Thermoregulation and Heat Stroke Prevention in Older Adults: Advances in Emerging Technologies and Interventions
Abstract
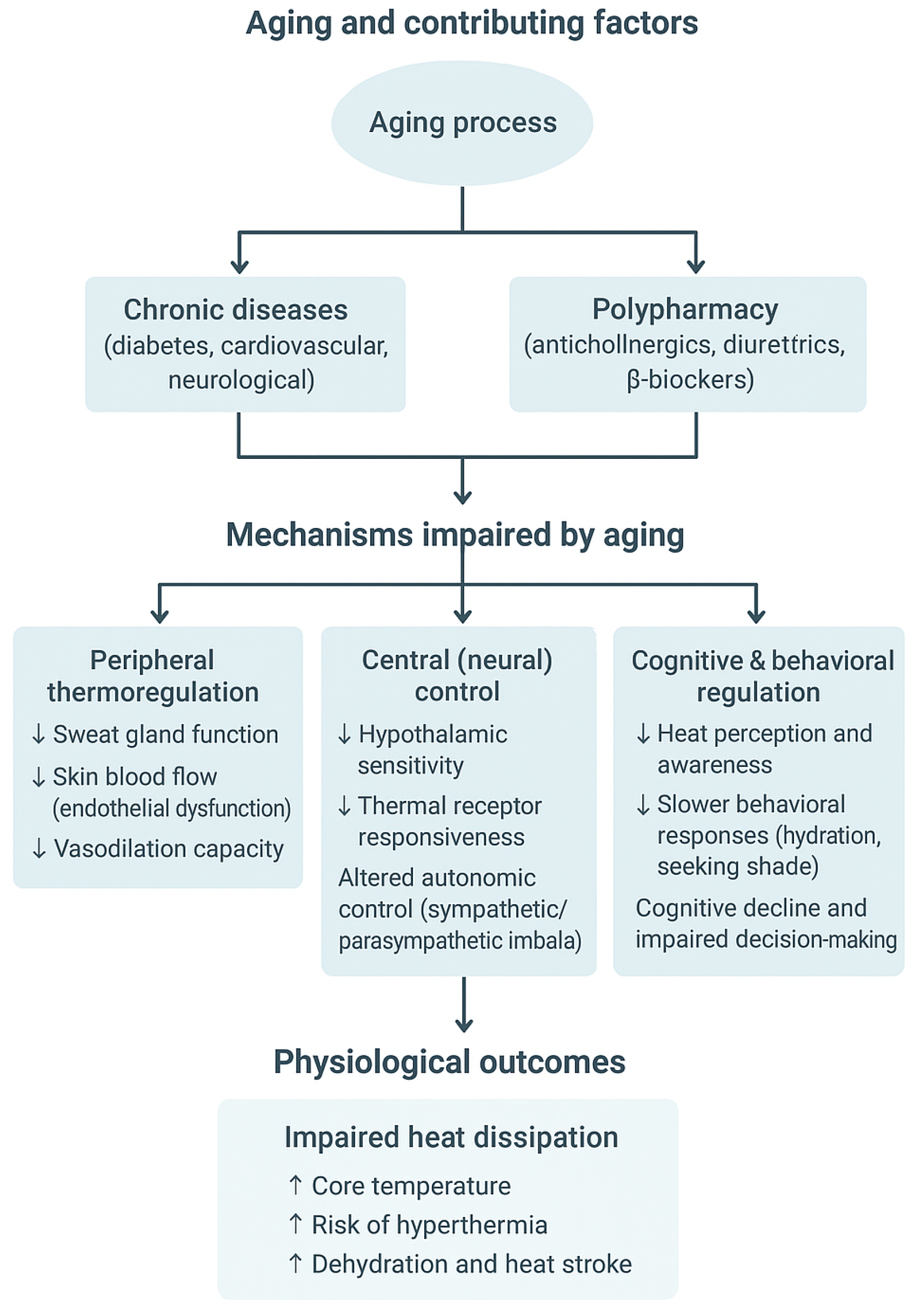
1. Introduction
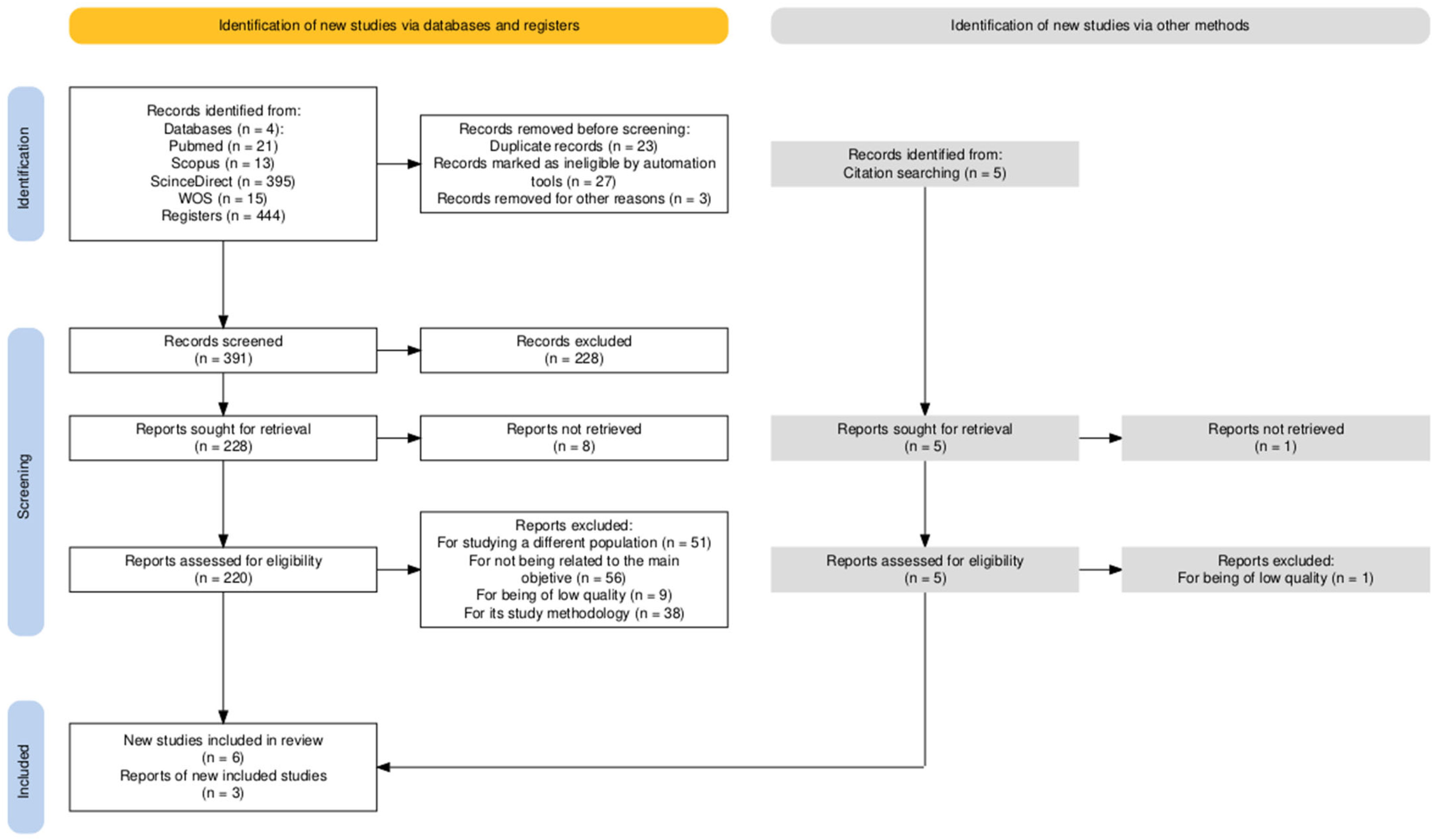
2. Materials and Methods
3. Results
3.1. Study Characteristics
3.2. Description of the Characteristics of the Studies
4. Discussion
- (a)
- Monitoring level: Includes wearable temperature sensors, sweat patches, infrared thermography, and environmental IoT nodes that continuously capture physiological and ambient parameters. These tools primarily enable real-time monitoring and early detection of deviations in thermal homeostasis. However, their application remains mostly limited to laboratory or controlled environments, with scarce validation in everyday contexts.
- (b)
- Prediction level: This group encompasses machine learning models that estimate thermal sensation, core temperature, or heat strain based on physiological and environmental inputs. Examples include regression and neural network approaches (Ridge, LSTM, GRU) that outperform traditional biophysical models. These tools form the analytical bridge between raw data and individualized thermal risk prediction.
- (c)
- Intervention level: Encompasses active cooling or heating systems, such as thermoelectric devices, ventilated clothing, and microclimatic chairs, as well as behavioral and educational strategies to enhance heat stress awareness. These technologies translate monitoring and predictive insights into actionable interventions, aiming to maintain comfort and prevent hyperthermia or hypothermia.
- (d)
- Ecological application level: Refers to the integration of the above technologies into real-world preventive frameworks, combining wearable data, environmental monitoring, and adaptive algorithms to guide decision-making by older adults, caregivers, or healthcare systems. Currently, no study has validated such integrated systems in community or institutional settings.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bach, A.J.E.; Cunningham, S.J.K.; Morris, N.R.; Xu, Z.; Rutherford, S.; Binnewies, S.; Meade, R.D. Experimental research in environmentally induced hyperthermic older persons: A systematic quantitative literature review mapping the available evidence. Temperature 2024, 11, 4–26. [Google Scholar] [CrossRef] [PubMed]
- Van Someren, E. Circadian and age-related modulation of thermoreception and temperature regulation: Mechanisms and functional implications. Ageing Res. Rev. 2002, 1, 721–778. [Google Scholar] [CrossRef] [PubMed]
- Balmagiya, T.; Rozovski, S.J. Age-related changes in thermoregulation in male albino rats. Exp. Gerontol. 1983, 18, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, R.; Yuan, L.; Yang, X.; Lv, J.; Ye, Z.; Huang, F.; He, T. Association between diabetes complicated with comorbidities and frailty in older adults: A cross-sectional study. J. Clin. Nurs. 2023, 32, 894–900. [Google Scholar] [CrossRef]
- McKenna, Z.J.; Foster, J.; Atkins, W.C.; Belval, L.N.; Watso, J.C.; Jarrard, C.P.; Orth, B.D.; Crandall, C.G. Age alters the thermoregulatory responses to extreme heat exposure with accompanying activities of daily living. J. Appl. Physiol. 2023, 135, 445–455. [Google Scholar] [CrossRef]
- Tamura, T.; Huang, M.; Yoshimura, T.; Umezu, S.; Ogata, T. An Advanced Internet of Things System for Heatstroke Prevention with a Noninvasive Dual-Heat-Flux Thermometer. Sensors 2022, 22, 9985. [Google Scholar] [CrossRef]
