Center of Mass (CoM) Motions and Foot Placement During Treadmill Walking Using One Time-of-Flight Camera
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
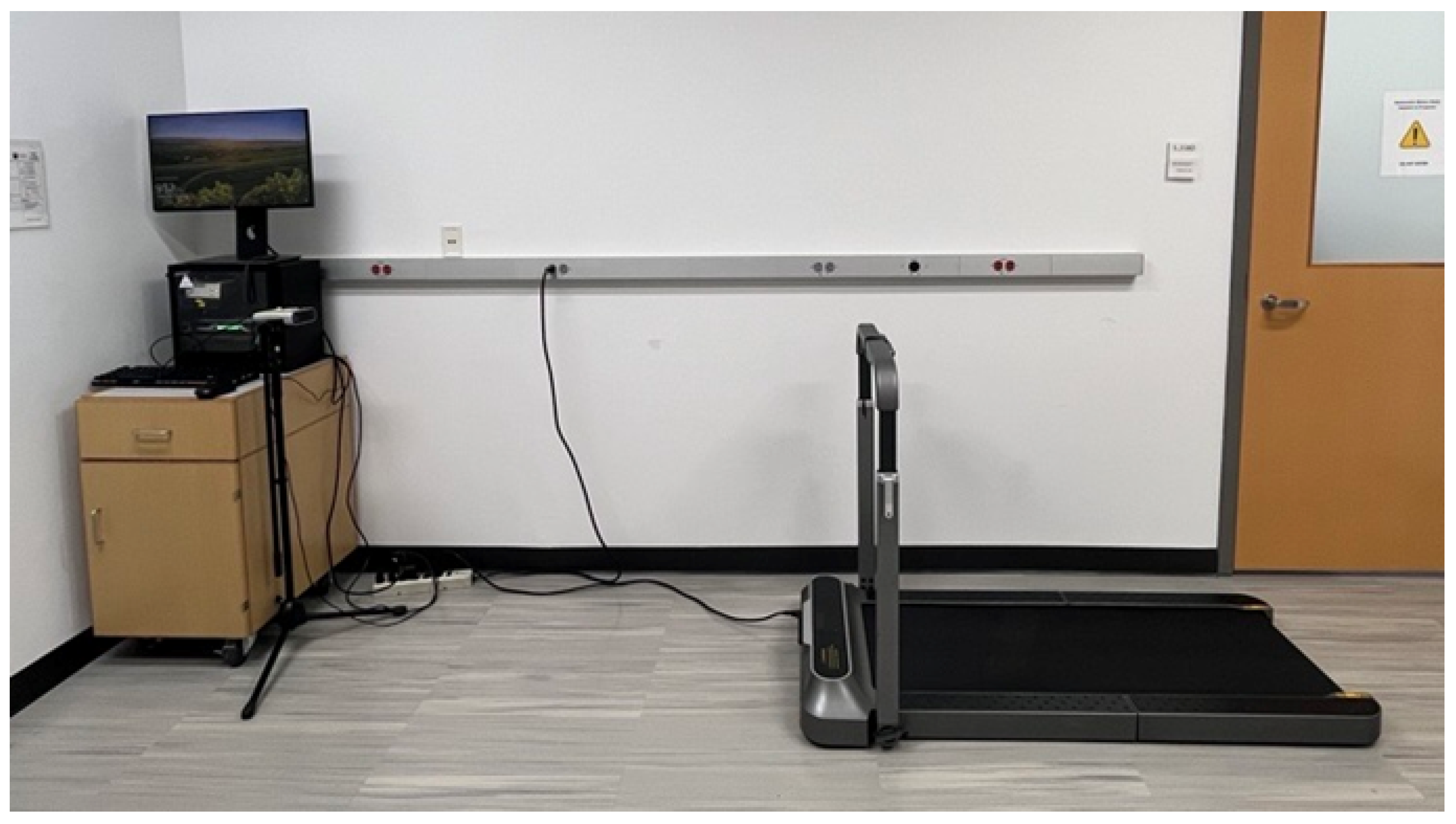
2.2. Hardware and Software
2.3. Data Collection
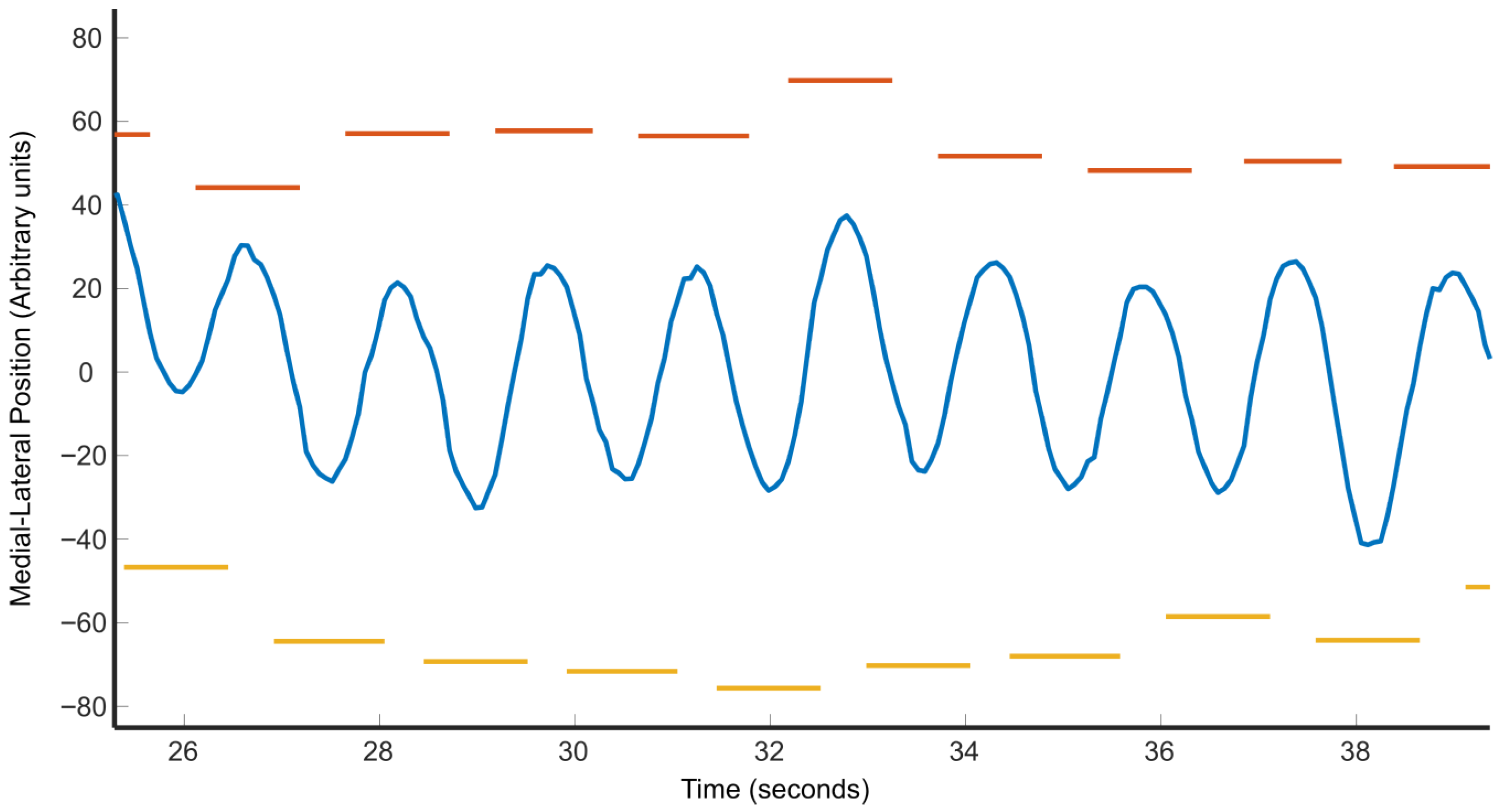
2.4. Data Processing and Metrics Collection
2.4.1. Gait Metrics Processing
2.4.2. CoM Metrics Processing
2.5. Statistical Analysis
2.6. Pregnancy Case Study
3. Results
3.1. Data Quality and Missingness
3.2. Statistical Analysis
3.3. Pregnancy Case Study
4. Discussions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lord, S.R.; Sherrington, C.; Naganathan, V. (Eds.) Falls in Older People: Risk Factors, Strategies for Prevention and Implications for Practice, 3rd ed.; Cambridge University Press: Cambridge, UK, 2021. [Google Scholar]
- Adolph, K.E.; Cole, W.G.; Komati, M.; Garciaguirre, J.S.; Badaly, D.; Lingeman, J.M.; Chan, G.L.Y.; Sotsky, R.B. How Do You Learn to Walk? Thousands of Steps and Dozens of Falls per Day. Psychol. Sci. 2012, 23, 1387–1394. [Google Scholar] [CrossRef]
- Dunning, K.; LeMasters, G.; Bhattacharya, A. A Major Public Health Issue: The High Incidence of Falls During Pregnancy. Matern. Child Health J. 2010, 14, 720–725. [Google Scholar] [CrossRef]
- Neri, S.G.; Oliveira, J.S.; Dario, A.B.; Lima, R.M.; Tiedemann, A. Does Obesity Increase the Risk and Severity of Falls in People Aged 60 Years and Older? A Systematic Review and Meta-analysis of Observational Studies. J. Gerontol. Ser. A 2020, 75, 952–960. [Google Scholar] [CrossRef] [PubMed]
- Reeves, N.D.; Orlando, G.; Brown, S.J. Sensory-Motor Mechanisms Increasing Falls Risk in Diabetic Peripheral Neuropathy. Medicina 2021, 57, 457. [Google Scholar] [CrossRef]
