Context-Aware Alerting in Elderly Care Facilities: A Hybrid Framework Integrating LLM Reasoning with Rule-Based Logic
Abstract
1. Introduction
- False Alarms: False alarms can be both positive and negative. A false positive alarm occurs when an alert is triggered even though there is no actual clinical need or emergency. A false negative alarm refers to a situation where a clinically important event occurs, but the system fails to detect or alert it.
- Unreachable Alarms: An unreachable alarm refers to an alert that is sent out but fails to reach the appropriate caregiver in time. This can be due to routing inefficiencies where an alert is sent to a nurse at such a time when the time to reach the elderly patient is not enough.
- Unattainable Alarms: An unattainable alarm is triggered and sent to a caregiver who is occupied or too far away to respond at the moment the event occurs.
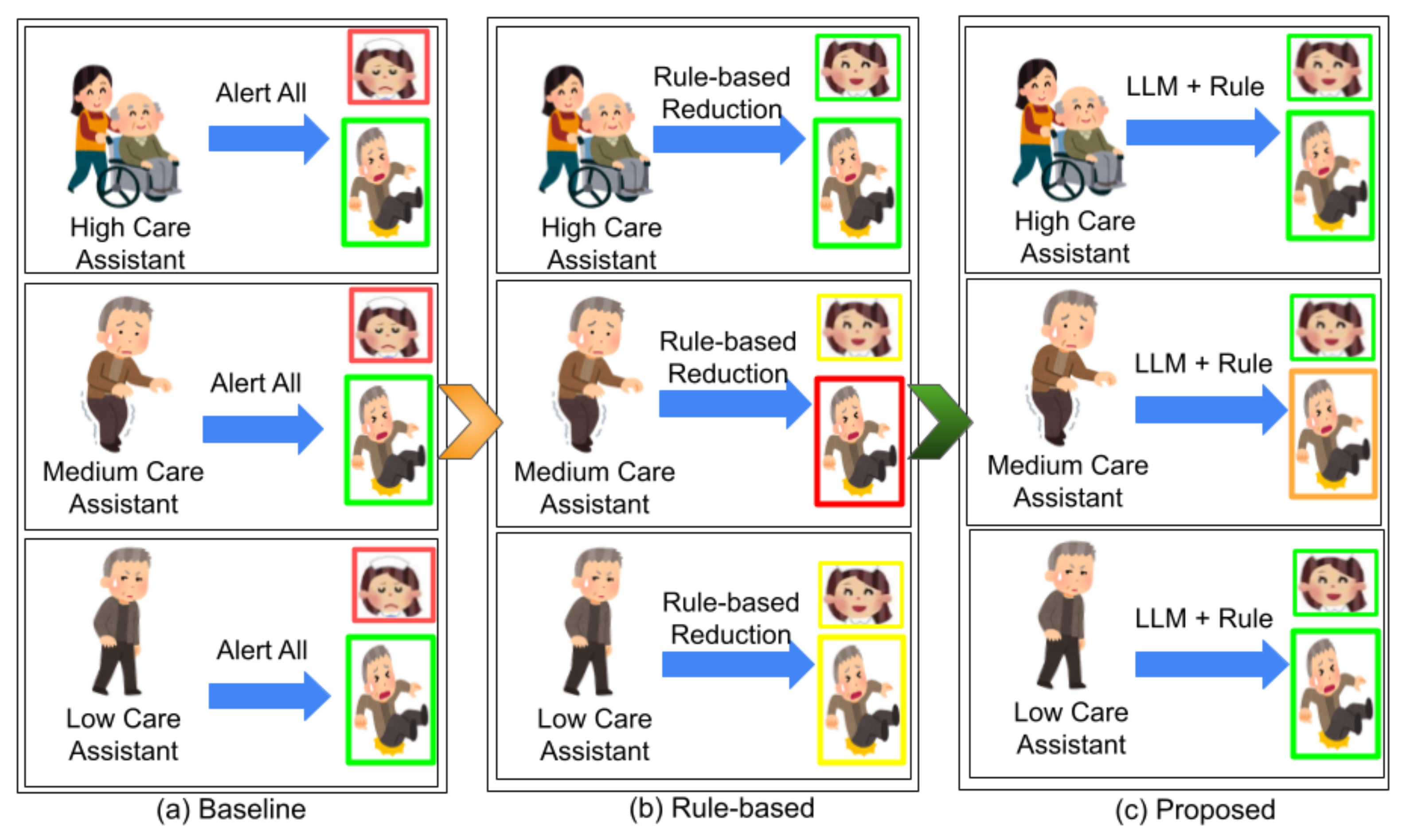
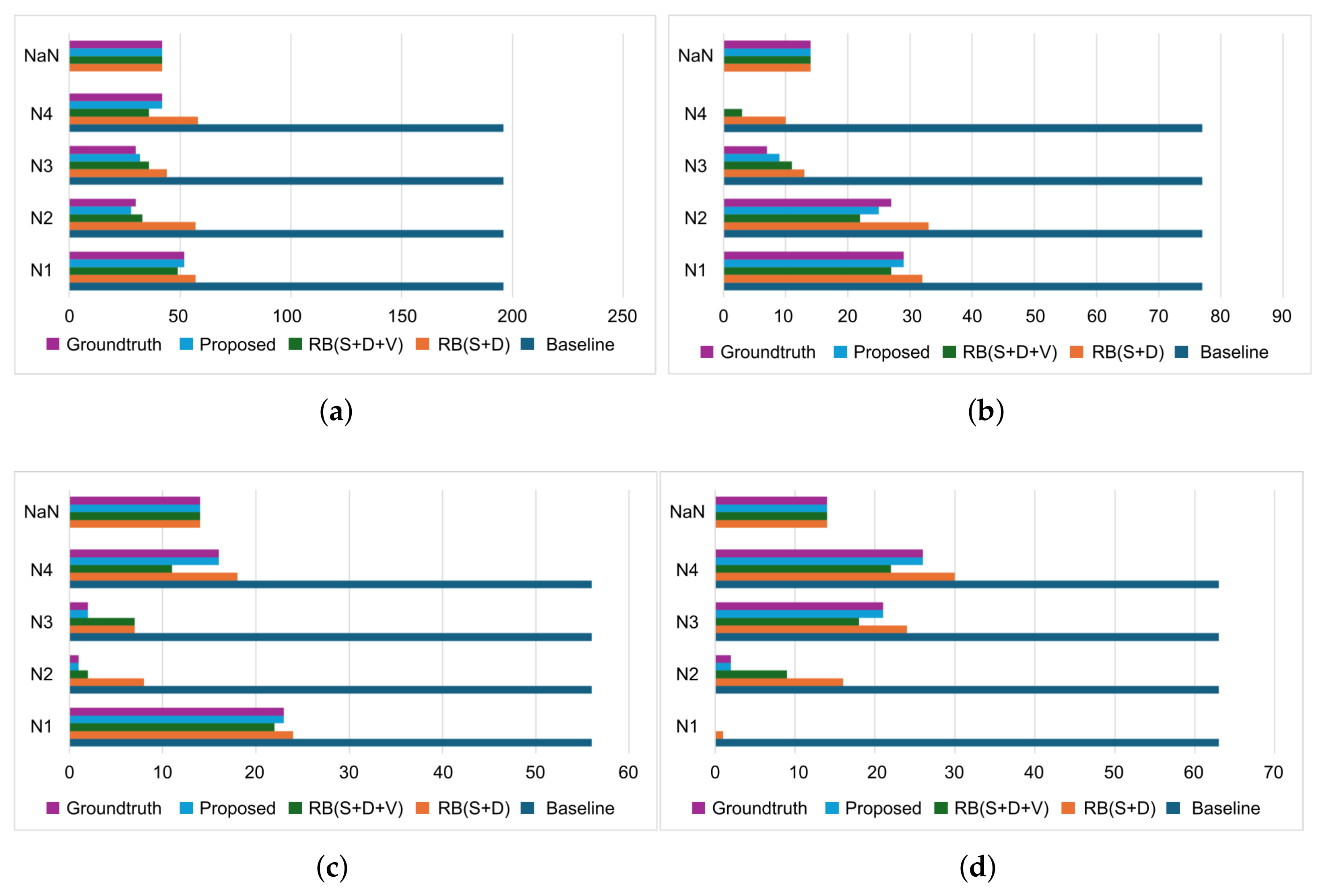
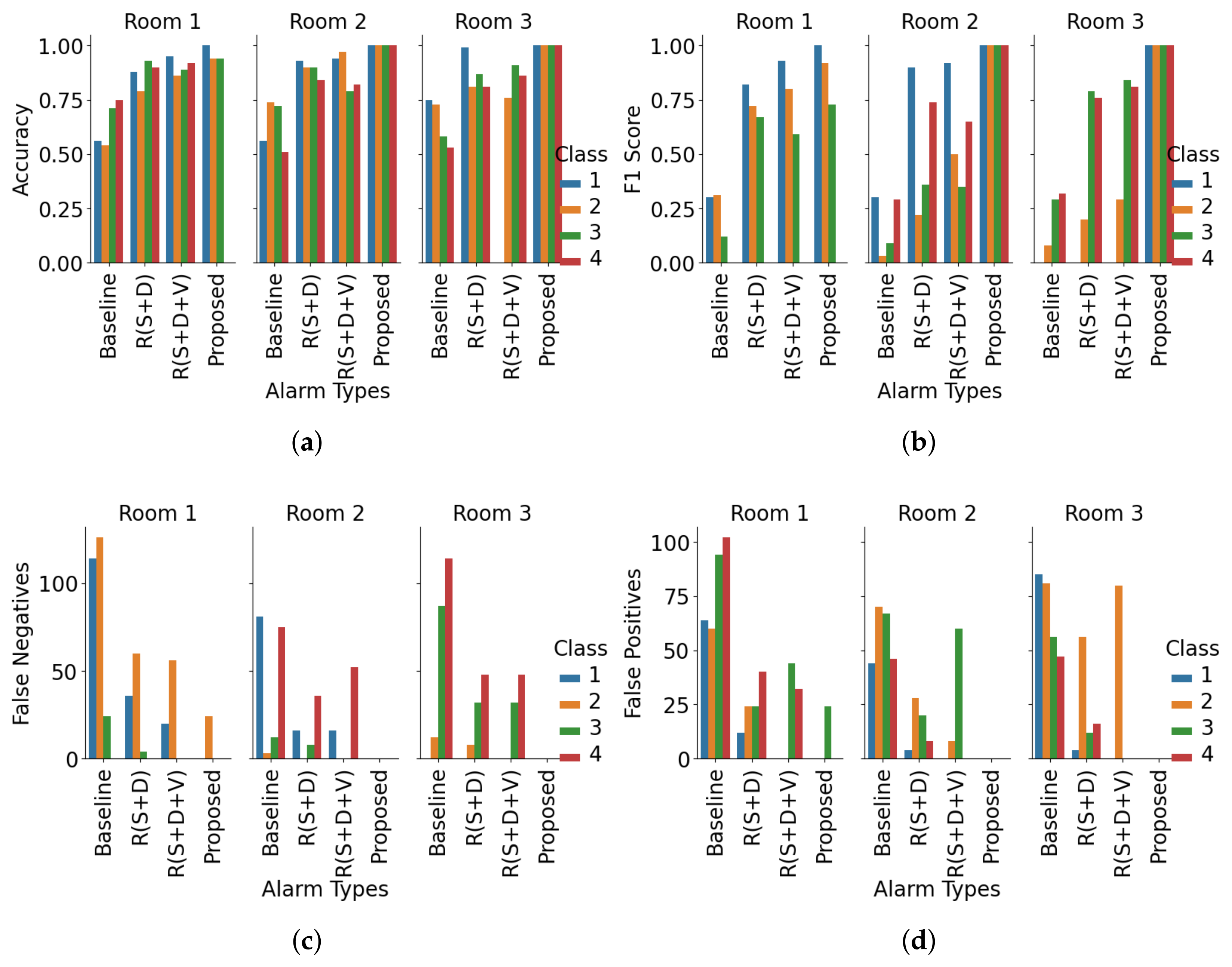
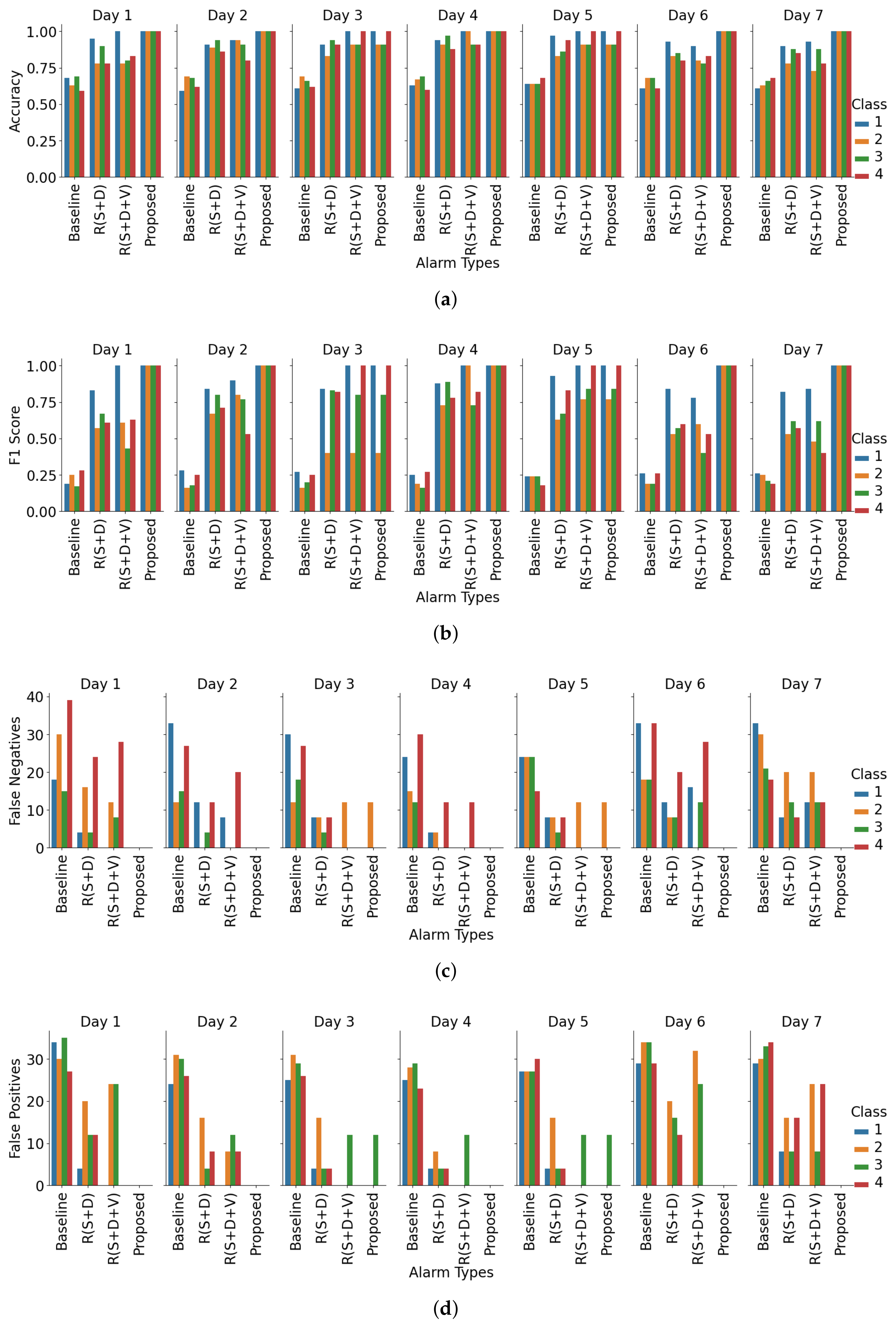
- Research question 1 (R1): How well does a hybrid alert framework consisting of rule-based logic and LLM reasoning minimize alert fatigue without compromising care quality?Contribution: This study introduces a hybrid alerting framework that combines rule-based logic with LLM reasoning to deliver context-aware alerts, aiming to reduce alarm fatigue without compromising care quality. Compared to the baseline scenario where all nurses were alerted (100% alarm load), the proposed framework lowered the average load to 27.5% but achieved an accuracy of 0.98 and a macro F1 score of 0.97, significantly surpassing the baseline (accuracy 0.21, macro F1 score 0.18).
