Overview of Respiratory Sensor Solutions to Support Patient Diagnosis and Monitoring
Abstract
1. Introduction
2. Materials and Methods
3. Open Database
- Simultaneous physiological measurements with five devices at different cognitive and physical loads: Measurement included electrocardiography (ECG), photoplethysmography, accelerometry, oxygen saturation respiration, heart rate (HR), heart rate variability (HRV), and RR intervals ranging from 1 Hz to 8000 Hz [6].
- MIMIC-IV waveform database: The MIMIC-IV waveform database is a collection of physiological signals and measurements from patients in intensive care units, including electrocardiograms, photoplethysmograms, respiratory parameters, blood pressure measured invasively and non-invasively, and other measurements. These measurements and signals are obtained directly from the bedside monitor and provide a detailed picture of the physiology of critically ill patients [7].
- NInFEA: Non-Invasive Multimodal Fetal ECG-Doppler Dataset for Antenatal Cardiology Research: The first publicly available dataset of simultaneous non-invasive electrophysiological recordings, fetal pulsed-wave Doppler (PWD), and maternal respiratory signals [8].
- Electrocardiogram, skin conductance and respiration from spider-fearful individuals watching spider video clips: This project includes an electrocardiogram, skin conductance, and respiration as raw data (unfiltered, unprocessed) recorded from consenting individuals afraid of spiders using a BITalino portable biosignal measurement device (PLUX—Wireless Biosignals SA, Lisbon, Portugal) with a sampling rate set to 100 Hz per channel at a resolution of 10 bits [9].
- MIMIC-III waveform database: The MIMIC-III waveform database contains 67,830 sets of records for approximately 30,000 intensive care unit patients. The majority of record sets include a waveform record containing digital signals (usually including ECG, ABP, respiration, and PPG) and a ‘numerical’ record containing a time series of periodic measurements, each representing a quasi-continuous record of vital signs [10].
- MIMIC-III waveform database matched subset: Matched subset of the ‘MIMIC-III waveform database’. Matches records with the older clinical database ‘MIMIC-III clinical database’. Contains 22,317 waveform records and 22,247 numerical records for 10,282 different ICU patients [11].
- Cerebral Vasoregulation in Elderly with Stroke: Contains multimodal data from a large study investigating the effects of ischemic stroke on cerebral vasoregulation. The cross sectional study compared 60 subjects who suffered strokes to 60 control subjects, collecting the following data for each patient across multiple days: transcranial Doppler of cerebral arteries, 24 h blood pressure numerics, high resolution waveforms (ECG, blood pressure, CO2, and respiration) during various movement tasks, 24 h ECG, EMG (electromyography), accelerometer recordings, and gait pressure recordings during a walking test [12].
- BIDMC PPG and Respiration Dataset: Dataset contains signals and numerics extracted from the larger MIMIC II matched waveform database, along with manual breath annotations made from two annotators using the impedance respiratory signal [13].
- Pressure, flow, and dynamic thoraco-abdominal circumferences data for adults breathing under CPAP therapy: This database of respiratory pressure, flow, and dynamic chest and abdominal circumferences was collected from 30 healthy adults at the University of Canterbury. Measurements were made using a bidirectional Venturi taper and a tape measure with rotary encoders, which recorded chest expansion and contraction at different pressures and breathing conditions. The data were intended to validate respiratory monitoring systems for use in primary care and home settings [14].
- Cerebral perfusion and cognitive decline in type 2 diabetes: This collection includes studies on vasoregulation and blood flow involving 70 patients with type 2 diabetes and 70 healthy control patients aged 50–85 years [15].
- Cerebromicrovascular Disease in Elderly with Diabetes: This database from a prospective study evaluates the effects of type 2 diabetes on cerebral vasoregulation, perfusion, and functional outcomes in 69 participants aged 55–75 with diabetes and in a control group. Data include measurements of blood flow, pressure, heart rate, respiratory parameters, gait, balance, and MRI images, including CASL, FLAIR, and DTI [16].
- CPAP Pressure and Flow Data from a Local Trial of 30 Adults at the University of Canterbury: The study includes pressure and flow measurements during breathing with CPAP (Continuous Positive Airway Pressure) from 30 patients [17].
- Upper body thermal images and associated clinical data from a pilot cohort study of COVID-19: The database contains upper-body thermal recordings from 252 patients in the COVID-19 study who performed breath-holds in four positions. The data include PCR results, demographics, vital signs, activities, medications, respiratory symptoms, and respiratory rate. The aim of the study was to analyze temperature patterns for developing algorithms to analyze thermal recordings [18].
- MIMIC-III and eICU-CRD: Feature Representation by FIDDLE Preprocessing: This collection of data is derived from the MIMIC-III and eICU databases, and includes the features and labels for five prediction tasks related to three adverse outcomes: in-hospital mortality (48 h), acute respiratory failure (4 h, 12 h), and shock (4 h, 12 h) [19].
- Cerebral Vasoregulation in Diabetes: A database of studies evaluating the effects of type 2 diabetes on cerebral vasoregulation and body function. It contains data from 37 diabetics and 49 control subjects aged 55–75, with continuous measurements of cerebral blood flow (TCD, MRI), heart rate, blood pressure, respiratory parameters, balance, gait, and laboratory results [20].
- OpenOximetry Repository: The OpenOximetry database contains clinical and laboratory data on pulse oximetry, including high-frequency waveforms, oxygen saturation readings, and other physiological parameters. It enables research on the impact of physiological variables on pulse oximeter performance [21].
- A Temporal Dataset for Respiratory Support in Critically Ill Patients: The dataset includes 90-day hourly respiratory parameters, such as ventilation data, breathing support interventions, and other parameters from 50,920 ICU patients. The data are sourced from MIMIC v2.2 and also contain laboratory results and therapy details [22].
- Respiratory and heart rate monitoring dataset from aeration study: The dataset includes respiratory pressure and flow, electrical impedance tomography (EIT), ECG, and heart rate belt (HRB) data collected from 20 healthy individuals. Participants breathed through a full-face mask with a pressure gauge and flowmeter [23].
- Simulated Obstructive Disease Respiratory Pressure and Flow: The dataset includes respiratory pressure and flow parameters collected from 20 healthy adults simulating COPD effects, such as gas trapping during exhalation. Tests were conducted using a Venturi splitter with a device attached to the oral exhalation outlet [24].
- Respiratory dataset from PEEP study with expiratory occlusion: The dataset includes respiratory pressure and flow, dynamic chest and abdominal circumference data, and aeration from EIT, which were collected from 80 adults. Participants breathed with CPAP support, and the study was conducted with approval from the University of Canterbury HREC [25].
- Cough Database contains samples of coughing and other breathing-related sounds. It is a useful source of data for research on respiratory problems [26].
- Chronic Obstructive Pulmonary Disease Gene “COPDGene” is a multi-center research project to understand and investigate the causes and mechanisms of chronic obstructive pulmonary disease (COPD), a serious respiratory condition [29].
4. Algorithms
5. Results
| Authors (Year) | Methods | Description |
|---|---|---|
| Parameters | ||
| Keywords: Respiratory Belt [Index Terms, Autor Keywords, IEEE Terms] | ||
| Coronel et al., 2021 [58] | 3D Camera, SpO2 desaturation. | Using the respiratory signal from a 3D camera, a new algorithm was developed that detects reduced respiratory motion and SpO2 desaturation to evaluate respiratory events |
| Respiratory motion. | ||
| He et al., 2020 [59] | “Kinect” sensor, IR-UWB Radar. | A system for monitoring respiratory rate in a room using three impulse radio ultra-wideband (IR-UWB) radars and a Kinect camera. The IR-UWB radar system covers the entire room, allowing for the respiratory monitoring of individuals regardless of their orientation relative to the radar. The Kinect camera tracks 3D joint coordinates, enabling the precise localization of individuals. The results demonstrated high effectiveness in tracking both single and multiple subjects and in estimating respiratory rate. |
| Respiratory motion. | ||
| Kusche et al., 2022 [60] | 32-channel differential EMG. | A novel non-invasive respiratory monitoring device using a dry electrode belt for capturing diaphragm EMG signals from the thorax. |
| Respiration through thorax movement. | ||
| Vanbuis et al., 2022 [61] | Cardio-respiratory polysomnography, tracheal sound sensors. | The three-step sleep scoring model for Type III sleep studies was trained and tested using 300 and 100 independent recordings from patients suspected of having sleep breathing disorders, with the steps as follows: classification using a multi-layer perceptron, correction of sleep transition rules according to AASM guidelines, and sequence correction using a Viterbi hidden Markov model. |
| Sound, respiration, heart rate, oxidation. | ||
| Alam et al., 2019 [62] | Electronic circuit with a push button (Arduino) integrated into a chest belt. | A non-invasive, wearable solution to track and analyze respiratory rate in real time. The circuit detects chest movements associated with breathing, and the push button registers these movements to calculate and display the respiratory rate via a Bluetooth application. |
| Respiratory rate. | ||
| Qiu et al., 2021 [63] | Two-electrode bioimpedance (BioZ) sensor. | It can be used for the accurate monitoring of breathing rate in both static and dynamic conditions, including the calculation of the respiratory rate. The sensor measures the change in chest impedance resulting from breathing. Additionally, an integrated medical-grade infrared temperature sensor allows for body temperature measurement. The recorded data are transmitted via a Bluetooth module to a computer for processing and visualization. |
| Respiratory rate. | ||
| Sharma et al., 2019 [64] | Radio frequency (RF) sensor (near-field coherent sensing) placed near the xiphoid process. | The sensor uses an RF signal at a frequency of 1.8 GHz, which is modulated by the movement of internal organs and then received and demodulated by the receiving antenna. This sensor enables the monitoring of breathing rate and lung volume by detecting peaks in the respiratory cycle. |
| Respiratory rate, lung volume. | ||
| Laufer et al., 2020 [65] | Thoracic belt to measure changes in the circumference of the chest or abdomen. | This belt allows for the accurate monitoring of changes in body circumference, enabling the determination of respiratory parameters such as breathing rate. The measurement results were compared with a motion capture system, which served as a reference. |
| Respiratory rate, tidal volume. | ||
| Nedoma et al., 2018 [66] | Optical interferometric sensor based on fiber-optic and connected to an optical interrogator. | Measures respiratory rate and pulse rate and allows for the improvement of MR images of the head, compensating the respiratory motion. The sensor is encased in a thin layer of polyurethane, which provides immunity to electromagnetic interference (EMI) and allows its use in environments with magnetic resonance imaging (MRI). |
| Respiratory rate, heart rate. | ||
| Shakhih et al., 2018 [67] | Infrared thermal imaging camera (ITI). | Uses an infrared thermal imaging camera (ITI) for thermal imaging to assess the timing of inspiration (TI) and expiration (TE) during prolonged expiration breathing. |
| Respiratory rate. | ||
| Nassi et al., 2022 [68] | Polysomnography, artificial neural network. | Uses a neural network (WaveNet) to analyze 9656 polysomnographic recordings from Massachusetts General Hospital (MGH). It detects obstructive apnea, central apnea, hypopnea, and respiratory effort-related arousals. |
| Respiratory rate, apnea. | ||
| Tataraidze et al., 2019 [69] | Wi-Fi signal. | Analyzes channel status information (CSI) from the Wi-Fi connection between the smartphone and the access point for breath detection. |
| Respiratory rate. | ||
| Wang et al., 2021 [70] | Breathing sensor in the form of a piezoresistive matrix. | It is used to monitor force distribution and dynamic resistance waveforms for respiratory rate analysis. The matrix (composed of graphite and silver paste) is placed on the mattress to record changes in the pressure exerted on it during breathing. |
| Respiratory rate. | ||
| Erdyarahman et al., 2022 [71] | A non-contact radar system using frequency-modulated continuous wave (FMCW) technology. | The radar uses frequency-modulated continuous wave (FMCW) technology to monitor small movements in near real time. Electromagnetic waves are emitted by a transmitting antenna (Tx), reflected off a target (e.g., chest), and received by a receiving antenna (Rx). |
| Respiratory rate. | ||
| Cruz et al., 2021 [72] | Pulse oximeter, artificial neural network. | The selected five pulse rate features, namely, time of peaks, peaks, time of valleys, valleys, and time since the last peak, provide a proper estimation of RR. The neural network helps in the classification of the labels of valleys such as inspiration, expiration, and neutral. |
| Respiratory rate through heart rate. | ||
| Bevilacqua et al., 2022 [73] | Piezoelectric belt, data acquisition is via a DAQ board. | The algorithm takes advantage of an adaptive bandwidth filter to identify the breathing condition and to quantitatively determine the respiratory rate. The algorithm detects moments of dyspnea by identifying outliers. Początek formularzaDół formularza |
| Respiratory rate. | ||
| Guede-Fernandez et al., 2019 [74] | Respiratory inductance plethysmography (RIP) belt. | Drowsiness detection is based on the real-time analysis of respiratory rate variability (RRV) using an RIP belt and signal quality assessment to reduce the number of false alarms associated with body movements. The method includes signal quality assessment to reduce false alarms caused by body movements, rather than drowsiness. |