- Martin, L.S.; Josset-Lamaugarny, A.; El Jammal, T.; Ducreux, S.; Chevalier, F.P.; Fromy, B. Aging is associated with impaired triggering of TRPV3-mediated cutaneous vasodilation: A crucial process for local heat exposure. Geroscience 2023, 46, 3567–3580. [Google Scholar] [CrossRef]
- Holowatz, L.A.; Kenney, W.L. Peripheral mechanisms of thermoregulatory control of skin blood flow in aged humans. J. Appl. Physiol. 2010, 109, 1538–1544. [Google Scholar] [CrossRef]
- Jung, D.; Kim, H.; An, J.; Hong, T. Thermoregulatory responses of young and elderly adults under temperature ramps. Build Environ. 2023, 244, 110760. [Google Scholar] [CrossRef]
- Lien, T.C.; Tabata, T. Regional incidence risk of heat stroke in elderly individuals considering population, household structure, and local industrial sector. Sci. Total Environ. 2022, 853, 158548. [Google Scholar] [CrossRef]
- Li, T.; Horton, R.M.; Bader, D.A.; Zhou, M.; Liang, X.; Ban, J.; Sun, Q.; Kinney, P.L. Aging Will Amplify the Heat-related Mortality Risk under a Changing Climate: Projection for the Elderly in Beijing, China. Sci. Rep. 2016, 6, 28161. [Google Scholar] [CrossRef] [PubMed]
- van Steen, Y.; Ntarladima, A.M.; Grobbee, R.; Karssenberg, D.; Vaartjes, I. Sex differences in mortality after heat waves: Are elderly women at higher risk? Int. Arch. Occup. Environ. Health 2019, 92, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Leon, L.R.; Helwig, B.G. Heat stroke: Role of the systemic inflammatory response. J. Appl. Physiol. 2010, 109, 1980–1988. [Google Scholar] [CrossRef] [PubMed]
- De Gea Grela, P.; Sánchez-González, D.; Gallardo Peralta, L.P. Urban and Rural Environments and Their Implications for Older Adults’ Adaptation to Heat Waves: A Systematic Review. Land 2024, 13, 1378. [Google Scholar] [CrossRef]
- Bunker, A.; Wildenhain, J.; Vandenbergh, A.; Henschke, N.; Rocklöv, J.; Hajat, S.; Sauerborn, R. Effects of Air Temperature on Climate-Sensitive Mortality and Morbidity Outcomes in the Elderly; a Systematic Review and Meta-analysis of Epidemiological Evidence. eBioMedicine 2016, 6, 258–268. [Google Scholar] [CrossRef]
- McGarr, G.W.; Meade, R.D.; Notley, S.R.; Akerman, A.P.; Richards, B.J.; McCourt, E.R.; King, K.E.; McCormick, J.J.; Boulay, P.; Sigal, R.J.; et al. Physiological responses to 9 hours of heat exposure in young and older adults. Part III: Association with self-reported symptoms and mood state. J. Appl. Physiol. 2024, 136, 408–420. [Google Scholar] [CrossRef]
- Wu, Y.; Zhang, Z.; Liu, H.; Li, B.; Chen, B.; Kosonen, R.; Jokisalo, J. Age differences in thermal comfort and physiological responses in thermal environments with temperature ramp. Build Environ. 2023, 228, 109887. [Google Scholar] [CrossRef]
- Chow, L.; Zhao, G.; Wu, P.; Huang, X.; Li, J.; Li, J.; Wang, W.; Guo, G.; Li, Z.; Wang, J.; et al. Soft, body conformable electronics for thermoregulation enabled by kirigami. Biodes Manuf. 2024, 7, 453–462. [Google Scholar] [CrossRef]
- Wu, B.; Lin, Y.; Tian, Y.; Wei, W.; Xu, Y.; Hu, Y.; Li, J.; Li, K.; Hou, C.; Zhang, Q.; et al. Bioinspired Wearable Thermoelectric Device Constructed with Soft-Rigid Assembly for Personal Thermal Management. Adv. Funct. Mater. 2024, 34, 2402319. [Google Scholar] [CrossRef]
- Hong, S.; Gu, Y.; Seo, J.K.; Wang, J.; Liu, P.; Meng, Y.S.; Xu, S.; Chen, R. Wearable thermoelectrics for personalized thermoregulation. Sci. Adv. 2019, 5, eaaw0536. [Google Scholar] [CrossRef]
- Zuo, X.; Zhang, X.; Qu, L.; Miao, J. Smart Fibers and Textiles for Personal Thermal Management in Emerging Wearable Applications. Adv. Mater. Technol. 2023, 8, 2201137. [Google Scholar] [CrossRef]
