and Tilman Calliess. 2025. "Patients with Robotic Arm-Assisted Medial Unicompartmental Knee Arthroplasty (mUKA) Regain Their Preoperative Activity Level Two Weeks Earlier Compared to Robotic Arm-Assisted Kinematically Aligned Total Knee Arthroplasty (rKA-TKA)" Sensors 25, no. 6: 1668. https://doi.org/10.3390/s25061668
APA StyleTheus-Steinmann, C., Witvoet-Braam, S., Huber, K., Calliess, S., Christen, B., & Calliess, T. (2025). Patients with Robotic Arm-Assisted Medial Unicompartmental Knee Arthroplasty (mUKA) Regain Their Preoperative Activity Level Two Weeks Earlier Compared to Robotic Arm-Assisted Kinematically Aligned Total Knee Arthroplasty (rKA-TKA). Sensors, 25(6), 1668. https://doi.org/10.3390/s25061668