| Respiratory rate. | ||
| Sanae et al., 2022 [75] | A sensor in the smart seatbelt buckle (SSB) to detect driver drowsiness based on breath duration. | The accuracy of the calculated breath time obtained using the smart seatbelt buckle (SSB) was assessed in comparison to reference respiratory sensors. Subsequently, based on this breath time, an attempt was made to estimate the drowsiness level during driving simulation, achieving a high correlation and indicating the possibility of assessing a drowsiness level of 4 or higher. |
| Respiratory rate. | ||
| Padasdao et al., 2018 [76] | Non-contact detection of chest circumference change. | The sensor uses a modified direct current (dc) motor as an electromagnetic (EM) generator, mounted on the chest, to record changes in chest circumference and tidal volume (TV), while simultaneously generating energy to power the sensor. |
| Respiratory rate, tidal volume. | ||
| Nedoma et al., 2022 [77] | Breath sensor (FOBM, pneumatic respiratory belt) in magnetic resonance (MR). | The article described the testing of fiber-optic Bragg grating embedded in an oxygen breathing mask (FOBM) in a real MR environment using 3 T imaging, as well as the comparison of results with other methods, such as the navigator technique and pneumatic respiratory belt. The FOBM approach provides reliable and accurate results, with an overall image quality score of 3.3 ± 0.4 for FOBM, compared to 3.7 ± 0.5 for the Siemens reference system and 3.8 ± 0.2 for respiratory belts. |
| Breath peaks. | ||
| Härmä et al., 2023 [78] | Deep learning, audio, RIP sensor. | Predicts the next moment of inhalation based on the speaker’s speech using deep learning techniques. |
| Inhalation moment. | ||
| Zhang et al., 2021 [79] | Radio frequency (RF) sensor integrated in furniture, near-field coherent sensing (NCS) technique. | A breath sensor integrated into a bed or chair that detects breathing by modifying the structure of a radio frequency (RF) coaxial cable with a designed notch and utilizes the near-field coherent sensing (NCS) technique. The sensor records respiratory waveforms and determines the breathing rate, and it can also assess the heart rate in the same configuration with appropriate filtering. The sensor design is engineered to tolerate significant positional variation, allowing it to adapt to different user positions. |
| Respiratory waveform, respiratory rate, heart rate. | ||
| Mukhopadhyay et al., 2018 [80] | A wearable IoT-based sensor. A pressure-sensitive textile fabric attached to a belt. | Real-time respiratory signal monitoring. The converted-to-electric-signal chest/stomach movement is transmitted to a central base station, where it is displayed in real time and uploaded to an online repository for future analysis. |
| Respiratory waveform. | ||
| Addeh et al., 2023 [81] | Elastic band around abdomen, fMRI. | There is no guarantee that a given respiratory event evident in the abdominal respiratory belt transducer timeseries, such as a deep breath or pause in breathing, will be detectable in both respiratory volume per time (RVT) and respiratory variation (RV). In addition, RVT and RV do not show similar behavior during some respiratory events, especially when the subject breathes deeply at a low rate, while they use similar respiratory response functions. |
| Respiratory rate, breathing pattern. | ||
| Piuzzi et al., 2019 [82] | A 1-channel bioimpedance and ECG using a one or two pair electrode configuration. | The measurement performance was compared in two-electrode and four-electrode configurations, assessing the sensitivity of heart activity detection and comparing the results with a respiratory belt and an ECG device. |
| Respiration rate and waveform through bioimpedance, ECG. | ||
| Erdogan et al., 2019 [83] | A 24 GHz microwave Doppler sensor. | A network system was developed to gather data from distributed nodes, simultaneously monitoring multiple patients and tracking parameters such as temperature, pressure, and humidity. The system also enables real-time monitoring of cough and apnea and provides warning signals to caregivers in emergency situations. |
| Respiratory rate. | ||
| Altekreeti et al., 2021 [84] | Chest belt with force–pressure sensor. | A neonatal apnea detection system utilizing a sensor embedded in a soft smart e-textile chest belt that is integrated with a smartphone app. |
| Respiratory rate. | ||
| Zhao et al., 2020 [85] | Doppler radar sensor, depth camera. | Non-contact respiration detection using the fusion of a Doppler radar sensor and depth camera. The proposed fusion scheme, using a Bayesian fusion algorithm, can provide more accurate respiratory rate estimation compared to using a single sensor. |
| Respiratory rate. | ||
| Nabavi et al., 2020 [86] | Direct oral cavity pressure sensor. | Tracks respiratory patterns and detects respiratory events regardless of airway, i.e., nasal and oral. Minimal susceptibility to motion artifacts. Direct measurement of oral pressure with 99% accuracy compared to a reference measurement. |
| Respiratory rate, breathing pattern. | ||
| Nallanthighal et al., 2021 [87] | Respiratory belt, microphone. | Analysis of breathing belt data and phoneme-matched audio data. |
| Respiratory waveform, speech signal. | ||
| Kjar et al., 2021 [88] | Plethysmography belt. | Analysis of respiratory and chest movement patterns using plethysmography belt signals to distinguish between obstructive and central sleep apnea. |
| Polysomnography (PSG). | ||
| Li et al., 2023 [89] | Four-dimensional imaging radar using a variational mode separation (VMS) algorithm to separate respiratory and cardiac signals. | The proposed VMS algorithm separates the weaker cardiac motion pattern from the stronger respiratory motion pattern, reducing the influence of respiratory harmonics on the heart signal. |
| Respiratory rate, heart rate. | ||
| Torres et al., 2019 [90] | RIP sensor, mobile app. | The system uses a sensor on a belt, a Raspberry Pi to process the data, and an HTTP server to upload the results to the mobile app. The device has been proven to be effective for people who are uncomfortable using a mouthpiece, and provides a convenient tool for initial lung diagnosis. |
| Respiratory rate, tidal volume. | ||
| Slastnikov et al., 2021 [91] | Review and analysis of methods for detecting the human respiratory wave: MRI with a respiratory belt; the acoustic method; polysomnography using a thermistor and nasal pressure transducer; and implementations of respiratory wave detection based on video signals from RGB, RGB-D, and thermal cameras. | The features of video-based respiratory wave detection in newborns are discussed, and a selected method for the video-based detection of this wave is presented. |
| Respiratory waveform. | ||
| Islam et al., [92] | Microwave Doppler radar. | Microwave Doppler radar was used for respiration monitoring, and the feasibility of separating the respiratory signals from multiple subjects was explored using ICA with the JADE algorithm. The method successfully separated signals from two subjects 1 m apart at a distance of 2.89 m from the radar. |
| Respiratory waveform. | ||
| Valentina et al., 2018 [93] | Respiratory belt, 14-channel electroencephalogram (EEG), 6-channel electrogastrogram (EGG), 1-channel electrooculogram (EOG), 1-channel electrocardiogram. | The study measured brain, eye, cardiac, respiratory, and gastric activity using EEG, EOG, ECG, a respiratory belt, and EGG. Subjects, after fasting, watched film clips with different emotional content, followed by undergoing a water load test. Results showed increased gastric activity in response to emotional stimuli, suggesting central nervous system (CNS) to enteric nervous system (ENS) inhibition, aligning with animal model findings. |
| Breathing pattern, EGG, EEG, EOG, ECG. | ||
| Sacco et al., 2020 [94] | Frequency-Modulated Continuous Wave (FMCW) radar | The 5.8 GHz FMCW radar, specifically designed for measuring respiratory rate and heartbeat, was tested in four orientations of the subject relative to the antenna. Results were compared with photoplethysmograph and respiratory belt measurements, demonstrating high accuracy in all scenarios. |
| Respiratory rate, heart rate | ||
| W. Kang et al., 2024 [95] | FMCW radar (Frequency-Modulated Continuous Wave) with a metasurface antenna and passive metasurface tags. | Monitors the breath of the driver and passengers in a car. The use of metasurface tags improves the signal-to-noise ratio and enables the precise differentiation of the breaths of different individuals in the presence of interference inside the vehicle. |
| Respiratory rate. | ||
| G. Deshpande et al., 2023 [96] | The microphone built into a smartphone. | Extracts breath patterns from speech signals recorded using a smartphone’s microphone. The study showed that different categories of breath can be identified based on speech signals with a classification accuracy of 79%. |
| Breathing pattern through speech. | ||
| Keyword: Respiratory Inductance Plethysmography [ALL] | ||
| Elfaramawy et al., 2019 [97] | The Inertial Measurement Unit (IMU) and microphone. | The wireless system uses wearable sensors with a low-power 9-axis IMU and MEMS microphone to monitor breathing and coughing rates in real time. Data processing algorithms calculate respiratory frequency and coughing events. Tests show high accuracy compared to respiratory inductance plethysmography. |
| Respiratory rate, breathing pattern, cough rate. | ||
| Bricout et al., 2019 [98] | Adaptive Accelerometry Derived Respiration (ADR). | The ADR method uses two 3-axis accelerometers to monitor breathing by analyzing chest and abdominal motions. Compared to measuring airflow through the nose, the method achieves 74% agreement, suggesting a high accuracy in assessing respiratory rate and volume. |
| Respiratory rate, tidal volume. | ||
| Bin Nesar et al., 2022 [99] | LiDAR (Light Detection and Ranging) system, multi-pixel thermal sensor. | The system consists of a rotating LiDAR scanner and a multi-pixel thermal sensor. It is used to determine both respiratory rate and tidal volume, and enables posture assessment and the separate evaluation of nasal and mouth breathing. |
| Respiratory rate, tidal volume. | ||
| Sadr et al., 2019 [100] | Electrocardiogram (ECG), respiratory induction plethysmography (RIP). | ECG and RIP signals were analyzed in different combinations. The QRS area and Principal Component Analysis (P CA) methods were used to estimate ECG-derived respiratory (EDR) signals and Cardiopulmonary Coupling (CPC) spectra. Classification of sleep apnea was performed using Linear Discriminant Analysis (LDA). |
| Respiratory rate, tidal volume. | ||
| Hurtado et al., 2020 [101] | RIP belt, temperature sensor, machine learning, Random Forest regression. | Temperature and breathing signals were used to process temperature-related features to train machine learning models to predict TV (tidal volume) and MV (minute ventilation). The best results were obtained with Random Forest regression, achieving minimal error for TV and MV. |
| Tidal volume, minute ventilation. | ||
| Huysmans et al., 2020 [102] | Tachogram, RIP sensor, convolutional neural network (CNN). | Tachogram data and respiratory inductive plethysmography (RIP) signals were used to classify sleep using a 1D convolutional neural network (CNN) to classify 30 s epochs and to detect and classify sleep apnea. |
| Respiratory rate, heart rate. | ||
| Mannee et al., 2020 [103] | RIP sensor in a smart shirt. | A smart t-shirt with an inductive sensor measures changes in the transverse circumference of the chest and abdomen. It was used to monitor lung hyperinflation (LH). The effects of temperature and girth on the sensor data were tested. The results showed a linear relationship between temperature and RIP signal, and confirmed a linear relationship between girth and sensor signal. |
| Respiratory rate, lung hyperinflation. | ||
| Hill et al., 2021 [104] | LiDAR system and thermal sensor in a breathing mask for non-contact breath monitoring. | The system measures changes in respiratory mask temperature and chest and abdominal movements using a thermal sensor and LiDAR system. The results were compared with data from RIP, capnometry, spirometry, and pulse oximetry. A high correlation was obtained between LiDAR measurements and tidal volume values and capnometer data. |
| Respiratory rate, tidal volume. | ||
| Guo et al., 2019 [105] | Flexible Tactile Sensor Array on a mattress. | A system of tactile sensors on a bed was used to distinguish between chest and abdominal movements by measuring pressure changes on the mattress. Tests were conducted, comparing the results with respiratory induction plethysmography (RIP). The sensor showed a high accuracy in measuring respiratory rate, and also noted differences in the phase of pressure changes depending on gender and lying position. |
| Respiratory rate. | ||
| Song et al., 2023 [106] | A bed-sized tactile sensor sheet. | A bed-sized tactile sensor sheet was used to monitor and identify chest and abdominal position and movements during sleep. Optimal measurement areas were studied based on the distribution of body pressure on the mat. A suitable mathematical model and discriminative feature procedure were proposed, which improved the accuracy of the measurements and the usefulness of the method in the early detection of respiratory diseases. |
| Respiratory rate, respiratory pressure distribution. | ||
| Rathore et al., 2022 [107] | RIP sensor, residual fluctuation analysis (DFA). | The utility of respiratory rate (BR) for determining the ventilatory threshold (VT1) was studied in comparison with classical methods based on gas analysis and heart rate (HR). Residual fluctuation analysis (DFA) and respiratory induction plethysmography (RIP) were used to validate the model. |
| Respiratory rate, ventilatory threshold. | ||
| Nabavi et al., 2023 [108] | A sensor based on surface acoustic waves (SAW) near the nose or mouth. | The SAW sensor for continuous breath monitoring, based on humidity measurements, was characterized by high sensitivity and precision in determining the respiratory rate and breath patterns. Its effectiveness has been confirmed through a comparison with a traditional breath monitoring belt. |