- Hu, R.; Liu, Y.; Shin, S.; Huang, S.; Ren, X.; Shu, W.; Cheng, J.; Tao, G.; Xu, W.; Chen, R.; et al. Emerging Materials and Strategies for Personal Thermal Management. Adv. Energy Mater. 2020, 10, 1903921. [Google Scholar] [CrossRef]
- Jung, Y.; Kim, M.; Kim, T.; Ahn, J.; Lee, J.; Ko, S.H. Functional Materials and Innovative Strategies for Wearable Thermal Management Applications. Nanomicro Lett. 2023, 15, 160. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Tan, J.; Tan, J.J.; Tang, H.T.; Yu, W.S.; Lam, N.Y.K. Intelligent Thermochromic Heating E-Textile for Personalized Temperature Control in Healthcare. ACS Appl. Mater. Interfaces 2025, 17, 5515–5526. [Google Scholar] [CrossRef]
- Wu, D.; Zhang, R.; Zang, L. Functional Design and Development of Smart Temperature Regulating Clothing Based on Artificial Intelligence. J. Comb. Math. Comb. Comput. 2025, 127, 4241–4255. [Google Scholar]
- Zhang, X.; Chen, J.; Zheng, Z.; Tang, S.; Cheng, B.; Zhang, Z.; Ma, R.; Chen, Z.; Zhuo, J.; Cao, L.; et al. Flexible Temperature Sensor with High Reproducibility and Wireless Closed-Loop System for Decoupled Multimodal Health Monitoring and Personalized Thermoregulation. Adv. Mater. 2024, 36, e2407859. [Google Scholar] [CrossRef]
- Nyein, H.Y.Y.; Bariya, M.; Tran, B.; Ahn, C.H.; Brown, B.J.; Ji, W.; Davis, N.; Javey, A. A wearable patch for continuous analysis of thermoregulatory sweat at rest. Nat. Commun. 2021, 12, 1823. [Google Scholar] [CrossRef]
- Cao, M.; Deng, W.; Ma, C.B.; Bai, J.; Bo, X.; Sun, M.; Bai, X.; Zhou, M. Entirely Self-Contained Electrochromic Epidermal Patch for Visualized and Multiplexed In Situ Sweat Analysis. ACS Sens. 2025, 10, 4220–4231. [Google Scholar] [CrossRef]
- Rovira, M.; Lafaye, C.; Demuru, S.; Kunnel, B.P.; Aymerich, J.; Cuenca, J.; Serra-Graells, F.; Margarit-Taulé, J.M.; Haque, R.; Saubade, M.; et al. Assessing the performance of a robust multiparametric wearable patch integrating silicon-based sensors for real-time continuous monitoring of sweat biomarkers. Biosens. Bioelectron. 2024, 262, 116560. [Google Scholar] [CrossRef]
- Zhou, H.; Kort, H.S.M.; Loomans, M.G.L.C.; Tran, T.H.; Wei, S.; Zhang, Y.; Wang, Y.; Shi, W.; Zhou, S.; Yu, W. Lab study on the physiological thermoregulatory abilities of older people with different frailty levels. Build Environ. 2024, 266, 112130. [Google Scholar] [CrossRef]
- Ou, Y.; Wang, F.; Zhao, J.; Deng, Q. Risk of heatstroke in healthy elderly during heatwaves: A thermoregulatory modeling study. Build Environ. 2023, 237, 110324. [Google Scholar] [CrossRef]
- Balmain, B.N.; Sabapathy, S.; Louis, M.; Morris, N.R. Aging and Thermoregulatory Control: The Clinical Implications of Exercising under Heat Stress in Older Individuals. Biomed Res. Int. 2018, 2018, 8306154. [Google Scholar] [CrossRef]
- Millyard, A.; Layden, J.D.; Pyne, D.B.; Edwards, A.M.; Bloxham, S.R. Impairments to Thermoregulation in the Elderly During Heat Exposure Events. Gerontol. Geriatr. Med. 2020, 6, 2333721420932432. [Google Scholar] [CrossRef]
- Sackett, D.L.; Rosenberg, W.M.C.; Gray, J.A.M.; Haynes, R.B.; Richardson, W.S. Evidence based medicine: What it is and what it isn’t. BMJ 1996, 312, 71–72. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- ISO 9886:2004(en); Ergonomics—Evaluation of Thermal Strain by Physiological Measurements [Internet]. International Organization for Standardization: Geneva, Switzerland, 2024. Available online: https://www.iso.org/obp/ui/#iso:std:iso:9886:ed-2:v1:en (accessed on 6 November 2025).