- Nnodim, J.O.; Yung, R.L. Balance and its Clinical Assessment in Older Adults—A Review. J. Geriatr. Med. Gerontol. 2015, 1, 003. [Google Scholar] [CrossRef]
- Beck Jepsen, D.; Robinson, K.; Ogliari, G.; Montero-Odasso, M.; Kamkar, N.; Ryg, J.; Freiberger, E.; Masud, T. Predicting Falls in Older Adults: An Umbrella Review of Instruments Assessing Gait, Balance, and Functional Mobility. BMC Geriatr. 2022, 22, 615. [Google Scholar] [CrossRef] [PubMed]
- Moro, M.; Marchesi, G.; Hesse, F.; Odone, F.; Casadio, M. Markerless vs. Marker-Based Gait Analysis: A Proof of Concept Study. Sensors 2022, 22, 2011. [Google Scholar] [CrossRef] [PubMed]
- Kudzia, P.; Jackson, E.; Dumas, G. Estimating Body Segment Parameters from Three-Dimensional Human Body Scans. PLoS ONE 2022, 17, e0262296. [Google Scholar] [CrossRef]
- Lam, W.W.T.; Tang, Y.M.; Fong, K.N.K. A Systematic Review of the Applications of Markerless Motion Capture (MMC) Technology for Clinical Measurement in Rehabilitation. J. Neuroeng. Rehabil. 2023, 20, 57. [Google Scholar] [CrossRef]
- Wang, Y.; Mei, Q.; Jiang, H.; Hollander, K.; Van Den Berghe, P.; Fernandez, J.; Gu, Y. The Biomechanical Influence of Step Width on Typical Locomotor Activities: A Systematic Review. Sport. Med.-Open 2024, 10, 83. [Google Scholar] [CrossRef]
- Cheung, D.; Cheung, J.; Cheung, V.; Jin, L. A New Quantitative Gait Analysis Method Based on Oscillatory Mechanical Energies Measured near Body Center of Mass. Sensors 2022, 22, 8656. [Google Scholar] [CrossRef]
- Hulleck, A.A.; Menoth Mohan, D.; Abdallah, N.; El Rich, M.; Khalaf, K. Present and Future of Gait Assessment in Clinical Practice: Towards the Application of Novel Trends and Technologies. Front. Med. Technol. 2022, 4, 901331. [Google Scholar] [CrossRef]