| Respiratory rate, breathing pattern. | ||
| Akamatsu et al., 2023 [109] | Face image analysis based on video recordings. | The CalibrationPhys method was applied, which enabled the measurement of heart rate and respiratory rate through the analysis of facial images in video. This method uses synchronized recordings from multiple cameras and employs contrastive learning to predict pulse and breath waves. |
| Respiratory rate and heart rate through facial video. | ||
| Keyword: Respiratory Inductive Plethysmography [ALL] | ||
| Senyurek et al., 2019 [110] | RIP sensor, AI algorithms. | The inductive sensor monitors changes in chest volume associated with smoking. The study compared the effectiveness of deep learning algorithms, such as convolutional neural networks (CNNs) and Long Short-Term Memory (LSTM), with traditional methods, such as support vector machines (SVMs), Markov models, and decision trees, in detecting smoke inhalation. |
| Tidal volume. | ||
| Schulz et al., 2018 [111] | RIP sensor, 64-channel EEG, 3-channel ECG. | The study monitored heart rate (BBI), respiratory rate, and power EEG (PEEG) from a 64-channel EEG in 21 healthy subjects to analyze interactions occurring in the Central Cardiovascular and Respiratory Network (CCRN). |
| Respiratory rate, heart rate, EEG, ECG. | ||
| Azimi et al., 2018 [112] | Dual RIP sensor. | The method uses the sum of signals from two RIP sensors as an alternative to the airflow signal in detecting apnea and shallow breathing events. |
| Respiratory rate, apnea. | ||
| Mateu-Mateus et al., 2020 [113] | Optical camera with computer algorithms, RIP sensor. | The method uses a camera to track chest movements from a lateral perspective. The algorithm analyzes the consecutive frames of the video in gray tones, which reduces the computational cost and allows for real-time analysis. In addition, a signal quality index is determined. |
| Breathing pattern. | ||
| Belsare et al., 2020 [114] | RIP sensor. | Personal Automatic Cigarette Tracker v2 (PACT-2) is a system that uses an RIP sensor to analyze respiratory signals. It measures parameters such as the duration of inhalation and exhalation, as well as respiratory volume, providing new indicators of the depth and timing of smoke inhalation. |
| Respiratory rate, tidal volume. | ||
| Lyakhova et al., 2018 [115] | Bioimpedance and plethysmography using inductive and piezoelectric sensors. | The wireless device records bioimpedance, inductive plethysmography, and piezoelectric signals, synchronizing the measurements. It analyzes the data in MATLAB, processing the signals and calculating the main relevant parameters. |
| Respiratory rate, respiratory wave. | ||
| Huang et al., 2021 [116] | RIP sensor. | The induction sensor measures chest wall and abdominal movements during the spontaneous breathing test (SBT). The instantaneous phase difference (IPD) method assesses the asynchrony of these movements, supporting extubation. |
| Respiratory rate, spontaneous breathing trial. | ||
| Huang et al., 2018 [117] | RIP using the instantaneous phase difference (IPD) method. | The RIP sensor measures tidal volume, and the instantaneous phase difference (IPD) method assesses the synchronization between chest wall movements (TMV) and abdominal wall movements (AWM) in patients with COPD. |
| Tidal volume. | ||
| Zhu et al., 2019 [118] | Infrared camera and video analysis | The use of an infrared camera and analysis of the recordings tracks the movement of selected feature points on the body of a sleeping patient and extracts the respiratory rate using independent component analysis. |
| Respiratory rate. | ||
| SolĂ-Soler et al., 2023 [119] | Pneumotachograph, RIP belt. | Pneumotachograph and inductive plethysmography belts for breath measurement.Comparison of the breathing pattern characteristics obtained from sensors, pneumotachograph, and inductive plethysmography belts was used to assess breathing variability in healthy volunteers. |
| Breathing pattern. | ||
| Zhang et al., 2024 [120] | Millimeter-wave radar (mmWave Radar), AI, RIP for reference. | The mmTAA system, based on millimeter-wave (mmWave) technology, is used for the non-invasive measurement of TAA (Target Angle and Azimuth) and for detecting and monitoring breath without physical contact. It utilizes an mmWave radar with multiple antennas and an advanced neural network, TAANet, which allows for the accurate determination of the centroid position of RC-AB, enabling precise measurements. |
| Breathing pattern. | ||
| Keyword: Artificial Intelligence AND (respiratory signal OR respiratory rate) [Index Terms, Autor Keywords, IEEE Terms] | ||
| Karvounis et al., 2021 [48] | Prototype wrist sensor. | The wrist sensor monitors real-time vital signs such as heart rate, respiratory rate, oxygen saturation, temperature, and changes in systolic blood pressure. The collected data are sent to a cloud-based environment, where it can be processed using machine learning techniques or Information Mining Algorithms. Automatic alerts are sent to medical personnel, enabling quick intervention. |
| Respiratory rate, temperature, SpO2, PPG, ECG, blood pressure, motion. | ||
| Chen et al., 2021 [49] | Barometric sensor and signal processing algorithm. | A barometric sensor placed on a desk in a person’s environment monitors pressure changes caused by breathing and coughing. A signal processing algorithm is used with a sparsity-based filter. It effectively detects coughing and assesses the respiratory rate, achieving 97.33% accuracy in detecting coughing and 98.98% specificity in assessing breath. |
| Respiratory rate, respiratory waveform, breathing pattern, cough detection. | ||
| Jiang et al., 2022 [50] | ECG, 9-axis MEMS IMU sensor, PPG. | The impact of the COVID-19 virus on overall health was discussed, and existing vital sign monitoring systems and their limitations were analyzed. Potential options for estimating lung function using sensor fusion and artificial intelligence (AI) techniques were also explored. The prototype device demonstrated performance comparable to or better than similar commercial devices. |
| Respiratory rate through ECG, lung volume through IMU sensor, heart rate, cough detection, temperature. | ||
| Ghimire et al., 2020 [121] | An overview of the applications of artificial intelligence, machine learning, and deep learning in solving COVID-19 pandemic problems. | An overview of the use of artificial intelligence, machine learning, and deep learning in the context of the COVID-19 pandemic. Applications included diagnostics, mortality forecasting, vaccine and drug development, sentiment analysis of comments on COVID-19, and disinformation detection. The review included the most successful models in the field. |
| Not specified. | ||
| Fakotakis et al., 2023 [122] | Acoustic sensor, machine learning techniques. | A monitoring system equipped with an acoustic sensor and sound detection was discussed for recognizing drug activation and assessing medication adherence in patients with asthma. The article presented the use of machine learning techniques in the Respiratory and Drug Actuation suite (RDA) for sound processing, feature extraction, and classification. |
| Sound detection for recognizing drug activation. | ||
| Elias et al., 2021 [123] | Acoustic collar, thermoelectric sensor, AI. | A neck device equipped with acoustic and thermoelectric sensors, linked to an artificial intelligence algorithm, was used for the non-invasive assessment of pathophysiological status and the dynamic observation of lesions resulting from COVID-19 infection. The device effectively distinguished between patients with mild symptoms and those with acute symptoms of respiratory failure. |
| Sound detection of vocal system. | ||
| Chawla i Walia, 2022 [52] | AI algorithms to analyze lung images, respiratory sounds, and medical textual data. | Artificial Intelligence based Techniques in Respiratory Healthcare Services: A Review |
| Not specified. | ||
| Husain et al., 2022 [124] | Review of AI technology for COVID-19 disease detection using cough, breath, and speech recordings. | The review included 24 studies and eight applications using artificial intelligence algorithms to detect COVID-19 from audio recordings of coughs, breathing, and speech. AI-based methods could prove effective in screening and diagnosing respiratory diseases, which could save time and play an important role in the fight against COVID-19 and future pandemics. |
| Not specified. | ||
| Yahyaoui i Yumusak, 2021 [125] | AI algorithms for detecting respiratory diseases | Deep And Machine Learning Towards Pneumonia And Asthma Detection |
| Not specified. | ||
| Ward et al., 2021 [126] | Long-wave infrared (LWIR) face detection, deep convolutional network (DNN), cough sounds. | The COVID-19 non-contact symptom detection device uses LWIR face detection to monitor facial temperature and an acoustic sensor and light convolutional network to determine whether a person is coughing. The system was tested on two datasets: one with infrared images of the face and the other with audio recordings of coughing, confirming its effectiveness in detecting symptoms. |
| Not specified. | ||
| Dong i Yao, 2021 [56] | Internet of Things (IoT) technology to monitor physiological parameters, including breathing. | The paper described the application of IoT technology for respiratory monitoring in the context of the COVID-19 pandemic, discussing various methods such as inertial sensors, thermal cameras, optical cameras, microphones, radar, and WiFi. An IoT platform for monitoring COVID-19 was presented, including symptoms, quarantine, contacts, social distance, epidemic forecasting, and virus mutation. |
| Not specified. | ||
| Misra et al., 2023 [57] | KEdge analytical platform (fuzzy interference system). | KEdge is an advanced analytics platform that uses IoT sensor data to assess patient health by analyzing physiological parameters such as respiratory rate, ECG signals, pulse rate (PR), blood oxygen saturation (SpO2), and blood pressure. The system uses a two-stage analytical process and a fuzzy inference system (FIS) to assess the severity of cardiac and respiratory conditions and the health condition index (CI). |
| Respiratory rate, ECG, heart rate, SpO2, blood pressure. | ||
| Campana et al., 2022 [127] | L3-Net deep embedding model for automatic analysis of audible cough and breath samples to identify patients with COVID-19 | L3-Net, based on Transfer Learning, enables COVID-19 detection from smartphone breath and cough recordings. The model, trained on 2 million audio recordings, effectively extracts hidden audio features, which are analyzed by SVM classifiers and logistic regression. It is suitable for deployment on mobile devices. |
| Not specified. | ||
| Abdullah i Bilal Er, 2022 [51] | Hybrid convolutional neural network (CNN)–Long Short-Term Memory (LSTM) model for lung signal classification | The model combines CNN and LSTM structures to extract features and classify lung sounds as normal or abnormal. It uses Cosine Similarity-based Multilevel Discrete Wavelet Transform Decomposition (CS-MDWTD) and the Butterworth filter for noise reduction, and then classifies sounds using CNN-LSTM networks. The model was tested on the Respiratory Sound Database (ICBHI 2017), achieving a classification accuracy of over 90%. |
| Not specified. | ||
| Rani et al., 2021 [53] | Machine learning classifiers: support vector machine (SVM), k-Nearest Neighbors (KNN), Naïve Bayes Classifier, and artificial neural networks (ANN); acoustic features of lung sounds. | Automatic lung sound classification model using artificial intelligence (SVM, KNN, Naïve Bayes, ANN) to diagnose lung diseases. The method identifies various differentiating features of lung sounds, such as the sound of wheezing, which can be useful in the diagnosis of asthma. The model achieved an average accuracy of 95.6%. |
| Lung sounds. | ||
| Grooby et al., 2023 [54] | An artificial intelligence-based model using non-negative matrix factorization (NMF) and non-negative matrix cofactorization (NMCF). | Noisy Neonatal Chest Sound Separation for high-quality heart and lung sound separation of neonatal chest sounds based on artificial intelligence NMF and NMCF methods. |
| Chest sounds. | ||
| Kuang et al., 2023 [55] | Remote photoplethysmography (rPPG) technology, facial video. | rPPG technology is used to measure physiological indicators based on facial video, including HR and respiratory rate (RR). Remote photoplethysmography signal are enhanced based on generative adversarial networks. |
| Respiratory rate, heart rate. | ||
| Romero Gomez i Orjuela-Canon, 2021 [128] | ANN, machine learning techniques, sound signal. | The use of artificial intelligence to analyze respiratory sounds, such as crackles and wheezes, which are associated with respiratory diseases. AI algorithms are used to classify these sounds based on the Respiratory Sound Database from the ICBHI 2017 challenge. |
| Not specified. | ||
| Türkçetin et al., 2023 [129] | ANN, sound signal. | The use of artificial intelligence to analyze sound signals, such as cough, breath, and the sound /a/, for diagnosing respiratory diseases (asthma, COPD, pneumonia). |
| Breath detection, cough detection. | ||
| Pouramirarsalani et al., 2024 [130] | The microphone built into a mobile phone. | The use of a microphone and mobile phone to record acoustic signals related to breathing during sleep, which are then analyzed for sleep apnea diagnosis. The classification model based on artificial intelligence and optimization using the PSO algorithm enabled effective diagnosis, achieving a classification accuracy of 87.5%. |
| Sleep apnea. | ||
| Saeed et al., 2023 [131] | Radar technology and Wi-Fi (radar systems based on SDR). | Utilization of radio technologies, including radar and SDR (software-defined radio), for detecting breath patterns. The radar system tracks subtle chest movements associated with breathing, while SDR systems analyze Wi-Fi signals, enabling the accurate classification of breath patterns using deep learning algorithms, achieving a high classification accuracy |
| Breathing pattern. | ||
5.1. Development of Respiratory Monitoring Technologies for Infants and Children
5.2. From Non-Specific Methods to Dedicated Solutions
5.3. The Need for Advanced Monitoring in a Medical Context
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Natus Medical Incorporated—Natus. Available online: https://natus.com/ (accessed on 3 November 2023).