- ThermoScan® IRT 3030 Heruntergeladen von Manualslib.de Handbücher-Suchmachiene. 2016. Available online: https://www.hot-europe.com (accessed on 6 November 2025).
- Predicted Mean Vote Index (PMV) [Internet]. Available online: https://www.engineeringtoolbox.com/predicted-mean-vote-index-PMV-d_1631.html (accessed on 6 November 2025).
- Adaptive Comfort Model [Internet]. Available online: https://cbe.berkeley.edu/research/adaptive-comfort-model/ (accessed on 6 November 2025).
- Foda, E.; Almesri, I.; Awbi, H.B.; Sirén, K. Models of human thermoregulation and the prediction of local and overall thermal sensations. Build Environ. 2011, 46, 2023–2032. [Google Scholar] [CrossRef]
- Lim, M.C.; Lukman, K.A.; Giloi, N.; Jeffree, M.S.; Saupin, S.S.; Sidek, Z.N.; Daud, M.N.M.; Andreas, G.D. Translation and cross-cultural adaptation of heat strain score index (HSSI) into the Malay language. PLoS ONE 2023, 18, e0281217. [Google Scholar] [CrossRef]
- Yazdanirad, S.; Foroushani, A.R.; Monazzam, M.R.; Dehghan, H.; Golbabaei, F. Development of an observational—Perceptual heat strain risk assessment (OPHSRA) index and its validation. BMC Public Health 2021, 21, 2323. [Google Scholar] [CrossRef]
- Wang, Z.; Yu, H.; Luo, M.; Wang, Z.; Zhang, H.; Jiao, Y. Predicting older people’s thermal sensation in building environment through a machine learning approach: Modelling, interpretation, and application. Build Environ. 2019, 161, 106231. [Google Scholar] [CrossRef]
- Yi Cyoon Childs, C.; Peng, C.; Robinson, D. Thermal comfort modelling of older people living in care homes: An evaluation of heat balance, adaptive comfort, and thermographic methods. Build Environ. 2022, 207, 108550. [Google Scholar] [CrossRef]
- Forbes, C.; Coccarelli, A.; Xu, Z.; Meade, R.D.; Kenny, G.P.; Binnewies, S.; Bach, A.J. Biophysical versus machine learning models for predicting rectal and skin temperatures in older adults. J. Therm. Biol. 2025, 128, 104078. [Google Scholar] [CrossRef] [PubMed]
- ISO 14001:2004; Norma Internacional. ISO Copyright Office: Geneva, Switzerland, 2004.
- Wang, J.; Li, Q.; Zhu, G.; Kong, W.; Peng, H.; Wei, M. Recognition and prediction of elderly thermal sensation based on outdoor facial skin temperature. Build Environ. 2024, 253, 111326. [Google Scholar] [CrossRef]
- Shaban, M.; Amer, F.G.M.; Shaban, M.M. The impact of nursing sustainable prevention program on heat strain among agricultural elderly workers in the context of climate change. Geriatr. Nurs. 2024, 58, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Lei, Y.; Liu, M.; Zhu, L.; Zhai, Y.; Zhou, X.; Qiu, X.; Fan, Q.; Li, J.; Li, Z. Differences in the elderly’s behaviour pattern of using room air conditioners between the normal and extremely-hot summers—A case in Chongqing, China. Energy Build. 2025, 328, 115237. [Google Scholar] [CrossRef]
- Chen, M.; Younes, J.; Farahani, A.V.; Kilpeläinen, S.; Kosonen, R.; Ghaddar, N.; Ghali, K.; Melikov, A.K. Evaluating thermal response when elderly people using local cooling devices: Correlation among overall and local thermal sensation with skin temperature. Build Environ. 2024, 251, 111217. [Google Scholar] [CrossRef]
- Younes, J.; Chen, M.; Ghali, K.; Kosonen, R.; Melikov, A.K.; Kilpeläinen, S.; Ghaddar, N. Enhancing thermal comfort of older adults during extreme weather: Combined personal comfort system and ventilated vest. Energy Build. 2024, 318, 114437. [Google Scholar] [CrossRef]
- Lee, J.; Seo, S.; Han, S.; Koo, C. A simplified machine learning model to forecast individual thermal comfort in older adults’ residential spaces without relying on wearable devices. Sustain. Cities Soc. 2025, 119, 106085. [Google Scholar] [CrossRef]
- Wang, Z.; Yu, H.; Jiao, Y.; Chu, X.; Luo, M. Chinese older people’s subjective and physiological responses to moderate cold and warm temperature steps. Build Environ. 2019, 149, 526–536. [Google Scholar] [CrossRef]
- Krayenhoff, E.S.; Broadbent, A.M.; Zhao, L.; Georgescu, M.; Middel, A.; Voogt, J.A.; Martilli, A.; Sailor, D.J.; Erell, E. Cooling hot cities: A systematic and critical review of the numerical modelling literature. Environ. Res. Lett. 2021, 16, 053007. [Google Scholar] [CrossRef]
- Crank, P.J.; Sailor, D.J.; Ban-Weiss, G.; Taleghani, M. Evaluating the ENVI-met microscale model for suitability in analysis of targeted urban heat mitigation strategies. Urban Clim. 2018, 26, 188–197. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
| Population | Older adults (≥60 years), in community, institutional, or clinical settings. |
| Intervention | Strategies, devices, or programs aimed at assessing or improving thermoregulation (e.g., wearables, smart clothing, community interventions during heat waves, cooling or hydration protocols). |
| Outcomes | Improvement in body temperature monitoring, early detection of alterations, reduction in heat- or cold-related adverse events, enhanced safety and well-being. |
| Research question | What interventions and technologies have been implemented in older adults to assess or improve thermoregulation, and what outcomes have they reported in terms of monitoring, prevention of adverse thermal events, and promotion of thermal well-being? |
| Data Base | Search Strategies |
|---|---|
| PubMed | ((“Aged” [MeSH] OR “Older adults” OR elderly OR “older people” OR seniors) AND (“Thermoregulation” [MeSH] OR thermoregulation OR “body temperature regulation” OR “heat stress disorders” [MeSH] OR “cold stress” OR “thermal stress”) AND (“Wearable Electronic Devices” [MeSH] OR wearable * OR “smart clothing” OR “sensors” OR “monitoring device *” OR “community intervention *” OR “public health intervention *”) AND (“Program Evaluation” [MeSH] OR intervention * OR technology OR prevention OR monitoring OR wellbeing OR safety)) |