- Bruijn, S.M.; Van Dieën, J.H. Control of Human Gait Stability through Foot Placement. J. R. Soc. Interface 2018, 15, 20170816. [Google Scholar] [CrossRef]
- Lu, H.L.; Kuo, M.Y.; Chang, C.F.; Lu, T.W.; Hong, S.W. Effects of gait on the body’s center of mass relative to center of pressure during over-ground walking. Hum. Mov. Sci. 2017, 54, 354–362. [Google Scholar] [CrossRef]
- Malloggi, C.; Rota, V.; Catino, L.; Malfitano, C.; Scarano, S.; Soranna, D.; Zambon, A.; Tesio, L. Three-Dimensional Path of the Body Centre of Mass during Walking in Children: An Index of Neural Maturation. Int. J. Rehabil. Res. 2019, 42, 112–119. [Google Scholar] [CrossRef]
- Reimann, H.; Fettrow, T.; Jeka, J.J. Strategies for the Control of Balance During Locomotion. Kinesiol. Rev. 2018, 7, 18–25. [Google Scholar] [CrossRef]
- Winter, D.A. Human Balance and Posture Control during Standing and Walking. Gait Posture 1995, 3, 193–214. [Google Scholar] [CrossRef]
- Bauby, C.E.; Kuo, A.D. Active Control of Lateral Balance in Human Walking. J. Biomech. 2000, 33, 1433–1440. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, M.K.; Mille, M.L. Lateral stability and falls in older people. Exer. Sport Sci. Rev. 2003, 31, 182–187. [Google Scholar]
- Robinovitch, S.N.; Feldman, F.; Yang, Y.; Schonnop, R.; Leung, P.M.; Sarraf, T.; Sims-Gould, J.; Loughin, M. Video capture of the circumstances of falls in elderly people residing in long term care: An observational study. Lancet 2013, 381, 47–54. [Google Scholar] [CrossRef]