- Modern Breath Training|Mindfield ® eSense Respiration. Available online: https://mindfield.de/en/esense-respiration/ (accessed on 3 November 2023).
- Respiration Sensor—SA9311M. Available online: https://thoughttechnology.com/respiration-sensor-sa9311m/ (accessed on 3 November 2023).
- RESPeRATE Ultra—2breathe. Available online: https://2breathe.com/product/productresperate-ultra/ (accessed on 3 November 2023).
- 2breathe—Sleep Inducer—2breathe. Available online: https://2breathe.com/product/2breathe-sleep-inducer/ (accessed on 3 November 2023).
- Vollmer, M.; Bläsing, D.; Reiser, J.E.; Nisser, M.; Buder, A. Simultaneous physiological measurements with five devices at different cognitive and physical loads (version 1.0.2). PhysioNet 2023. [Google Scholar] [CrossRef]
- Moody, B.; Hao, S.; Gow, B.; Pollard, T.; Zong, W.; Mark, R. MIMIC-IV Waveform Database (version 0.1.0). PhysioNet 2022. [Google Scholar] [CrossRef]
- Pani, D.; Sulas, E.; Urru, M.; Sameni, R.; Raffo, L.; Tumbarello, R. NInFEA: Non-Invasive Multimodal Foetal ECG-Doppler Dataset for Antenatal Cardiology Research (version 1.0.0). PhysioNet 2020. [Google Scholar] [CrossRef]
- Ihmig, F.R.; Gogeascoechea, A.; Schäfer, S.; Lass-Hennemann, J.; Michael, T. Electrocardiogram, skin conductance and respiration from spider-fearful individuals watching spider video clips (version 1.0.0). PhysioNet 2020. [Google Scholar] [CrossRef]
- Moody, B.; Moody, G.; Villarroel, M.; Clifford, G.; Silva, I. MIMIC-III Waveform Database (version 1.0). PhysioNet 2020. [Google Scholar] [CrossRef]
- Moody, B.; Moody, G.; Villarroel, M.; Clifford, G.; Silva, I. MIMIC-III Waveform Database Matched Subset (version 1.0). PhysioNet 2020. [Google Scholar] [CrossRef]
- Novak, V. Cerebral Vasoregulation in Elderly with Stroke. PhysioNet 2018. [Google Scholar] [CrossRef]
- Pimentel, M.; Johnson, A.E.W.; Charlton, P.; Birrenkott, D.; Watkinson, P.; Tarassenko, L.; Clifton, D. BIDMC PPG and Respiration Dataset. PhysioNet 2018. [Google Scholar] [CrossRef]
- Guy, E.F.S.; Knopp, J.; Lerios, T.; Chase, J.G. Pressure, flow, and dynamic thoraco-abdominal circumferences data for adults breathing under CPAP therapy (version 1.0.0). PhysioNet 2023. [Google Scholar] [CrossRef]
- Novak, V.; Quispe, R.; Saunders, C. Cerebral perfusion and cognitive decline in type 2 diabetes (version 1.0.1). PhysioNet 2022. [Google Scholar] [CrossRef]
- Novak, V.; Quispe, R. Cerebromicrovascular Disease in Elderly with Diabetes (version 1.0.1). PhysioNet 2022. [Google Scholar] [CrossRef]
- Guy, E.; Knopp, J.; Chase, G. CPAP Pressure and Flow Data from a Local Trial of 30 Adults at the University of Canterbury (version 1.0.1). PhysioNet 2022. [Google Scholar] [CrossRef]
- Tamez-Peña, J.; Yala, A.; Cardona, S.; Ortiz-Lopez, R.; Trevino, V. Upper body thermal images and associated clinical data from a pilot cohort study of COVID-19 (version 1.1). PhysioNet 2021. [Google Scholar] [CrossRef]
- Tang, S.; Davarmanesh, P.; Song, Y.; Koutra, D.; Sjoding, M.; Wiens, J. MIMIC-III and eICU-CRD: Feature Representation by FIDDLE Preprocessing (version 1.0.0). PhysioNet 2021. [Google Scholar] [CrossRef]
- Novak, V.; Mendez, L. Cerebral Vasoregulation in Diabetes (version 1.0.0). PhysioNet 2020. [Google Scholar] [CrossRef]
- Fong, N.; Lipnick, M.; Bickler, P.; Feiner, J.; Law, T. OpenOximetry Repository (version 1.0.1). PhysioNet 2024. [Google Scholar] [CrossRef]
- Moukheiber, M.; Moukheiber, L.; Moukheiber, D.; Hao, S.; Celi, L.A.; Lee, H.-C. A Temporal Dataset for Respiratory Support in Critically Ill Patients (version 1.0.0). PhysioNet 2024. [Google Scholar] [CrossRef]
- Guy, E.F.S.; Flett, I.; Clifton, J.A.; Caljé-van der Klei, T.; Chen, R.; Knopp, J.; Moeller, K.; Chase, J.G. Respiratory and heart rate monitoring dataset from aeration study (version 1.0.0). PhysioNet 2024. [Google Scholar] [CrossRef]
- Clifton, J.A.; Guy, E.F.S.; Caljé-van der Klei, T.; Knopp, J.; Chase, J.G. Simulated Obstructive Disease Respiratory Pressure and Flow (version 1.0.0). PhysioNet 2023. [Google Scholar] [CrossRef]
- Guy, E.F.S.; Clifton, J.A.; Caljé-van der Klei, T.; Chen, R.; Knopp, J.; Moeller, K.; Chase, J.G. Respiratory dataset from PEEP study with expiratory occlusion (version 1.0.0). PhysioNet 2023. [Google Scholar] [CrossRef]
- Orlandic, L.; Teijeiro, T.; Atienza, D. The COUGHVID crowdsourcing dataset, a corpus for the study of large-scale cough analysis algorithms. Sci. Data 2021, 8, 156. [Google Scholar] [CrossRef] [PubMed]
- Mueller, R. Sleep Heart Health Study (SHHS). Natl. Sleep Res. Resour. 2014. [Google Scholar] [CrossRef]
- Sleep Data—National Sleep Research Resource—NSRR. Available online: https://sleepdata.org/ (accessed on 3 November 2023).
- Home | COPDGene. Available online: https://www.copdfoundation.org/Research/Research-Projects-and-Consortia/COPDGene.aspx (accessed on 3 November 2023).
- Respiratory Rate Estimation by Peterhcharlton. Available online: https://peterhcharlton.github.io/RRest/index.html (accessed on 15 January 2024).
- Charlton, P.H.; Bonnici, T.; Tarassenko, L.; Clifton, D.A.; Beale, R.; Watkinson, P.J. An assessment of algorithms to estimate respiratory rate from the electrocardiogram and photoplethysmogram. Physiol. Meas. 2016, 37, 610–626. [Google Scholar] [CrossRef] [PubMed]
- Nagy, Á. Cezius/Neonatal-Respiration-Monitoring-Algorithm. GitHub 2023. Available online: https://github.com/cezius/Neonatal-Respiration-Monitoring-Algorithm (accessed on 6 February 2025).
- Nagy, Á.; Földesy, P.; Jánoki, I.; Terbe, D.; Siket, M.; Szabó, M.; Varga, J.; Zarándy, Á. Continuous Camera-Based Premature-Infant Monitoring Algorithms for NICU. Appl. Sci. 2021, 11, 7215. [Google Scholar] [CrossRef]
- Misharin, A. Lvetech/ALT. GitHub 2024. Available online: https://github.com/lvetech/ALT (accessed on 6 February 2025).
- Contactless Sleep Monitoring. Available online: https://lvetechnologies.com/ (accessed on 28 August 2024).
- Mishra, M. Mayank31398/Real-Time-Visual-Respiration-Rate-Estimation-with-Dynamic-Scene-Adaptation. GitHub 2023. Available online: https://github.com/mayank31398/real-time-visual-respiration-rate-estimation-with-dynamic-scene-adaptation (accessed on 6 February 2025).
