1. Introduction
Dental professionals perform lengthy procedures that often require them to assume mechanically disadvantageous postures [
1]. Consequently, musculoskeletal disorders (MSDs) have been widely reported in dental professionals, ranging globally from 10.8% to 92.9% [
2,
3]. According to a 2018 systematic literature review and meta-analysis, MSDs were most reported in the neck (58.5%), lower back (56.4%), shoulder (43.1%), and upper back (41.1%) [
4]. Since MSDs often develop gradually over years or even decades, isolating a single causative factor is inherently challenging, particularly when accounting for the cumulative effects of dental education and subsequent clinical practice [
5]. Nonetheless, prior research has identified correlations between perceived pain and the adoption of mechanically disadvantageous postures in dentistry, suggesting that such postures may serve as early risk indicators for developing MSDs [
6].
According to a 2020 systematic review, there is some evidence suggesting that ergonomic interventions including magnification loupes/microscopes, prismatic spectacles, training courses, specially designed dental chairs, and instruments have the potential to reduce the severity of MSDs by improving work posture among dental professionals [
3]. The extent to which ergonomic interventions are applied in dentistry, as well as the specific barriers to their implementation, remains poorly understood. Strengthening the body of high-quality, objective evidence demonstrating the effectiveness of different interventions will be essential for identifying the best strategies to prioritize incorporating into dental education and clinical practice [
1].
Ergonomics education can be taught through awareness and training exercises. Ergonomic awareness refers to an individual’s general understanding of ergonomic principles, whereas ergonomic training involves structured instruction and practice aimed at applying those principles effectively in specific tasks or work environments. The Commission on Dental Accreditation (CODA), which oversees accreditation for U.S. dental schools, does not currently mandate specific ergonomic training as part of its core standard for predoctoral education, leaving ergonomics training and awareness as a voluntary pursuit in dental education [
7]. The absence of ergonomic training has been found to exacerbate the effects of developing MSDs in dental school, which is direct evidence that ergonomics awareness alone is not a solution to reducing the risk of developing MSDs in new dentists [
8]. Awareness of suggested ergonomic practices alone has been shown to be insufficient to combat the rising prevalence of MSDs within dentistry, though ergonomic training can reduce reported pain [
9]. In a 2016 study, interventions targeting muscles for posture and balance were assessed six months post-intervention [
10]. The intervention group engaged in an eight-week ergonomic intervention that included ergonomic awareness lectures, workstation modification, ergonomic training, surveying ergonomics at the workstation, and a regular exercise program. While the authors reported statistically significant differences in MSDs in multiple body parts [
10], a systematic review determined that the study provided very low-quality evidence for several different reasons, including “inappropriate use of statistical tests and calculation” ([
1] p. 19).
Incorporating ergonomics into dental education is complicated by the tendency of dental students to sacrifice healthy ergonomic behaviors early on in their clinical training. This situation often occurs in favor of completing clinical procedures more efficiently, particularly when indirect vision through mirrors is challenging or when suctioning must be performed without the assistance of a dedicated dental assistant. Additionally, students are unlikely to experience significant pain or discomfort during the early stages of their education, yet the repetitive nature of clinical tasks and the development of muscle memory can lead to the onset of MSDs over time. Therefore, continuous ergonomic training, ideally introduced concurrently with instruction on technical procedures, is essential to effectively address the high rates of MSDs among dental professionals.