- Sidaway, B.; Bennett, J.; Berenyi, S.; Bryant, P.; Cushman, K.; DiMonte, R.; Downing, K.; Gleeson, S.; McGibney, S.; Minard, H.; et al. The Identification of Fall Risk through Tests of Mediolateral Stability during Gait. Exp. Gerontol. 2022, 163, 111803. [Google Scholar] [CrossRef]
- Riley, P.O.; Paolini, G.; Della Croce, U.; Paylo, K.W.; Kerrigan, D.C. A Kinematic and Kinetic Comparison of Overground and Treadmill Walking in Healthy Subjects. Gait Posture 2007, 26, 17–24. [Google Scholar] [CrossRef]
- Watt, J.R.; Franz, J.R.; Jackson, K.; Dicharry, J.; Riley, P.O.; Kerrigan, D.C. A Three-Dimensional Kinematic and Kinetic Comparison of Overground and Treadmill Walking in Healthy Elderly Subjects. Clin. Biomech. 2010, 25, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.; Youm, C.; Park, H.; Lee, M.; Noh, B. Characteristics of Gait Variability in the Elderly While Walking on a Treadmill with Gait Speed Variation. Int. J. Environ. Res. Public Health 2021, 18, 4704. [Google Scholar] [CrossRef]
- Krkeljas, Z. Changes in gait and posture as factors of dynamic stability during walking in pregnancy. Hum. Mov. Sci. 2018, 58, 315–320. [Google Scholar] [CrossRef]
- Beauchet, O.; Allali, G.; Sekhon, H.; Verghese, J.; Guilain, S.; Steinmetz, J.P.; Kressig, R.W.; Barden, J.M.; Szturm, T.; Launay, C.P.; et al. Guidelines for Assessment of Gait and Reference Values for Spatiotemporal Gait Parameters in Older Adults: The Biomathics and Canadian Gait Consortiums Initiative. Front. Hum. Neurosci. 2017, 11, 353. [Google Scholar] [CrossRef] [PubMed]
- Tesio, L.; Rota, V. The Motion of Body Center of Mass During Walking: A Review Oriented to Clinical Applications. Front. Neurol. 2019, 10, 999. [Google Scholar] [CrossRef] [PubMed]