- Chatterjee, A.; Prathosh, A.P.; Praveena, P.; Upadhya, V. Real-Time Visual Respiration Rate Estimation with Dynamic Scene Adaptation. In Proceedings of the 2016 IEEE 16th International Conference on Bioinformatics and Bioengineering (BIBE), Taichung, Taiwan, 31 October–2 November 2016; pp. 154–160. [Google Scholar]
- Grund, M.; Al, E.; Pabst, M.; Dabbagh, A.; Stephani, T.; Nierhaus, T.; Gaebler, M.; Villringer, A. Respiration, Heartbeat, and Conscious Tactile Perception. J. Neurosci. 2022, 42, 643–656. [Google Scholar] [CrossRef]
- Sun, H.; Ganglberger, W.; Panneerselvam, E.; Leone, M.J.; Quadri, S.A.; Goparaju, B.; Tesh, R.A.; Akeju, O.; Thomas, R.J.; Westover, M.B. Sleep staging from electrocardiography and respiration with deep learning. Sleep 2020, 43, zsz306. [Google Scholar] [CrossRef]
- Pal, S.; Bauer, S.; Kumar, C. isuparnopal/RF_respiration_monitoring. GitHub 2024. Available online: https://github.com/isuparnopal/RF_respiration_monitoring (accessed on 6 February 2025).
- Yang, Y.; Cao, J.; Liu, X.; Liu, X. Multi-Breath: Separate Respiration Monitoring for Multiple Persons with UWB Radar. In Proceedings of the 2019 IEEE 43rd Annual Computer Software and Applications Conference (COMPSAC), Milwaukee, WI, USA, 15–19 July 2019; pp. 840–849. [Google Scholar]
- Kim, M. Mins-n/UWB_Radar_Respiration_Monitoring. GitHub 2024. Available online: https://github.com/mins-n/UWB_Radar_Respiration_Monitoring (accessed on 6 February 2025).
- Manne, S.K.R.; Zhu, S.; Ostadabbas, S.; Wan, M. Automatic Infant Respiration Estimation from Video: A Deep Flow-Based Algorithm and a Novel Public Benchmark. In Perinatal, Preterm and Paediatric Image Analysis; Link-Sourani, D., Abaci Turk, E., Macgowan, C., Hutter, J., Melbourne, A., Licandro, R., Eds.; Lecture Notes in Computer Science; Springer Nature: Cham, Switzerland, 2023; Volume 14246, pp. 111–120. ISBN 978-3-031-45543-8. [Google Scholar]
- Ubicomplab/rPPG-Toolbox. GitHub 2024. Available online: https://github.com/Ubicomplab/rPPG-Toolbox/ (accessed on 6 February 2025).
- Rathore, K.S. Kapil19-dev/RESPIRATION_RATE_ESTIMATION. GitHub 2024. Available online: https://github.com/Kapil19-dev/RESPIRATION_RATE_ESTIMATION (accessed on 6 February 2025).
- Ghibaudo, V.; Granget, J.; Dereli, M.; Buonviso, N.; Garcia, S. A Unifying Method to Study Respiratory Sinus Arrhythmia Dynamics Implemented in a New Toolbox. eNeuro 2023, 10. ENEURO.0197-23.2023. [Google Scholar] [CrossRef]
- Samuel, G. samuelgarcia/physio. GitHub 2024. Available online: https://github.com/samuelgarcia/physio (accessed on 6 February 2025).
- Karvounis, E.; Vavva, M.; Giannakeas, N.; Tzallas, A.T.; Smanis, I.; Tsipouras, M.G. A Hospital Healthcare Monitoring System Using Internet of Things Technologies. In Proceedings of the 2021 6th South-East Europe Design Automation, Computer Engineering, Computer Networks and Social Media Conference (SEEDA-CECNSM), Preveza, Greece, 24–26 September 2021; pp. 1–6. [Google Scholar]
- Chen, X.; Jiang, S.; Li, Z.; Lo, B. A Pervasive Respiratory Monitoring Sensor for COVID-19 Pandemic. IEEE Open J. Eng. Med. Biol. 2021, 2, 11–16. [Google Scholar] [CrossRef]
- Jiang, W.; Majumder, S.; Kumar, S.; Subramaniam, S.; Li, X.; Khedri, R.; Mondal, T.; Abolghasemian, M.; Satia, I.; Deen, M.J. A Wearable Tele-Health System towards Monitoring COVID-19 and Chronic Diseases. IEEE Rev. Biomed. Eng. 2022, 15, 61–84. [Google Scholar] [CrossRef]
- Abdullah, K.H.; Bilal Er, M. Lung sound signal classification by using Cosine Similarity-based Multilevel Discrete Wavelet Transform Decomposition with CNN-LSTM Hybrid model. In Proceedings of the 2022 4th International Conference on Artificial Intelligence and Speech Technology (AIST), Delhi, India, 9–10 December 2022; pp. 1–4. [Google Scholar]
- Chawla, J.; Walia, N.K. Artificial Intelligence based Techniques in Respiratory Healthcare Services: A Review. In Proceedings of the 2022 3rd International Conference on Computing, Analytics and Networks (ICAN), Rajpura, Punjab, India, 18–19 November 2022; pp. 1–4. [Google Scholar]
- Rani, S.; Chaurasia, A.; Dutta, M.K.; Myska, V.; Burget, R. Machine learning approach for automatic lungs sound diagnosis from pulmonary signals. In Proceedings of the 2021 44th International Conference on Telecommunications and Signal Processing (TSP), Brno, Czech Republic, 26–28 July 2021; pp. 366–371. [Google Scholar]
- Grooby, E.; Sitaula, C.; Fattahi, D.; Sameni, R.; Tan, K.; Zhou, L.; King, A.; Ramanathan, A.; Malhotra, A.; Dumont, G.; et al. Noisy Neonatal Chest Sound Separation for High-Quality Heart and Lung Sounds. IEEE J. Biomed. Health Inform. 2023, 27, 2635–2646. [Google Scholar] [CrossRef]
- Kuang, H.; Ao, C.; Ma, X.; Liu, X. Remote photoplethysmography signals enhancement based on generative adversarial networks. In Proceedings of the 2023 IEEE 3rd International Conference on Information Technology, Big Data and Artificial Intelligence (ICIBA), Chongqing, China, 26–28 May 2023; pp. 792–796. [Google Scholar]
- Dong, Y.; Yao, Y.-D. IoT Platform for COVID-19 Prevention and Control: A Survey. IEEE Access 2021, 9, 49929–49941. [Google Scholar] [CrossRef] [PubMed]
- Misra, S.; Pal, S.; Deb, P.K.; Gupta, E. KEdge: Fuzzy-Based Multi-AI Model Coalescence Solution for Mobile Healthcare System. IEEE Syst. J. 2023, 17, 1721–1728. [Google Scholar] [CrossRef]
- Coronel, C.; Wiesmeyr, C.; Garn, H.; Kohn, B.; Wimmer, M.; Mandl, M.; Glos, M.; Penzel, T.; Klosch, G.; Stefanic-Kejik, A.; et al. 3D Camera and Pulse Oximeter for Respiratory Events Detection. IEEE J. Biomed. Health Inform. 2021, 25, 181–188. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Mehta, V.; Bolic, M. A Joint Localization Assisted Respiratory Rate Estimation using IR-UWB Radars. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 489–493. [Google Scholar]
- Kusche, R.; Grashoff, J.; Oltmann, A.; Rostalski, P. A Multichannel EMG System for Spatial Measurement of Diaphragm Activities. IEEE Sens. J. 2022, 22, 23393–23402. [Google Scholar] [CrossRef]
- Vanbuis, J.; Feuilloy, M.; Baffet, G.; Meslier, N.; Gagnadoux, F.; Girault, J.-M. A New Sleep Staging System for Type III Sleep Studies Equipped With a Tracheal Sound Sensor. IEEE Trans. Biomed. Eng. 2022, 69, 1225–1236. [Google Scholar] [CrossRef]
- Alam, M.M.; Hussain, M.; Amin, M.A. A Novel Design of a Respiratory Rate Monitoring System using a Push Switch Circuit and Arduino Micocontroller. In Proceedings of the 2019 International Conference on Robotics, Electrical and Signal Processing Techniques (ICREST), Dhaka, Bangladesh, 10–12 January 2019; pp. 470–473. [Google Scholar]
- Qiu, C.; Yuce, M.R. A Wearable Bioimpedance Chest Patch for IoHT-Connected Respiration Monitoring. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Guadalajara, Jalisco, Mexico, 1–5 November 2021; pp. 6924–6927. [Google Scholar]
- Sharma, P.; Hui, X.; Kan, E.C. A Wearable RF Sensor for Monitoring Respiratory Patterns. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 1217–1223. [Google Scholar]
- Laufer, B.; Krueger-Ziolek, S.; Docherty, P.D.; Hoeflinger, F.; Reindl, L.; Moeller, K. An alternative way to measure respiration induced changes of circumferences: A pilot study. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 4632–4635. [Google Scholar]
- Nedoma, J.; Fajkus, M.; Kepak, S.; Cubik, J.; Zabka, S.; Martinek, R.; Slany, V.; Marecek, J. An Interferometric Sensor for Monitoring Respiratory and Heart Rate of the Human Body. In Proceedings of the 2018 IEEE 20th International Conference on e-Health Networking, Applications and Services (Healthcom), Ostrava, Czech Republic, 17–20 September 2018; pp. 1–5. [Google Scholar]
- Shakhih, M.F.; Nursyazana, R.; Asnida, A.W.; Maheza Irna, M.S. Assessment of Prolonged Expiration Breathing Using Infrared Thermal Imaging Modality: A Case Study. In Proceedings of the 2018 2nd International Conference on BioSignal Analysis, Processing and Systems (ICBAPS), Kuching, Malaysia, 24–26 July 2018; pp. 181–186. [Google Scholar]
- Nassi, T.E.; Ganglberger, W.; Sun, H.; Bucklin, A.A.; Biswal, S.; Van Putten, M.J.A.M.; Thomas, R.J.; Westover, M.B. Automated Scoring of Respiratory Events in Sleep with a Single Effort Belt and Deep Neural Networks. IEEE Trans. Biomed. Eng. 2022, 69, 2094–2104. [Google Scholar] [CrossRef]
- Tataraidze, A.; Olesyuk, R.; Pikhletsky, M. Can We Monitor Breathing During Sleep via Wi-Fi on Smartphone? In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 6710–6713. [Google Scholar]
- Wang, R.; Zhang, Y.; Chen, X.; Lin, F.; He, R.; Lv, R.; Gao, S. Chest and Abdomen Respiratory Monitoring by Large Area Piezoresistive Array. In Proceedings of the 2021 IEEE International Conference on Flexible and Printable Sensors and Systems (FLEPS), Manchester, UK, 20–23 June 2021; pp. 1–4. [Google Scholar]