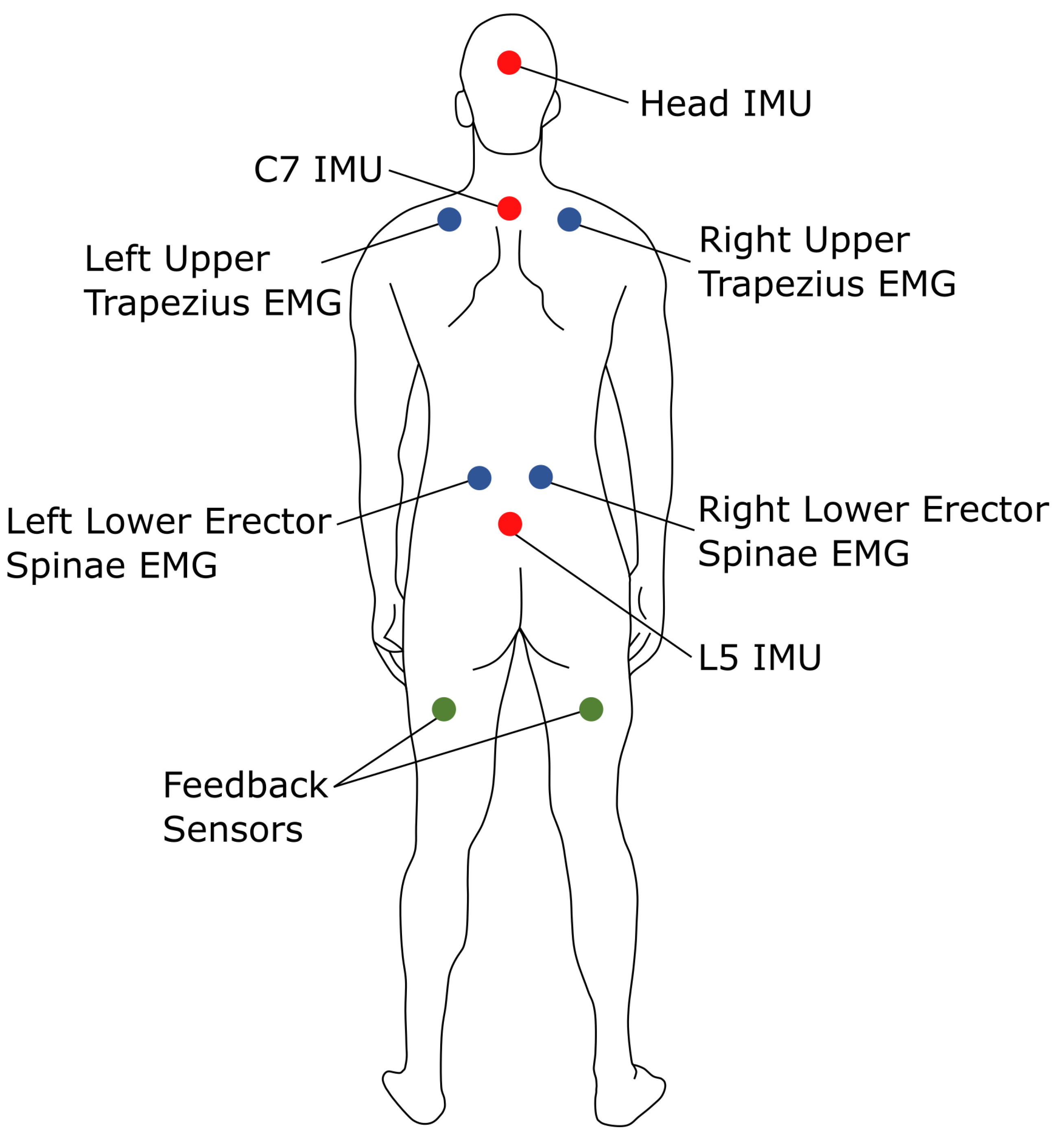
One promising approach to training dental students to adopt healthy biomechanical behaviors is through real-time feedback provided by wearable sensors, whose utility has been demonstrated in multiple settings [
11,
12,
13]. Wearable sensor-driven feedback systems alert users when they maintain mechanically disadvantageous postures for a prolonged period of time, ideally training them to become more mindful of their biomechanical behaviors during typical clinical procedures. As an alternative to previous work that has relied on human observers for real-time feedback, wearable technology offers a scalable, personalized, and calibrated solution or adjunctive tool to support ergonomics training. The goal is not to eliminate specific postures entirely but to foster an environment that prompts frequent postural adjustments throughout a procedure. This approach is guided by the success of intraoperative “micro-breaks” implemented in other surgical settings [
14,
15], which have been shown to reduce the duration of static and often asymmetric loading of their muscles and joints [
16]. Furthermore, these posture changes promote the recruitment of a more diverse set of muscles groups, allowing for intermittent recovery during procedures.