| Scopus | (TITLE-ABS-KEY(“older adults” OR elderly OR “older people” OR seniors) AND TITLE-ABS-KEY(thermoregulation OR “body temperature regulation” OR “thermal stress” OR “heat stress” OR “cold stress”) AND TITLE-ABS-KEY(wearable * OR “smart clothing” OR sensor * OR “monitoring device *” OR “community intervention *” OR “public health intervention *”) AND TITLE-ABS-KEY(intervention * OR technology OR prevention OR monitoring OR wellbeing OR safety)) |
| ScienceDirect | (“older adults” OR elderly) AND (thermoregulation OR “thermal stress”) AND (wearable OR sensor OR “smart clothing” OR cooling)AND (“body temperature” OR “adverse events”) |
| WOS | TS = (“older adults” OR elderly OR “older people” OR seniors) AND TS = (thermoregulation OR “body temperature regulation” OR “thermal stress” OR “heat stress” OR “cold stress”) AND TS = (wearable * OR “smart clothing” OR sensor * OR “monitoring device *” OR “community intervention *” OR “public health intervention *”) AND TS = (intervention * OR technology OR prevention OR monitoring OR wellbeing OR safety) |
| Typology/Main Objective | Participants | Variables/Instruments | Main Findings | International Banking Institute (JBI) | |
|---|---|---|---|---|---|
| [43] | Design: non-randomized experimental study. Objective: To develop predictive models of thermal sensation in older adults using field and laboratory data, and to evaluate their accuracy against existing PMV and UCB models. | N field = 1040 Age = 70–97 years Sex (f/m)%: 66.3%/33.7% N laboratory: 18 Age: 65–83 Sex (f/m): 9/9 | Demographic: age, sex, self-reported health, degree of acclimatization, lifestyle habits (questionnaire) Environmental: air temperature (WSZY-1), relative humidity (10–90%), black globe temperature (TM200), air velocity (Air velocity meter 9515), illuminance (ZDS-10F-3D: Shanghai Precision Instrument Co., Ltd; Shangai, China), CO2 concentration (Testo 535), sound level (TES-1350A) Physiological: skin temperature (Pyrobutton-L) at 8 locations in the laboratory, measured every 1 min Thermal sensation: TSV using a 7-point scale (field and laboratory), subsequently recoded into 3 categories (Cool, Neutral, Warm) | In the field study, air temperature was the strongest predictor of older adults’ thermal sensation, with “Cool” at ~13 °C, “Warm” at ~30 °C, and “Neutral” around 14 °C and 28 °C. Other significant predictors included air velocity, illuminance, CO2 concentration, length of stay in aged-care homes, and self-reported health. The field study model achieved 56.6% overall accuracy, outperforming the PMV model (36.6%), which was biased toward “Cool.” In the lab study, five skin temperatures (head, lower arm, upper leg, chest, back) predicted thermal sensation with 76.7% accuracy, better than the UCB model (46.6%). Head and lower arm temperatures were the most important local predictors, and an air velocity threshold (~0.25 m/s) indicated adaptive behaviors that reduce heat perception. Neutral temperature ranges varied by season and health: summer 25.3–32.5 °C, mid-season 9.2–27.6 °C, winter 6.4–19.9 °C; healthy, long-stay residents tolerated cooler temperatures. A simplified head temperature-only model reached 53.4% accuracy, showing single-site measurements can be useful but less precise than multi-site models. | 8/9 |
| [44] | Design: non-randomized experimental study Objective: To evaluate the applicability of three methods for measuring thermal comfort (Predicted Mean Vote, Adaptive Comfort, and infrared thermography of extremities) in older adults living in care homes, considering differences between participants with and without dementia. | N older adults: 69 Age older adults: 60–101 years N young adults: 17 Age young adults: 18–34 years | Age, sex, clinical frailty: 7-point frailty scale (Dalhousie University, version 2007-09) Indoor environmental conditions: air temperature, relative humidity, air speed (Kestrel 3000) Clothing insulation (clo): weighted valuation of clothing ensembles Body temperature: tympanic measurement (thermo-scan, Model LF 40, Braun) Subjective thermal comfort: Thermal Sensation Vote (TSV), ASHRAE 7-point scale (−3 to +3); Thermal preference: McIntyre thermal preference scale (cooler, no change, warmer) | The study evaluated 69 older adults (34 with dementia and 35 without dementia) in 15 care homes in the UK over one year. The mean indoor temperature was 23.6 °C, with no significant differences between summer and heating periods, and clothing insulation remained stable (0.6–0.7 clo). Residents with dementia wore slightly thicker clothing (0.70 vs. 0.60 clo, p = 0.005) and were in slightly cooler spaces (23.15 °C vs. 24.07 °C, p = 0.001), while residents without dementia adjusted their clothing according to temperature. The PMV model indicated a comfort threshold between −0.51 and −0.76 PMV, with an estimated MET centered between 1.3 and 1.39, showing sensitivity to low activity levels. The adaptive approach estimated the comfort zone for non-dementia residents between 22.8 and 23.6 °C, with 80% reporting no desire to change the temperature. Infrared thermography measurements (ΔT1) between fingers and wrist correlated with comfort perception in young adults and older adults without dementia (r = 0.667–0.839, p < 0.05), but were not useful for residents with dementia; in older adults, core body temperature (+) and clothing insulation (−) were the most influential factors on ΔT1. | 8/9 |