- Patejak, S.; Forrest, J.; Harting, E.; Sisk, M.; Schussler, E. A Systematic Review of Center of Mass as a Measure of Dynamic Postural Control Following Concussion. Int. J. Sports Phys. Ther. 2021, 16, 1222–1234. [Google Scholar] [CrossRef]
- Baček, T.; Oetomo, D.; Tan, Y. Gait Adaptations Under Functional Asymmetry: Exploring the Role of Step Width, Step Length, and CoM in Lateral Stability. In Proceedings of the 2025 International Conference On Rehabilitation Robotics (ICORR), Chicago, IL, USA, 12–16 May 2025. [Google Scholar] [CrossRef]
- Takada, Y.; Atomi, T.; Yagi, T.; Yamamoto, S.; Tomita, M.; Shimizu, M.; Atomi, Y. Effects of step width and gait speed on the variability of mediolateral control in the head and trunk during gait. PLoS ONE 2025, 20, e0320652. [Google Scholar] [CrossRef]
- Guimaraes, V.; Sousa, I.; Correia, M.V. Gait events detection from heel and toe trajectories: Comparison of methods using multiple datasets. In Proceedings of the 2021 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Lausanne, Switzerland, 23–25 June 2021; pp. 1–6. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, B.; Zhou, Z.; Cai, S.; Xie, L. A Novel Center of Mass (CoM) Perception Approach for Lower-Limbs Stroke Rehabilitation. In Social Robotics; Li, H., Ge, S.S., Wu, Y., Wykowska, A., He, H., Liu, X., Li, D., Perez-Osorio, J., Eds.; Springer International Publishing: Cham, Switzerland, 2021; Volume 13086, pp. 606–615. [Google Scholar] [CrossRef]
- Whittle, M.W. Three-Dimensional Motion of the Center of Gravity of the Body during Walking. Hum. Mov. Sci. 1997, 16, 347–355. [Google Scholar] [CrossRef]