Wearable sensors like inertial measurement units (IMUs) have been utilized extensively for monitoring posture. For example, Porta et al. [
17] used a single IMU to monitor trunk flexion in nurses to quantify how much time was spent in potentially harmful postures. The authors determined that the IMU-based approach was a promising alternative for capturing different biomechanical behaviors over long periods of time compared to traditional methods requiring a human observer. Several studies explicitly integrated the rapid upper limb assessment (RULA) [
18] in combination with IMU data to evaluate the ergonomic risks associated with different postures. For example, Tanthuwapathom et al. [
19] and Humadi et al. [
20] both reported strong agreement between IMU-based and traditional RULA assessments, supporting the use of IMUs for ergonomic screening. However, Nowara et al. [
21] found that applying RULA using IMU data systematically produced higher risk scores than applying RULA using traditional methods, particularly for the arm and wrist, in a study population of 130 dentists and dental assistants. Finally, Carbonaro et al. [
22] monitored one surgeon’s posture during laproscopic surgery to identify prolonged periods of neck extension and trunk flexion. Their results suggested that the surgeon’s RULA scores were high enough to warrant a change in operating conditions. Importantly, the authors also acknowledged the value of also monitoring muscle activation via electromyography (EMG). These studies suggest that, while IMU-based RULA offers greater discriminatory power and objectivity, methodological differences must be considered when interpreting or comparing results across studies or with historical data. Further, there is an opportunity to enhance the ergonomic risk assessment with the addition of EMG sensors.
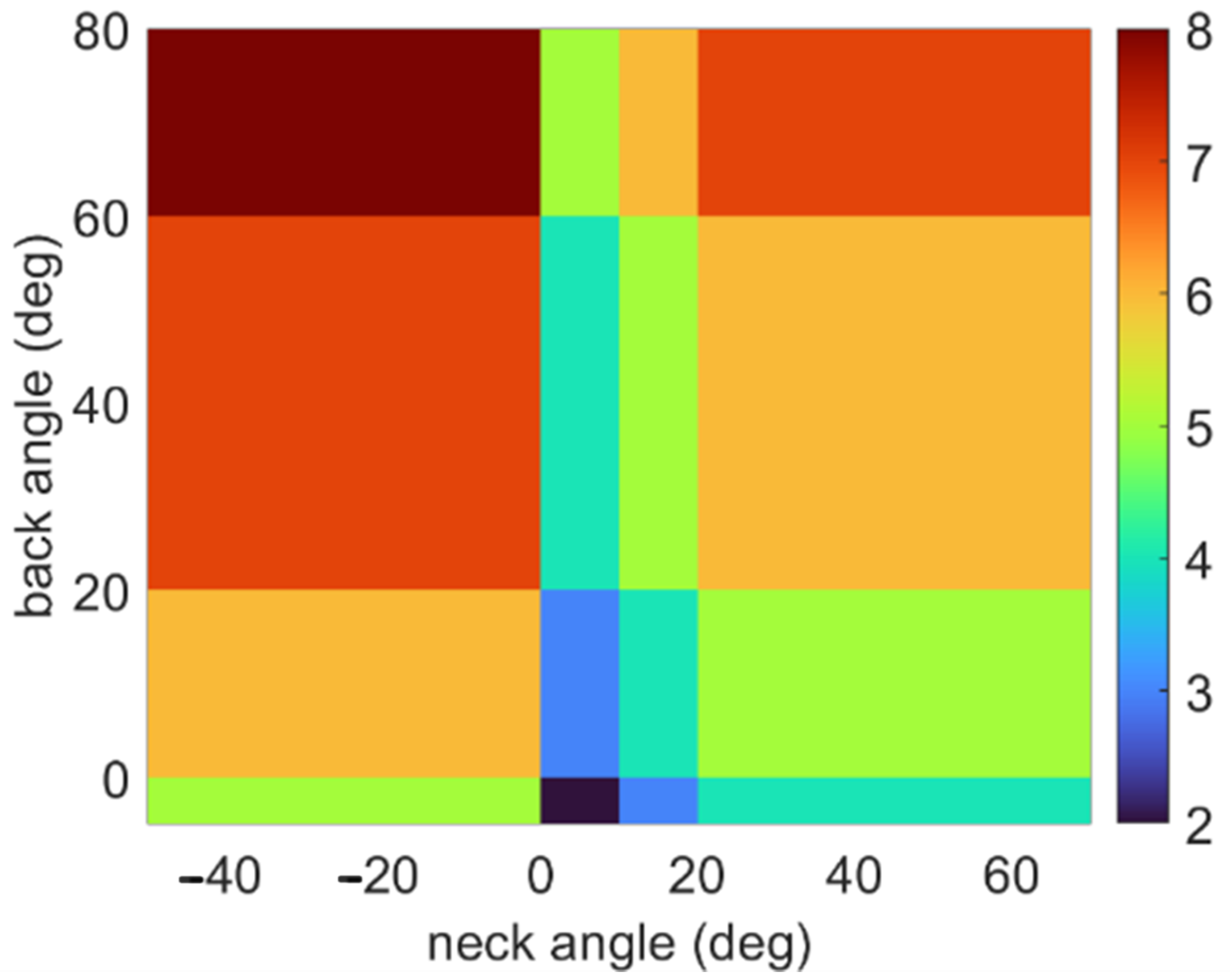
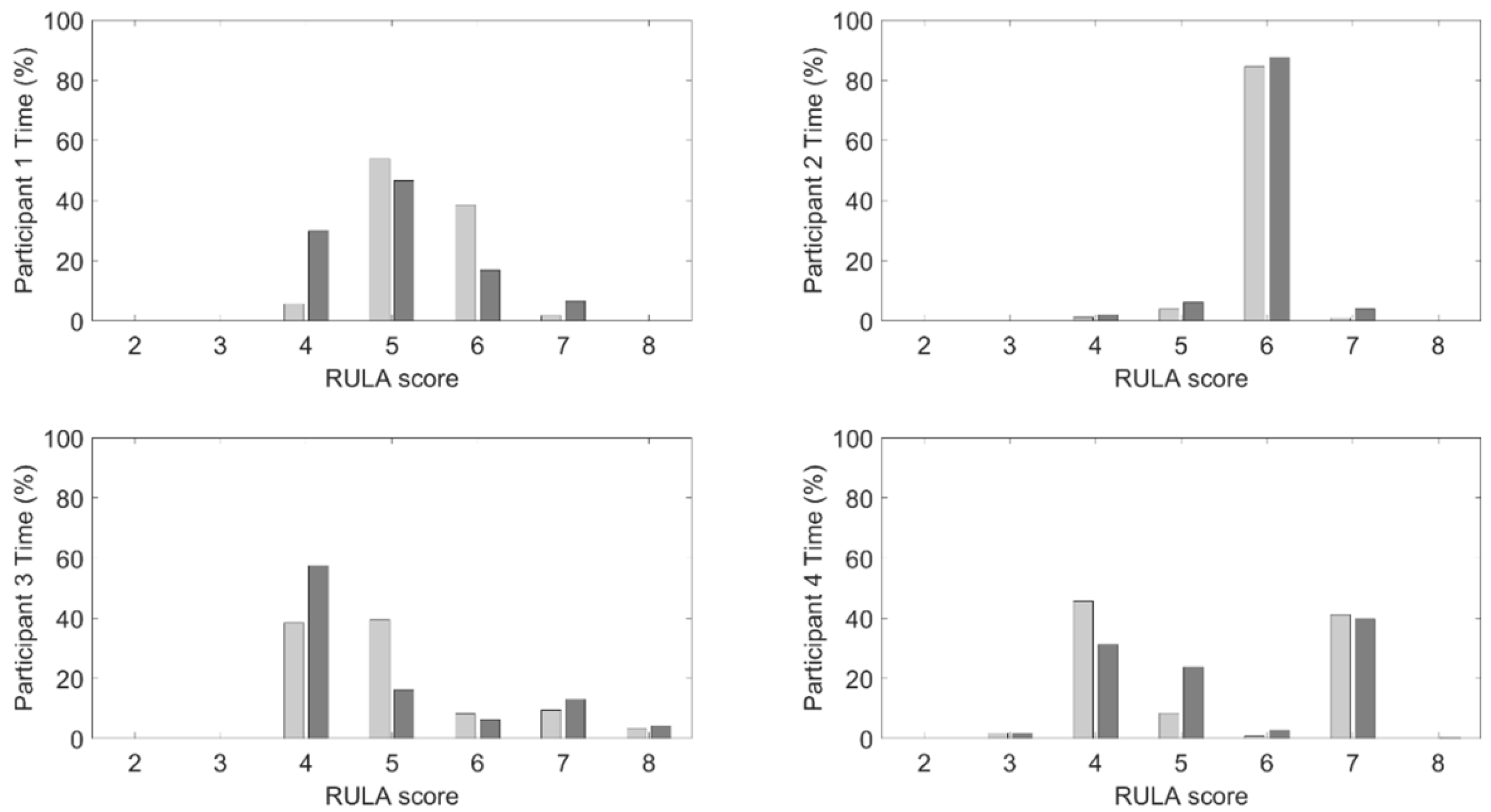
To define what constitutes a mechanically disadvantageous posture in dental settings, this study will also utilize the RULA for guidance [
18]. As described above, this tool enables evaluators to identify a dentist’s worst-case posture, which can guide how to set thresholds for recognizing disadvantageous postures during procedures [
23]. A significant limitation of RULA is its inability to accurately account for posture duration and muscle recovery time [