- Erdyarahman, R.; Suratman, F.Y.; Pramudita, A.A. Contactless Human Respiratory Frequency Monitoring System Based on FMCW Radar. In Proceedings of the 2022 IEEE Asia Pacific Conference on Wireless and Mobile (APWiMob), Bandung, Indonesia, 9–10 December 2022; pp. 1–7. [Google Scholar]
- Cruz, J.C.D.; Mercado, I.L.R.; Algabre, M.K.N. Deriving Heart Rate and Respiratory Rate from Pulse Oximetry Using Neural Networks. In Proceedings of the 2021 IEEE 13th International Conference on Humanoid, Nanotechnology, Information Technology, Communication and Control, Environment, and Management (HNICEM), Manila, Philippines, 28–30 November 2021; pp. 1–6. [Google Scholar]
- Bevilacqua, N.; Andria, G.; Attivissimo, F.; Di Nisio, A.; Spadavecchia, M. Development of an adaptive bandwidth filter for the estimation of respiratory parameters using a piezoelectric belt. In Proceedings of the 2022 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Messina, Italy, 22–24 June 2022; pp. 1–6. [Google Scholar]
- Guede-Fernandez, F.; Fernandez-Chimeno, M.; Ramos-Castro, J.; Garcia-Gonzalez, M.A. Driver Drowsiness Detection Based on Respiratory Signal Analysis. IEEE Access 2019, 7, 81826–81838. [Google Scholar] [CrossRef]
- Sanae, A.; Kawanaka, H.; Oguri, K. Drowsiness Estimation from Respiratory Index Obtained by Using Smart Seat Belt Buckle. In Proceedings of the 2022 IEEE 11th Global Conference on Consumer Electronics (GCCE), Osaka, Japan, 18–21 October 2022; pp. 479–481. [Google Scholar]
- Padasdao, B.; Shahhaidar, E.; Stickley, C.; Boric-Lubecke, O. Electromagnetic Biosensing of Tidal Volume. IEEE Sens. J. 2018, 18, 6391–6398. [Google Scholar] [CrossRef]
- Nedoma, J.; Kostelansky, M.; Vilimek, D.; Ladrova, M.; Martinek, R.; Kahankova, R.; Fajkus, M.; Brablik, J.; Hanzlikova, P.; Mohammed, M.A.; et al. Fiber-Optic Breathing Mask: An Alternative Solution for MRI Respiratory Triggering. IEEE Trans. Instrum. Meas. 2022, 71, 1–13. [Google Scholar] [CrossRef]
- Härmä, A.; Großekathöfer, U.; Ouweltjes, O.; Nallanthighal, V.S. Forecasting of Breathing Events from Speech for Respiratory Support. In Proceedings of the ICASSP 2023—2023 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP), Rhodes Island, Greece, 4–10 June 2023; pp. 1–5. [Google Scholar]
- Zhang, Z.; Sharma, P.; Zhou, J.; Hui, X.; Kan, E.C. Furniture-Integrated Respiration Sensors by Notched Transmission Lines. IEEE Sens. J. 2021, 21, 5303–5311. [Google Scholar] [CrossRef]
- Mukhopadhyay, B.; Sharma, O.; Kar, S. IoT Based Wearable Knitted Fabric Respiratory Monitoring System. In Proceedings of the 2018 IEEE SENSORS, New Delhi, India, 28–31 October 2018; pp. 1–4. [Google Scholar]
- Addeh, A.; Ardila, K.; Vega, F.; Golestani, A.; MacDonald, M.E. Limitations of the Derived Respiratory Variation Measurements Used in Functional Magnetic Resonance Imaging. In Proceedings of the 2023 IEEE 20th International Symposium on Biomedical Imaging (ISBI), Cartagena, Colombia, 18–21 April 2023; pp. 1–5. [Google Scholar]
- Piuzzi, E.; Pisa, S.; Pittella, E.; Podesta, L.; Sangiovanni, S. Low-Cost and Portable Impedance Plethysmography System for the Simultaneous Detection of Respiratory and Heart Activities. IEEE Sens. J. 2019, 19, 2735–2746. [Google Scholar] [CrossRef]
- Erdogan, S.; Yilmaz, S.; Oncu, A. Microwave Noncontact Vital Sign Measurements for Medical Applications. In Proceedings of the 2019 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Istanbul, Turkey, 26–28 June 2019; pp. 1–5. [Google Scholar]
- Altekreeti, A.; Roberts, M.; Convey, D.; Leighton, S.; Setear, M.; Cay, G.; Solanki, D.; Mankodiya, K. NAPNEA: A Cost Effective Neonatal Apnea Detection System. In Proceedings of the 2021 IEEE/ACM Conference on Connected Health: Applications, Systems and Engineering Technologies (CHASE), Washington, DC, USA, 16–18 December 2021; pp. 113–114. [Google Scholar]
- Zhao, H.; Gao, X.; Jiang, X.; Hong, H.; Liu, X. Non-contact Robust Respiration Detection by Using Radar-Depth Camera Sensor Fusion. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 4183–4186. [Google Scholar]
- Nabavi, S.; Bhadra, S. Oral Cavity Pressure Measurement-based Respiratory Monitoring System with Reduced Susceptibility to Motion Artifacts. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 5900–5904. [Google Scholar]
- Nallanthighal, V.S.; Harma, A.; Strik, H.; Doss, M.M. Phoneme Based Respiratory Analysis of Read Speech. In Proceedings of the 2021 29th European Signal Processing Conference (EUSIPCO), Dublin, Ireland, 23–27 August 2021; pp. 191–195. [Google Scholar]
- Kjar, M.R.; Brink-Kjar, A.; Hanif, U.; Mignot, E.; Jennum, P.; Sorensen, H.B.D. Polysomnographic Plethysmography Excursions are Reduced in Obese Elderly Men. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Guadalajara, Jalisco, Mexico, 1–5 November 2021; pp. 2396–2399. [Google Scholar]
- Li, Z.; Jin, T.; Hu, X.; Song, Y.; Zhang, J.; Sang, Z. Remote Respiratory and Cardiac Motion Patterns Separation With 4D Imaging Radars. IEEE J. Biomed. Health Inform. 2023, 27, 2717–2728. [Google Scholar] [CrossRef]
- Torres, J.L.; Yumang, A.; Hortinela, C.; Plameras, J.M.F.; Si, J.E.Z.; Uywan, J.A.O. Respiratory Inductance Plethysmography for Long-Distance Medical Consultation Using Mobile Application for Android Smartphones. In Proceedings of the 2019 IEEE International Conference on Consumer Electronics—Asia (ICCE-Asia), Bangkok, Thailand, 12–14 June 2019; pp. 187–189. [Google Scholar]
- Slastnikov, K.; Koscheeva, E.; Chupov, A.; Konstantinova, A. Review of Instrumental Methods for Detecting the Respiratory Signal. In Proceedings of the 2021 IEEE Ural-Siberian Conference on Computational Technologies in Cognitive Science, Genomics and Biomedicine (CSGB), Novosibirsk-Yekaterinburg, Russia, 26–28 May 2021; pp. 110–113. [Google Scholar]
- Islam, S.M.M.; Yavari, E.; Rahman, A.; Lubecke, V.M.; Boric-Lubecke, O. Separation of Respiratory Signatures for Multiple Subjects Using Independent Component Analysis with the JADE Algorithm. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 1234–1237. [Google Scholar]
- Valentina, Z.; Mario, V.; Juliane, C.; Vincent, N.; Sami, A.; Morwena, L. The Gastric Myoelectrical Activity Response to Emotional Stimuli. In Proceedings of the 2018 IX International Seminar of Biomedical Engineering (SIB), Bogota, Colombia, 16–18 May 2018; pp. 1–5. [Google Scholar]
- Sacco, G.; Piuzzi, E.; Pittella, E.; Pisa, S. Vital Signs Monitoring for Different Chest Orientations Using an FMCW Radar. In Proceedings of the 2020 XXXIIIrd General Assembly and Scientific Symposium of the International Union of Radio Science, Rome, Italy, 29 August–5 September 2020; pp. 1–4. [Google Scholar]
- Kang, W.; Zhou, C.; Wu, W. Respiration Monitoring of All Occupants in a Vehicle Using Time-Division Multiplexing FMCW Radar Based on Metasurface Technology. IEEE Trans. Microw. Theory Technol. 2024, 72, 4960–4974. [Google Scholar] [CrossRef]
- Deshpande, G.; Schuller, B.W.; Deshpande, P.; Joshi, A.R. Automatic Breathing Pattern Analysis from Reading-Speech Signals. In Proceedings of the 2023 45th Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Sydney, Australia, 24–27 July 2023; pp. 1–4. [Google Scholar]
- Elfaramawy, T.; Fall, C.L.; Arab, S.; Morissette, M.; Lellouche, F.; Gosselin, B. A Wireless Respiratory Monitoring System Using a Wearable Patch Sensor Network. IEEE Sens. J. 2019, 19, 650–657. [Google Scholar] [CrossRef]
- Bricout, A.; Fontecave-Jallon, J.; Colas, D.; Gerard, G.; Pepin, J.-L.; Gumery, P.-Y. Adaptive Accelerometry Derived Respiration: Comparison with Respiratory Inductance Plethysmography during Sleep. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 6714–6717. [Google Scholar]
- Bin Nesar, M.S.; Trippe, K.; Stapley, R.; Whitaker, B.M.; Hill, B. Improving Touchless Respiratory Monitoring via LiDAR Orientation and Thermal Imaging. In Proceedings of the 2022 IEEE Aerospace Conference (AERO), Big Sky, MT, USA, 5–12 March 2022; pp. 1–8. [Google Scholar]
- Sadr, N. Non-invasive Diagnosis of Sleep Apnoea Using ECG and Respiratory Bands. Available online: https://pubmed.ncbi.nlm.nih.gov/31946204/ (accessed on 6 February 2025).
- Hurtado, D.E.; Chavez, J.A.P.; Mansilla, R.; Lopez, R.; Abusleme, A. Respiratory Volume Monitoring: A Machine-Learning Approach to the Non-Invasive Prediction of Tidal Volume and Minute Ventilation. IEEE Access 2020, 8, 227936–227944. [Google Scholar] [CrossRef]
- Huysmans, D.; Castro, I.; Heffinck, E.; Deviaene, M.; Borzée, P.; Buyse, B.; Testelmans, D.; Van Huffel, S.; Varon, C. Sleep-Wake Classification for Home Monitoring of Sleep Apnea Patients. Comput. Cardiol. 2020, 2020, 9344196. [Google Scholar]