- Al-Makhalas, A.; Abualait, T.; Ahsan, M.; Abdulaziz, S.; Al Muslem, W. A Gender Based Comparison and Correlation of Spatiotemporal Gait Parameters and Postural Stability. Acta Biomed. Atenei Parm. 2023, 94, e2023057. [Google Scholar] [CrossRef]
- Minetti, A.E.; Cisotti, C.; Mian, O.S. The Mathematical Description of the Body Centre of Mass 3D Path in Human and Animal Locomotion. J. Biomech. 2011, 44, 1471–1477. [Google Scholar] [CrossRef]
- Tesio, L.; Rota, V.; Chessa, C.; Perucca, L. The 3D Path of Body Centre of Mass during Adult Human Walking on Force Treadmill. J. Biomech. 2010, 43, 938–944. [Google Scholar] [CrossRef] [PubMed]
- Lulic, T.J.; Muftic, O. Trajectory of the Human Body Mass Centre during Walking at Different Speed. In Proceedings of the DS 30: DESIGN 2022, 7th International Deisgn Conference, Dubrovnik, Croatia, 14–17 May 2002. [Google Scholar]
- McAndrew-Young, P.M.; Dingell, J.B. Voluntarily changing step length or step width affects dynamic stability of human walking. Gait Posture 2012, 35, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Hof, A.L.; Gazendam, M.G.J.; Sinke, W.E. The Condition for Dynamic Stability. J. Biomech. 2005, 38, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Hof, A.L.; Curtze, C. A Stricter Condition for Standing Balance after Unexpected Perturbations. J. Biomech. 2016, 49, 580–585. [Google Scholar] [CrossRef]
- Hof, A.L.; Vermerris, S.M.; Gjaltema, W.A. Balance Responses to Lateral Perturbations in Human Treadmill Walking. J. Exp. Biol. 2010, 213, 2655–2664. [Google Scholar] [CrossRef]



| Gait Metrics | CoM Metrics |
|---|---|
| Stride Length | COM Fore Aft |
| Stride Times | COM Width |
| Single Support Times | COM Length |
| Double Support Times | |
| Step Width |
| Metric | Male Mean (SD) | Female Mean (SD) | t-Value | p-Value |