| [45] | Design: non-randomized experimental study Objective: Develop and evaluate models for predicting body temperature (rectal and skin) in older adults (≥60 years) under different temperature and humidity conditions, and compare them with existing biological models. | N = 76 Age: ≥60 years Sex (f/m): 32/44 | Rectal temperature (core): Continuous measurement using rectal thermometer (per minute) Mean skin temperature: Calculated according to ISO 2004 [46] using weighted measurements from: forehead (7%), right scapula (17.5%), upper left chest (17.5%), upper right arm (7%), right forearm (7%), left hand (5%), right anterior thigh (19%), left calf (20%) Height: Measured in centimeters (cm) Body mass: Measured in kilograms (Kg) Ambient temperature: Measured in chamber (°C) Relative humidity: Measured in chamber (%) Previous temperatures: Rectal and skin temperatures from the previous minute (input for point-wise models) Model type: Linear regression, Ridge regression, Recurrent Neural Network (RNN), Long Short-Term Memory (LSTM), Gated Recurrent Unit (GRU) Model evaluation: Root-Mean Squared Error (RMSE), Mean Bias Error (MBE), Bland–Altman Limits of Agreement, proportion of participants within clinical thresholds (0.3 °C rectal, 1.0 °C skin) | This study developed machine learning models and compared their accuracy with biophysical models to predict rectal and skin temperature in older adults. The Ridge and Linear Regression models predicted temperatures better than traditional biophysical models. Ridge Regression had the lowest root mean square error (RMSE) for rectal temperature (0.27 °C), skin (0.73 °C), and body (0.34 °C). Among sequence models, GRU was the most accurate, while RNN performed the worst. The Takahashi and Ji biophysical models predicted reasonably well; Takahashi was better for skin and body, Ji for rectal. Ridge Regression achieved 114 out of 162 participants with rectal temperature within a clinical limit of 0.3 °C and 142 out of 162 for skin within 1 °C. Most machine learning models showed mean biases (MBE) close to zero, indicating no systematic over- or underestimation. Age slightly increased the rectal temperature predicted by Ridge, while height and weight affected it variably depending on the model. High ambient temperature and humidity increased predicted temperatures, with some exceptions in GRU. Sequence models could outperform simple regression models in more dynamic conditions if trained with more data. These individualised predictions could improve heat risk monitoring and guide preventive interventions in older adults. | 7/9 |
| [47] | Design: non-randomized experimental study Objective: To explore whether facial skin temperature measured using infrared imaging can be used as an indicator of thermal sensation in older adults, and to evaluate the performance of different machine learning models in predicting that sensation. | N: 34 Age: ≥60 years, mean 83 years Sex (f/m): 20/14 | Facial skin temperature (forehead, eyes, nose, cheek, chin): Testo 872 thermal imaging camera (resolution 320 × 240 px, accuracy ±2 °C, thermal sensitivity <0.05 °C). Air temperature (Ta) and relative humidity (RH): HOBO MX2302A (accuracy ±0.02 °C; ±2.5% RH; frequency: 1 min). Wind speed (v) and black globe temperature (Tg): HD32.3 (accuracy ±0.15 m/s; class 1/3 DIN; frequency: 1 min). Mean radiant temperature (Tmrt): calculated from Tg, Ta, v and physical constants. Basic information: age, gender, weight, height, clothing. Perceptions: wind chill, thermal comfort, preferences (air, humidity, solar radiation, air speed). | During the experiment, the average air temperature was 31.5 °C, relative humidity was 73.5%, wind speed was 1.5 m/s, and solar radiation was 200 W/m2, representative of summer in Guangzhou. In terms of perceived temperature and comfort ratings, the more exercise the participants did, many participants reported neutral or comfortable sensations even in warm environments, which may reflect altered thermal perception rather than true heat tolerance. In terms of environmental preferences, older adults showed low sensitivity to humidity but a marked preference for higher air velocity, indicating ventilation as key to thermal comfort. The average facial temperature was highest on the nose (35.1 °C) and lowest on the cheek (34.2 °C). The recorded range was: nose: 31.9–39.1 °C, eyes: 32.6–38.3 °C, forehead: 31.5–38.6 °C, cheek: 30.7–38.0 °C, chin: 30.8–37.8 °C. There were significant differences between facial regions (p < 0.001). The greatest effect was observed between the nose and cheeks (d = 0.813, large). Facial temperature was related to the thermal sensation: In ‘neutral’: nose 35.4 °C, eyes 35.3 °C, cheek 34.5 °C; In ‘heat’: nose 36.5 °C, eyes 36.1 °C, cheek 35.3 °C. Of the prediction models, Random Forest (RF) was the most accurate (AUC = 0.889, accuracy = 80.6%), outperforming other algorithms (SVM and LR with AUC = 0.706). For prediction with fewer measurFor prediction with fewer measurement points, the best single site was the nose (AUC = 0.825). With two points: nose + cheek (AUC = 0.856); with three points: forehead + nose + chin (AUC = 0.876); with four points: eyes + forehead + nose + chin (AUC = 0.888). The nose was present in all optimal combinations, making it the key site for monitoring thermal sensation in older adults. | 9/9 |