- Research question 2 (R2): To what extent can the inclusion of clinically interpretable information help minimize false alarms in long-term care settings?Contribution: Our method leverages clinically interpretable parameters like resident care condition, nurse–resident distance, and mobility to generate alerts, minimizing false alarms. Compared to the baseline (FPR 0.20, FNR 0.79), the method achieves markedly lower error rates (FPR 0.005, FNR 0.023).
- Research question 3 (R3): Is a flexible, context-driven alert validation strategy more effective than static rule-based thresholds in addressing the unique needs of elderly care?Contribution: We introduce an LLM-based validation module that incorporates spatial, temporal, and clinical context, instead of rule-based thresholding. Our model achieved an accuracy of 0.98 and a macro F1 score of 0.97, outperforming the rule-based approach (accuracy 0.78, macro F1 score 0.79).
2. Related Works
2.1. Alarm Suppression Algorithms
2.2. Middleware Solutions and Notification Delay-Based Strategies
2.3. Alarm Validation Approaches
2.4. Challenges and Motivation
- Clinically non-interpretable suppression often leads to false negatives in LTC, where subtle transitions carry significant risk. Our proposed approach addresses this by discarding unattainable alerts by rules based on patient condition, nurse-to-patient distance, and nurse and patient speed.
- Rigid or middleware-based delays can endanger timely responses and impose technical overhead. We replace these with dynamic, context-driven delay mechanisms that balance responsiveness and workload.
- Context-unaware validation fails to capture care priorities, ignoring workload and resident-specific needs. Hence, we integrate spatial, temporal, and clinical context to ensure alerts are both technically valid and clinically actionable.
3. Problem Statement
- Suppression Function (:
- Distance Constraint: alarms are suppressed if the nurse is beyond a maximum reachable distance .
- Urgency Constraint: alarms triggered by very slow or clinically insignificant motion, i.e., trying to stand up slowly or moving to a side () are suppressed.
- Care Level Constraint: if the care level of the elderly resident indicates low dependency or low fall risk, alerts are suppressed unless overridden by urgent context.
- Delay Function ():
- Urgency: faster patient movement (e.g., abrupt standing up) implies shorter delays.
- Nurse Workload: overloaded nurses should receive alerts slightly later to reduce interruptions if the event is non-urgent.
- Resident Stability: higher risk of fall or instability reduces permissible delay.
- Validation Function ():
- Optimization Goal:
4. Context-Aware Alert System
| Algorithm 1 Context-Aware Alert Decision Framework |
|
4.1. Anomalous Event Detection
4.2. Feature Extraction and Representation Module
- (1)
- Temporal Context ():
- (2)
- Spatial Context ():
- (3)
- Urgency Context ():
- (4)
- Clinical Context ():
- (5)
- Resource Context ():
- (6)
- Feature Vector Construction:
4.3. Rule-Based Suppression Module
- Unreachable Alarms: This condition arises when a caregiver cannot reach the elderly within a clinically acceptable time window. In our study, we define this as the nurse failing to arrive within s, a value chosen empirically based on the nurse movement speed in our case study. It is adjustable depending on the requirements of the deployment setup. Here, , and the acceptable reaching time is expressed as .
- Unattainable Alarms: Alarms that are technically triggered but represent conditions that do not require further intervention. For our considered scenario, this condition is applied for fully dependent elderly residents. As there is always one attendant nurse beside them, there is no necessity for the alarm to be generated.
- Non-Urgent Context: Alarms where resident movement or posture change is within the normal behavioral profile based on their care level and history.
4.4. Context-Aware Delay Assignment Module
4.5. LLM-Driven Validation and Prioritization Module
4.6. Notification Sending and Preparation for Next Alert
- Releases the nurse from temporary lock if acknowledgment was successful.
- Updates the workload index and availability status .
- Clears the current alert context and fetches the next candidate alert from the queue.
- Invokes the full validation–assignment–dispatch loop for .