- Mannee, D.; Van Helvoort, H.; De Jongh, F. The Feasibility of Measuring Lung Hyperinflation with a Smart Shirt: An in Vitro Study. IEEE Sens. J. 2020, 20, 15154–15162. [Google Scholar] [CrossRef]
- Hill, B.; Stapley, R.; Bin Nesar, M.S.; Whitaker, B.M. Touchless Respiratory Monitor Preliminary Data and Results. In Proceedings of the 2021 IEEE Aerospace Conference (50100), Big Sky, MT, USA, 6–13 March 2021; pp. 1–7. [Google Scholar]
- Guo, S.; Zhao, X.; Matsuo, K.; Liu, J.; Mukai, T. Unconstrained Detection of the Respiratory Motions of Chest and Abdomen in Different Lying Positions Using a Flexible Tactile Sensor Array. IEEE Sens. J. 2019, 19, 10067–10076. [Google Scholar] [CrossRef]
- Song, Y.; Guo, S.; Xiao, S.; Zhao, X. Unconstrained Identification of the Positions of Chest and Abdomen and Detection of Respiratory Motions in Sleep by Using a Bed-Size Tactile Sensor Sheet. IEEE Sens. J. 2023, 23, 16276–16286. [Google Scholar] [CrossRef]
- Rathore, K.S.; Sricharan, V.; Preejith, S.; Sivaprakasam, M. MRNet—A Deep Learning Based Multitasking Model for Respiration Rate Estimation in Practical Settings. In Proceedings of the 2022 IEEE 10th International Conference on Serious Games and Applications for Health (SeGAH), Sydney, Australia, 10–12 August 2022; pp. 1–6. [Google Scholar]
- Nabavi, S.K.; Moghadam, A.K.; Salahi, S. A Highly Sensitive Surface Acoustic Wave Sensor for Continuous Respiratory Monitoring. In Proceedings of the 2023 IEEE SENSORS, Vienna, Austria, 29 October–1 November 2023; pp. 1–4. [Google Scholar]
- Akamatsu, Y.; Umematsu, T.; Imaoka, H. CalibrationPhys: Self-supervised Video-based Heart and Respiratory Rate Measurements by Calibrating Between Multiple Cameras. arXiv 2023, arXiv:2310.15043. [Google Scholar] [CrossRef]
- Senyurek, V.Y.; Imtiaz, M.H.; Belsare, P.; Tiffany, S.; Sazonov, E. A Comparison of SVM and CNN-LSTM Based Approach for Detecting Smoke Inhalations from Respiratory signal. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 3262–3265. [Google Scholar]
- Schulz, S.; Serra Juhé, A.; Giraldo, B.; Haueisen, J.; Baer, K.-J.; Voss, A. Analysis of Linear and Nonlinear Central-Cardiorespiratory Coupling Pathways in Healthy Subjects. In Proceedings of the 2018 Computing in Cardiology Conference, Maastricht, The Netherlands, 23–26 September 2018. [Google Scholar]
- Azimi, H.; Gilakjani, S.S.; Bouchard, M.; Goubran, R.A.; Knoefel, F. Automatic apnea-hypopnea events detection using an alternative sensor. In Proceedings of the 2018 IEEE Sensors Applications Symposium (SAS), Seoul, Republic of Korea, 12–14 March 2018; pp. 1–5. [Google Scholar]
- Mateu-Mateus, M.; Guede-Fernandez, F.; Garcia-Gonzalez, M.A.; Ramos-Castro, J.J.; Fernandez-Chimeno, M. Camera-Based Method for Respiratory Rhythm Extraction from a Lateral Perspective. IEEE Access 2020, 8, 154924–154939. [Google Scholar] [CrossRef]
- Belsare, P.; Senyurek, V.Y.; Imtiaz, M.H.; Tiffany, S.; Sazonov, E. Computation of Cigarette Smoke Exposure Metrics from Breathing. IEEE Trans. Biomed. Eng. 2020, 67, 2309–2316. [Google Scholar] [CrossRef] [PubMed]
- Lyakhova, E.K.; Shlyakhotka, A.V.; Sutyagina, A.D. Design of a wearable module for respiratory rate registration rased on multiply network. In Proceedings of the 2018 IEEE Conference of Russian Young Researchers in Electrical and Electronic Engineering (EIConRus), Moscow, Russia, 29 January–1 February 2018; pp. 1212–1215. [Google Scholar]
- Huang, P.-H.; Chung, W.-C.; Sheu, C.-C.; Tsai, J.-R.; Hsiao, T.-C. Is the asynchronous phase of thoracoabdominal movement a novel feature of successful extubation? A preliminary result. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Guadalajara, Jalisco, Mexico, 1–5 November 2021; pp. 752–756. [Google Scholar]
- Huang, P.-H.; Luo, Y.-F.; Yeh, C.-F.; Hsiao, T.-C. Towards instantaneous phase difference on the COPD pre-discrimination. In Proceedings of the 2018 IEEE 23rd International Conference on Digital Signal Processing (DSP), Shanghai, China, 19–21 November 2018; pp. 1–5. [Google Scholar]
- Zhu, K.; Li, M.; Akbarian, S.; Hafezi, M.; Yadollahi, A.; Taati, B. Vision-Based Heart and Respiratory Rate Monitoring During Sleep—A Validation Study for the Population at Risk of Sleep Apnea. IEEE J. Transl. Eng. Health Med. 2019, 7, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Solà-Soler, J.; Pérez, D.R.; Balchin, L.; Serra, A.M.; Torné, M.L.; Koborzan, M.R.P.; Giraldo, B.F.G. Respiratory Pattern Analysis for Different Breathing Types and Recording Sensors in Healthy Subjects. In Proceedings of the 2023 45th Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Sydney, Australia, 24–27 July 2023; pp. 1–4. [Google Scholar]
- Zhang, F.; Zhang, Z.; Kang, L.; Zhou, A. mmTAA: A Contact-Less Thoracoabdominal Asynchrony Measurement System Based on Mmwave Sensing. IEEE Trans. Mobile Comput. 2024, 24, 627–641. [Google Scholar] [CrossRef]
- Ghimire, A.; Thapa, S.; Jha, A.K.; Kumar, A.; Kumar, A.; Adhikari, S. AI and IoT Solutions for Tackling COVID-19 Pandemic. In Proceedings of the 2020 4th International Conference on Electronics, Communication and Aerospace Technology (ICECA), Coimbatore, India, 5–7 November 2020; pp. 1083–1092. [Google Scholar]
- Nikos Fakotakis, D.; Nousias, S.; Arvanitis, G.; Zacharaki, E.I.; Moustakas, K. AI Sound Recognition on Asthma Medication Adherence: Evaluation With the RDA Benchmark Suite. IEEE Access 2023, 11, 13810–13829. [Google Scholar] [CrossRef]
- Elias, V.; Rabih, A.; Bin, S.; Aziz, H.; Nassar, G. An autonomous acoustic collar to quantify the severity of covid-19 effects by analyzing the vibratory components of vocal and respiratory systems. In Proceedings of the 2021 IEEE International Conference on Design & Test of Integrated Micro & Nano-Systems (DTS), Sfax, Tunisia, 7–10 June 2021; pp. 1–7. [Google Scholar]
- Husain, M.; Simpkin, A.; Gibbons, C.; Talkar, T.; Low, D.; Bonato, P.; Ghosh, S.S.; Quatieri, T.; O’Keeffe, D.T. Artificial Intelligence for Detecting COVID-19 With the Aid of Human Cough, Breathing and Speech Signals: Scoping Review. IEEE Open J. Eng. Med. Biol. 2022, 3, 235–241. [Google Scholar] [CrossRef]
- Yahyaoui, A.; Yumusak, N. Deep and Machine Learning Towards Pneumonia And Asthma Detection. In Proceedings of the 2021 International Conference on Innovation and Intelligence for Informatics, Computing, and Technologies (3ICT), Zallaq, Bahrain, 29–30 September 2021; pp. 494–497. [Google Scholar]
- Ward, R.J.; Mark Jjunju, F.P.; Kabenge, I.; Wanyenze, R.; Griffith, E.J.; Banadda, N.; Taylor, S.; Marshall, A. FluNet: An AI-Enabled Influenza-Like Warning System. IEEE Sens. J. 2021, 21, 24740–24748. [Google Scholar] [CrossRef]
- Campana, M.G.; Rovati, A.; Delmastro, F.; Pagani, E. L3-Net Deep Audio Embeddings to Improve COVID-19 Detection from Smartphone Data. In Proceedings of the 2022 IEEE International Conference on Smart Computing (SMARTCOMP), Helsinki, Finland, 20–24 June 2022; pp. 100–107. [Google Scholar]
- Romero Gomez, A.F.; Orjuela-Canon, A.D. Respiratory Sounds Classification employing a Multi-label Approach. In Proceedings of the 2021 IEEE Colombian Conference on Applications of Computational Intelligence (ColCACI), Cali, Colombia, 26–28 May 2021; pp. 1–5. [Google Scholar]
- Türkçetin, A.Ö.; Koç, T.; Çilekar, Ş. The Use of ANN in the Sound Detection of Lung Diseases: Example of COPD, Asthma, Pneumonia. In Proceedings of the 2023 31st Signal Processing and Communications Applications Conference (SIU), IEEE, Istanbul, Turkiye, 5–8 July 2023; pp. 1–4. [Google Scholar]
- Pouramirarsalani, S.; Maleki, S.E.; Rajebi, S.; Manaf, N.V.; Roohany, A. Diagnosis of sleep apnea by optimal fuzzy system based on respiratory signals. In Proceedings of the 2024 10th International Conference on Artificial Intelligence and Robotics (QICAR), Qazvin, Iran, 29 February 2024; pp. 100–105. [Google Scholar]
- Saeed, U.; Zheng, D.; Shah, B.A.; Shah, S.I.; Jan, S.U.; Ahmad, J.; Abbasi, Q.H.; Shah, S.A.; Boulila, W. Contactless Breathing Waveform Detection Through RF Sensing: Radar vs. Wi-Fi Techniques. In Proceedings of the 2023 IEEE Tenth International Conference on Communications and Networking (ComNet), Hammamet, Tunisia, 1–3 November 2023; pp. 1–10. [Google Scholar]
- AL-Khalidi, F.Q.; Saatchi, R.; Burke, D.; Elphick, H.; Tan, S. Respiration rate monitoring methods: A review. Pediatr. Pulmonol. 2011, 46, 523–529. [Google Scholar] [CrossRef]
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep learning. Nature 2015, 521, 436–444. [Google Scholar] [CrossRef]
- Kalaiyarasan, K.; Sridhar, R. Artificial Intelligence in Respiratory Medicine: The Journey So Far—A review. J. Assoc. Pulmonol. Tamil Nadu 2023, 6, 53–68. [Google Scholar] [CrossRef]