|---|---|---|---|---|
| Left Stride Length | 705.39 (111.68) | 678.22 (88.83) | 0.6069 | 0.5515 |
| Left Stride Time | 0.71 (0.23) | 0.74 (0.23) | −0.3605 | 0.7227 |
| Right Stride Length | 689.27 (106.26) | 658.91 (87.54) | 0.7012 | 0.4921 |
| Right Stride Time | 0.71 (0.24) | 0.74 (0.25) | −0.3071 | 0.7623 |
| Left SS Time | 0.58 (0.16) | 0.55 (0.25) | 0.3062 | 0.7630 |
| Right SS Time | 0.56 (0.17) | 0.55 (0.23) | 0.0833 | 0.9345 |
| Left to Right DS Time | 0.50 (0.38) | 0.46 (0.42) | 0.1835 | 0.8564 |
| Right to Left DS Time | 0.48 (0.38) | 0.47 (0.41) | 0.0861 | 0.9323 |
| CoM Fore-Aft | 31.29 (4.81) | 34.17 (5.95) | −1.1704 | 0.2571 |
| CoM Width | 41.56 (10.69) | 52.88 (13.09) | −2.0834 | 0.0517 |
| CoM Height | 28.54 (9.66) | 27.53 (6.98) | 0.2717 | 0.7889 |
| Step Width | 159.79 (37.98) | 130.33 (23.95) | 2.1159 | 0.0486 |
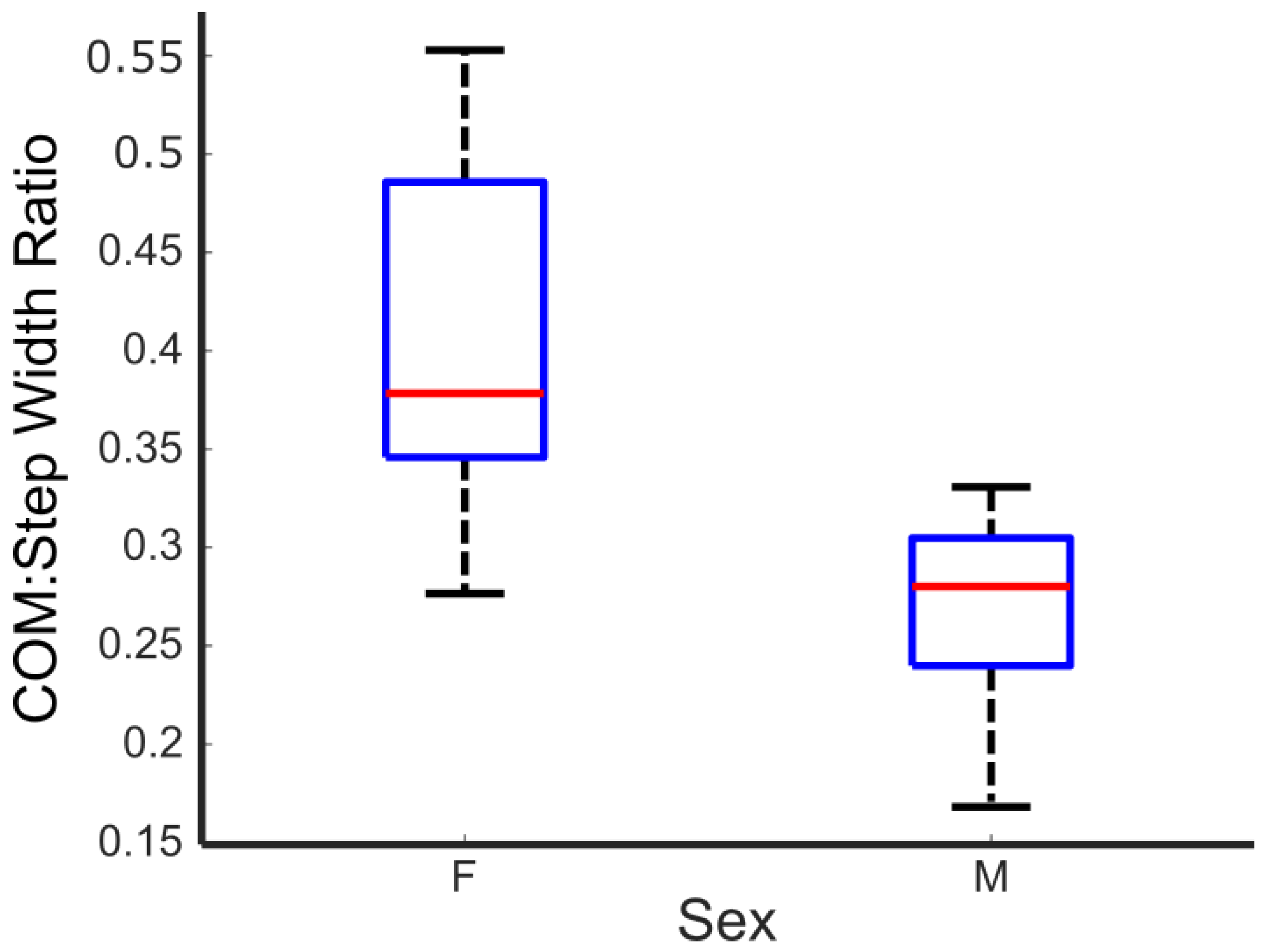
| CoM:Step Width Ratio * | 0.27 (0.05) | 0.41 (0.09) | −4.2519 | 0.0005 |
| Metric | SE | t-Value | p-Value | ||
|---|---|---|---|---|---|
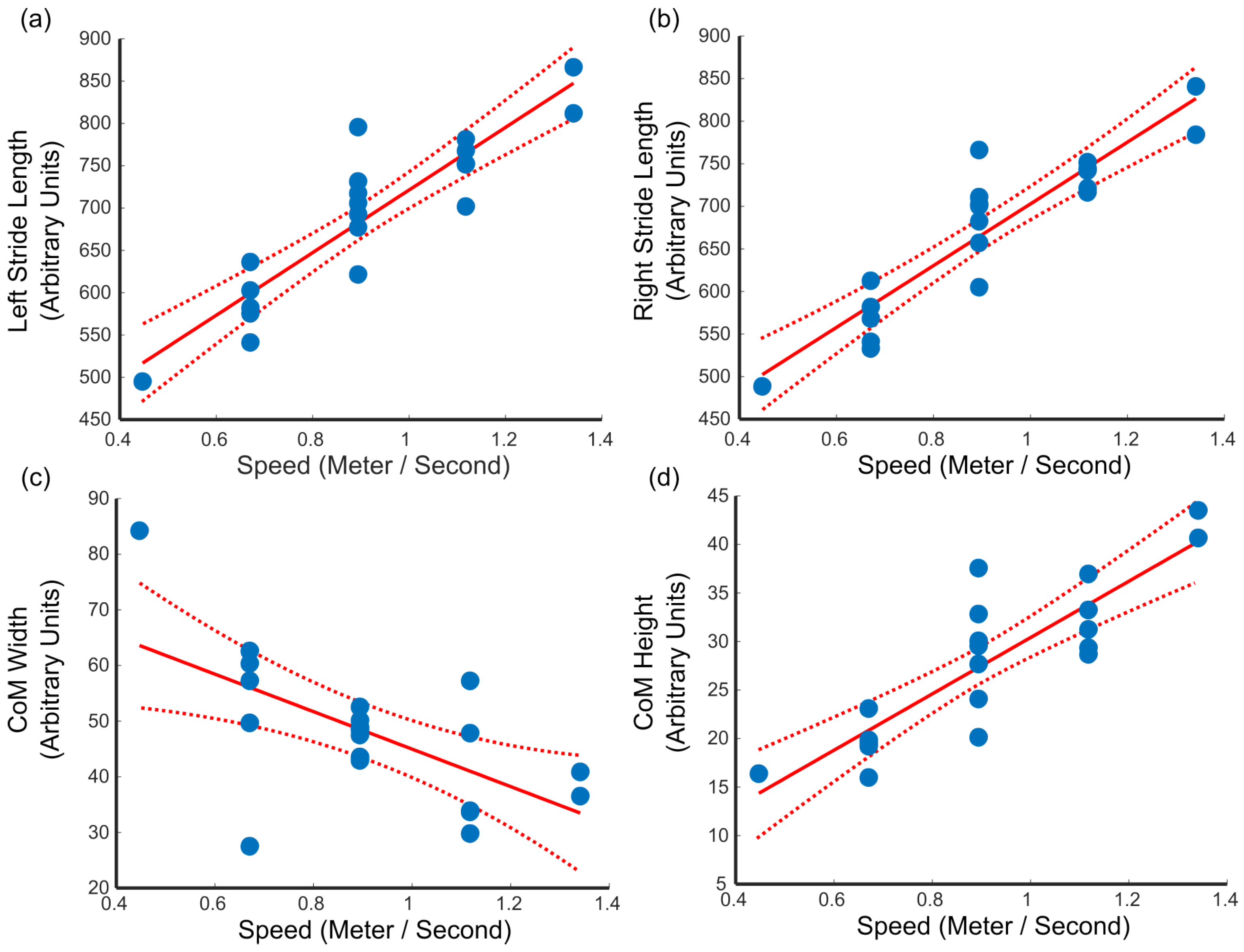
| Left Stride Length * | 369.973 | 41.179 | 8.985 | <0.001 | 0.818 |
| Left Stride Time | −0.234 | 0.217 | −1.077 | 0.296 | 0.061 |
| Right Stride Length * | 362.660 | 37.984 | 9.548 | <0.001 | 0.835 |
| Right Stride Time | −0.240 | 0.228 | −1.053 | 0.306 | 0.058 |
| Left SS Time | −0.091 | 0.207 | −0.441 | 0.664 | 0.011 |
| Right SS Time | −0.187 | 0.192 | −0.970 | 0.345 | 0.050 |
| Left to Right DS Time | −0.217 | 0.381 | −0.571 | 0.575 | 0.018 |
| Right to Left DS Time | −0.240 | 0.380 | −0.633 | 0.535 | 0.022 |
| CoM Fore-Aft | −7.951 | 5.104 | −1.558 | 0.137 | 0.119 |