5. Experiment and Analysis
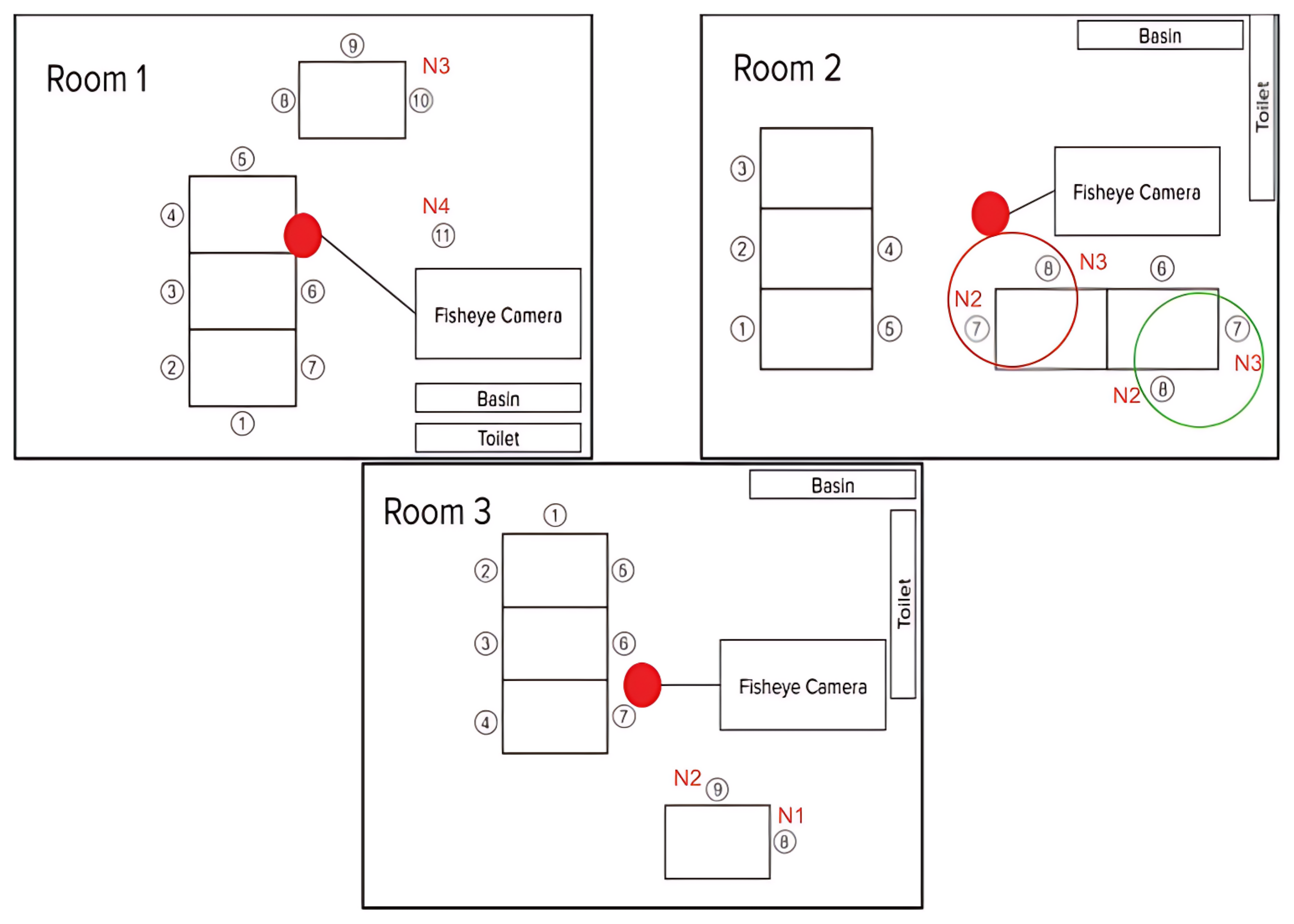
5.1. Data Collection
5.2. Validation Strategy
5.3. Results
6. Discussion
6.1. Contributions
6.2. Limitations and Future Challenges
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dykes, P.C.; Bogaisky, M.; Carter, E.J.; Duckworth, M.; Hurley, A.C.; Jackson, E.M.; Khasnabish, S.; Lindros, M.E.; Lipsitz, S.R.; Scanlan, M.; et al. Development and validation of a fall prevention knowledge test. J. Am. Geriatr. Soc. 2019, 67, 133–138. [Google Scholar] [CrossRef]
- Giordano, A.; Bonometti, G.P.; Vanoglio, F.; Paneroni, M.; Bernocchi, P.; Comini, L.; Giordano, A. Feasibility and cost-effectiveness of a multidisciplinary home-telehealth intervention programme to reduce falls among elderly discharged from hospital: Study protocol for a randomized controlled trial. BMC Geriatr. 2016, 16, 209. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, S. A Global Report on Falls Prevention. Epidemiology of Falls; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Røyset, B.; Talseth-Palmer, B.A.; Lydersen, S.; Farup, P.G. Effects of a fall prevention program in elderly: A pragmatic observational study in two orthopedic departments. Clin. Interv. Aging 2019, 14, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Florence, C.S.; Bergen, G.; Atherly, A.; Burns, E.; Stevens, J.; Drake, C. Medical costs of fatal and nonfatal falls in older adults. J. Am. Geriatr. Soc. 2018, 66, 693–698. [Google Scholar] [CrossRef] [PubMed]
- Haddad, L.M.; Annamaraju, P.; Toney-Butler, T.J. Nursing Shortage. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- De Raeve, N.; Shahid, A.; De Schepper, M.; De Poorter, E.; Moerman, I.; Verhaevert, J.; Van Torre, P.; Rogier, H. Bluetooth-Low-Energy-Based Fall Detection and Warning System for Elderly People in Nursing Homes. J. Sens. 2022, 2022, 9930681. [Google Scholar] [CrossRef]
- Harari, Y.; Shawen, N.; Mummidisetty, C.K.; Albert, M.V.; Kording, K.P.; Jayaraman, A. A smartphone-based online system for fall detection with alert notifications and contextual information of real-life falls. J. Neuroeng. Rehabil. 2021, 18, 124. [Google Scholar] [CrossRef]
- Bugarin, C.A.Q.; Lopez, J.M.M.; Pineda, S.G.M.; Sambrano, M.F.C.; Loresco, P.J.M. Machine vision-based fall detection system using mediapipe pose with IoT monitoring and alarm. In Proceedings of the 2022 IEEE 10th Region 10 Humanitarian Technology Conference (R10-HTC), Hyderabad, India, 16–18 September 2022; pp. 269–274. [Google Scholar]
- Saod, A.H.M.; Mustafa, A.A.; Soh, Z.H.C.; Ramlan, S.A.; Harron, N.A. Fall detection system using wearable sensors with automated notification. In Proceedings of the 2021 11th IEEE International Conference on Control System, Computing and Engineering (ICCSCE), Penang, Malaysia, 27–28 August 2021; pp. 182–187. [Google Scholar]
- Madona, E.; Ulfa, S.; Nasution, A. Implementation of IMU sensor for Fall Detection in Dementia Syndrome Patients with Location Notification System. J. Phys. Conf. Ser. 2022, 2406, 012010. [Google Scholar]
- Genco, E.K.; Forster, J.E.; Flaten, H.; Goss, F.; Heard, K.J.; Hoppe, J.; Monte, A.A. Clinically inconsequential alerts: The characteristics of opioid drug alerts and their utility in preventing adverse drug events in the emergency department. Ann. Emerg. Med. 2016, 67, 240–248. [Google Scholar] [CrossRef]
- McFarlane, D.C.; Doig, A.K.; Agutter, J.A.; Brewer, L.M.; Syroid, N.D.; Mittu, R. Faster clinical response to the onset of adverse events: A wearable metacognitive attention aid for nurse triage of clinical alarms. PLoS ONE 2018, 13, e0197157. [Google Scholar] [CrossRef]
- The Joint Commission. Sentinel Event Alert 50: Medical Device Alarm Safety in Hospitals. Available online: https://www.jointcommission.org/en-us/knowledge-library/newsletters/sentinel-event-alert/issue-50 (accessed on 1 July 2025).