- Artificial Intelligence in Pulmonary Medicine: Computer Vision, Predictive Model and COVID-19. Available online: https://err.ersjournals.com/lens/errev/29/157/200181 (accessed on 6 September 2024).
- De Georgia, M.A.; Deogaonkar, A. Multimodal Monitoring in the Neurological Intensive Care Unit. Neurologist 2005, 11, 45–54. [Google Scholar] [CrossRef]
- Alvarez-Estevez, D.; Rijsman, R.M. Computer-assisted analysis of polysomnographic recordings improves inter-scorer associated agreement and scoring times. PLoS ONE 2022, 17, e0275530. [Google Scholar] [CrossRef] [PubMed]
- Shen, S.; Zhou, Q.; Chen, G.; Fang, Y.; Kurilova, O.; Liu, Z.; Li, S.; Chen, J. Advances in wearable respiration sensors. Mater. Today 2024, 72, 140–162. [Google Scholar] [CrossRef]
- Njeru, C.M.; Ansermino, J.M.; Macharia, W.M.; Dunsmuir, D.T. Variability of respiratory rate measurements in neonates- every minute counts. BMC Pediatr. 2022, 22, 16. [Google Scholar] [CrossRef]
- Arzi, A.; Sela, L.; Green, A.; Givaty, G.; Dagan, Y.; Sobel, N. The Influence of Odorants on Respiratory Patterns in Sleep. Chem. Sens. 2010, 35, 31–40. [Google Scholar] [CrossRef]
- Kinney, H.C.; Thach, B.T. The Sudden Infant Death Syndrome. N. Engl. J. Med. 2009, 361, 795–805. [Google Scholar] [CrossRef]
- Fraile-Martinez, O.; García-Montero, C.; Díez, S.C.; Bravo, C.; De Guadalupe Quintana-Coronado, M.; Lopez-Gonzalez, L.; Barrena-Blázquez, S.; García-Honduvilla, N.; De León-Luis, J.A.; Rodriguez-Martín, S.; et al. Sudden Infant Death Syndrome (SIDS): State of the Art and Future Directions. Int. J. Med. Sci. 2024, 21, 848–861. [Google Scholar] [CrossRef]
- Papadopoulos, N.G.; Custovic, A.; Deschildre, A.; Gern, J.E.; Nieto Garcia, A.; Miligkos, M.; Phipatanakul, W.; Wong, G.; Xepapadaki, P.; Agache, I.; et al. Recommendations for asthma monitoring in children: A PeARL document endorsed by APAPARI, EAACI, INTERASMA, REG, and WAO. Pediatr. Allergy Immunol. 2024, 35, e14129. [Google Scholar] [CrossRef]
- Cloutier, M.M.; Teach, S.J.; Lemanske, R.F.; Blake, K.V. The 2020 Focused Updates to the NIH Asthma Management Guidelines: Key Points for Pediatricians. Pediatrics 2021, 147, e2021050286. [Google Scholar] [CrossRef]
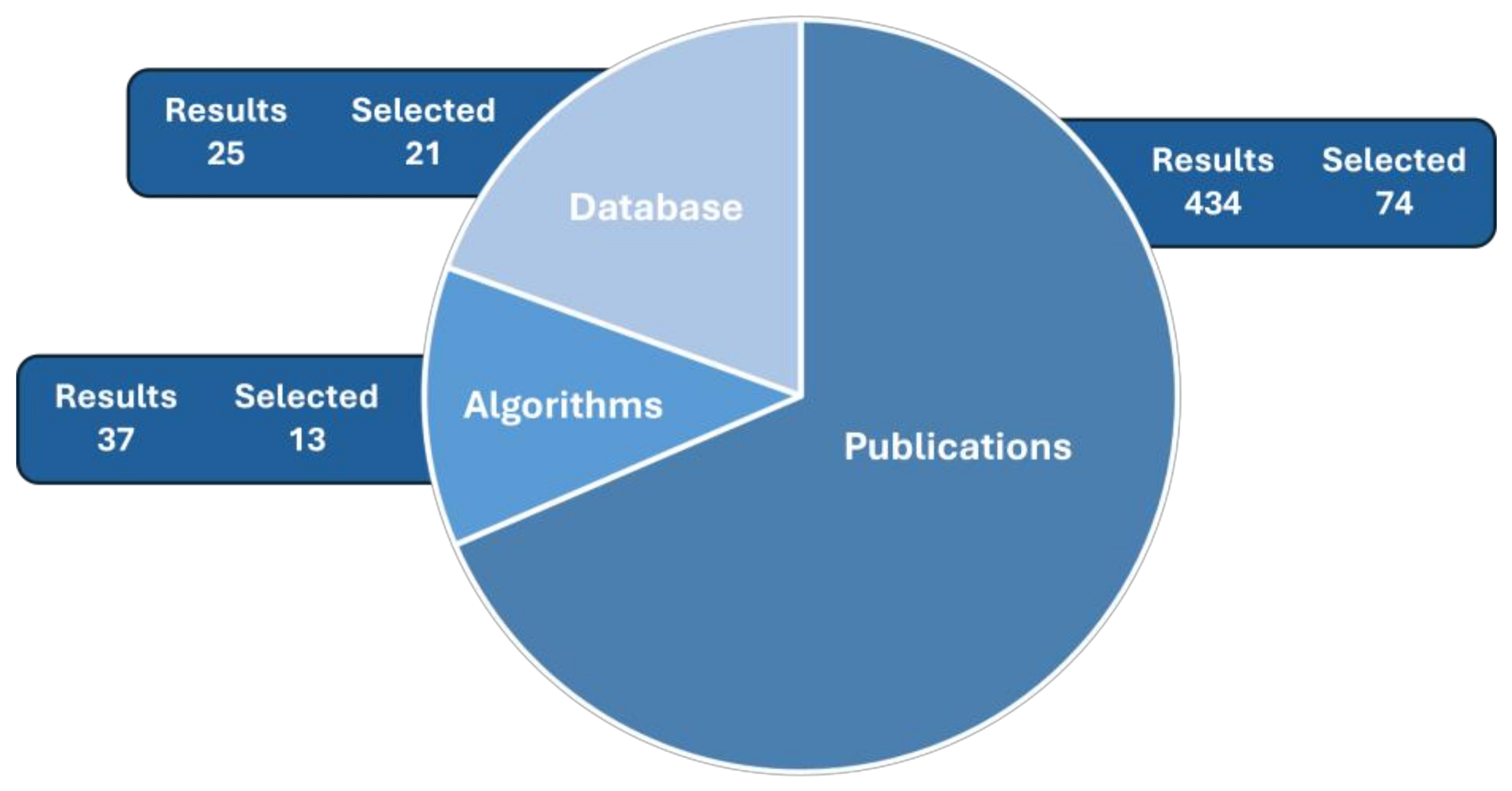
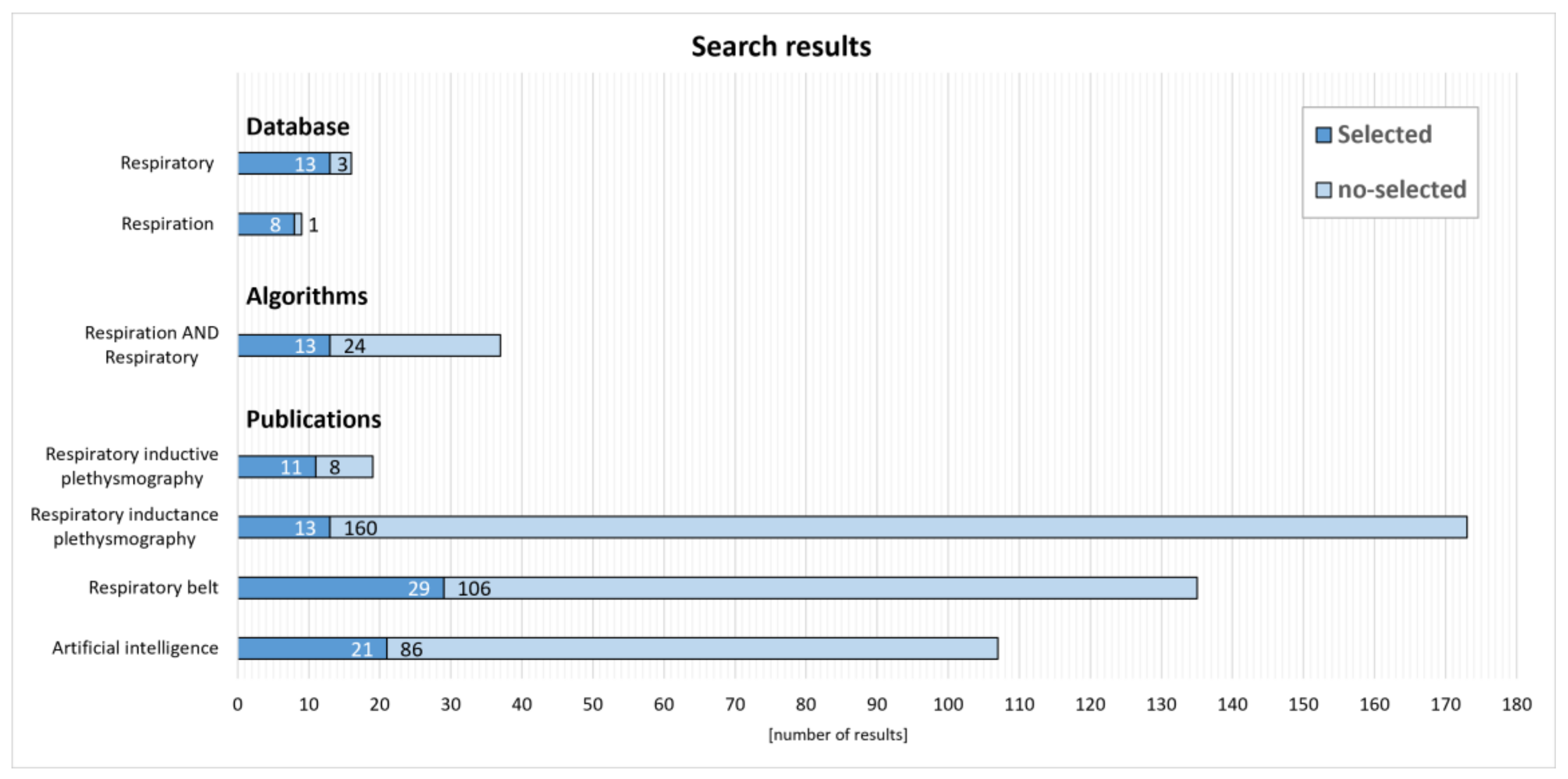
| Name | Description | Programming Language/Environment | Author |
|---|---|---|---|
| Rrest [30,31] | The algorithm estimates the respiratory rate from ECG or PPG. It analyzes frequency (Fourier) and checks the time between successive ECG heartbeats or PPG beat episodes. It then modulates the signal in three ways—changing the baseline, amplitude, or frequency. | Matlab | Peter Charlson |
| Neonatal-Respiration-Monitoring-Algorithm [32,33] | The algorithm estimates the respiratory rate based on a video (individual, consecutive frames). A convolutional neural network searches for abdominal movements in the area of interest (ROI) and estimates the respiratory rate (RPM) based on them. The algorithm is designed for videos of infants lying in care units (works with good focus and lighting). It works only on hdf5 files. | Python | Adam Nagy |
| ALT [34,35] | Embedded on a Raspberry Pi, the system includes a camera and a light source (sub-black) with a depth-of-field detector. The collected image frames are processed by the AI—ALT “superimposes” a texture (dots) on the person, mapping the positions of the various body parts, then checks the differences in the positions of the superimposed dots for each successive frame. In this way, it checks, for example, chest movements both through breaths and small areas with a visible heartbeat. It is mainly used to monitor vital signs during sleep. | Python | Alexander Misharin |
| Real-time visual respiration rate estimation with dynamic scene adaptation [36,37] | The algorithm focuses on the real-time estimation of respiration rate based on video analysis. It uses image processing and machine learning techniques to track chest and abdominal movements, even in changing scene conditions, such as variations in lighting or a person’s position. The algorithm is designed to work in different environments, making it useful for remote health monitoring. | Python/Matlab | Mayank Mishra |
| respirationCA [38] | The algorithm analyzes how phases of the respiratory cycle and moments in the cardiac cycle affect tactile perception. It synchronizes (phase-locking) respiratory signals with expected stimuli to identify moments of peak heart rate and associated higher alertness. The analysis reveals that tactile detection is lowest when the pulse wave reaches the finger and highest during diastole. This suggests that these changes are not merely physiological artifacts but result from cognitive processes that model the body’s internal state and may adjust respiration to fit the task at hand. | Matlab/R | Martin Grund |
| ecg_respiration_sleep_staging [39] | Deep neural networks are developed to classify sleep stages using the ECG and respiratory signals from 8682 polysomnographs. Five types of networks are trained to analyze ECG R-peaks and respiratory effort. | Python + PTH models | Harvard Medical School |
| RF_respiration_monitoring [40] | The algorithm uses radio frequency signals to monitor respiration. It processes reflected RF waves to detect breathing movements and extract respiratory patterns. The system is designed for real-time monitoring, offering continuous updates on the breathing rate and patterns. | Matlab + simulink | isuparnopal |
| UWB_Radar_Respiration_Monitoring [41,42] | The algorithm uses ultra-wideband (UWB) radar to monitor respiration rates. It processes radar signals to detect and analyze chest movements caused by breathing. The algorithm extracts respiratory patterns from the radar data and calculates the respiratory rate. This non-invasive method enables the real-time monitoring of respiration without physical contact. | Python, Matlab | Minsun Kim |
| Infant-Respiration-Estimation [43] | The algorithm estimates infant respiration rates from video data. It uses computer vision techniques to analyze subtle chest movements associated with breathing. The algorithm processes these movements to accurately determine the respiratory rate in real time. This non-invasive method is designed to monitor infant breathing without the need for physical sensors. | Python | Sarah Ostadabbas (Northeastern University) |
| rPPG_Toolbox [44] | The algorithm estimates respiration and heart rates using remote photoplethysmography (rPPG). It processes video data to extract and analyze subtle changes in skin color caused by blood flow variations. The toolbox provides tools for detecting and tracking these physiological signals in real time. This non-invasive method offers an alternative to traditional monitoring techniques by leveraging standard video footage. | Python | Ubiquitous Computing Lab (University of Washington) |
| RESPIRATION_RATE_ESTIMATION [45] | The algorithm estimates respiration rates from video footage. It uses computer vision techniques to analyze the motion of the chest and abdomen, extracting features related to breathing. The algorithm processes these features to calculate the respiratory rate in real time. This approach offers a non-invasive method for monitoring respiration by leveraging visual data. | Python | Kapil Singh Rahtore (Indian Institute Of Tecnhology Madras) |
| Physio [46,47] | The repository is designed for processing and analyzing physiological signals, such as ECG and EEG. It provides tools for handling, preprocessing, and extracting features from these signals. The repository also includes visualization capabilities to aid in interpreting the data. It is intended to streamline the analysis of physiological data, potentially integrating with existing databases like PhysioNet. | Python | Samuel Garcia |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karpiel, I.; Mysiński, M.; Olesz, K.; Czerw, M. Overview of Respiratory Sensor Solutions to Support Patient Diagnosis and Monitoring. Sensors 2025, 25, 1078. https://doi.org/10.3390/s25041078
Karpiel I, Mysiński M, Olesz K, Czerw M. Overview of Respiratory Sensor Solutions to Support Patient Diagnosis and Monitoring. Sensors. 2025; 25(4):1078. https://doi.org/10.3390/s25041078
Chicago/Turabian StyleKarpiel, Ilona, Maciej Mysiński, Kamil Olesz, and Marek Czerw. 2025. "Overview of Respiratory Sensor Solutions to Support Patient Diagnosis and Monitoring" Sensors 25, no. 4: 1078. https://doi.org/10.3390/s25041078
APA StyleKarpiel, I., Mysiński, M., Olesz, K., & Czerw, M. (2025). Overview of Respiratory Sensor Solutions to Support Patient Diagnosis and Monitoring. Sensors, 25(4), 1078. https://doi.org/10.3390/s25041078