24], both of which are of interest in this study. Thus, RULA is used in concordance with muscle activation measurements to better understand how the feedback influences not only their posture, but also muscle recruitment. Building upon prior research that has explored the relationship between real-time posture feedback and muscle recruitment [
25], this feasibility study investigates the impact of a novel wearable sensor-based feedback system on postural and muscle activation behaviors during a typical dental procedure.
4. Discussion
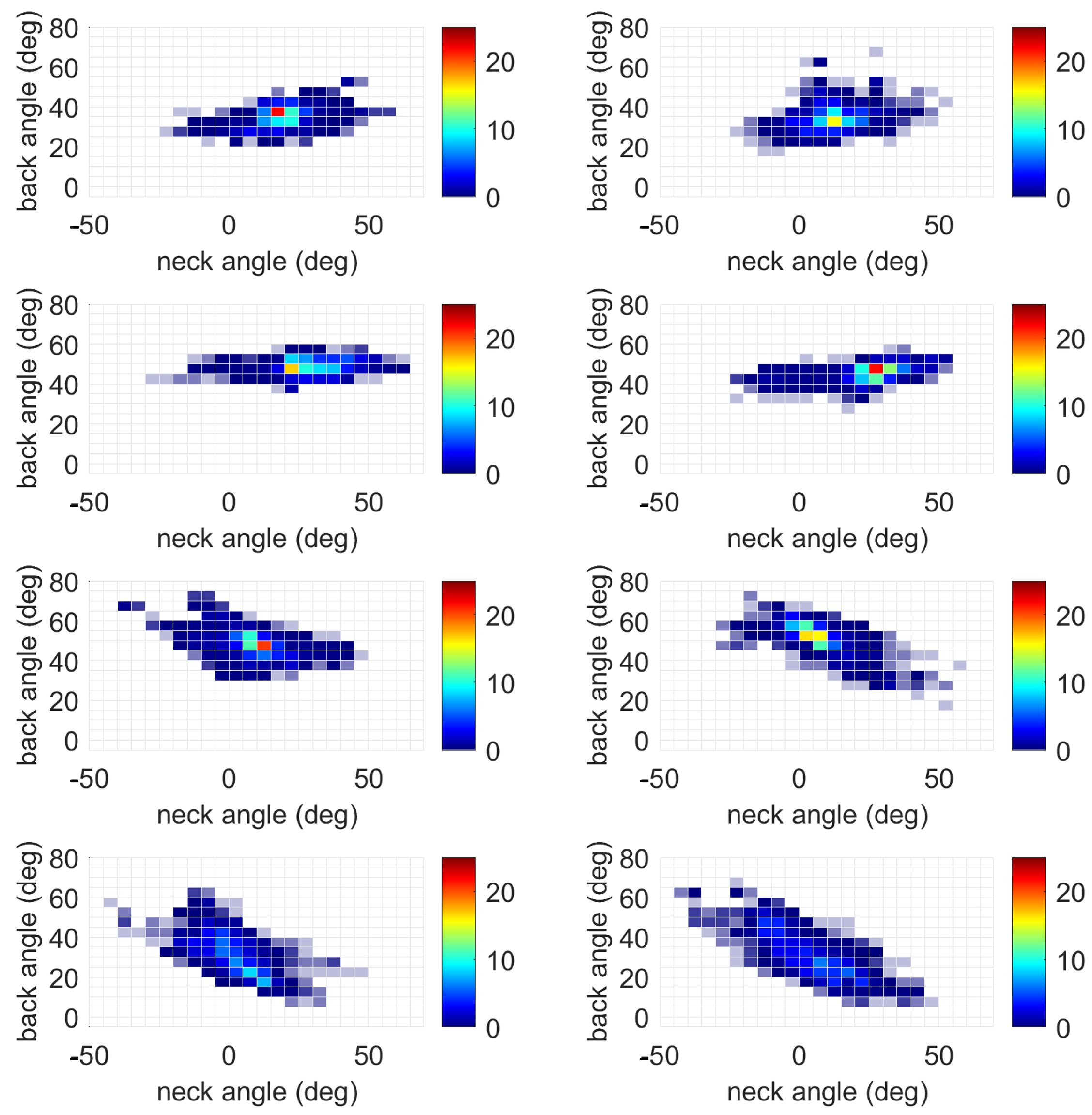
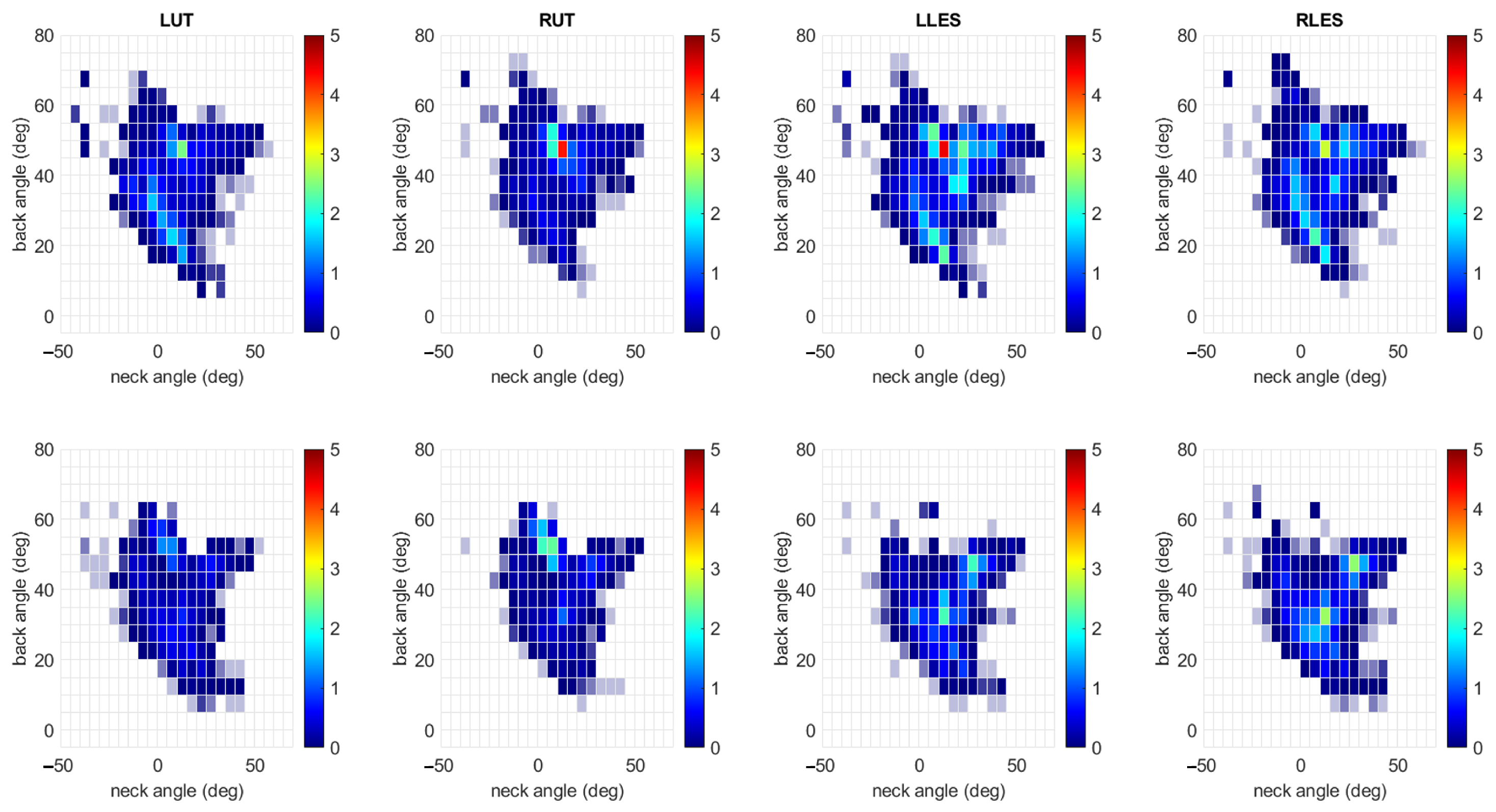
This feasibility study explored the use of a novel wearable sensor-based vibrotactile feedback system to facilitate ergonomic training by promoting ergonomic awareness and training during a standard dental procedure. Interestingly, the most notable outcome of the posture-driven vibrotactile feedback was a reduction in muscle activation. The most consistent effect of the haptic feedback system was observed in a reduction in upper trapezius muscle activation on both sides, though these reductions occurred in the presence of a statistically significant increase in neck angles. However, it should be noted that the neck angles remained on average below the feedback threshold of 20 degrees