- Sowan, A.K.; Staggers, N.; Reed, C.C.; Austin, T.; Chen, Q.; Xu, S.; Lopez, E. State of Science in Alarm System Safety: Implications for researchers, vendors, and clinical leaders. Biomed. Instrum. Technol. 2022, 56, 19–28. [Google Scholar] [CrossRef]
- Dee, S.A.; Tucciarone, J.; Plotkin, G.; Mallilo, C. Determining the impact of an alarm management program on alarm fatigue among ICU and telemetry RNs: An evidence based research project. SAGE Open Nurs. 2022, 8, 23779608221098713. [Google Scholar] [CrossRef]
- Nyarko, B.A.; Yin, Z.; Chai, X.; Yue, L. Nurses’ alarm fatigue, influencing factors, and its relationship with burnout in the critical care units: A cross-sectional study. Aust. Crit. Care 2024, 37, 273–280. [Google Scholar] [CrossRef]
- Lewandowska, K.; Weisbrot, M.; Cieloszyk, A.; Mędrzycka-Dąbrowska, W.; Krupa, S.; Ozga, D. Impact of alarm fatigue on the work of nurses in an intensive care environment—a systematic review. Int. J. Environ. Res. Public Health 2020, 17, 8409. [Google Scholar] [CrossRef]
- Shanmugham, M.; Strawderman, L.; Babski-Reeves, K.; Bian, L. Alarm-related workload in default and modified alarm settings and the relationship between alarm workload, alarm response rate, and care provider experience: Quantification and comparison study. JMIR Hum. Factors 2018, 5, e11704. [Google Scholar] [CrossRef] [PubMed]
- Winters, B.D.; Cvach, M.M.; Bonafide, C.P.; Hu, X.; Konkani, A.; O’Connor, M.F.; Rothschild, J.M.; Selby, N.M.; Pelter, M.M.; McLean, N.; et al. Society for Critical Care Medicine Alarm and Alert Fatigue Task Force. Technological distractions (part 2): A summary of approaches to manage clinical alarms with intent to reduce alarm fatigue. Crit. Care Med. 2018, 46, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Cvach, M. Monitor alarm fatigue: An integrative review. Biomed. Instrum. Technol. 2012, 46, 268–277. [Google Scholar] [CrossRef]
- Drew, B.J.; Harris, P.; Zègre-Hemsey, J.K.; Mammone, T.; Schindler, D.; Salas-Boni, R.; Bai, Y.; Tinoco, A.; Ding, Q.; Hu, X. Insights into the problem of alarm fatigue with physiologic monitor devices: A comprehensive observational study of consecutive intensive care unit patients. PLoS ONE 2014, 9, e110274. [Google Scholar] [CrossRef]
- Sowan, A.K.; Gomez, T.M.; Tarriela, A.F.; Reed, C.C. Changes in default alarm settings and standard in-service are insufficient to improve alarm fatigue in an intensive care unit: A pilot project. JMIR Hum. Factors 2016, 3, e5098. [Google Scholar] [CrossRef]
- Criscitelli, T. Alarm management: Promoting safety and establishing guidelines. AORN J. 2016, 103, 518–521. [Google Scholar] [CrossRef]
- Imhoff, M.; Kuhls, S. Alarm algorithms in critical care monitoring. Anesth. Analg. 2006, 102, 1525–1537. [Google Scholar] [CrossRef]
- Sieben, W.; Gather, U. Classifying alarms in intensive care-Analogy to hypothesis testing. In Proceedings of the Conference on Artificial Intelligence in Medicine in Europe, Amsterdam, The Netherlands, 7–11 July 2007; Springer: Berlin/Heidelberg, Germany; pp. 130–138. [Google Scholar]
- Imhoff, M.; Morik, K.; Gather, U. Development of Decision Support Algorithms for Intensive Care Medicine: A Hybrid System of Time Series Analysis and a Knowledge Base System. In Proceedings of the The AMIA 2001 Annual Symposium, Washington, DC, USA, 3–7 November 2001; p. 931. [Google Scholar]
- Mira, J.J.; Lorenzo, S.; Carrillo, I.; Ferrús, L.; Silvestre, C.; Astier, P.; Iglesias-Alonso, F.; Maderuelo, J.A.; Pérez-Pérez, P.; Torijano, M.L.; et al. Lessons learned for reducing the negative impact of adverse events on patients, health professionals and healthcare organizations. Int. J. Qual. Health Care 2017, 29, 450–460. [Google Scholar] [CrossRef]
- Funk, M.; Ruppel, H.; Blake, N.; Phillips, J. Research: Use of monitor watchers in hospitals: Characteristics, training, and practices. Biomed. Instrum. Technol. 2016, 50, 428–438. [Google Scholar] [CrossRef]