| CoM Width * | −33.696 | 10.162 | −3.316 | 0.004 | 0.379 |
| CoM Height * | 29.022 | 4.049 | 7.168 | <0.001 | 0.741 |
| Step Width | 10.559 | 33.076 | 0.319 | 0.753 | 0.006 |
| CoM/Step Width Ratio | −0.253 | 0.084 | −3.023 | 0.007 | 0.337 |
| Metric | 3-Month Mean (SD) | 8-Month Mean (SD) | p-Value |
|---|---|---|---|
| CoM fore-aft | 36.40 (12.51) | 33.64 (13.39) | 0.0001 |
| CoM width | 50.14 (11.18) | 58.98 (11.43) | <0.0001 |
| CoM height | 27.69 (4.25) | 31.60 (3.95) | <0.0001 |
| Step width | 138.70 (22.48) | 141.67 (22.42) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, J.T.; Ragatz, A.; Ganesh, A.; Quiros Padilla, A.P.; Devins, M.R.; Mihova, C.V.; Milton, J.G. Center of Mass (CoM) Motions and Foot Placement During Treadmill Walking Using One Time-of-Flight Camera. Sensors 2025, 25, 5850. https://doi.org/10.3390/s25185850
Chang JT, Ragatz A, Ganesh A, Quiros Padilla AP, Devins MR, Mihova CV, Milton JG. Center of Mass (CoM) Motions and Foot Placement During Treadmill Walking Using One Time-of-Flight Camera. Sensors. 2025; 25(18):5850. https://doi.org/10.3390/s25185850
Chicago/Turabian StyleChang, Joshua T., Alisha Ragatz, Anjana Ganesh, Ana P. Quiros Padilla, Mikayla R. Devins, Christina V. Mihova, and John G. Milton. 2025. "Center of Mass (CoM) Motions and Foot Placement During Treadmill Walking Using One Time-of-Flight Camera" Sensors 25, no. 18: 5850. https://doi.org/10.3390/s25185850
APA StyleChang, J. T., Ragatz, A., Ganesh, A., Quiros Padilla, A. P., Devins, M. R., Mihova, C. V., & Milton, J. G. (2025). Center of Mass (CoM) Motions and Foot Placement During Treadmill Walking Using One Time-of-Flight Camera. Sensors, 25(18), 5850. https://doi.org/10.3390/s25185850