| [48] | Design: non-randomized experimental study Objective: Evaluate the effectiveness of a sustainable heat stress prevention program (Sustainable Prevention Programme) in reducing excessive heat among agricultural workers over the age of 60. | N = 120 Age: ≥60 years Sex (f/m): 41/79 | Perceived heat strain: Observational-Perceptual Heat Strain Risk Assessment (OPHSRA) Individual heat strain: Heat Strain Score Index (HSSI) Knowledge and behaviors regarding heat prevention: Socio-demographic questionnaire and interviews Environmental exposure: Measurement of temperature, humidity, and solar exposure | The intervention consisted of education on hydration, breaks, protective clothing, and recognition of heat stress symptoms, delivered over six weeks in interactive sessions. The results showed significant improvements in the intervention group: the percentage of participants classified as “safe” on the HSSI increased from 26.7% to 45.0% (p = 0.007), while those considered “at risk” decreased from 25.0% to 15.0% (p = 0.014). Similarly, the OPHSRA indicated an increase in low risk from 18.3% to 31.7% (p = 0.003) and a decrease in very high risk from 11.7% to 5.0% (p = 0.001). The control group showed no significant changes. In the OPHSRA, the ‘low’ risk increased from 18.3% to 31.7% after the program (p = 0.003). The ‘very high’ risk in OPHSRA was reduced from 11.7% to 5.0% in the intervention group (p = 0.001). The intervention tripled the odds of lower heat stress incidence (OR = 3.38; p < 0.001). Being male was associated with a higher risk of heat stress (OR = 1.55; p = 0.013). Each additional hour of exposure to high temperatures increased the risk by 9% (OR = 1.09; p = 0.003). Having hypertension increased the risk of heat stress by 68% (OR = 1.68; p = 0.006), and diabetes by 57% (OR = 1.57; p = 0.026). Age and work experience were associated with a reduced risk of heat stress (OR = 0.95 and 0.97; p = 0.039 and 0.016, respectively). | 9/9 |
| [49] | Design: Observational Objective: Investigate differences in air conditioning use and indoor thermal demand among older adults during an extremely hot summer (2022) and a normal summer (2023) in Chongqing, China. | N = 26 Age: 84 ± 7 years Sex (f/m): 12/14 | Age, sex, height, weight, BMI: Initial questionnaire/anthropometric data. Indoor air temperature: Hobo temperature/relative humidity data logger—UX100-003. Indoor relative humidity: Hobo temperature/relative humidity data logger—UX100-003. Outdoor air temperature: Hobo temperature/relative humidity data logger—UX100-003 (installed in open staircase). Air conditioner (RAC) operation time: Cloud platform connected via IoT to RAC. Air conditioner (RAC) activation frequency: Cloud platform connected via IoT to RAC. Air conditioner (RAC) setpoint temperature: Cloud platform connected via IoT to RAC. | During the extremely hot summer, the outdoor temperature exceeded 35 °C for 19 days, and the average indoor temperature was higher (29.8 °C vs. 28.4 °C in a normal summer). Thermal comfort was limited: only 12% of the time was within the comfortable range in extreme summer with air conditioning on, compared to 34% in a normal summer. Air conditioning (RAC) use was 2.4 times higher in extreme summer (26% of the time vs. 11% in normal summer), with more prolonged episodes (>10 h). The elderly turned on the RAC more often in extreme summer (44% multiple times/day), but one-third never used it, even in intense heat. The RAC was turned on at higher indoor temperatures in extreme summer (29.8 °C vs. 28.3 °C, p < 0.001). In normal summer, frequent switching on before dawn suggests possible sleep interruptions. Set points were higher in extreme summer (28.8 °C, preference 30 °C) than in normal summer (26.7 °C, preference 26 °C). Predictive analysis showed that each 1 °C increase in outdoor temperature increased the probability of RAC use by 6.9% (extreme summer) and 8.4% (normal summer). However, even at >40 °C, maximum use reached only 60%. | 10/11 |
| [50] | Design: non-randomized experimental study Objective: To evaluate how the use of three local cooling devices (table fan, air jacket, and evaporative device) affects skin temperature and thermal sensation in older adults, and to explore the relationship between skin temperature and thermal sensation. | N = 26 Age: ~70.8 years Sex (f/m): 19/7 | Local skin temperature: iButton sensors (DS1923, accuracy ± 0.5 °C) Core temperature (tympanic): Ear thermometer (Braun IRT6520, accuracy ± 0.2 °C) Overall thermal sensation: Questionnaire, 7-point scale (−3 cold to +3 hot) Local thermal sensation (head, torso, limbs, extremities): Questionnaire, 7-point scale (−3 cold to +3 hot) Air temperature (Ta): TinyTag 2 Plus data loggers (accuracy ±0.5 °C) Relative humidity (RH): TinyTag 2 Plus data loggers (accuracy ± 3%) Operative temperature (To): ComfortSense probes (accuracy ± 0.2 °C) Air velocity: ComfortSense probes (accuracy ± 0.02 m/s) Cooling effect on body segments (heat loss): Thermal manikin with 27 body segments, electricity consumption measurements Power consumption of cooling devices: Device specifications + manikin test measurements | Ambient temperature (Ta) significantly influenced skin temperature (p < 0.05), whereas relative humidity did not (p > 0.05). In older adults, distal regions (head, hands, feet) showed lower skin temperatures than in younger adults. The MST (mean skin temperature) decreased significantly in the first 10 min after using cooling devices, with reductions <0.5 °C (p < 0.05). The core temperature decreased significantly after using devices compared to the uniform condition (p < 0.05), remaining stable during the cooling phase. Significant local temperature decreases: Fan: chest, forearm and palm (up to −0.8 °C and −0.6 °C in slightly warm conditions, p < 0.01). Evaporative device: forearm (−0.9 °C) and chest (−1.1 °C) in warm conditions (p < 0.01). Air jacket: chest and lumbar region (−0.6 to −0.7 °C, p < 0.01). The evaporative and air jacket devices were more effective in warm environments, while the fan was more effective in slightly warm environments. Cooling mainly affected exposed parts (chest, arms, hands, upper and lower back), while unexposed parts (feet, calves) remained further from the neutral range. The thermal sensation (TSV) was significantly reduced in exposed areas (p < 0.05), with greatest influence on overall perception. The strongest correlation between skin temperature and thermal sensation was observed in the extremities and hands, especially in the fingers (highest r). The thermosensory mean skin temperature (TMST) was a better predictor of overall thermal sensation than the classic MST (p < 0.01). | 8/9 |