- Allan, S.H.; Doyle, P.A.; Sapirstein, A.; Cvach, M. Data-driven implementation of alarm reduction interventions in a cardiovascular surgical ICU. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 62–70. [Google Scholar] [CrossRef]
- Cvach, M.M.; Frank, R.J.; Doyle, P.; Stevens, Z.K. Use of pagers with an alarm escalation system to reduce cardiac monitor alarm signals. J. Nurs. Care Qual. 2014, 29, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Schmid, F.; Goepfert, M.S.; Reuter, D.A. Patient monitoring alarms in the ICU and in the operating room. Crit. Care 2013, 17, 216. [Google Scholar] [CrossRef]
- Chromik, J.; Klopfenstein, S.A.I.; Pfitzner, B.; Sinno, Z.C.; Arnrich, B.; Balzer, F.; Poncette, A.S. Computational approaches to alleviate alarm fatigue in intensive care medicine: A systematic literature review. Front. Digit. Health 2022, 4, 843747. [Google Scholar] [CrossRef] [PubMed]
- López-Espuela, F.; Rodríguez-Martin, B.; Garcia, J.L.; Toribio-Felipe, R.; Amarilla-Donoso, F.J.; Rodriguez Almagro, J.J.; Ribeiro, A.S.F.; Fernandes, V.S.; Moran-García, J.M. Experiences and mediating factors in nurses’ responses to electronic device alarms: A phenomenological study. J. Nurs. Manag. 2022, 30, 1303–1316. [Google Scholar] [CrossRef] [PubMed]
- Piri, H.; Huh, W.T.; Shechter, S.M.; Hudson, D. Individualized dynamic patient monitoring under alarm fatigue. Oper. Res. 2022, 70, 2749–2766. [Google Scholar] [CrossRef]
- Guglielmello, G.; Stawicki, S.P. Combating alarm fatigue: The quest for more accurate and safer clinical monitoring equipment. Vignettes Patient Saf. 2019, 4, 93. [Google Scholar]
- Patel, N.Z.; Patel, D.V.; Phatak, A.G.; Patel, V.G.; Nimbalkar, S.M. Reducing false alarms and alarm fatigue from pulse oximeters in a neonatal care unit: A quality improvement study. J. Neonatol. 2022, 36, 135–142. [Google Scholar] [CrossRef]
- Vieira, J.C.F. Human-Centred Design of Clinical Auditory Alarms. Ph.D. Thesis, Universidade de Lisboa, Lisboa, Portugal, 2022. [Google Scholar]
- van Rossum, M.C.; Vlaskamp, L.B.; Posthuma, L.M.; Visscher, M.J.; Breteler, M.J.; Hermens, H.J.; Kalkman, C.J.; Preckel, B. Adaptive threshold-based alarm strategies for continuous vital signs monitoring. J. Clin. Monit. Comput. 2022, 36, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Isma’ila, U.A.; Danyaro, K.U.; Hassan, M.F.; Liew, M.S.; Maiwada, U.D.; Muazu, A.A. Evaluation on bot-IoT dataset enabled reducing false alarm rate for IoT threats. Kepes 2023, 21, 490–504. [Google Scholar]
- Silveira, S.Q.; Nersessian, R.S.F.; Abib, A.D.C.V.; Santos, L.B.; Bellicieri, F.N.; Botelho, K.K.; de Oliveira Lima, H.; de Queiroz, R.M.; dos Anjos, G.S.; dos Santos Fernandes, H.; et al. Decreasing inconsistent alarms notifications: A pragmatic clinical trial in a post-anesthesia care unit. Braz. J. Anesthesiol. 2024, 74, 744456. [Google Scholar] [CrossRef]
- Fernandes, C.O. Patient Monitoring and Caregivers Notification Based on a Reasoning Model to avoid Alarm Fatigue. Ph.D. Thesis, PUC-Rio, Gávea, Brazil, 2019. [Google Scholar]
- Fernandes, C.; Miles, S.; Lucena, C.J.P. Detecting false alarms by analyzing alarm-context information: Algorithm development and validation. JMIR Med. Inform. 2020, 8, e15407. [Google Scholar] [CrossRef]
- Mileski, M.; Brooks, M.; Topinka, J.B.; Hamilton, G.; Land, C.; Mitchell, T.; Mosley, B.; McClay, R. Alarming and/or alerting device effectiveness in reducing falls in long-term care (LTC) facilities? A systematic review. Healthcare 2019, 7, 51. [Google Scholar] [CrossRef]
- WongKinYiu. (n.d.). GitHub—WongKinYiu/yolov7: Implementation of Paper—YOLOv7: Trainable Bag-of-Freebies Sets New State-of-the-Art for Real-Time Object Detectors. GitHub. Available online: https://github.com/WongKinYiu/yolov7 (accessed on 1 February 2025).