without (9.7 degrees) and with feedback (13.9 degrees). These changes, however, are relevant given the established link between sustained neck flexion and the development of neck and shoulder pain in dental professionals [
6]. The decrease in muscle activity when feedback was present suggests that participants were more aware of their muscle activation and adjusted their muscle recruitment accordingly, despite the slight increase in neck angle. This finding aligns with prior research on intraoperative micro-breaks in surgical settings, which have been shown to reduce fatigue and improve posture without compromising task performance [
14,
15]. Here, the reduced muscle strain is achieved by providing a vibrotactile stimulus reminding the user to regularly adopt a different posture.
Feedback did not significantly affect the back angle or left erector spinae activation. This finding may be due to the nature of the dental procedure, which requires forward trunk flexion that is difficult to avoid without additional ergonomic equipment such as a microscope or specialized prismatic loupes. Future studies could consider evaluating the effects of such equipment utilizing a wearable sensor system to better understand how the users adapt to the change in their environmental set up. Alternatively, the feedback thresholds or delivery may not have been sensitive enough to prompt consistent changes to improve back posture. Future work should consider different threshold levels or potentially adaptive thresholds that can respond to muscle fatigue. The right erector spinae activation did incur an increase in muscle activity, but the effect sizes suggested that the change was small. These findings highlight the importance of tailoring feedback systems to the specific biomechanical demands of dental tasks and suggest that future iterations may benefit from more nuanced or adaptive feedback algorithms [
13]. It is possible that designing feedback to incorporate muscle activation data could also benefit the user. It is possible that future iterations of ergonomic equipment and assistive devices may be able to offload muscle strain during a procedure while a dentist is in a traditionally mechanically disadvantageous posture. For example, several research groups have explored the use of trunk exoskeletons to offload back muscle loading in a number of different applications including dentistry [
40,
41], surgery [
42,
43], and industrial tasks [
44].