| [51] | Design: non-randomized experimental study Objective: To evaluate the effect of a personal comfort system (PCS) based on a microclimatic chair combined with a ventilated vest on the thermal sensation (TS) of elderly people in hot conditions, optimizing thermal comfort and reducing energy consumption. | N = 29 Age: 70.9 ± 5.8 years Sex: not specified | Whole-body Thermal Sensation, TS: Subjective voting on ASHRAE 7-point scale Mean and segmental skin temperature: Temperature sensors in thermal manikin and experimental human data Air velocity and temperature in microclimate: Omnidirectional anemometers and thermocouples Ventilation and air flow in vest: Fan flow rate and flow sensors Energy consumption: Electrical power calculations for compressors and fans | The temperature predicted by Computational Fluid Dynamics (CFD) and the vest model matched experimental measurements within a range of ±0.5 °C. The predicted air velocity matched measurements within ±0.2 m/s. Activation of the vest reduced internal temperatures in the torso by up to 3.4 °C (Personalized Conditioning System (PCS) switched on). The maximum difference between the predicted and measured temperature in the vest was 0.6 °C. Impact on skin temperature and thermal sensation in older adults: With PCS alone (33 °C, 22 °C, 17–21 l/s): mean skin temperature (Tsk) 34.0–34.1 °C, TS ≈ 0.8–0.9 (slightly warm). PCS + vest (33 °C, 22 °C, PCS 17–21 l/s, vest 6–11 l/s): Tsk 33.7–34.0 °C, TS 0.5–0.8 (neutral to slightly warm). PCS + vest reduces trunk Tsk by up to 1.7 °C compared to PCS alone. At 29 °C, PCS alone (22 °C, 17–21 l/s): Tsk 33.3–33.4 °C, TS ≈ 0 to −0.1 (neutral). PCS + vest (29 °C, 22 °C, PCS 21 l/s, vest 11 l/s): Tsk 32.8 °C, TS ≈ −0.4 (slightly cool). PCS creates a cool microclimate around the body (~28–30 °C). Vest extracts cool air from the microclimate, which can raise the temperature in the lower body by up to 0.5 °C, but does not significantly affect the inner skin. Wider microclimate with high-flow PCS and low-flow vest; finer microclimate with activated vest and lower flow. | 8/9 |
| [52] | Design: non-randomized experimental study Objective: Develop and validate a simplified machine learning model to predict individual thermal comfort in older adults without using wearable devices, using personal, environmental, and temporal variables. | N = 8 Age: ≥60 years Sex: Not specified | Physical activity/metabolic rate (MET): machine learning model using proxy variables Individual thermal comfort (PMV): Calculated with PMV considering air temperature, relative humidity (SHT30 sensors), assumed mean radiant temperature, air velocity (0.1 m/s), clothing insulation (0.5–1 clo), and metabolic rate Height, Weight, BMI, Percent body fat (PBF), Skeletal muscle mass (SMM), Body fat mass (BFM), Visceral fat level (VFL): Inbody dial WH20 N body composition analyzer Air temperature, Relative humidity: IoT sensor SHT30 | Welch’s ANOVA showed significant differences in thermal comfort among the eight older adults even under similar thermal environments (Levene p < 0.001; ANOVA p < 0.05 in all seasons). The Random Forest model accurately predicts metabolic activity and thermal comfort without the need for portable devices. Mean absolute error (MAE) of metabolic activity (MET): 0.097–0.106 depending on the season, average 0.098. MAE of thermal comfort (PMV): 0.039–0.058 depending on the season, average 0.048. The prediction tends to overestimate when actual values are low and underestimate when they are high. It is recommended to adjust predictions according to the population mean to improve accuracy. | 9/9 |
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | |
|---|---|---|---|---|---|---|---|---|---|
| [43] | + | + | + | - | + | + | + | + | + |
| [44] | + | + | + | - | + | + | + | + | + |
| [45] | + | + | - | + | - | + | + | + | + |
| [47] | + | + | + | + | + | + | + | + | + |
| [48] | + | + | + | + | + | + | + | + | + |
| [50] | + | + | + | - | + | + | + | + | + |
| [51] | + | + | - | + | + | + | + | + | + |
| [52] | + | + | + | + | + | + | + | + | + |
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| [49] | + | + | + | + | + | + | + | + | + | - | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Núñez-Rodríguez, S.; Collazo-Riobó, C.; Menéndez-Vega, F.; Sedano, J.; Sánchez-Iglesias, A.I.; González-Bernal, J.J.; González-Santos, J. Thermoregulation and Heat Stroke Prevention in Older Adults: Advances in Emerging Technologies and Interventions. Sensors 2025, 25, 7058. https://doi.org/10.3390/s25227058
Núñez-Rodríguez S, Collazo-Riobó C, Menéndez-Vega F, Sedano J, Sánchez-Iglesias AI, González-Bernal JJ, González-Santos J. Thermoregulation and Heat Stroke Prevention in Older Adults: Advances in Emerging Technologies and Interventions. Sensors. 2025; 25(22):7058. https://doi.org/10.3390/s25227058
Chicago/Turabian StyleNúñez-Rodríguez, Sandra, Carla Collazo-Riobó, Félix Menéndez-Vega, Javier Sedano, Ana Isabel Sánchez-Iglesias, Jerónimo Javier González-Bernal, and Josefa González-Santos. 2025. "Thermoregulation and Heat Stroke Prevention in Older Adults: Advances in Emerging Technologies and Interventions" Sensors 25, no. 22: 7058. https://doi.org/10.3390/s25227058
APA StyleNúñez-Rodríguez, S., Collazo-Riobó, C., Menéndez-Vega, F., Sedano, J., Sánchez-Iglesias, A. I., González-Bernal, J. J., & González-Santos, J. (2025). Thermoregulation and Heat Stroke Prevention in Older Adults: Advances in Emerging Technologies and Interventions. Sensors, 25(22), 7058. https://doi.org/10.3390/s25227058