- Noorkhokhar. (n.d.). People-Tracking-yolov7/README.md at main · noorkhokhar99/people-tracking-yolov7. GitHub. Available online: https://github.com/noorkhokhar99/people-tracking-yolov7/blob/main/README.md (accessed on 1 February 2025).
- Facebook. (n.d.). GitHub—Facebook/Prophet: Tool for Producing High Quality Forecasts for Time Series Data That Has Multiple Seasonality with Linear or Non-Linear Growth. GitHub. Available online: https://github.com/facebook/prophet (accessed on 1 February 2025).
- Matsuda, S.; Muramatsu, K.; Hayashida, K. Eligibility Classification Logic of the Japanese Long Term Care Insurance. Asian Pac. J. Dis. Manag. 2011, 5, 65–74. [Google Scholar] [CrossRef][Green Version]



| Components | Mathematical Expressions |
|---|---|
| Time in an instant | |
| Nurse-to-patient distance | |
| Urgency context | |
| Clinical context | |
| Nurse availability | |
| Alarm instance | |
| Maximum reachable distance threshold | |
| Minimum urgency threshold | |
| Suppression component | |
| Delay component | |
| Dynamic threshold computed by the LLM | |
| Nurse alert acknowledgment time window |
| Alarm Type | Class | Precision | Recall | F1 Score |
|---|---|---|---|---|
| Baseline | 1 | 0.25 | 0.25 | 0.25 |
| 2 | 0.18 | 0.25 | 0.21 | |
| 3 | 0.16 | 0.25 | 0.19 | |
| 4 | 0.24 | 0.25 | 0.25 | |
| NaN | 0.00 | 0.00 | 0.00 | |
| R(S+D) | 1 | 0.91 | 0.80 | 0.85 |
| 2 | 0.53 | 0.64 | 0.58 | |
| 3 | 0.68 | 0.73 | 0.71 | |
| 4 | 0.72 | 0.67 | 0.69 | |
| NaN | 1.00 | 1.00 | 1.00 | |
| R(S+D+V) | 1 | 1.00 | 0.86 | 0.93 |
| 2 | 0.60 | 0.70 | 0.65 | |
| 3 | 0.56 | 0.80 | 0.66 | |
| 4 | 0.83 | 0.60 | 0.70 | |
| NaN | 1.00 | 1.00 | 1.00 | |
| Proposed | 1 | 1.00 | 1.00 | 1.00 |
| 2 | 1.00 | 0.87 | 0.93 | |
| 3 | 0.87 | 1.00 | 0.93 | |
| 4 | 1.00 | 1.00 | 1.00 | |
| NaN | 1.00 | 1.00 | 1.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nahid, N.; Ahad, M.A.R.; Inoue, S. Context-Aware Alerting in Elderly Care Facilities: A Hybrid Framework Integrating LLM Reasoning with Rule-Based Logic. Sensors 2025, 25, 6560. https://doi.org/10.3390/s25216560
Nahid N, Ahad MAR, Inoue S. Context-Aware Alerting in Elderly Care Facilities: A Hybrid Framework Integrating LLM Reasoning with Rule-Based Logic. Sensors. 2025; 25(21):6560. https://doi.org/10.3390/s25216560
Chicago/Turabian StyleNahid, Nazmun, Md Atiqur Rahman Ahad, and Sozo Inoue. 2025. "Context-Aware Alerting in Elderly Care Facilities: A Hybrid Framework Integrating LLM Reasoning with Rule-Based Logic" Sensors 25, no. 21: 6560. https://doi.org/10.3390/s25216560
APA StyleNahid, N., Ahad, M. A. R., & Inoue, S. (2025). Context-Aware Alerting in Elderly Care Facilities: A Hybrid Framework Integrating LLM Reasoning with Rule-Based Logic. Sensors, 25(21), 6560. https://doi.org/10.3390/s25216560