The results regarding the effects of activity type on posture and muscle activation were also notable. In particular, drilling was associated with higher back angles, greater upper trapezius activation, and greater lower erector spinae activation compared to other activities. This finding also reinforces the notion that task-specific ergonomic interventions may be required and provides additional evidence that certain procedures, or tasks within those procedures, may carry a higher risk of MSD development. Educators may consider incorporating targeted ergonomic training during these high-risk activities to reinforce healthy movement patterns. Quantifying the risk associated with different procedures may also be useful when scheduling appointments, with enough rest planned between high-risk activities for recovery [
45].
The findings support the theory that biomechanical awareness, when prompted through real-time feedback, can lead to adaptive motor responses even in novice practitioners, suggesting that wearable feedback systems may serve as effective tools for embedding ergonomic principles into procedural memory during early clinical training. From an educational perspective, the integration of real-time feedback into preclinical training offers several advantages. First, it provides immediate, objective information about posture, which may be more impactful than retrospective ergonomic instruction [
13]. Second, it encourages students to develop self-awareness and self-regulation skills that are essential for long-term musculoskeletal health. Finally, it aligns with competency-based education models by offering individualized, performance-based feedback that can be integrated into existing simulation-based curricula [
46].
If a dental student reports or is being treated for an MSD, the authors of [
45] recommend that the dental faculty assess the student’s understanding of ergonomics through extended observation during clinical and simulation activities. They also highlighted the potential to implement real-time feedback to correct harmful habits, and it is likely that the symptoms will recur post-treatment unless the root cause of the ergonomic issue is determined. Additionally, to address the ergonomic shortcomings in dental education, schools can take proactive steps to mitigate the inevitable development of poor ergonomic behaviors that arise when students are required to work alone, even though dentistry is most effectively practiced with an assistant. One effective strategy is to adapt the curriculum to ensure that students have access to peer support during procedures that demand suctioning, mirror clearing, and moisture control, particularly during times of drilling, in which ergonomic form is often compromised by the need to hold a suction device instead of a mirror. Integrating modern dental innovations such as Isovacs or combination devices that consolidate suction, air, water, and mirror functions can further support ergonomic practices, especially when paired with proper supervision and haptic feedback mechanisms. Early education, hands-on training, and timely correction are essential to reducing the incidence of musculoskeletal disorders (MSDs) among dental students and promoting long-term occupational health.
Current Limitations
The small sample size and single-institution design limit generalizability. Although the statistical power for this study is approximately 10%, indicating limited sensitivity to detect small effects, the findings still offer valuable preliminary insights to inform future research directions, help refine hypotheses, and contribute to the broader understanding of the topic. While the results should be interpreted with caution, the study lays important groundwork for more robust future investigations. Additionally, the use of manikins rather than live patients may not fully replicate the physical and cognitive demands of clinical care. With respect to the sEMG data, a potential uncontrolled error may have been introduced by having a research team member provide the opposing force during the MVC exercises instead of a dynamometer. Additionally, it is possible that skin motion artifacts (i.e., relative motion between the IMU and the underling skeletal structure) may have affected the accuracy of the spinal orientation estimates.
Despite these limitations, this study provides valuable preliminary evidence supporting the feasibility and potential benefits of wearable feedback systems in dental education. Future research should explore the long-term effects of feedback on posture retention, the integration of other feedback modes (e.g., visual or auditory cues), and the impact of such systems on clinical performance and patient outcomes. Future work should explore adaptive thresholds based on posture and possibly muscle activation variability to better tailor feedback timing to individual users and task demands. Larger, multi-institutional, longitudinal studies are needed to validate these findings and inform best practices for implementation.